Professional Documents
Culture Documents
Clinpatho - S03.T02 - Lipids and Dyslipoproteinemia
Clinpatho - S03.T02 - Lipids and Dyslipoproteinemia
Uploaded by
Rea Dominique Cabanilla0 ratings0% found this document useful (0 votes)
29 views6 pagesThis document provides an overview of lipids and dyslipidemia. It discusses the main lipids found in human plasma, including cholesterol, triglycerides, phospholipids, and non-esterified fatty acids. It also describes the four major classes of lipoproteins - chylomicrons, VLDL, LDL, and HDL - focusing on their composition, density, and the apolipoproteins they contain. Specifically, it provides details on the structure and function of chylomicrons, which transport dietary triglycerides from the intestines to other tissues.
Original Description:
Original Title
CLINPATHO_S03.T02_-LIPIDS AND DYSLIPOPROTEINEMIA
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides an overview of lipids and dyslipidemia. It discusses the main lipids found in human plasma, including cholesterol, triglycerides, phospholipids, and non-esterified fatty acids. It also describes the four major classes of lipoproteins - chylomicrons, VLDL, LDL, and HDL - focusing on their composition, density, and the apolipoproteins they contain. Specifically, it provides details on the structure and function of chylomicrons, which transport dietary triglycerides from the intestines to other tissues.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
29 views6 pagesClinpatho - S03.T02 - Lipids and Dyslipoproteinemia
Clinpatho - S03.T02 - Lipids and Dyslipoproteinemia
Uploaded by
Rea Dominique CabanillaThis document provides an overview of lipids and dyslipidemia. It discusses the main lipids found in human plasma, including cholesterol, triglycerides, phospholipids, and non-esterified fatty acids. It also describes the four major classes of lipoproteins - chylomicrons, VLDL, LDL, and HDL - focusing on their composition, density, and the apolipoproteins they contain. Specifically, it provides details on the structure and function of chylomicrons, which transport dietary triglycerides from the intestines to other tissues.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
LIPIDS AND DYSLIPOPROTEINEMIA
CLIN.PATHOLOGY (3rd Shifting) | (Aira Liza F. De Chavez, MD, FPSP) | (January 15, 2021)
LEGENDS • Constitute about 25% of LDL mass (lecithin: sphingomyelin ratio =
Important 2:1)
Book Powerpoint Sabi ni Clinical • Constitute about 30% of HDL mass (lecithin: sphingomyelin ratio =
for Exam
Knowledge Information Doc Importance 5:1)
(OT)
❒ ⌨ ♪ ★ ☤ NEFA (Non-Esterified Fatty Acid)
• Very important source of energy
OUTLINE • Constitute a very small fraction of total plasma lipids
I. Lipids V. Blood Sampling Storage • Transported in plasma complexed with albumin
A. Lipoprotein Structure VI. Estimation of Plasma Lipids III. PLASMA LIPOPROTEIN
B. Subheading A. Cholesterol • Four major lipoproteins:
II. Main Lipids In The Human B. Triglycerides 1. Chylomicrons
Plasma VII. NCEP 2. VLDL
III. Plasma Lipoprotein VIII. Major Risk Factors That 3. LDL
A. Lipoprotein Differentiation Modify LDL 4. HDL
B. Chylomicron IX. Testing and treatment • Basis for differentiation: Buoyant density & electrophoretic mobility
C. VLDL X. Drug therapy/hyperlipidemia
drugs A. LIPOPROTEIN DIFFERENTIATION
D. LDL
1. Ultracentrifugation
E. HDL XI. Hypertriglyceridemia
1. separates lipoprotein based on buoyant density
IV. Minor and Abnormal XII. Analysis of apoprotein levels
2. The density of a lipoprotein is determined by its protein &
Lipoprotein
triglyceride (lipid) content.
I. LIPIDS 3. The higher the lipid content, the less dense is the lipoprotein
particle & so upon centrifugation, the closer it migrates to the
• Organic substance insoluble in water but soluble in organic
top of the tube.
substance like chloroform & ether.
4. Chylomicrons (CM) & VLDL have higher triglyceride (TG) and
• Cholesterol & triglycerides are transported in plasma & ECF as part
less protein content.
of water-soluble complexes called LIPOPROTEINS.
5. HDL has high protein content & low TG content
A. LIPOPROTEIN STRUCTURE 6. LDL & IDL are denser than VLDL but less dense than HDL
• Contains cholesterol in 2 forms: 2. Electrophoresis
1. 30% free cholesterol - a polar non-esterified alcohol 1. uses agarose gel as support medium because of its speed,
2. 70% cholesterol ester – a hydrophobic form wherein sensitivity and ability to resolve the lipoprotein classes
cholesterol is linked to a fatty acid. 2. Lipoprotein are named according to their mobilities.
• It is a spherical structure arranged like a micelle. 3. CM – remain at the origin
a. Core – composed of the more hydrophobic lipids such as 4. HDL (a-lipoprotein) - migrates the fastest & moves with alpha
cholesterol esters and triglycerides. a1-globulin
5. LDL (B-lipoprotein)- migrates with the beta (B) globulins
b. Surface – is composed of the more hydrophilic lipids such as
6. VLDL (pre-B lipoprotein) migrates with the B2 globulins
free cholesterol & phospholipids arranged pointing outwards.
• Apolipoproteins are also located on the surface. Lipoproteins can also be classified based on the presence or
• Amphiphilic characteristic: absence of apo-B.
1. Hydrophobic residues interact with the hydrophobic core 1. Apo-B containing: CM, VLDL, IDL, LDL
2. Hydrophilic residues interact with the hydrophilic surface. 2. Non apo-B-containing: HDL
• Importance of apo-B:
II. MAIN LIPIDS IN THE HUMAN PLASMA 1. Only 1 apo-B molecule is present per lipoprotein and this is a
A. Cholesterol nonexchangeable apoprotein.
B. Cholesteryl esters 2. Apo-B containing lipoproteins may or may not contain additional
C. Triglycerides apoproteins such as apo-A, apo-C & apo-E. Apo-B serves as a
D. Phospholipids structural protein for these and is always associated with these
E. NEFA - non-esterified fatty acids particles.
• Apo-B are synthesized by hepatocytes and enterocytes.
