Professional Documents
Culture Documents
Classification:: 2. Split-Thickness Grafts
Classification:: 2. Split-Thickness Grafts
Uploaded by
cayla mae carlosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Classification:: 2. Split-Thickness Grafts
Classification:: 2. Split-Thickness Grafts
Uploaded by
cayla mae carlosCopyright:
Available Formats
Classification:
1. Autographs – tissue is obtained from the
patient’s own skin.
2. Allograph (allogeneic, homograft) – tissue
obtained from a donor of the same species
3. Xenograft (Heterography) – tissue obtained
from another specie
2. Split-thickness grafts - involves removing
the epidermis and dermis. These layers are
taken from the donor site, which is the area
where the healthy skin is located. Split-
thickness skin grafts are usually harvested from
the front or outer thigh, abdomen, buttocks, or
back.
TYPES OF SKIN GRAFTS:
- pinch
- Split-thickness
- Full-thickness
1. Pinch grafts - very small squares of skin are
attached to the area that needs to be covered,
these small pieces of skin will then grow to
3. Full-thickness grafts - involves removing all
cover injured sites.
of the epidermis and dermis from the donor
These will grow even in areas of poor blood
site. These are usually taken from the
supply and resist infection.
abdomen, groin, forearm, or area above the
clavicle
For weight-bearing portions of the body and
friction prone areas such as, feet and joints.
PRE-OP: Recipient and Donor sites must be free of
infection and have a stable blood supply.
Success of a skin graft can be determined within 72
hours of the surgery- NO REJECTION
Contains all of the layers of the
skin including blood vessels
Blood vessels will begin growing from
the recipient area into the transplanted
skin with in 36 hours
A dermatome is a surgical instrument used to
produce thin slices of skin from a donor area, in
order to use them for making skin grafts.
-Dermatomes can be operated either manually or
electrically.
-Electrical dermatomes are better for cutting out
thinner and longer strips of skin with a more
homogeneous thickness.
Free- Hand Knives
-These are manual dermatomes and the term knife or
scalpel is used to describe them Absorbent gauze dressings- to absorb blood or serum
from the wound
-their disadvantages are harvesting of grafts with
irregular edges and grafts with irregular edges and
grafts of variable thickness.
-The operator has to be experienced in their use for
optimal results.
Hand or arm – may be immobilized with a splint
Lower extremity – elevate
Membrane dressing (Opsite) Ambulation permitted - elastic stockings to counter
- Transparent, allows the wound to be observed balance venous pressure
without disturbing the dressing
2. Inspect the dressing daily report unusual drainage or
-Permits the patient to shower without fear of an inflammatory reaction around the wound margin
saturating the dressing from water
3. After 2-3 weeks, apply lanolin cream to moisten the
graft
BOWEL MANAGEMENT SYSTEM
BMS - soft catheter is inserted into the rectum for fecal
management to contain and divert fecal waste.
- Prolonged diarrhea
Donor site care PAIN MANAGEMENT
Keep it clean and dry
After healing, keep the donor site -Most severe forms of acute pain
soft and pliable (lanolin, olive oil) -Pain accompanies care, and treatments such as
6-12 mos. wound cleaning and dressing changes
-Analgesics
Protect donor site and grafted area from -IV use during emergent and acute phases
- exposure to extremes of temperature -Morphine - PCA
- external trauma -Role of anxiety in pain
- sunlight ( at least 6 mos.) -Effect of sleep derivation on pain
-Non pharmacologic measures
Conditions for the graft to survive NUTRITIONAL SUPPORT
ENOUGH BLOOD SUPPLY Burn injuries:
Enteral route is preferred.
-Graft must be in close contact with its bed to avoid Jejunal feedings Goal of nutritional support is to
accumulation of blood or fluid between the graft and promote a state of nitrogen balance and match
recipient site. nutrient utilization.
-Graft must be fixed firmly
OTHER MAJOR CARE ISSUES
-Area must be free of infection
-Pulmonary care
Nursing Intervention -Psychological support of patient and family
1. Keep affected part immobilize as possible -Patient and family education
Face – avoid strenuous activity
-Restoration of function
PHASES OF MANAGEMENT
3. Rehabilitative phase
Overlaps acute phase of care
Extends beyond hospitalization
Rehabilitation is begun as early as possible in the
emergent phase and extend for a long period after the
injury.
GOAL: client can gain independence and achieve
maximal function
REHABILITATION PHASE
Focus is upon
-wound healing
-psychosocial support
-self-image
-lifestyle
-restoring maximal functional abilities so the patient
can have the best quality life, both personally and
socially.
