Professional Documents
Culture Documents
Brenner 2009
Uploaded by
OanaDavidCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Brenner 2009
Uploaded by
OanaDavidCopyright:
Available Formats
ORIGINAL ARTICLE
Risk Factors for Recurrence After Repair
of Enterocutaneous Fistula
Megan Brenner, MD, MS; John L. Clayton, MD, PhD; Areti Tillou, MD, MSEd;
Jonathan R. Hiatt, MD; H. G. Cryer, MD, PhD
Objectives: To assess outcomes after repair of entero- cluded the presence of inflammatory bowel disease (OR,
cutaneous fistulae (ECF) and identify factors that pre- 4.9; 95% CI, 1.5-16.1), interval between diagnosis and
dict mortality and recurrence. operation of 36 weeks or longer (OR, 5.4; 95% CI, 1.8-
16.4), location of fistulae in the small intestine (OR, 9.8;
Design: Retrospective study. 95% CI, 1.7-57.6), and resection with stapled anastomo-
sis (OR, 4.1; 95% CI, 1.3-13.2). Recurrence of ECF was
Setting: University hospital. 35% with resection and stapled anastomosis, 22% with
simple oversew, and 11% with resection and hand-sewn
Patients: One hundred thirty-five patients undergoing anastomosis. Recurrence of ECF was 12% when opera-
ECF repair between 1989 and 2005. tion was performed prior to 36 weeks from diagnosis,
compared with 36% if performed at or beyond 36 weeks.
Main Outcome Measures: Mortality and recurrence
of ECF. Conclusions: The primary determinant of mortality af-
ter ECF repair is a failed operation leading to recur-
Results: Definitive operation for ECF was attempted in rence of the fistula. Risk factors for ECF recurrence in-
135 patients. Mortality was 8%, recurrence was 17%, and clude inflammatory bowel disease, fistula located in the
84% of patients eventually survived with a closed fis- small intestine, an interval of 36 weeks or longer be-
tula. The primary determinant of mortality was ECF re- tween diagnosis and operation, and resection with stapled
currence (odds ratio [OR], 6.7; 95% confidence interval anastomosis.
[CI], 1.9-23.4). Factors independently associated with
ECF recurrence by multivariate logistic regression in- Arch Surg. 2009;144(6):500-505
E
NTEROCUTANEOUS FISTULAE attempted definitive surgical repair vary
(ECF) are challenging sur- between 9% and 33% and have not im-
gical problems. The prin- proved in recent years.1,4-6
ciples of management are The present study was undertaken to
well established and begin analyze a current series of patients with
with resuscitation, sepsis control, nutri- ECF in a large university medical center
tional support, anatomical characteriza- and to identify variables affecting the out-
tion, and adequate drainage of fistula ef- come of operative repair. We hypoth-
fluent.1,2 Fewer than 25% of ECF will close esized that nutritional repletion, delay of
spontaneously,3 with the remainder re- operative therapy for at least 3 months, re-
quiring operative repair. section of the intestinal segment contain-
ing the ECF, and restoration of intestinal
CME available online at continuity with a hand-sewn, 2-layer anas-
www.jamaarchivescme.com tomosis would minimize recurrence and
and questions on page 495 mortality.
Recent advances in nutritional sup- METHODS
Author Affiliations: Division
of General Surgery,
port, interventional radiology, and wound
Department of Surgery, management have greatly improved op- PATIENTS
David Geffen School of tions for treatment of ECF, with a de-
Medicine at University cline in overall mortality to 3% to 12%. De- We reviewed records of all patients who un-
of California, Los Angeles. spite this decline, recurrence rates after derwent an index definitive surgical proce-
(REPRINTED) ARCH SURG/ VOL 144 (NO. 6), JUNE 2009 WWW.ARCHSURG.COM
500
©2009 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a University of Manitoba User on 06/08/2015
dure for the treatment of ECF originating from the stomach,
duodenum, small bowel, or colon at University of California, Table 1. Comorbid Conditions in 135 Patients
Los Angeles (UCLA) Medical Center from January 1989 to De- With Enterocutaneous Fistulae
cember 2005. Enteroenteric, enterovesical, enterovaginal, and
peristomal fistulae were excluded. Preoperative data selected Condition No. (%)
for retrieval included age, sex, etiology, prior abdominal Cancer 32 (24)
operations, comorbidities, serum analyte levels (albumin, Inflammatory bowel disease 31 (23)
prealbumin, creatinine), immunosuppression (corticoste- Immunosuppression 23 (17)
roids, antirejection medications, or infection with human im- Diverticulitis 18 (13)
munodeficiency virus), type of nutritional support, location of Diabetes mellitus 10 (7)
fistula, referral from outside institution, time from diagnosis Hypertension 22 (16)
to operation, and elective or emergent operation. Operative de- Chronic obstructive pulmonary disease 5 (4)
tails included resection vs direct repair of the fistula, type of Congestive heart failure 3 (3)
anastomosis (hand-sewn vs stapled), blood loss, and degree of Prior irradiation 8 (6)
adhesiolysis. Postoperative information included fistula recur-
rence and mortality. This study was approved by the institu-
tional review board at UCLA.
Table 2. Rate of Enterocutaneous Fistula Recurrence
by Interval From Diagnosis to Operation
STATISTICAL ANALYSES
No. (%)
Univariate and multivariate analyses were performed using Pear-
son 2 test, Fisher exact test for categorical variables, and analy- Interval, wk Patients Recurrence
sis of variance for continuous variables. Unadjusted analyses
⬍2 7 (5) 0
were performed to assess whether any preoperative risk fac- 2-6 12 (9) 1 (8)
tors, comorbidities, operative technique, or postoperative com- 7-12 15 (11) 2 (27)
plications were associated with recurrence and mortality. Mul- 13-36 70 (52) 7 (10)
tivariate logistic regression was performed to identify factors ⬎36 31 (23) 11 (36)
that independently predicted recurrence or death after defini-
tive repair of ECF. The Hosmer-Lemeshow goodness-of-fit test
was used to determine the percentage of variance accounted and 7 with anastomotic leak and peritonitis. Difficult ad-
for by the final multivariate model.