Cholesterol
• An unsaturated steroid alcohol B. CHYLOMICRON
• Important component of cell membranes • Produced by the intestines
• Precursor for the synthesis of bile acids & steroid hormones • Contain 85-95% triglycerides from exogenous source (dietary)
• 60-70% transported in plasma by LDL • Poor in free cholesterol, phospholipids & proteins
• 20-35% transported in plasma by HDL • Contain 1-2 % proteins
• 5-12% transported in plasma by VLDL • Very high lipid (TG) content - less dense in water (floats without
centrifugation)
Triglycerides
• High chylomicron content in plasma results to “milky” appearance
• Long chain fatty acid esters of glycerol
upon standing (floating “cream” layer) → (standing plasma test)
• Constitute about 95% of adipose tissues
• Contains apolipoproteins: apo-B48 (intestinal origin), apo C-1, apo
• Main form of lipid storage in man
C-II, apo C-III, apo A-1, apo A-IV and apo-E
• Transported in plasma in the form of chylomicrons & VLDL
• When acted upon by lipoprotein lipase → reduced to small particles
• Present in small amounts in LDL & HDL
with less triglycerides and some surface elements → ”chylomicron
• Constitute 95% of adipose tissue by weight
remnants”
Phospholipids • Chylomicron remnants are removed from the circulation by the
• Esters of glycerol that contain 2 fatty acyl group & phosphatidic liver through the interaction of apo-E with receptors such as
acid proteoglycans, LDL receptor, and the LDL receptor-related protein
• Main plasma phospholipids are sphingomyelin, lecithin, cephalins (LRP).
C. VLDL (Very Low Density Lipoprotein)
S 03 // T 02 MED2023 – Cabanilla, Rea 1 of 6
• Particles smaller than chylomicrons 3. Electrophoretic activity is usually pre-B
• Rich in triglycerides (but lower than chylomicrons) 4. Increased levels are related to genetic disorder (autosomal
• Has lower lipid to protein ratio dominant inheritance) & associated with increased risk of CHD.
• When excessive amounts are present in the plasma, it can cause 5. Atherogenic properties are not yet well understood. Lp(a) might
“turbidity” interfere with normal thrombolysis by virtue of its similarity to
• VLDL are produced by the liver plasminogen.
• Supply the tissues of the body with endogenous TG (from hepatic 2. LpX lipoprotein
origin) and cholesterol 1. Seen in patients with obstructive biliary disease and those with
• This contains apo B-100, apo C-I, apo C-II, apo C-III & apo E. LCAT (lecithin/cholesterol acytransferase) deficiency
• Lipoprotein lipase (LPL) hydrolyzes VLDL and this produces VLDL 2. 90% of its weight is lipids (phospholipids, unesterified &
remnants (highly atherogenic particle) & IDL. esterified cholesterol)
3. Apo C & albumin constitute less than 10% of its weight.
D. LDL (Low Density Lipoprotein)
3. B-VLDL (Floating B Lipoprotein)
• Constitute about 50% of total lipoprotein mass in human plasma
1. An abnormal lipoprotein that accumulates in type 3
• Produced through the metabolism of VLDL in circulation
hyperlipoproteinemia
• Particles are smaller than VLDL & CM
2. Richer in cholesterol than VLDL & apparently results from
• Does not scatter light or alter the clarity of plasma even at greatly
defective catabolism of VLDL.
increased concentration
3. Found in the VLDL density range but migrates
• Consists approx. 50% C, mostly esterified, 25% protein, mostly apo
electrophoretically with or near LDL.
B-100 with traces of apo C, 20% P & some TG
• The apo B is the largest component of protein in this particle and
this serves as the ligand for the hepatic LDL receptor.
E. HDL (High Density Lipoprotein)
• Its major apoprotein is apo A1
1. Apo A1 comprises 70% of HDL protein
• This is formed in the liver
• A small particle made up of:
a. 50% protein – Apo A-I, Apo A-II, Apo E
b. 20% esterified cholesterol
c. 30 % phospholipids
d. traces of triglycerides
• Produced by the liver & intestine
• Protective mechanism against atherosclerosis by:
1. Involved in reverse cholesterol transport wherein excess
cholesterol in the tissues are transported back to the liver,
where it is re-used or excreted in bile.
▪ Mechanism is by selective uptake of cholesterol esters from
HDL by the SR-B1 receptor in the liver.
▪ SR-B1 promotes cholesterol uptake without apolipoprotein ♪NOTE! Read the chapter on Lipids & Dyslipoproteinemia.
degradation. Pay particular attention to all the Tables presented in this chapter.
▪ Cholesterol esters are removed from the internalized HDL V. BLOOD SAMPLING & STORAGE
particles and cholesterol- depleted HDL are re-secreted. A. Fasting
▪ Mouse models that lack SR-B1 show increased plasma HDL, 1. 10-12 hours (because chylomicrons are cleared within 9 hours of
slower HDL uptake by the liver and increased atherosclerosis fasting)
and reverse cholesterol transport is reduced. 2. Presence of chylomicrons after 12 hours of fasting is abnormal
▪ Mouse models with overproduction of SR-B1 show opposite 3. Chylomicrons can markedly increase triglyceride concentration
of the above findings. 4. Fasting has little effect on plasma total cholesterol level & HDL-
▪ * SR-B1- scavenger receptor class B member 1 C.
2. HDL also possess anti-inflammatory, antioxidant, antithrombotic B. Position upon blood extraction:
and nitric oxide-inducing mechanisms believed to add to its 1. Standing patient who reclines- about 10% decrease in the value of
protective effect. total cholesterol, LDL, HDL, apo-B, Apo A-I after 20 mins of
▪ Such protection may come from HDL function rather than recumbence (due to transfer of extravascular water to the
from its increased plasma levels. vascular system- dilution effect); for TG, the decreased is 50%
• Has 2 subclasses: HDL 2 & HDL 3 greater.
