Professional Documents
Culture Documents
The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1
The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1
Uploaded by
Jewel Alexis Mendoza AGAYANOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1
The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Ltd. 1
Uploaded by
Jewel Alexis Mendoza AGAYANCopyright:
Available Formats
Chapter 15
The Urinary System
Functions of the Urinary System
• Kidneys dispose of waste products in urine
• Nitrogenous wastes
• Toxins
• Drugs
• Excess ions
• Kidneys’ regulatory functions include:
• Production of renin to maintain blood pressure
• Production of erythropoietin to stimulate red blood cell production
• Conversion of vitamin D to its active form
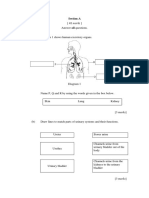
Organs of the Urinary System
• Kidneys
• Ureters
• Urinary bladder
• Urethra
Kidneys
• Location and structure
• The kidneys are situated against the dorsal body wall in a retroperitoneal
position (behind the parietal peritoneum)
• The kidneys are situated at the level of the T 12 to L3 vertebrae
• The right kidney is slightly lower than the left (because of position of the liver)
Kidneys
• Kidney structure
• An adult kidney is about 12 cm (5 in) long and 6 cm (2.5 in) wide
• Renal hilum
• A medial indentation where several structures enter or exit the kidney
(ureters, renal blood vessels, and nerves)
• An adrenal gland sits atop each kidney
Kidneys
• Kidney structure (continued)
• Three protective layers enclose the kidney
• Fibrous capsule encloses each kidney
• Perirenal fat capsule surrounds the kidney and cushions against blows
• Renal fascia is the most superficial layer that anchors the kidney and
adrenal gland to surrounding structures
© 2018 Pearson Education, Ltd. 1
Kidneys
• Kidney structure (continued)
• Three regions revealed in a longitudinal section
1. Renal cortex—outer region
2. Renal medulla—deeper region
• Renal (medullary) pyramids—triangular regions of tissue in the
medulla
• Renal columns—extensions of cortexlike material that separate
the pyramids
Kidneys
• Kidney structure (continued)
• Three regions (continued)
3. Renal pelvis—medial region that is a flat, funnel-shaped tube
• Calyces form cup-shaped “drains” that enclose the renal
pyramids
• Calyces collect urine and send it to the renal pelvis, on to the
ureter, and to the urinary bladder for storage
Kidneys
• Blood supply
• One-quarter of the total blood supply of the body passes through the kidneys
each minute
• Renal artery provides each kidney with arterial blood supply
• Renal artery divides into segmental arteries → interlobar arteries → arcuate
arteries → cortical radiate arteries
Kidneys
• Venous blood flow
• Cortical radiate veins → arcuate veins → interlobar veins → renal vein
• There are no segmental veins
• Renal vein returns blood to the inferior vena cava
Nephrons
• Structural and functional units of the kidneys
• Each kidney contains over a million nephrons
• Each nephron consists of two main structures
1. Renal corpuscle
2. Renal tubule
2 © 2018 Pearson Education, Ltd.
Nephrons
• Renal corpuscle consists of:
1. Glomerulus, a knot of capillaries made of podocytes
• Podocytes make up the inner (visceral) layer of the glomerular capsule
• Foot processes cling to the glomerulus
• Filtration slits create a porous membrane—ideal for filtration
2. Glomerular (Bowman’s) capsule is a cup-shaped structure that surrounds the
glomerulus
• First part of the renal tubule
Nephrons
• Renal tubule
• Extends from glomerular capsule and ends when it empties into the collecting
duct
• From the glomerular (Bowman’s) capsule, the subdivisions of the renal tubule
are:
1. Proximal convoluted tubule (PCT)
2. Nephron loop (loop of Henle)
3. Distal convoluted tubule (DCT)
Nephrons
• Cortical nephrons
• Located entirely in the cortex
• Include most nephrons
• Juxtamedullary nephrons
• Found at the cortex-medulla junction
• Nephron loop dips deep into the medulla
• Collecting ducts collect urine from both types of nephrons, through the renal
pyramids, to the calyces, and then to the renal pelvis
Nephrons
• Two capillary beds associated with each nephron
1. Glomerulus
2. Peritubular capillary bed
© 2018 Pearson Education, Ltd. 3
Nephrons
• Glomerulus
• Fed and drained by arterioles
• Afferent arteriole—arises from a cortical radiate artery and feeds the
glomerulus
• Efferent arteriole—receives blood that has passed through the
glomerulus
• Specialized for filtration
• High pressure forces fluid and solutes out of blood and into the glomerular
capsule
Nephrons
• Peritubular capillary beds
• Arise from the efferent arteriole of the glomerulus
• Low-pressure, porous capillaries
• Adapted for absorption instead of filtration
• Cling close to the renal tubule to receive solutes and water from tubule cells
• Drain into the interlobar veins
Urine Formation and Characteristics
• Urine formation is the result of three processes
1. Glomerular filtration
2. Tubular reabsorption
3. Tubular secretion
Urine Formation and Characteristics
• Glomerular filtration
• The glomerulus is a filter
• Filtration is a nonselective passive process
• Water and solutes smaller than proteins are forced through glomerular
capillary walls
• Proteins and blood cells are normally too large to pass through the
filtration membrane
• Once in the capsule, fluid is called filtrate
• Filtrate leaves via the renal tubule
Urine Formation and Characteristics
• Glomerular filtration (continued)
• Filtrate will be formed as long as systemic blood pressure is normal
• If arterial blood pressure is too low, filtrate formation stops because
glomerular pressure will be too low to form filtrate
4 © 2018 Pearson Education, Ltd.