hesiolysis was described in 97 operations (72%). Opera-
tive techniques for repair of fistulae included resection
RESULTS and hand-sewn, 2-layer anastomosis in 91 patients (67%);
resection and stapled anastomosis in 26 patients (19%);
We identified 135 patients who underwent definitive sur- and direct repair by simple oversew techniques in 18 pa-
gical repair of ECF at UCLA Medical Center from 1989 tients (13%). Abdominal wall defects required mesh clo-
to 2005. The mean age was 54 years, and 53% were male. sure in 19 patients (14%). Mean estimated blood loss was
Sites of fistulae included small bowel in 90 patients (67%), 483 mL (range, 0-2200 mL).
colon in 44 patients (33%), duodenum in 3 patients (2%), For the 18 patients in whom oversew techniques were
and stomach in 2 patients (2%). Some patients had fis- used, adhesions were too dense or vascular to allow com-
tulae in more than one location. Comorbidities are shown plete dissection of the involved intestine in 7 patients.
in Table 1. Immunosuppression included patients re- In 3 patients, small-bowel fistulae were present that could
ceiving steroids (n = 20) and/or antirejection medica- have been treated with resection.
tions following organ transplantation (n = 4) or infec-
tion with human immunodeficiency virus (n = 1). The MORTALITY
majority of patients (52%) were referred from an out-
side institution. Of 135 patients, 114 ultimately survived with a closed
fistula (84%), 10 survived with a recurrent fistula (8%),
PREOPERATIVE MANAGEMENT and 11 died (8%). All deaths were due to sepsis and mul-
tiorgan failure (7 associated with a recurrent fistula; 2,
Nutrition was maintained parenterally in 69% of pa- with postoperative wound infection and dehiscence; 1,
tients and enterally in 30%, with 5 of the latter group re- with gastric necrosis after embolization for bleeding; and
ceiving parenteral supplementation. Serum albumin level 1, with aspiration pneumonia and adult respiratory dis-
at the time of operation was lower than 3 g/dL (to con- tress syndrome after small-bowel obstruction). The only
vert to grams per liter, multiply by 10) in 64% of pa- significant predictor for mortality in both univariate and
tients. Mean interval between diagnosis of the fistula and multivariate analysis was postoperative recurrence of the
operative repair was 25 weeks (range, 1-208 weeks), as ECF (odds ratio [OR], 6.69; 95% confidence interval [CI],
shown in Table 2. 1.92-23.39; P=.003).
OPERATIVE MANAGEMENT ECF RECURRENCE
Most procedures were elective. Emergency operations Of the 135 patients undergoing definitive operation to
were performed in 14 patients (10%), 7 with intra- repair ECF, 23 developed a recurrence of the fistula (17%).
abdominal abscesses necessitating to the abdominal wall The recurrence rates for various intervals from diagno-
(REPRINTED) ARCH SURG/ VOL 144 (NO. 6), JUNE 2009 WWW.ARCHSURG.COM
501
©2009 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a University of Manitoba User on 06/08/2015
Table 3. Univariate Predictors of Enterocutaneous Fistula Recurrence
No. (%)
P
Predictor Recurrence No Recurrence Odds Ratio Value
Serum albumin level, g/dL
⬍3 14 (16) 72 (84) 0.99 .76
ⱖ3 9 (18) 40 (82) 1.00
Prealbumin level, g/dL, mean (SD) 15.7 (8.8) 16.3 (8.7) .85
Preoperative alimentation
Parenteral 19 (20) 75 (80) 3.21 .21
Enteral 4 (10) 37 (90) 1.00
Comorbid conditions
Inflammatory bowel disease 9 (29) 22 (71) 2.6 .04
Immunosuppression 4 (17) 19 (83) 1.03 .58
Hypertension 8 (36) 14 (64) 3.7 .01
Location of fistulae
Small intestine 21 (23) 69 (77) 6.3 .007
Large intestine 2 (5) 42 (95) 1.00
Interval from diagnosis to operation, wk
⬍36 12 (12) 92 (88) 1.00
ⱖ36 11 (36) 20 (64) 4.21 .002
Type of fistula repair
Stapled anastomosis 9 (35) 17 (65) 4.3 .01
Hand-sewn anastomosis 10 (11) 81 (89) 1.00
Direct repair, oversew 4 (22) 14 (78) 2.3 .24
Mesh used in closure 5 (26) 14 (74) 2.08 .17
Death 7 (64) 4 (36) 6.2 .006
SI conversion factors: To convert serum albumin to grams per liter, multiply by 10; prealbumin to milligrams per liter, multiply by 10.
levels; emergency operation; prior radiation; extensive
Table 4. Multivariate Predictors of Enterocutaneous adhesiolysis; number of prior abdominal operations; pre-
Fistula Recurrence
operative comorbidities; immunosuppression; opera-
Adjusted Odds
tive blood loss; oversew repair; and the use of mesh for
Ratio (95% abdominal closure.
Confidence P Multivariate analysis of ECF recurrence is shown in
Predictor Interval) Value Table 4. Variables included in the model were operative
Type of fistula repair technique, presence of inflammatory bowel disease, inter-
Hand-sewn anastomosis 1 [Reference] val from diagnosis to operation, and location of fistulae. The
Stapled anastomosis 4.1 (1.3-13.2) .02
Direct repair, oversew 3.3 (0.7-15.3) .12
proportion of the variance explained by these variables
Inflammatory bowel disease is greater than 87% as determined by the Hosmer and
No 1 [Reference] Lemeshow goodness-of-fit test, indicating that a high per-
Yes 4.9 (1.5-16.1) .008 centage of the total variability between recurrence and non-
Interval from diagnosis to operation, wk recurrence is explained by this model. The model confirms
⬍36 1 [Reference]
ⱖ36 5.4 (1.8-16.4) .003
location of the fistula in the small intestine, inflammatory
Location of fistulae bowel disease, interval from diagnosis to operation of 36
Large intestine 1 [Reference] weeks or longer, and resection with stapled anastomosis as
Small intestine 9.8 (1.7-57.6) .01 variables independently affecting ECF recurrence.