1. HDL 2 is more cardioprotective than HDL 3 2. Standing to sitting position- wait for 5 minutes before extracting.
• Sub-fractionation of HDL into: • Therefore: patient position should be standardized.
1. Particles that contain Apo A-I but not Apo A-II • Prolonged venous occlusion can lead to hemoconcentration which
2. Particles that contain both Apo A-I & Apo A-II can cause 10-15% increase in cholesterol.
• Significance: • Therefore, tourniquets should not be applied longer than a minute
1. Apo A-I is present in all HDL particles and makes up 70% of the or two.
protein content 3. Sample to be used – either serum or plasma
2. Apo A-II is present on about 2/3 of HDL particles in humans. It 4. If plasma is to be used, EDTA anticoagulant is the best
makes up 20% of the HDL lipoprotein. 5. Blood samples could be frozen ( -70 degrees centigrade)
3. Apo A –II plays an important role in maintaining levels of HDL in
plasma. VI. ESTIMATION OF PLASMA LIPIDS
4. Apo A-I & II are required for normal HDL biosynthesis & A. CHOLESTEROL
metabolism. 1. Colorimetric – not very accurate because of interfering substances
• A high percentage of HDL2 particles falls into the Apo A-I only like increased bilirubin, high hemoglobin, very high triglycerides
category. 2. Enzymatic – commonly used because it can give more precise
IV. MINOR AND ABNORMAL LIPOPROTEIN results; easier to use and can be done rapidly
1. Lipoprotein (a) – Lp(a) B. TRIGLYCERIDES
1. Similar to LDL in density and overall composition 1. Chemical method
2. It is believed to be an LDL particle to which an apo(a) is added, 2. Enzymatic method
linked to apo B-100 by disulfide bond 1. more specific, rapid & easy to use
PATHO Lipids and Dyslipoproteinemia 2 of 6
2. not affected by interfering substances like phospholipids &
glucose
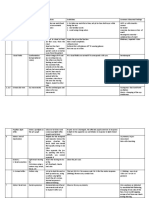
VII. NCEP (NATIONAL CHOLESTEROL EDUCATION PROGRAM
INTERPRETATION (NCEP- national cholesterol education program
& ATP III - adult treatment plan III) (mg/dl)
Total Cholesterol <200 – desirable
200-239 – borderline high
>240 - high
Triglycerides <150 – normal
150-199 – borderline high
VIII. MAJOR RISK FACTORS THAT MODIFY LDL GOALS
200-499 – high
1. Cigarette smoking
>500 – very high
2. Hypertension (BP >/= 140/90 or on antihypertensive meds)
LDL-C <100 – optimal 3. Low HDL–C (<40mg/dl)
100-129 – near optimal /above optimal 4. Family history of premature CHD
130-159 – borderline high a. CHD in a male 1st degree relative <55
160-189 – high b. CHD in a female 1st degree relative <65
>190 – very high 5. Age
HDL-C <40 – low a. Men = >/= 45 yrs old
>60 - high b. Women = >/= 55 years old
INTERPRETATION 6. Diabetes mellitus
Borderline high LDL cholesterol – 130-159 mg/dl 7. Pre-existing CHD
Total cholesterol – 150-199 mg/dl
Borderline high risk Total cholesterol = 5.195 – 6.202 mmol/L
(risk is 2x greater) or 200 – 239 mg/dl
LDL cholesterol = 3.377 – 4.130 mmol/L or
130 – 159 mg/dl
High risk Total cholesterol = greater or equal to
(risk is 3x-4x 6.234 mmol/L or 240 mg/dl
greater)
LDL cholesterol = greater or equal to
4.156 mmol/L or 160 mg/dl
A. HDL
• A very strong independent correlate of CHD
CUTPOINTS FOR PLASMA CHOLESTEROL (NCEP)
• Low levels of HDL (< 40 mg/dl) may be associated with increased
• Detection, evaluation & treatment of high blood cholesterol in
cardiovascular heart disease even if the cholesterol & LDL levels
Adults:
are within normal limits.
1. Total cholesterol level is the basis for initial patient
• Increased HDL may be solely responsible for the increased
classification
hypercholesterolemia in 5% of adults and in 20% of children and not
2. All blood cholesterol levels above 5.195 mmol/L (200 mg/dl)
connote cardiovascular disease risk.
should be confirmed by repeat measurements and the average
• Some factors which may be associated with low levels of HDL:
value is used to guide clinical decisions
1. Male gender
3. With borderline high cholesterol levels, consider other risk
2. Progesterone
factors for coronary heart disease in selecting follow-up
3. Obesity
measures.
4. Increased carbohydrate intake
4. All patients with levels 6.234 mmol/L (240 mg/dl) or above, do
5. Sedentary lifestyle
lipoprotein analysis.
6. DM type 2
5. Individuals in whom lipoprotein analysis are performed are
7. Hypertriglyceridemia
subsequently treated according to their LDL-Cholesterol levels.
8. Cigarette smoking
♪NOTE! LDL-cholesterol level is the basis for decision about • Some factors which are associated with high levels of HDL:
initiating dietary or drug therapy: 1. Female gender
• Patients with LDL-cholesterol levels of 4.156 mmol/L (160 mg/dl) 2. Estrogens
or greater are considered as high risks for CHD. They should be 3. Exercise
given cholesterol-lowering treatment. 4. Moderate intake of alcohol
• Patients with LDL-cholesterol levels of 3.377 to 4.130 mmol/L 5. Intake of nicotinic acid
(130 mg/dl-159 mg/dl) should also be treated to lower their • LDL & HDL are independent risk factors
cholesterol if they have definite CHD or two other CHD risk • The less cholesterol carried in LDL and the more in HDL, the lower
factors is the risk of cardiovascular disease.
• There is an inverse relationship between HDL & TG, such that
elevated TG tend to be associated with decreased HDL levels.
• Elevated TG is an independent risk factor for CHD.
• The protective effect of high HDL level is mediated primarily by the
HDL2 component.
• Exercise and moderate alcohol consumption can increase HDL2
levels.