-Reconstructive surgery to improve function and
appearance.
-Vocational counseling and support groups may assist
the patient.
BURN SCAR CONTRACTURES
- refers to the tightening of the skin after a second or
third degree burn.
When skin is burned, the surrounding skin begins to
pull together, resulting in a contracture.
It needs to be treated as soon as possible because the
scar can result in restriction of movement around the
injured area. A hypertrophic scar is a cutaneous condition
characterized by deposits of excessive amounts of
collagen which gives rise to a raised scar, but not to the
degree observed with keloids.
Keloids are a type of raised scar. They occur where the
skin has healed after an injury. They can grow to be
much larger than the original injury that caused the
scar.
Pressure garments are worn after a burn to control
scarring, to help the scar mature, and to improve the
look of the injured skin.
Compression minimizes the development of scars by
interfering with the production of collagen and
helping to realign the collagen fibers
Psychlogical support
-Grief and loss – physical injury, loss of control from
the forced dependency on others, loss of family
members/friends who may have perished in the injury,
loss of homes and possessions (RESIDENTIAL FIRE)
-PTSD –Post traumatic stress disorder
-Promote a healthy body image
Reconstructive surgery
The goals of reconstructive burn surgery are to
improve both the function and
the cosmetic appearance of burn scars.
REHABILITATION
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pediatric Cardiovascular DisordersDocument9 pagesPediatric Cardiovascular Disorderscayla mae carlos0% (1)
- OnlineWOD Open Prep Program 7 Day Trial PDFDocument8 pagesOnlineWOD Open Prep Program 7 Day Trial PDFJomari ServanoNo ratings yet
- NCP Tissue Perfusion For Pre-EclampsiaDocument2 pagesNCP Tissue Perfusion For Pre-Eclampsiaanreilegarde83% (23)
- Gapuz Review CenterDocument3 pagesGapuz Review CenterKyle CasanguanNo ratings yet
- Newborn Disorders - : Small For Gestational Age (Sga) NewbornDocument11 pagesNewborn Disorders - : Small For Gestational Age (Sga) Newborncayla mae carlos100% (1)
- Stages of LabourDocument43 pagesStages of LabourhaisureshNo ratings yet
- Pediatric Genitourinary DisordersDocument7 pagesPediatric Genitourinary Disorderscayla mae carlosNo ratings yet
- Separating MixturesDocument30 pagesSeparating Mixturescayla mae carlosNo ratings yet
- Practice Application of Nursing InformaticsDocument3 pagesPractice Application of Nursing Informaticscayla mae carlos100% (3)
- BKD Project ShareDocument3 pagesBKD Project ShareAbby- Gail14 CabralNo ratings yet
- HACCP Plan For ChikenDocument8 pagesHACCP Plan For ChikenPeter George0% (1)
- The Need of Improving Social Sustainability in Sri Lankan Construction ProjectsDocument28 pagesThe Need of Improving Social Sustainability in Sri Lankan Construction Projectslakshan mahanamaNo ratings yet
- Local Anaesthetic Dosing For Male CircumcisionDocument4 pagesLocal Anaesthetic Dosing For Male CircumcisionAssenav ZednemNo ratings yet
- The WASH Benefits Bangladesh, WASH Benefits Kenya, and SHINE Trials: A Summary of Their FindingsDocument2 pagesThe WASH Benefits Bangladesh, WASH Benefits Kenya, and SHINE Trials: A Summary of Their Findingscayla mae carlosNo ratings yet
- For Learners Handwashing StepsDocument1 pageFor Learners Handwashing Stepscayla mae carlosNo ratings yet
- Arrythmias 2-3Document4 pagesArrythmias 2-3cayla mae carlosNo ratings yet
- Pediatric Respiratory Disorders General InterventionsDocument2 pagesPediatric Respiratory Disorders General Interventionscayla mae carlosNo ratings yet
- Extraordinary Measures Jop 13 346Document1 pageExtraordinary Measures Jop 13 346cayla mae carlosNo ratings yet
- Cop Lec - Unit Iv - Physical Care of OlderDocument3 pagesCop Lec - Unit Iv - Physical Care of Oldercayla mae carlosNo ratings yet