Since timing of operation was a major predictor of re-
currence, we performed a univariate analysis for pa-
sis to operation are shown in Table 2. Since the recur-
tients who underwent operation within (n=104) or at 36
rence rates were not significantly different for periods less
than 36 weeks, these were combined to allow categori- weeks or longer (n=31) to identify potential covariates.
cal variables for subsequent statistical analysis. Other than recurrence, the only variables that were sta-
As shown by univariate analysis in Table 3, vari- tistically different between the 2 groups were preopera-
ables significantly associated with recurrence included tive TPN dependence, emergency operation, and sex. Nu-
location of the fistula in the small intestine, inflamma- trition was provided enterally in 55% of patients in the
tory bowel disease, interval from diagnosis to operation 36 weeks or longer group, compared with only 26% in
of 36 weeks or longer, hypertension, and resection with the less than 36 weeks group (OR, 2.34; P =.04).
stapled anastomosis. Notable variables that were not sig- We evaluated the reasons for the long delay prior to
nificantly different between patients with and without re- operation in these 31 patients. Prolonged medical man-
currence included dependence on total parenteral nu- agement was used in 20 patients with a low- to moderate-
trition (TPN); serum albumin, prealbumin, and creatinine output fistula in the hope that it would eventually close
(REPRINTED) ARCH SURG/ VOL 144 (NO. 6), JUNE 2009 WWW.ARCHSURG.COM
502
©2009 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a University of Manitoba User on 06/08/2015
spontaneously, and 8 developed recurrence (40%). An
additional 9 patients had a prolonged wait to achieve more 23 ECF recurrence
favorable wound characteristics in large slow-healing
wounds, and 3 developed recurrence (33%). It was not
possible to determine the reason for the prolonged wait
8 No operation 15 Reoperation
in the remaining 2 patients.
We also performed a univariate analysis for patients
with resection and hand-sewn or stapled anastomosis to
7 Chronic fistula 1 Spontaneous 7 Successful 8 Second
identify potential covariates. Recurrence was the only vari- closure closure recurrence
able significantly different between the groups. of ECF
The subsequent course of the patients who devel-
oped postoperative recurrence of the ECF is shown in 4 Lived 1 Lived 5 Lived 6 Lived
the Figure. Of the 23 patients, only 15 underwent a sub-
sequent attempt at fistula closure. Two patients died, 1 3 Died 2 Died 2 Died
in the early postoperative period of acute pulmonary and
renal failure and another of aspiration associated with a
Figure. Schematic showing outcome of patients with recurrent
small-bowel resection 1 year after successful reopera- enterocutaneous fistulae (ECF).
tion. The fistula recurred a second time in 8 patients, and
2 of these patients died, both of complications associ-
ated with the fistula and wound. No attempt was made Massachusetts General Hospital in the era prior to use
to repair the recurrent fistula in 8 patients. The fistula of TPN and concluded that an early operative attack on
closed spontaneously in 1 patient, and 7 were left with a the fistula might avoid the complications associated with
chronic fistula. Three of these 7 patients died, all of sep- malnutrition and fluid and electrolyte problems. Subse-
tic complications of the fistula and wound. In summary, quent series6-8,11,12 showed that the routine use of TPN
of 23 patients with recurrence after index operative re- all but eliminated mortality from these complications and
pair of ECF, only 26% ultimately had a successful out- allowed a delay for potential spontaneous closure of the
come with a closed fistula, while 43% lived with a chronic fistula and, when closure did not occur, for the resolu-
fistula, and 30% died. tion of maximal inflammation13 and for complex wounds
to soften14 prior to attempted repair. Many recent series
report relatively long waiting periods with TPN support
COMMENT
prior to operative attempts. As an example, Hollington
et al9 reported a median preoperative interval of 9 months
Advances in imaging, percutaneous drainage, and wound and fistula recurrence rate of 35% in patients undergo-
care technology have markedly improved the ability to ing definitive repair. We found a similar recurrence rate
identify and control septic foci prior to attempting de- of 36% for patients with operation at 9 months or later
finitive operative closure of ECF.2 Comparing 6 early se- after diagnosis, far higher than our 12% recurrence rate
ries prior to 1989 with 4 later ones (Table 5), mortal- with operation within 9 months of diagnosis.
ity rates fell from 17% to 5%, while recurrence rates were The reason for increased failure of fistula repair after
relatively constant at 18% in the earlier era and 19% in 36 weeks is not obvious but may be related to other co-
the later. Our figures for mortality (8%) and recurrence variates. We found that patients with TPN dependence
(17%) are consistent with earlier reports. or requiring emergency operation were more likely to have
Recurrence of ECF was the only variable signifi- operation within 36 weeks, while patients who under-
cantly associated with mortality in our series, emphasiz- went later operations were more likely to be fed enter-
ing the importance of an effort to define risk factors for ally. Implicating enteral nutrition as a potential cause of
this serious complication. Factors that independently in- recurrence is counterintuitive, as the enteral route should
creased the rate of fistula recurrence included inflam- improve intestinal barrier function and immune compe-
matory bowel disease, location of fistulae in the small in- tence. The most common reason for delay appeared to
testine, interval from diagnosis to operation of 36 weeks be prolonged nonoperative management at another in-
or longer, and intestinal resection with stapled anasto- stitution with the hope that the fistula would eventually
mosis. The first 2 are well-recognized causes of ECF re- close or a reluctance to operate for undetermined rea-
currence, while the latter 2 are new observations from sons. Approximately one-third of the patients had a seem-
the present study. ingly appropriate delay to await better wound charac-
Rates of ECF recurrence following operations at 36 weeks teristics. Given the limitations imposed by a lack of a
or later (36%) after diagnosis were significantly higher than specific protocol and variability introduced from pa-
for operations earlier than 36 weeks (12%). Moreover, af- tients transferred from other institutions, a prospective
ter accounting for all other risk factors, the later group had study with a protocol that specifies timing of operation
a 5-fold increase in risk of ECF recurrence when com- according to specific criteria may be necessary to iden-
pared with the earlier group. This observation suggests that tify factors that increase risk for ECF recurrence when
prolonged preoperative management can increase recur- repair is delayed past 36 weeks.