B. LDL
PATHO Lipids and Dyslipoproteinemia 3 of 6
• Serum cholesterol is composed mainly of LDL f. Some diseases – DM type 2, CRF, nephritic syndrome
• LDL is difficult to measure, so cholesterol is used as a substitute for g. Some drugs- corticosteroids, estrogens, retinoids, higher doses
the initial screening for lipid disorders of B-adrenergic blocking agents
• LDL cholesterol is estimated using the Friedewald formula: h. genetic diseases- familial combined hyperlipidemia, familial
hypertriglyceridemia, familial dysbetalipoproteinemia
Computations:
• Primary aim of therapy – achieve target level for LDL-C.
• LDL cholesterol = total cholesterol – HDL - TG/5)
1. Higher levels of LDL- weight reduction, exercise, medications
1. used when values are in mg/dl
(nicotinic or fibrate)
• LDL cholesterol = total cholesterol – HDL - TG /2.2)
2. Borderline high levels- weight reduction, exercise
1. used when the values are in mmol/L
• TG/5 or TG/2.2 = VLDL cholesterol A. NEW CONCEPTS FOR EVALUATION OF HYPERLIPIDEMIA
• Cannot be used when the TG value is 10.39 mmol/L or 400 mg/dl • Diabetes mellitus is now considered a risk equivalent because it
or higher confers a high risk of new CHD within 10 years.
1. It means that DM patients with elevated cholesterol are treated
IX. TESTING AND TREATMENT like patients who already have CHD.
• Cholesterol goals: • Metabolic syndrome
1. ATP III recommends a complete lipoprotein profile (TC, LDL, HDL 1. a physiologic syndrome, with risk factors like:
& TG) as initial test for evaluating blood cholesterol. a. abdominal obesity
2. Testing should be done in all adults 20 years & older and should b. atherogenic dyslipidemia (increased TG, LDL & decreased
be repeated at least once every 5 years. HDL)
▪ If nonfasting state – TG & HDL only c. increased BP
▪ If TC is 200 mg/dl or HDL is <40 mg/dl, perform follow-up lipid d. Insulin resistance (with or without glucose intolerance
profile e. Prothrombotic states
3. LDL is used as the primary target for cholesterol–lowering f. Pro-inflammatory states
therapy *** LDL is the main target of therapy.
▪ TLC – therapeutic lifestyle change (1st line of therapy) ***Treatment of underlying causes like obesity and other risk factors.
a. Dietary change DISEASE STATES
b. Physical activity A. Single Gene Disorder:
c. Regular follow-up
1. Familial hypercholesterolemia
▪ Drug therapy
▪ decreased activity of LDL receptors → Increased LDL
X. DRUG THERAPY/HYPERLIPIDEMIA DRUGS cholesterol in the plasma
1. Statins: ▪ Autosomal dominant
2. primary effect – lower LDL-C (20-60%) ▪ Premature coronary atherosclerosis, xanthomas in skin &
3. Secondary effect – small decreases in elevated TG & modest tendons, arcus cornea
increases in HDL ▪ (Type II hyperlipoproteinemia)
4. MOA: inhibit HMG-COA reductase
2. Familial Hypertriglyceridemia
5. Side effects- GI disturbance (rare); liver problems;
▪ Increased VLDL in the blood accompanied by the triad of
rhabdomyolysis
obesity, hyperglycemia, & hyperinsulinemia (glucose
6. Ex. Lovastatin, Simvastatin, Pravastatin, Atrovastatin
intolerance)
2. Fibric acid derivatives (TG-lowering drug) ▪ Xanthomas are not characteristic of this disease
1. primary effect – lower TG (20-50%) ▪ Autosomal dominant
2. Secondary effect- small increases in HDL (10- 15%) ▪ (Type IV hyperlipoproteinemia)
3. MOA: not clearly defined; may decrease catabolism of HDL; ▪ There’s a block in the conversion of VLDL to IDL and LDL .
increase the activity of LPL; inhibit hepatic synthesis of VLDL
3. Familial dyslipoproteinemia or broad beta disease
4. Side effects – GI disturbances, increased incidence of cholesterol
▪ A rare disorder
gallstones, increased effects of warfarin, tendency of statins to
▪ Elevated both triglycerides & cholesterol
cause rhabdomyolysis
▪ Electrophoresis show “floating B” lipoprotein
5. Ex. Gemfibrozil, Fenofibrate
▪ Impaired uptake & metabolism of VLDL in the liver
3. Bile acid resins ▪ (Type III hyperlipoproteinemia)
1. Primary effect- lower LDL (10-20%)
4. Multiple-lipoprotein-type hyperlipidemia or familial combined
2. Secondary effect- bind bile acids in intestine leading to
hyperlipidemia
secretion
▪ Autosomal dominant
3. MOA: cholestyramine (bile acid sequestrant)
▪ Increase triglycerides & or cholesterol
4. Side effects – GI disturbance
▪ Increased hepatic secretion of VLDL
5. Ex. Colestipol, Colesevelam
▪ Premature atherosclerosis but no xanthomas
4. Niacin /Nicotinic acid (TG-lowering drug)
B. MULTIFACTORIAL DISORDERS:
1. Primary effect – lowers TG (20-50%)
1. Polygenic hypercholesterolemia
2. Secondary effect – raises HDL (15-35%)
▪ Elevated LDL cholesterol in the blood
3. MOA:
▪ The cholesterol levels are sensitive to different
1. Decreased VLDL production in the liver by inhibition of
environmental factors like drugs, diet, alcohol intake, obesity
mobilization of FA in adipocytes via C-protein-coupled
& concurrent disease/s.
receptor HM74A
2. Sporadic hypertriglyceridemia
2. reduce LDL (10-20%)
▪ Elevated levels of endogenous triglycerides with or without
1. Side effects- GI disturbance, flushing, chills, pruritus, gout,
elevated levels of chylomicrons
elevated blood sugar
XI. HYPERTRIGLYCERIDEMIA
• ATP III identifies elevated TG as an independent risk factor for CHD
• Factors associated with high TG
a. Obesity
b. Physical inactivity
c. Cigarette smoking
d. Excess alcohol intake
e. High carbohydrate diet (>60% of energy intake)
PATHO Lipids and Dyslipoproteinemia 4 of 6
▪ Etiology is not genetics but as a result of outside factors ▪ Hepatic lipase deficiency
▪ Cholesterol 7-alpha-hydroxylase deficiency
• Low Total C & TG
→ uncommon disorder
→ due to defective apo B synthesis or metabolism leading to low
or non-existent apo B lipoproteins (CM, VLDL, &LDL)
→ Fat soluble vitamin deficiencies are common
→ Therapy: low fat or diet therapy are required
a. Abetalipoproteinemia
b. Hypobetalipoproteinemia (Bazen-Kornzweig syndrome)
c. Chylomicron retention disease – Anderson’s disease
• Isolated low HDL
→ associated with CHD
a. Familial hypoalphalipoproteinemia
b. apoA-1 def & apo C-III def
c. apoA-1 variants
d. Tangier disease- rare autosomal recessive disorder;
complete absence of HDL
e. LCAT def.
