0% found this document useful (0 votes)
958 views7 pagesPediatric Genitourinary Disorders
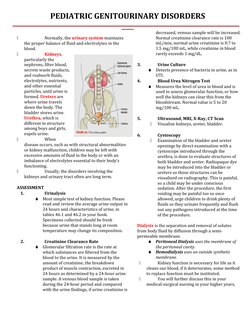
This document discusses pediatric genitourinary disorders. It summarizes common disorders like hypospadias, urinary tract infections, vesicoureteral reflux, and hydronephrosis. It describes diagnostic tests used to assess kidney function like urinalysis and creatinine clearance rate. Surgical procedures are outlined to correct defects like hypospadias. Kidney replacement through dialysis is mentioned if function deteriorates.
Uploaded by
cayla mae carlosCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
958 views7 pagesPediatric Genitourinary Disorders
This document discusses pediatric genitourinary disorders. It summarizes common disorders like hypospadias, urinary tract infections, vesicoureteral reflux, and hydronephrosis. It describes diagnostic tests used to assess kidney function like urinalysis and creatinine clearance rate. Surgical procedures are outlined to correct defects like hypospadias. Kidney replacement through dialysis is mentioned if function deteriorates.
Uploaded by
cayla mae carlosCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as DOCX, PDF, TXT or read online on Scribd