rence rates after operative repair of ECF. Several studies have cautioned against early operation,
A single published study has addressed this possibil- when a dense peritoneal reaction makes dissection diffi-
ity. Edmunds and colleagues3 reviewed ECF care at the cult and causes bleeding, enterotomies, and a high fistula
(REPRINTED) ARCH SURG/ VOL 144 (NO. 6), JUNE 2009 WWW.ARCHSURG.COM
503
©2009 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a University of Manitoba User on 06/08/2015
Table 5. Operative Repair of Enterocutaneous Fistula: Collected Series
No. (%)
Source Period Definitive Operation Recurrence Death
Edmunds et al,3 1960 1946-1959 67 8 (12) 10 (15)
Soeters et al,7 1979 1960-1970 76 13 (17) 11 (14)
Reber et al,6 1978 1968-1977 108 22 (20) 22 (20)
Aguirre et al,8 1974 1970-1973 38 8 (30) 6 (22)
Soeters et al,7 1979 1970-1975 88 19 (22) 18 (20)
Conter et al,5 1988 1978-1986 46 5 (11) 4 (9)
Hollington et al,9 2004 1992-2002 167 55 (33) 5 (3) a
Lynch et al,4 2004 1994-2001 203 42 (21) 6 (3)
Draus et al,10 2006 1997-2005 77 8 (11) b
Visschers et al,1 2008 1990-2005 107 10 (9) 13 (12)
Current study 1989-2005 135 23 (17) 11 (8)
a These deaths were “fistula related within 30 days of surgery.”
b The number of deaths in patients who were operated on could not be determined in this study.
recurrence rate.5,13 We found no recurrences in the few pa- (P=.12), twice that seen with resection and hand-sewn
tients who underwent operation prior to 2 weeks and only anastomosis. Oversew was performed when highly vas-
1 recurrence (8%) in patients who underwent operation cular phlegmonous adhesions obscured discernible tis-
between 2 and 6 weeks. The recurrence rate increased to sue planes or when operation was performed during the
27% for patients with operation between 6 and 12 weeks, period of maximal inflammation between 2 and 12 weeks.
but this difference was not statistically significant. The over- While our numbers are small and did not reach statisti-
all recurrence rate of 19% in our patients with operation cal significance, we concur with other authors3,4,6 that
between 2 and 12 weeks is much lower than that reported oversew should be avoided as a definitive repair where
by Lynch et al,4 who found that recurrence was 28% with possible and that resection may be feasible if operation
reoperation between 2 and 12 weeks, compared with 15% can be delayed until more favorable wound characteris-
with reoperation after 12 weeks. Patient selection is the likely tics are present. However, oversew remains an alterna-
principal reason for this observation. Patients in our early tive if it is deemed unsafe to attempt the full dissection
group accounted for 11 of the 14 emergency operations, needed for segmental bowel resection and primary
and 41% had more favorable colonic fistulas; there were anastomosis.
only 2 recurrences in the 44 patients with repair of co- In summary, mortality rates following ECF repair have
lonic fistulae in our study. While most authors advocate declined, while recurrence remains common. Recur-
waiting at least 12 weeks prior to definitive operative re- rence was the sole predictor of mortality in our series and
pair of ECF, Visschers and colleagues1 recently reported a was influenced by 4 variables, including inflammatory
success rate of 90% in 107 patients with a median time to bowel disease, location of fistula in the small intestine,
operation of 53 days. They reiterated the importance of stapled anastomosis, and operative delay beyond 36 weeks.
awaiting the desired softness of the wound, a known prin- Our data are the first to our knowledge to suggest that
ciple of ECF management. While we do not advocate early resection with hand-sewn anastomosis and operation
operation, our data do suggest that carefully selected pa- within 36 weeks of diagnosis may improve mortality by
tients may have successful ECF closure within 12 weeks reducing recurrence. Future investigations should fo-
of diagnosis. cus on operative technique and timing for repair of fis-
The second important finding in our study was that re- tulae involving the small intestine.
currence was influenced by the technique of fistula repair.
The majority of patients (87%) had successful resection of Accepted for Publication: April 27, 2008.
the segment(s) of bowel containing the fistulae, followed Correspondence: H. G. Cryer, MD, PhD, Division of
by primary anastomosis. The anastomosis was hand sewn Trauma/Critical Care, Department of Surgery, UCLA,
in 2 layers in 91 of these patients (78%) and stapled in 26 10833 Le Conte Ave, Los Angeles, CA 90095-6904 (hcryer
(22%). The recurrence rate was significantly higher in pa- @mednet.ucla.edu).
tients with stapled anastomosis (35%), compared with hand Author Contributions: Study concept and design: Bren-
sewn (11%). Moreover, multivariate analysis found a 4-fold ner and Cryer. Acquisition of data: Brenner, Clayton, and
increase in recurrence for stapled compared with hand- Cryer. Analysis and interpretation of data: Clayton, Tillou,
sewn anastomosis when all other risk factors were con- Hiatt, and Cryer. Drafting of the manuscript: Brenner, Clay-
trolled. While prior studies have reported the highest suc- ton, Hiatt, and Cryer. Critical revision of the manuscript
cess rate for operative repair of ECF with resection and hand- for important intellectual content: Clayton, Tillou, Hiatt,
sewn end-to-end anastomosis, ours is the first to our and Cryer. Statistical analysis: Clayton and Cryer. Ad-
knowledge that compares results of stapled and hand- ministrative, technical, and material support: Cryer. Study
sewn anastomoses after resection of ECF. supervision: Tillou, Hiatt, and Cryer.
Simple oversew of the fistula was used infrequently Financial Disclosure: None reported.
(13%) but was associated with a recurrence rate of 22% Previous Presentation: This paper was presented at the
(REPRINTED) ARCH SURG/ VOL 144 (NO. 6), JUNE 2009 WWW.ARCHSURG.COM
504
©2009 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a University of Manitoba User on 06/08/2015
Pacific Coast Surgical Association Annual Meeting; Feb- 7. Soeters PB, Ebeid AM, Fischer JE. Review of 404 patients with gastrointestinal
fistulas: impact of parenteral nutrition. Ann Surg. 1979;190(2):189-202.
ruary 16, 2008; San Diego, California.