B. SECONDARY HYPERLIPOPROTEINEMIAS • Isolated High HDL
• Third trimester of pregnancy or those taking contraceptives a. Cholesteryl ester transfer protein defects
→ Elevated levels of VLDL XII. ANALYSIS OF APOPROTEIN LEVELS
→ Due to an estrogen-induced increase in hepatic secretion of • Not routinely done in clinical setting
VLDL • Strong predictors of Coronary heart disease:
• Patients taking thiazide diuretics – hyperlipidemia 1. Low Apoprotein A1 (a major component of HDL)
• Nephrotic syndrome 2. High Apoprotein B
→ elevated TG & cholesterol 3. Apoprotein A1 to Apoprotein B ratio
→ Due to a defect in the clearance of VLDL & LDL from the
peripheral tissues ★ KEYPOINTS:
→ Or due to an overproduction of lipoproteins in the liver in 1. TG & Cholesterol, the major lipids of the blood, are
response to hypoalbuminemia transported in lipoproteins.
• Cushing’s syndrome ▪ VLDL & LDL are primarily responsible for the delivery of
→ associated with increased levels of TG and cholesterol TG and cholesterol, respectively to peripheral tissues.
→ Due to increased hepatic secretions of VLDL → LDL ▪ HDL is involved in the return transport of cholesterol to
• Extrahepatic biliary obstruction & Primary biliary cirrhosis the liver for reuse/secretion to bile.
→ increased cholesterol levels 2. Hyperlipidemia may result from primary & secondary
→ Due to impairment in the biliary excretion & the enterohepatic disorders of lipoproteins.
circulation of cholesterol ▪ Primary hyperlipoproteinemias may reflect single gene
• Hypothyroidism defects or multifactorial disorders.
→ associated with increased levels of cholesterol ▪ Secondary hyperlipoproteinemias are associated with a
→ Due to decreased metabolism of LDL wide variety of conditions.
DISORDERS 3. Evaluation of a suspected lipid disorder is based on
• High C with high LDL: measurements of total cholesterol and TG in blood.
→ Polygenic (nonfamilial) hypercholesterolemia ▪ HDL can also be easily measured.
→ Familial hypercholesterolemia ▪ The amount of LDL cholesterol is then estimated by the
→ Familial defective apo-B Friedewald formula.
→ Sitosterolemia 4. In general, the more cholesterol is carried in LDL and the
▪ plant sterols (phytosterols/are absorbed & accumulated in less carried in HDL the greater the risk of cardiovascular
plasma & peripheral tissues) disease; conversely, the less cholesterol carried in LDL and
→ Autosomal dominant & autosomal recessive the more carried in HDL, the lower the risk.
hypercholesterolemia
5. The National Cholesterol Education Program (NCEP)
• High TG with normal C recommends screening for risk of cardiovascular disease
→ related to elevations of TG-rich particles (CM or VLDL) using total serum cholesterol; decisions regarding therapy
→ due to hyperbetalipoproteinemia (VLDL) and may be due to should be made on the basis of calculated LDL cholesterol
secondary causes like excess alcohol intake or high levels.
carbohydrate diet. ▪ The NCEP’s categories for total cholesterol are: desirable,
→ Fredrickson types 1 & 4 borderline-high, and high.
a. Diabetic dyslipidemia
b. Familial hypertriglyceridemia ★ SUMMARY:
c. Lipoprotein lipase deficiency (hyperlipoproteinemia type I or • All lipoproteins contain TG, cholesterol, phospholipids and
hyperchylomicronemia) proteins in proportions characteristic for each type.
d. Apo C-II deficiency – activating co-factor for LPL • It also contains apoproteins or apolipoproteins which bind
e. Apo C-III excess – interferes with action of LPL selectively to different cell receptors thus initiating cellular
f. Apo A-V deficiency metabolism
• High C with High TG • Lipoproteins are separated by:
→ associated with increased cardiac risk; most common primary 1. Ultracentrifugation – HDL, LDL, VLDL, Chylomicrons
hyperlipoproteinemia 2. Electrophoresis – alpha, beta, pre-beta, chylomicrons (do not
→ Fredrickson types 2B & 3 migrate)
▪ Familial combined hyperlipidemia (type 2B) • VLDL is responsible for the delivery of TG to the peripheral
▪ Acquired combined hyperlipidemia tissues
▪ Dysbetalipoproteinemia (type 3)
PATHO Lipids and Dyslipoproteinemia 5 of 6
• LDL is responsible for the delivery of cholesterol to peripheral
tissues
• HDL is involved in the return transport of cholesterol to the liver
for excretion (good cholesterol)
• HYPERLIPIDEMIA – increase in blood lipids. i.e TG or Cholesterol
or Both.
• HYPERLIPOPROTEINEMIA – increase in one or more lipoproteins
& is almost always accompanied by hyperlipidemia.
• Although ultracentrifugation and electrophoresis are of
historical significance, most useful lipid & lipoprotein testing
methods are now enzymatic.
• LDL can be measured directly but it is usually calculated using
Friedewald formula. Calculated values require evaluation of
fasting samples.
• LDL is currently considered the MOST important value in
assessing cardiac risk & directing therapy.