- Problems With Eating and Feeding, Incontinence, Confusion, Evidence of Falls, and Skin BreakdownDocument1 pageProblems With Eating and Feeding, Incontinence, Confusion, Evidence of Falls, and Skin Breakdowncayla mae carlosNo ratings yet
- The COVIDDocument2 pagesThe COVIDcayla mae carlosNo ratings yet
- Lumad's Belief and ValuesDocument1 pageLumad's Belief and Valuescayla mae carlosNo ratings yet
- Made of A-Grade Poured Concrete and Over-Sized Steel Bars, With Thick Hardwood FlooringDocument2 pagesMade of A-Grade Poured Concrete and Over-Sized Steel Bars, With Thick Hardwood Flooringcayla mae carlosNo ratings yet
- Parental ConsentDocument1 pageParental Consentcayla mae carlosNo ratings yet
- Subject Code Subject Title Course Grade Numeric EquivalentDocument2 pagesSubject Code Subject Title Course Grade Numeric Equivalentcayla mae carlosNo ratings yet
- Diseases of The Digestive SystemDocument5 pagesDiseases of The Digestive SystemmeiuuNo ratings yet
- Ig2 Risk Assessment Self Evaluation ChecklistDocument2 pagesIg2 Risk Assessment Self Evaluation ChecklistprinceNo ratings yet
- How To Run An Effective Journal Club A Systematic ReviewDocument14 pagesHow To Run An Effective Journal Club A Systematic Reviewsidra khaliqNo ratings yet
- Hypertensive Cardiovascular Disease Also Known As Hypertensive Heart Disease Occurs Due To The Complication of Hypertension or High Blood PressureDocument3 pagesHypertensive Cardiovascular Disease Also Known As Hypertensive Heart Disease Occurs Due To The Complication of Hypertension or High Blood Pressurejoanneceline16No ratings yet
- The-Effects-of - Social-Media-on-a-TeenagersDocument13 pagesThe-Effects-of - Social-Media-on-a-TeenagersJanella EuniceNo ratings yet
- Rodriguez, B. O., & Sanchez, T. L. (2020) .Document6 pagesRodriguez, B. O., & Sanchez, T. L. (2020) .Yanreza Dwi HermawanNo ratings yet
- Paradise TrialDocument26 pagesParadise TrialMiguel Martinez DuranNo ratings yet
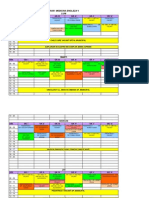
- Orar Medicina Engleza V Luni: ORA Gr. I Gr. Ii Gr. Iii Gr. Iv Gr. V Gr. ViDocument3 pagesOrar Medicina Engleza V Luni: ORA Gr. I Gr. Ii Gr. Iii Gr. Iv Gr. V Gr. ViCornel MihaiNo ratings yet
- Think Global Manila ProgramDocument16 pagesThink Global Manila ProgramRenzo R. GuintoNo ratings yet
- Indonesia Case StudyDocument42 pagesIndonesia Case StudyChad McMillenNo ratings yet
- February 2016 Ophthalmic Pearls PDFDocument3 pagesFebruary 2016 Ophthalmic Pearls PDFIndah IndrianiNo ratings yet
- PneumoniaDocument8 pagesPneumoniaNader Smadi100% (2)
- Cor Jesu College, IncDocument12 pagesCor Jesu College, Incalmira garciaNo ratings yet
- Case Study About Food Safety and SecurityDocument3 pagesCase Study About Food Safety and SecurityALCARAZ ChristineNo ratings yet
- Phoebe Lam ResumeDocument1 pagePhoebe Lam ResumeAnonymous 9gOf6VGNo ratings yet
- Psychiatric Mental Health Comprehensive Case StudyDocument12 pagesPsychiatric Mental Health Comprehensive Case Studyapi-508432180No ratings yet
- Monthly Health CalendarDocument4 pagesMonthly Health CalendarMercicae ANo ratings yet
- Nurse Role in Caring For Women Victim of Ipv Sri Lankan ContextDocument9 pagesNurse Role in Caring For Women Victim of Ipv Sri Lankan Contextkaysa refaNo ratings yet
- Ozdemir Et Al-2015-Journal of Advanced Nursing PDFDocument15 pagesOzdemir Et Al-2015-Journal of Advanced Nursing PDFIMaa Wati AlbiizzahNo ratings yet
- CommunityNCP Ricafort140717Document3 pagesCommunityNCP Ricafort140717Dara Ellaine RicafortNo ratings yet
- From The Desk of Vice President-Elect: Mrugesh VaishnavDocument1 pageFrom The Desk of Vice President-Elect: Mrugesh Vaishnavgion.nandNo ratings yet
- CDC - HIV in Pregnant WomenDocument2 pagesCDC - HIV in Pregnant WomenMyrna Dianita SavitriNo ratings yet
- DocumentDocument4 pagesDocumentCeline RillonNo ratings yet