8. Aguirre A, Fischer JE, Welch CE. The role of surgery and hyperalimentation in
therapy of gastrointestinal-cutaneous fistulae. Ann Surg. 1974;180(4):393-
REFERENCES 401.
9. Hollington P, Mawdsley J, Lim W, Gabe SM, Forbes A, Windsor AJ. An 11-year
1. Visschers RGJ, Olde Damink SWM, Winkens B, Soeters PB, van Gemert W. experience of enterocutaneous fistula. Br J Surg. 2004;91(12):1646-1651.
Treatment strategies in 135 consecutive patients with enterocutaneous fistulas. 10. Draus JM Jr, Huss SA, Harty NJ, Cheadle WG, Larson GM. Enterocutaneous fis-
World J Surg. 2008;32(3):445-453. tula: are treatments improving? Surgery. 2006;140(4):570-576; discussion, 576-
2. Evenson AR, Fischer JE. Current management of enterocutaneous fistula. J Gas- 578.
trointest Surg. 2006;10(3):455-464. 11. Dudrick SJ, Wilmore DW, Vars HM, Rhoads JE. Long-term total parenteral nu-
3. Edmunds LH Jr, Williams GM, Welch CE. External fistulas arising from the gas- trition with growth, development, and positive nitrogen balance. Surgery. 1968;
trointestinal tract. Ann Surg. 1960;152:445-471. 64(1):134-142.
4. Lynch AC, Delaney CP, Senagore AJ, Connor JT, Remzi FH, Fazio VW. Clinical 12. MacFadyen BV Jr, Dudrick SJ, Ruberg RL. Management of gastrointestinal fis-
outcome and factors predictive of recurrence after enterocutaneous fistula surgery. tulas with parenteral hyperalimentation. Surgery. 1973;74(1):100-105.
Ann Surg. 2004;240(5):825-831. 13. Fazio VW, Coutsoftides T, Steiger E. Factors influencing the outcome of treat-
5. Conter RL, Roof L, Roslyn JJ. Delayed reconstructive surgery for complex en- ment of small bowel cutaneous fistula. World J Surg. 1983;7(4):481-488.
terocutaneous fistulae. Am Surg. 1988;54(10):589-593. 14. Alvarez C, McFadden DW, Reber HA. Complicated enterocutaneous fistulas: fail-
6. Reber HA, Roberts C, Way LW, Dunphy JE. Management of external gastroin- ure of Octreotide to improve healing. World J Surg. 2000;24(5):533-537; dis-
testinal fistulas. Ann Surg. 1978;188(4):460-467. cussion, 538.
Call for Papers
Maintenance of Certification
D uring 2009, we are soliciting manuscripts on
maintenance of certification. The editorial board
has selected this topic as our year-long theme. Ac-
cepted manuscripts will be given priority publication.
Please indicate in your cover letter that your manu-
script is to be considered for this theme.
(REPRINTED) ARCH SURG/ VOL 144 (NO. 6), JUNE 2009 WWW.ARCHSURG.COM
505
©2009 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a University of Manitoba User on 06/08/2015
a series of 81 patients older than 65 years and 510 In the end, it might be wise to put forward a more cau-
younger controls that postoperative complications were tious conclusion from this interesting and important study
significantly increased among the elderly (40% vs 28%, by Seybt et al; that is, thyroid surgery in elderly patients
P = .01). The elderly also tend to have more advanced can be safe when preoperative selection is appropriate,
and/or aggressive thyroid cancers, which in part might preparation is meticulous, and the procedures are per-
explain some of the disparity in outcomes observed formed by experienced thyroid surgeons, such as the au-
based on age. thors of this study. More data are needed regarding in-
On a population level, there is published literature dications for thyroidectomy in the elderly and the overall
demonstrating that clinical and economic outcomes for benefits, including long-term survival, quality of life, re-
currence (for those with a diagnosis of thyroid cancer),
patients aged 65 years or older undergoing thyroidec-
and the effects of subsequent need for additional treat-
tomy in the inpatient setting are considerably worse than
ment of their thyroid disease.
for similar, younger patients. Based on a study of 4836
elderly thyroidectomy patients, those aged 80 years or Julie Ann Sosa, MA, MD
older appear to have significantly longer lengths of stay,
higher complication rates, and higher hospital costs than Correspondence: Dr Sosa, Divisions of Endocrine Sur-
gery and Surgical Oncology, Yale University School of
similar patients aged 65 to 79 years.4 In part, this might
Medicine, Room TMP 204, 333 Cedar St, New Haven,
result from the observation that most thyroidectomies
CT 06520 (julie.sosa@yale.edu)
in aging Americans are performed by low-volume sur- Financial Disclosure: None reported.
geons. If anything, this study underestimated the rates
of adverse postoperative events, in that readmission was
REFERENCES
not captured by the data set.
It is known that surgery in the elderly entails an in- 1. Passler C, Avanessian R, Kaczirek K, Prager G, Scheuba C, Niederle B. Thyroid
creased risk of rehospitalization, which is frequent and surgery in the geriatric patient. Arch Surg. 2002;137(11):1243-1248.
costly.5 In a recent study of 1.9 million patients enrolled 2. Bliss R, Patel N, Guinea A, Reeve TS, Delbridge L. Age is no contraindication to
in the Medicare fee-for-service program discharged from thyroid surgery. Age Ageing. 1999;28(4):363-366.
3. Rı́os A, Rodriguez JM, Galindo PJ, Canteras M, Parrilla P. Surgical treatment for
4926 hospitals in 2003-2004, Jencks et al5 showed that multinodular goitres in geriatric patients. Langenbecks Arch Surg. 2005;390(3):
51.5% of those who had been discharged after select sur- 236-242.
gical procedures were rehospitalized or died within the 4. Sosa JA, Mehta PJ, Wang TS, Boudourakis L, Roman SA. A population-based study
of outcomes from thyroidectomy in aging Americans: at what cost? J Am Coll
first year after discharge. Among patients who were re-
Surg. 2008;206(3):1097-1105.
hospitalized within 30 days of surgical discharge, 70.5% 5. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the
were readmitted for a medical condition. Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418-1428.