• The profile currently recommended for initial screening in adults,
age 20 or older includes TC, LDL, HDL & TG. Testing should be
repeated at least once every 5 years.
• Other tests including apolipoprotein level and lipoprotein
subclasses, may prove valuable in fine-tuning risk assessment
& evaluating response to therapy.
• New guidelines elevate the perceived atherosclerotic risk of DM
& support aggressive intervention in diabetic patients and
patients with metabolic syndrome.
V. REFERENCES
• Dr. De Chavez’s PPT
EFERENCES
PATHO Lipids and Dyslipoproteinemia 6 of 6
You might also like
- Let Previous Actual Test Gen Ed Prof Ed Elementary Secondary PDFDocument197 pagesLet Previous Actual Test Gen Ed Prof Ed Elementary Secondary PDFchat50% (8)
- Warrior Shredding ProgramDocument2 pagesWarrior Shredding ProgramStefan Vladut0% (1)
- Airway ManagementDocument48 pagesAirway ManagementRea Dominique CabanillaNo ratings yet
- Challenger Space Shuttle Disaster Case StudyDocument16 pagesChallenger Space Shuttle Disaster Case Studyتاجر الذهب100% (1)
- Book & Media Reviews: Polymer Chemistry: An Introduction, 3rd EditionDocument1 pageBook & Media Reviews: Polymer Chemistry: An Introduction, 3rd EditionAbdul QodirNo ratings yet
- In America by Keri Day. Orbis Books: Maryknoll, NY, 2012.: SummaryDocument2 pagesIn America by Keri Day. Orbis Books: Maryknoll, NY, 2012.: SummaryRod100% (1)
- Chip Leadsinger 1979 SongsDocument40 pagesChip Leadsinger 1979 SongskmsguetioNo ratings yet
- Lecture Topic 8: Lipids and Lipoproteins: SAN PEDRO COLLEGE - Created By: JC Louise P. BandalaDocument6 pagesLecture Topic 8: Lipids and Lipoproteins: SAN PEDRO COLLEGE - Created By: JC Louise P. BandalaMay Ann EnoserioNo ratings yet
- (NF) (MT6317) Introduction and Generalities of LipidsDocument14 pages(NF) (MT6317) Introduction and Generalities of LipidsJC DomingoNo ratings yet
- Clinical Chem 1 - FinalsDocument21 pagesClinical Chem 1 - FinalsJullienne ZyraNo ratings yet
- Metabolisme Lipoprotein Modul 2.2Document72 pagesMetabolisme Lipoprotein Modul 2.2Rizky AkbarNo ratings yet
- Instructor's Presentation-Lipids and LipoproteinsDocument43 pagesInstructor's Presentation-Lipids and Lipoproteinsjomel rondinaNo ratings yet
- Lipids and Dyslipoproteinemia - 2020Document116 pagesLipids and Dyslipoproteinemia - 2020Aria Jean MostajoNo ratings yet
- 1.02 - Hemostasis, Surgical Bleeding and TransfusionsDocument7 pages1.02 - Hemostasis, Surgical Bleeding and TransfusionsPhilip Patrick LeeNo ratings yet
- Mockboards Reviewer FinalDocument161 pagesMockboards Reviewer FinalRoselle Joyce Arce CalubanNo ratings yet
- BCH 307-LipoproteinsDocument3 pagesBCH 307-LipoproteinsIsabel WilliamsNo ratings yet
- 08 01 MedLipid 2012english JavDocument100 pages08 01 MedLipid 2012english Javanthony.johNo ratings yet
- Lipids and Lipoprotein PDFDocument13 pagesLipids and Lipoprotein PDFJezzah Mae CañeteNo ratings yet
- (CLINPATH) Lipids and DyslipoproteinemiaDocument5 pages(CLINPATH) Lipids and DyslipoproteinemiaJolaine ValloNo ratings yet
- Lipids and LipoproteinsDocument5 pagesLipids and LipoproteinsMica BernardoNo ratings yet
- LIPIDSDocument6 pagesLIPIDSluzvi3110No ratings yet
- Lecture 10 - 18.9.08 - Lipid Metabolism and Diet - Lipid Transport Element 5 Lect 10 RevisedDocument26 pagesLecture 10 - 18.9.08 - Lipid Metabolism and Diet - Lipid Transport Element 5 Lect 10 RevisedRatnahKumar28No ratings yet
- 11metabolism of LipidsDocument80 pages11metabolism of LipidsHumrazNo ratings yet
- 22 - Hypolipdemic DrugsDocument64 pages22 - Hypolipdemic Drugsmashe1No ratings yet
- 2.5.2 LipidsDocument10 pages2.5.2 Lipidscamille chuaNo ratings yet
- LG - Lipid MetabolismDocument116 pagesLG - Lipid MetabolismRawa AyubNo ratings yet
- Mls 311 Lecture Notes 4Document28 pagesMls 311 Lecture Notes 4CoffeeswanNo ratings yet
- Student Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentDocument5 pagesStudent Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentMelody PardilloNo ratings yet
- FLASHCARDSDocument5 pagesFLASHCARDSAngel CalambaNo ratings yet
- Module 3 LipidsDocument9 pagesModule 3 LipidsZabelle BungarNo ratings yet
- LipidsDocument12 pagesLipidsOsannah Irish InsongNo ratings yet
- Lipioprotein Lec11 PDFDocument44 pagesLipioprotein Lec11 PDFحسن محمد سعيد جاسمNo ratings yet
- Pathology and Pathophysiology ALL+QUIZDocument235 pagesPathology and Pathophysiology ALL+QUIZomer.buzagloNo ratings yet
- 7 Overview of LipidDocument85 pages7 Overview of LipidReda SoNo ratings yet
- LipidsDocument6 pagesLipidsJohn Fritz Gerald BascoNo ratings yet
- Interpretation of Lipid Parameters by Prof. Dr. M. JawedDocument24 pagesInterpretation of Lipid Parameters by Prof. Dr. M. Jawedفيصل فهدNo ratings yet
- Lipoprotein MetabolismDocument6 pagesLipoprotein MetabolismVincent MwirigiNo ratings yet