Urine Formation and Characteristics
• Tubular reabsorption
• The peritubular capillaries reabsorb useful substances from the renal tubule
cells, such as:
• Water
• Glucose
• Amino acids
• Ions
• Some reabsorption is passive; most is active (ATP)
• Most reabsorption occurs in the proximal convoluted tubule
Urine Formation and Characteristics
• Tubular secretion
• Reabsorption in reverse
• Some materials move from the blood of the peritubular capillaries into the
renal tubules to be eliminated in filtrate
• Hydrogen and potassium ions
• Creatinine
Urine Formation and Characteristics
• Tubular secretion (continued)
• Secretion is important for:
• Getting rid of substances not already in the filtrate
• Removing drugs and excess ions
• Maintaining acid-base balance of blood
• Materials left in the renal tubule move toward the ureter
Urine Formation and Characteristics
• Nitrogenous wastes
• Nitrogenous waste products are poorly reabsorbed, if at all
• Tend to remain in the filtrate and are excreted from the body in the urine
• Urea—end product of protein breakdown
• Uric acid—results from nucleic acid metabolism
• Creatinine—associated with creatine metabolism in muscles
Urine Formation and Characteristics
• In 24 hours, about 1.0 to 1.8 liters of urine are produced
• Urine and filtrate are different
• Filtrate contains everything that blood plasma does (except proteins)
• Urine is what remains after the filtrate has lost most of its water, nutrients, and
necessary ions through reabsorption
• Urine contains nitrogenous wastes and substances that are not needed
© 2018 Pearson Education, Ltd. 5
Urine Formation and Characteristics
• Urine characteristics
• Clear and pale to deep yellow in color
• Yellow color is normal and due to the pigment urochrome (from the
destruction of hemoglobin) and solutes
• Dilute urine is a pale, straw color
• Sterile at the time of formation
• Slightly aromatic, but smells like ammonia with time
• Slightly acidic (pH of 6)
• Specific gravity of 1.001 to 1.035
Urine Formation and Characteristics
• Solutes normally found in urine
• Sodium and potassium ions
• Urea, uric acid, creatinine
• Ammonia
• Bicarbonate ions
Urine Formation and Characteristics
• Solutes NOT normally found in urine
• Glucose
• Blood proteins
• Red blood cells
• Hemoglobin
• WBCs (pus)
• Bile
Ureters
• Slender tubes 25–30 cm (10–12 inches) attaching the kidney to the urinary bladder
• Continuous with the renal pelvis
• Enter the posterior aspect of the urinary bladder
• Run behind the peritoneum
• Peristalsis aids gravity in urine transport
Urinary Bladder
• Smooth, collapsible, muscular sac situated posterior to the pubic symphysis
• Stores urine temporarily
• Trigone—triangular region of the urinary bladder base based on three openings
• Two openings from the ureters (ureteral orifices)
• One opening to the urethra (internal urethral orifice)
• In males, the prostate surrounds the neck of the urinary bladder
6 © 2018 Pearson Education, Ltd.