Correction
Error in Table. In the Original Article titled “Risk Fac-
tors for Recurrence After Repair of Enterocutaneous
Fistula” by Brenner et al, published in the June issue of
the Archives (2009;144[6]:500-505), an error occurred
in Table 2. There were 4 recurrences (27%), not 2 (27%),
at 7 to 12 weeks.
(REPRINTED) ARCH SURG/ VOL 145 (NO. 1), JAN 2010 WWW.ARCHSURG.COM
10
©2010 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a University of Manitoba User on 06/08/2015
You might also like
- Fast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeFrom EverandFast Facts: Complex Perianal Fistulas in Crohn's Disease: A multidisciplinary approach to a clinical challengeNo ratings yet
- Operative Management of Anastomotic Leaks After Colorectal SurgeryDocument6 pagesOperative Management of Anastomotic Leaks After Colorectal SurgeryJorge OsorioNo ratings yet
- Chua 2012Document8 pagesChua 2012Devi DaryaningsihNo ratings yet
- Management of Colorectal Anastomotic Leakage-Differences Between Salvage and Anastomotic TakedownDocument6 pagesManagement of Colorectal Anastomotic Leakage-Differences Between Salvage and Anastomotic TakedownDumitru RadulescuNo ratings yet
- Curative Resection For Esophageal Adenocarcinoma: Analysis of 100 en Bloc EsophagectomiesDocument12 pagesCurative Resection For Esophageal Adenocarcinoma: Analysis of 100 en Bloc EsophagectomiesYacine Tarik AizelNo ratings yet
- Analysis of Long-Term Survivors After Surgical Resection For Pancreatic CancerDocument5 pagesAnalysis of Long-Term Survivors After Surgical Resection For Pancreatic CancermohamedNo ratings yet
- Proof: Gynecologic OncologyDocument2 pagesProof: Gynecologic OncologyCamilaBurgosNo ratings yet
- Systematized Management of Postoperative Enterocutaneous Fistulas. A 14 Years ExperienceDocument5 pagesSystematized Management of Postoperative Enterocutaneous Fistulas. A 14 Years ExperienceYacine Tarik AizelNo ratings yet
- Agaoglu2005 2Document6 pagesAgaoglu2005 2Ngo Quang MinhNo ratings yet
- No Está Claro Dar RT A Lo Bestia Sino Se CuraDocument7 pagesNo Está Claro Dar RT A Lo Bestia Sino Se Curaouf81No ratings yet
- Diffuse Malignant Peritoneal Mesothelioma PDFDocument9 pagesDiffuse Malignant Peritoneal Mesothelioma PDFAndreeaPopescuNo ratings yet
- Etiology of ECF Predicts OutcomeDocument5 pagesEtiology of ECF Predicts OutcomeYacine Tarik AizelNo ratings yet
- CA EsofágicoDocument45 pagesCA EsofágicoValeria ValdezNo ratings yet
- Surgical technique of coccygectomy: review of 28 studiesDocument7 pagesSurgical technique of coccygectomy: review of 28 studiesDiaz RandanilNo ratings yet
- Song 2017Document8 pagesSong 2017Patricia BezneaNo ratings yet
- Long-Term Outcomes of Primary Endoscopic Resection Vs Surgery For T1Document16 pagesLong-Term Outcomes of Primary Endoscopic Resection Vs Surgery For T1ellya zalfaNo ratings yet
- Refraction ManagementDocument8 pagesRefraction ManagementRaissaNo ratings yet
- Abdominoperineal Resection For Squamous Cell Anal Carcinoma: Survival and Risk Factors For RecurrenceDocument8 pagesAbdominoperineal Resection For Squamous Cell Anal Carcinoma: Survival and Risk Factors For RecurrenceWitrisyah PutriNo ratings yet
- Chevallay 2020Document17 pagesChevallay 2020Maria PalNo ratings yet
- J HPB 2016 02 489Document2 pagesJ HPB 2016 02 489hud6427No ratings yet
- 2022 GlS. Mid-term Efficacy of Surgical Treatments for Post-hysterectomy Vaginal Vault Prolapse; A Retrospective StudyDocument11 pages2022 GlS. Mid-term Efficacy of Surgical Treatments for Post-hysterectomy Vaginal Vault Prolapse; A Retrospective StudyJoseTeodomiroQuispeRicciNo ratings yet
- Glandula SalivarDocument8 pagesGlandula SalivarporsanimedNo ratings yet
- Histopathologic Features and Clinical Outcomes in 71 Cases of Bladder DiverticulaDocument6 pagesHistopathologic Features and Clinical Outcomes in 71 Cases of Bladder DiverticulaIrma Suriani DarwisNo ratings yet
- Tabrizi An 2009Document4 pagesTabrizi An 2009Dung Tran HoangNo ratings yet
- Infections After Laparoscopic and Open Cholecystectomy: Ceftriaxone Versus Placebo A Double Blind Randomized Clinical TrialDocument6 pagesInfections After Laparoscopic and Open Cholecystectomy: Ceftriaxone Versus Placebo A Double Blind Randomized Clinical TrialvivianmtNo ratings yet
- Rectal Cancer Partial VaginectomyDocument5 pagesRectal Cancer Partial VaginectomyArham ArsyadNo ratings yet
- Article. Loop Ileostomy Morbidity. Timing of Closure Matters.2006Document7 pagesArticle. Loop Ileostomy Morbidity. Timing of Closure Matters.2006Trí Cương NguyễnNo ratings yet
- MÁS RADIOTERAPIA SI RECAÍDA y Biopsia A Todos. 310 PersonasDocument13 pagesMÁS RADIOTERAPIA SI RECAÍDA y Biopsia A Todos. 310 Personasouf81No ratings yet
- Ojmn20120100002 97302300 2 PDFDocument5 pagesOjmn20120100002 97302300 2 PDFD s.No ratings yet
- Prognostic Value and Adverse Events of Cytoreductive Surgery With Hyperthermic Intraperitoneal Chemotherapy in Primary Advanced and PlatinumDocument14 pagesPrognostic Value and Adverse Events of Cytoreductive Surgery With Hyperthermic Intraperitoneal Chemotherapy in Primary Advanced and PlatinumChris El HadiNo ratings yet