- Biochem 1Document40 pagesBiochem 1LinhNguyeNo ratings yet
- 4-Biological Membrane and Transport 21-22Document21 pages4-Biological Membrane and Transport 21-22sarahwassel2015No ratings yet
- Dislipidemia Obesitas SM HiperurisemiaDocument154 pagesDislipidemia Obesitas SM HiperurisemiaKurniawanArhamNo ratings yet
- Plasma Lipid LectureDocument40 pagesPlasma Lipid LectureJolaoluwa AkinyemiNo ratings yet
- Annals of Clinical Biochemistry: International Journal of Laboratory MedicineDocument93 pagesAnnals of Clinical Biochemistry: International Journal of Laboratory MedicinePaula VillaNo ratings yet
- Plasma Lipoproteins - METABOLISM PDFDocument4 pagesPlasma Lipoproteins - METABOLISM PDFRishabhNo ratings yet
- LipoproteinsDocument30 pagesLipoproteinsApurba PradhanNo ratings yet
- Physiology Study MaterialsDocument68 pagesPhysiology Study MaterialsBruntNo ratings yet
- Lipid TransportDocument5 pagesLipid TransportMark Joseph PalicNo ratings yet
- Structure of Cell Membrane & Cellular Junctions: Pradeep Singh M.Sc. Medical Biochemistry Himsr, Jamia HamdardDocument37 pagesStructure of Cell Membrane & Cellular Junctions: Pradeep Singh M.Sc. Medical Biochemistry Himsr, Jamia HamdardFarhan AhmedNo ratings yet
- Carol Davila Pathophysiology NotesDocument10 pagesCarol Davila Pathophysiology NotesGiorgos Doukas KaranasiosNo ratings yet
- Lipids and Lipoproteins: Major Lipoprotein ClassesDocument1 pageLipids and Lipoproteins: Major Lipoprotein ClassesLOU BLESSY CASINONo ratings yet
- Assignment 3.1 - LipidsDocument4 pagesAssignment 3.1 - LipidsJameseu KimNo ratings yet
- 2 - Blood and ImmunologyDocument66 pages2 - Blood and Immunologyharami666No ratings yet
- CB CH 07 LipidsDocument30 pagesCB CH 07 LipidsDeemaNo ratings yet
- Lipoproteins AsmDocument34 pagesLipoproteins AsmHassan HarunaNo ratings yet
- LDL y AterogenesisDocument6 pagesLDL y AterogenesisMEDICOBLASTO EN PROSESONo ratings yet
- Triglyceride in Nephrotic SyndromeDocument2 pagesTriglyceride in Nephrotic Syndromemd191031No ratings yet
- Komponen Lipid, Katabolisme Asam Lemak, Biosintesis Asam LemakDocument69 pagesKomponen Lipid, Katabolisme Asam Lemak, Biosintesis Asam Lemakalvaedison00No ratings yet
- Lipoprotein MetabolismDocument60 pagesLipoprotein MetabolismI MADE MIARTA YASANo ratings yet
- BloodDocument32 pagesBloodPushpa AdhikariNo ratings yet
- Lec. 12 Biochemistry IIDocument22 pagesLec. 12 Biochemistry IIGames beautifulNo ratings yet
- Lipoprotein MetabolismDocument23 pagesLipoprotein MetabolismDarien LiewNo ratings yet
- LipidsDocument3 pagesLipidsBEA PETILNo ratings yet
- Chemistry, Synthesis and Functions of Lipoproteins (LDL, VLDL, Chylomicrons) Learning ObjectivesDocument8 pagesChemistry, Synthesis and Functions of Lipoproteins (LDL, VLDL, Chylomicrons) Learning ObjectivesPatar HutagalungNo ratings yet
- Lipid Profile Disease and DiagnosisDocument31 pagesLipid Profile Disease and DiagnosisGeetanjali Jha100% (1)
- 22 MembranesDocument27 pages22 MembranesSierra OrtizNo ratings yet
- Lipid Metabolism 2009Document12 pagesLipid Metabolism 2009alphius_mendozaNo ratings yet
- One Hundred Thousand People End Up in The Hospital Every YearDocument4 pagesOne Hundred Thousand People End Up in The Hospital Every YearRea Dominique CabanillaNo ratings yet
- Peripheral Venous and LymphaticsDocument34 pagesPeripheral Venous and LymphaticsRea Dominique CabanillaNo ratings yet
- Surgery II: Congenital Heart DiseaseDocument10 pagesSurgery II: Congenital Heart DiseaseRea Dominique CabanillaNo ratings yet
- #2A CNS Tumors RCE Revised 20211029 1of2 1Document36 pages#2A CNS Tumors RCE Revised 20211029 1of2 1Rea Dominique CabanillaNo ratings yet
- CP3 Assignment1Document2 pagesCP3 Assignment1Rea Dominique CabanillaNo ratings yet
- Conduct of Normal Labor and DeliveryDocument141 pagesConduct of Normal Labor and DeliveryRea Dominique CabanillaNo ratings yet
- Basic Diagnostic Test Part 1Document13 pagesBasic Diagnostic Test Part 1Rea Dominique CabanillaNo ratings yet
- Aplastic Anemia Drug Drug Category Mechanism of ActionDocument21 pagesAplastic Anemia Drug Drug Category Mechanism of ActionRea Dominique CabanillaNo ratings yet
- Im Cluster 2 Master Table UpdatedDocument246 pagesIm Cluster 2 Master Table UpdatedRea Dominique CabanillaNo ratings yet
- CP3 Assignment1Document2 pagesCP3 Assignment1Rea Dominique CabanillaNo ratings yet
- IM: Gastroenterology: Approach To Patients With Liver DisordersDocument15 pagesIM: Gastroenterology: Approach To Patients With Liver DisordersRea Dominique CabanillaNo ratings yet
- CLINICAL DIAGNOSTIC TEST PART 2 Without KeyDocument22 pagesCLINICAL DIAGNOSTIC TEST PART 2 Without KeyRea Dominique CabanillaNo ratings yet
- Cranial Nerve AsxDocument3 pagesCranial Nerve AsxRea Dominique CabanillaNo ratings yet
- Obstetrics: Topic OutlineDocument22 pagesObstetrics: Topic OutlineRea Dominique CabanillaNo ratings yet
- Respiratory Disorders & TB in Children (Part I and Ii) - Dr. MendozaDocument17 pagesRespiratory Disorders & TB in Children (Part I and Ii) - Dr. MendozaRea Dominique CabanillaNo ratings yet
- Ophthalmology 0201B Blurring3Document11 pagesOphthalmology 0201B Blurring3Rea Dominique CabanillaNo ratings yet
- Quiz On Peripheral Venous Lymphatic DiseaseDocument5 pagesQuiz On Peripheral Venous Lymphatic DiseaseRea Dominique CabanillaNo ratings yet
- OB Normal Labor and Delivery 1Document6 pagesOB Normal Labor and Delivery 1Rea Dominique CabanillaNo ratings yet
- Pedia 031 Kawasaki Disease 1Document18 pagesPedia 031 Kawasaki Disease 1Rea Dominique CabanillaNo ratings yet
- Cryptococcosis: Further ReadingDocument4 pagesCryptococcosis: Further ReadingRea Dominique CabanillaNo ratings yet
- Obstetrics: Topic OutlineDocument5 pagesObstetrics: Topic OutlineRea Dominique CabanillaNo ratings yet
- Blurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocDocument15 pagesBlurring of Vision Ii: Retinal Vascular Disorders: Dr. Jose BondocRea Dominique CabanillaNo ratings yet
- EVAL OF FEMALE PELVIS TRANS Dr. ReylesDocument5 pagesEVAL OF FEMALE PELVIS TRANS Dr. ReylesRea Dominique CabanillaNo ratings yet
- Rheumatic Fever and Rheumatic Heart Disease: PediatricsDocument8 pagesRheumatic Fever and Rheumatic Heart Disease: PediatricsRea Dominique CabanillaNo ratings yet
- Allergology and ImmunologyDocument14 pagesAllergology and ImmunologyRea Dominique CabanillaNo ratings yet
- PATHO S01.T01 - Cellular Adaptation Cell Injury and Cell DeathDocument7 pagesPATHO S01.T01 - Cellular Adaptation Cell Injury and Cell DeathRea Dominique CabanillaNo ratings yet
- Congestive Heart Failure: Pediatrics 2Document11 pagesCongestive Heart Failure: Pediatrics 2Rea Dominique CabanillaNo ratings yet
- Quotient of Powers Property 9.3: ActivityDocument6 pagesQuotient of Powers Property 9.3: ActivityPAVO, JUDY V.No ratings yet
- Niroula RK - Cytogenetics of Rice Thesis 2003-2012Document172 pagesNiroula RK - Cytogenetics of Rice Thesis 2003-2012mnkjhpNo ratings yet
- Child Laour 6Document24 pagesChild Laour 6Momina SaeedNo ratings yet
- Analysis of Customer Segmentation Based On Recency, Frequency, and Monetary at PT Pegadaian in Padang City As Basis On The Analysis of Segmentation and Developing CRM StrategiesDocument8 pagesAnalysis of Customer Segmentation Based On Recency, Frequency, and Monetary at PT Pegadaian in Padang City As Basis On The Analysis of Segmentation and Developing CRM StrategiesAnonymous izrFWiQNo ratings yet
- First Grading English Reviewer-Grade VIDocument9 pagesFirst Grading English Reviewer-Grade VIloraineNo ratings yet
- Takuji Kawano - Soul CaliburDocument2 pagesTakuji Kawano - Soul CaliburMatthew MeleadyNo ratings yet
- UnpublishedDocument6 pagesUnpublishedScribd Government DocsNo ratings yet
- Ma Trận Đề Thi Kiểm Tra Chất Lượng Học Kỳ IiDocument4 pagesMa Trận Đề Thi Kiểm Tra Chất Lượng Học Kỳ IiAlaska EnglishNo ratings yet
- 3 - Physiology (BusySPR 2016 SBAs)Document144 pages3 - Physiology (BusySPR 2016 SBAs)KeeranmayeeishraNo ratings yet
- Recit 11 AnswersDocument4 pagesRecit 11 AnswersDiyanikaNo ratings yet
- NEET Biology MCQDocument6 pagesNEET Biology MCQIsh MalikNo ratings yet
- Paat v. CA GR 111107Document7 pagesPaat v. CA GR 111107Luna KimNo ratings yet
- Briefly Describe The Three Common Types of Models and Give An Example of EachDocument3 pagesBriefly Describe The Three Common Types of Models and Give An Example of Eachsamuel debebeNo ratings yet
- Kathryn Pawelko - Edci 410 - English Classroom Technology Statement - FinalDocument6 pagesKathryn Pawelko - Edci 410 - English Classroom Technology Statement - Finalapi-502308514No ratings yet
- AssignmentDocument3 pagesAssignmentTinasheNo ratings yet
- Kapferer Magic Reason Beyond RationalismDocument31 pagesKapferer Magic Reason Beyond RationalismcartilepemasaNo ratings yet
- An Introduction To Cuban TheatreDocument15 pagesAn Introduction To Cuban TheatreChandrima BanerjeeNo ratings yet
- Integrated Course DesignDocument15 pagesIntegrated Course DesignAngelica Gaspay EstalillaNo ratings yet
- 10th Math Workbook PDFDocument292 pages10th Math Workbook PDFsuraj100% (2)
- E-Portfolio Reflective IntroDocument6 pagesE-Portfolio Reflective IntroAnonymous MNn0v3No ratings yet
- Chapter 3: Graduate Tracer StudyDocument30 pagesChapter 3: Graduate Tracer StudyEn TenNo ratings yet
- Implementation of HIRARC in A Small Sized Organization: September 2015Document7 pagesImplementation of HIRARC in A Small Sized Organization: September 2015faizNo ratings yet
- LCFesR Meter InstallationDocument3 pagesLCFesR Meter InstallationbiotekyNo ratings yet
- The Second Mile Annual Report 2010Document12 pagesThe Second Mile Annual Report 2010mosesloaf8619No ratings yet