- 203 FullDocument7 pages203 FullDonNo ratings yet
- Whole Ovary TransplantationDocument7 pagesWhole Ovary Transplantationari naNo ratings yet
- Wong 2017Document9 pagesWong 2017Mely GallardoNo ratings yet
- Neoadjuvant Chemoradiotherapy Followed by Surgery VersusDocument15 pagesNeoadjuvant Chemoradiotherapy Followed by Surgery VersusRaul Matute MartinNo ratings yet
- Original ArticleDocument9 pagesOriginal ArticlePatricia BezneaNo ratings yet
- Baek 2017Document10 pagesBaek 2017witaNo ratings yet
- Pi Is 1743919113001738Document5 pagesPi Is 1743919113001738Yacine Tarik AizelNo ratings yet
- Systemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal CancerDocument8 pagesSystemic Therapy For Advanced Appendiceal Adenocarcinoma: An Analysis From The NCCN Oncology Outcomes Database For Colorectal Canceralberto cabelloNo ratings yet
- Simultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDocument8 pagesSimultaneous Versus Delayed Resection For Initially Resectable Synchronous Colorectal Cancer Liver MetastasesDr Shiv ChopraNo ratings yet
- Hemdan 2014Document6 pagesHemdan 2014DavorIvanićNo ratings yet
- Jco 19 00337Document13 pagesJco 19 00337alberto cabelloNo ratings yet
- AppendicitisDocument3 pagesAppendicitisRindayu Julianti NurmanNo ratings yet
- Complications of Pancreatic SurgeryDocument5 pagesComplications of Pancreatic Surgeryhenok seifeNo ratings yet
- Kim 2009Document7 pagesKim 2009stefan ursuNo ratings yet
- Fit and Fecal Calprotectin 2020Document6 pagesFit and Fecal Calprotectin 2020sashadilanNo ratings yet
- Sattar M. Hashim JPMCDocument5 pagesSattar M. Hashim JPMCprastiaNo ratings yet
- cắt bỏ u xơ và thuyên tắc mạchDocument12 pagescắt bỏ u xơ và thuyên tắc mạchTiến Nguyễn VănNo ratings yet
- 2007-03 - Intestinal Autotransplantation For Adenocarcinoma of Pancreas Involving The Mesenteric Root - Our Experience and Literature Review PDFDocument3 pages2007-03 - Intestinal Autotransplantation For Adenocarcinoma of Pancreas Involving The Mesenteric Root - Our Experience and Literature Review PDFNawzad SulayvaniNo ratings yet
- Gine 2Document9 pagesGine 2Cimpean SorinNo ratings yet
- Malignancies of The Colorectum and Anus in Solid Organ RecipientsDocument8 pagesMalignancies of The Colorectum and Anus in Solid Organ RecipientsDaniel Alfonso GamezNo ratings yet
- International Wound Journal - 2016 - Bobkiewicz - Management of Enteroatmospheric Fistula With Negative Pressure WoundDocument10 pagesInternational Wound Journal - 2016 - Bobkiewicz - Management of Enteroatmospheric Fistula With Negative Pressure WoundDiana Carolina RochaNo ratings yet
- A Propensity Score Matched Analysis of Open Versus Minimally Invasive Transthoracic Esophagectomy in The NetherlandsDocument8 pagesA Propensity Score Matched Analysis of Open Versus Minimally Invasive Transthoracic Esophagectomy in The NetherlandsLuca BellaioNo ratings yet
- Acs 06 02 167Document8 pagesAcs 06 02 167MixalisKaplanisNo ratings yet
- Obstetric Anal Sphincter Injury and Anal Incontinence Following Vaginal Birth PDFDocument11 pagesObstetric Anal Sphincter Injury and Anal Incontinence Following Vaginal Birth PDFaldyNo ratings yet
- Esofago Carvical Valmasoni 2018Document9 pagesEsofago Carvical Valmasoni 2018Carlos N. Rojas PuyolNo ratings yet
- Perforacion ColonosDocument5 pagesPerforacion ColonosKeyla barriosNo ratings yet
- Management Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreDocument9 pagesManagement Guidelines For Penetrating Abdominal Trauma: Walter L. Biffl and Ernest E. MooreArsy Mira PertiwiNo ratings yet
- Unukovych 2016Document7 pagesUnukovych 2016jdavies231No ratings yet
- Evaluating Esophagectomy Complications Using International Consensus DefinitionsDocument7 pagesEvaluating Esophagectomy Complications Using International Consensus DefinitionsPaulo RoseroNo ratings yet
- Detection of A Story CCM1 Frameshift Mutation in A Chinese Language Han Loved Ones Using Numerous Cerebral Cavernous MalformationsmqjvuDocument2 pagesDetection of A Story CCM1 Frameshift Mutation in A Chinese Language Han Loved Ones Using Numerous Cerebral Cavernous Malformationsmqjvumapmaple2No ratings yet
- Blunt: To TheDocument9 pagesBlunt: To TheOanaDavidNo ratings yet
- Nutritio 2Document1 pageNutritio 2OanaDavidNo ratings yet
- 2017 Article 135Document7 pages2017 Article 135OanaDavidNo ratings yet
- Childhood Trauma PDFDocument21 pagesChildhood Trauma PDFOanaDavidNo ratings yet
- International Journal of Surgery: Levent Kaptanoglu, Necmi Kurt, Hasan Ediz SikarDocument5 pagesInternational Journal of Surgery: Levent Kaptanoglu, Necmi Kurt, Hasan Ediz SikarOanaDavidNo ratings yet
- Medical Hypotheses: SciencedirectDocument9 pagesMedical Hypotheses: SciencedirectOanaDavidNo ratings yet
- Renal Trauma in The West of Ireland - A Regional ReviewDocument7 pagesRenal Trauma in The West of Ireland - A Regional ReviewOanaDavidNo ratings yet
- 595 2013 Article 515Document6 pages595 2013 Article 515OanaDavidNo ratings yet
- WJG 19 9003 PDFDocument10 pagesWJG 19 9003 PDFTheodore LiwonganNo ratings yet
- Multiple TraumaDocument3 pagesMultiple TraumaOanaDavidNo ratings yet
- Tomita ScoreDocument11 pagesTomita ScoreMukharradhi NanzaNo ratings yet
- Cord Candea+cecDocument122 pagesCord Candea+cecOanaDavidNo ratings yet
- Mal Leo 2014Document10 pagesMal Leo 2014OanaDavidNo ratings yet
- Blunt TraumaDocument14 pagesBlunt TraumaOanaDavidNo ratings yet
- Mcdonnell 1998Document1 pageMcdonnell 1998OanaDavidNo ratings yet
- Martinez 2007Document8 pagesMartinez 2007Yacine Tarik AizelNo ratings yet
- Atlas of Vascular Surgery and Endovascular Therapy - Anatomy and Technique 1E 2014 PDF UnitedVRG 3 PDFDocument795 pagesAtlas of Vascular Surgery and Endovascular Therapy - Anatomy and Technique 1E 2014 PDF UnitedVRG 3 PDFOanaDavid100% (3)
- Knot Tying ManualDocument50 pagesKnot Tying ManualAdriana Vick100% (1)
- Anatomic Exposure in Vascular Surgery, 3E (2013) (PDF) (UnitedVRG)Document605 pagesAnatomic Exposure in Vascular Surgery, 3E (2013) (PDF) (UnitedVRG)Rafael Castillo85% (13)
- Pharmaceutical Issues When Crushing, Opening or Splitting Oral Dosage FormsDocument7 pagesPharmaceutical Issues When Crushing, Opening or Splitting Oral Dosage FormsMohamed OmerNo ratings yet
- Ali, B.H., Al Wabel, N., Blunden, G., 2005Document8 pagesAli, B.H., Al Wabel, N., Blunden, G., 2005Herzan MarjawanNo ratings yet
- Nursing Intervention Plan for Fracture PatientDocument2 pagesNursing Intervention Plan for Fracture PatientAce Dioso TubascoNo ratings yet
- HSRCDocument53 pagesHSRCAbhishek Kumar SharmaNo ratings yet
- Healthmedicinet Com II 2014 JunDocument320 pagesHealthmedicinet Com II 2014 JunHeal ThmedicinetNo ratings yet
- Oral SurgeryDocument40 pagesOral Surgeryshekinah echavezNo ratings yet
- IELTS Listening Practice Test 69Document17 pagesIELTS Listening Practice Test 69Daniel perez100% (3)
- 7 Types of Stretching ExercisesDocument11 pages7 Types of Stretching ExercisesCzarina RimallaNo ratings yet
- CystolithiasisDocument7 pagesCystolithiasisRaul Nocete100% (1)
- ICF and Guidelines - ComPsych v.2022Document5 pagesICF and Guidelines - ComPsych v.2022JAY JOB TabiNo ratings yet
- Landmark Trials Genitourinary CompilationDocument55 pagesLandmark Trials Genitourinary CompilationBhanuNo ratings yet
- Pilot Study of The Effectiveness of Butterfly Technique of SCENAR Therapy On Heart Rate VariabilityDocument7 pagesPilot Study of The Effectiveness of Butterfly Technique of SCENAR Therapy On Heart Rate VariabilityParallaxsterNo ratings yet
- The - Erlangen - Test - of - Activities - of - Daily - Living - in ADocument3 pagesThe - Erlangen - Test - of - Activities - of - Daily - Living - in Akwstas79No ratings yet
- Benefits of CuminDocument14 pagesBenefits of CumindhiraniaNo ratings yet
- Press-Kit iMuco-Gingival Recessions Version 2.0Document13 pagesPress-Kit iMuco-Gingival Recessions Version 2.0carcuacNo ratings yet
- Local Anaesthetic AgentsDocument21 pagesLocal Anaesthetic AgentsSuresh KumarNo ratings yet
- Airway ExamDocument7 pagesAirway ExamCharmaine LingdasNo ratings yet
- Review of Literature on Prevalence Studies of Diabetes and Prediabetes in IndiaDocument39 pagesReview of Literature on Prevalence Studies of Diabetes and Prediabetes in Indiapatan ShabanaNo ratings yet
- NEW Tugas Dr. Ahmad Ridwan, MO, MSC 2Document36 pagesNEW Tugas Dr. Ahmad Ridwan, MO, MSC 2dr.rinanovitriani94No ratings yet
- Homework Week 2Document3 pagesHomework Week 2Niki100% (2)
- Desmopressin Full Prescribing Information, Dosage & Side Effects MIMS - Com IndonesiaDocument2 pagesDesmopressin Full Prescribing Information, Dosage & Side Effects MIMS - Com IndonesiayokiduarsaNo ratings yet
- Accepted Manuscript: Complementary Therapies in MedicineDocument24 pagesAccepted Manuscript: Complementary Therapies in MedicineAndrea BarresiNo ratings yet
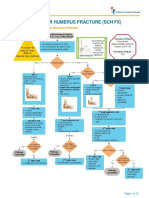
- Fracture Supracondylar HumerusDocument12 pagesFracture Supracondylar HumeruskemsNo ratings yet
- Disinfection by Sodium Hypochlorite. Dialysis Applications (2007)Document168 pagesDisinfection by Sodium Hypochlorite. Dialysis Applications (2007)Popoviciu SimonaNo ratings yet
- Psych - Chapters 11, 12, 13, and 14 Test Study GuideDocument5 pagesPsych - Chapters 11, 12, 13, and 14 Test Study Guidejustinaw1024No ratings yet
- Retrospective Study of Cholangiocarcinomas Diagnosed in The Hospital of Fuenlabrada in The Period 20062016Document3 pagesRetrospective Study of Cholangiocarcinomas Diagnosed in The Hospital of Fuenlabrada in The Period 20062016Riya CassendraNo ratings yet
- SpirulinaDocument57 pagesSpirulinaMarcus Gibson100% (4)
- 2019 Complication After Epilepsy Surgery AChA InfarctDocument7 pages2019 Complication After Epilepsy Surgery AChA InfarctSafitri MuhlisaNo ratings yet
- Drug To Drug InteractionDocument47 pagesDrug To Drug InteractionMannan SokaNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (17)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)