Urinary Bladder
• Wall of the urinary bladder
• Three layers of smooth muscle collectively called the detrusor muscle
• Mucosa made of transitional epithelium
• Walls are thick and folded in an empty urinary bladder
• Urinary bladder can expand significantly without increasing internal pressure
Urinary Bladder
• Capacity of the urinary bladder
• A moderately full bladder is about 5 inches long and holds about 500 ml of
urine
• Capable of holding twice that amount of urine
Urethra
• Thin-walled tube that carries urine from the urinary bladder to the outside of the body
by peristalsis
• Function
• Females—carries only urine
• Males—carries urine and sperm
Urethra
• Release of urine is controlled by two sphincters
1. Internal urethral sphincter
• Involuntary and made of smooth muscle
2. External urethral sphincter
• Voluntary and made of skeletal muscle
Urethra
• Length
• In females: 3 to 4 cm (1.5 inches long)
• In males: 20 cm (8 inches long)
• Location
• Females—anterior to the vaginal opening
• Males—travels through the prostate and penis
• Prostatic urethra
• Membranous urethra
• Spongy urethra
© 2018 Pearson Education, Ltd. 7
Micturition
• Micturition
• Voiding, or emptying of the urinary bladder
• Two sphincters control the release of urine, the internal urethral sphincter and
external urethral sphincter
• Bladder collects urine to 200 ml
• Stretch receptors transmit impulses to the sacral region of the spinal cord
• Impulses travel back to the bladder via the pelvic splanchnic nerves to cause
bladder contractions
Micturition
• When contractions become stronger, urine is forced past the involuntary internal
sphincter into the upper urethra
• Urge to void is felt
• The external sphincter is voluntarily controlled, so micturition can usually be delayed
Fluid, Electrolyte, and Acid-Base Balance
• Blood composition depends on three factors
1. Diet
2. Cellular metabolism
3. Urine output
Fluid, Electrolyte, and Acid-Base Balance
• Kidneys have four roles in maintaining blood composition
1. Excreting nitrogen-containing wastes (previously discussed)
2. Maintaining water balance of the blood
3. Maintaining electrolyte balance of the blood
4. Ensuring proper blood pH
Maintaining Water Balance of the Blood
• Normal amount of water in the human body
• Young adult females = 50%
• Young adult males = 60%
• Babies = 75%
• The elderly = 45%
• Water is necessary for many body functions, and levels must be maintained
8 © 2018 Pearson Education, Ltd.
Maintaining Water Balance of the Blood
• Water occupies three main fluid compartments
1. Intracellular fluid (ICF)
• Fluid inside cells
• Accounts for two-thirds of body fluid
2. Extracellular fluid (ECF)
• Fluids outside cells; includes blood plasma, interstitial fluid (IF), lymph,
and transcellular fluid
3. Plasma (blood) is ECF, but accounts for 3L of total body water.
• Links external and internal environments (Figure 15.9)
Maintaining Water Balance of the Blood
• The link between water and electrolytes
• Electrolytes are charged particles (ions) that conduct electrical current in an
aqueous solution
• Sodium, potassium, and calcium ions are electrolytes
Maintaining Water Balance of the Blood
• Regulation of water intake and output
• Water intake must equal water output if the body is to remain properly
hydrated
• Sources for water intake
• Ingested foods and fluids
• Water produced from metabolic processes (10%)
• Thirst mechanism is the driving force for water intake
Maintaining Water Balance of the Blood
• Thirst mechanism
• Osmoreceptors are sensitive cells in the hypothalamus that become more
active in reaction to small changes in plasma solute concentration
• When activated, the thirst center in the hypothalamus is notified
• A dry mouth due to decreased saliva also promotes the thirst mechanism
• Both reinforce the drive to drink
Maintaining Water Balance of the Blood
• Sources of water output
• Lungs (insensible since we cannot sense the water leaving)
• Perspiration
• Feces
• Urine
© 2018 Pearson Education, Ltd. 9
Maintaining Water Balance of the Blood
• Hormones are primarily responsible for reabsorption of water and electrolytes by the
kidneys
• Antidiuretic hormone (ADH) prevents excessive water loss in the urine and
increases water reabsorption
• ADH targets the kidney’s collecting ducts
Maintaining Electrolyte Balance
• Small changes in electrolyte concentrations cause water to move from one fluid
compartment to another
• A second hormone, aldosterone, helps regulate blood composition and blood volume
by acting on the kidney
• For each sodium ion reabsorbed, a chloride ion follows, and a potassium ion
is secreted into the filtrate
• Water follows salt: when sodium is reabsorbed, water follows it passively back
into the blood
Electrolyte Balance
• Renin-angiotensin mechanism
• Most important trigger for aldosterone release
• Mediated by the juxtaglomerular (JG) apparatus of the renal tubules
• When cells of the JG apparatus are stimulated by low blood pressure, the
enzyme renin is released into blood
Electrolyte Balance
• Renin-angiotensin mechanism (continued)
• Renin catalyzes reactions that produce angiotensin II
• Angiotensin II causes vasoconstriction and aldosterone release
• Result is increase in blood volume and blood pressure
Maintaining Acid-Base Balance of Blood
• Blood pH must remain between 7.35 and 7.45 to maintain homeostasis
• Alkalosis—pH above 7.45
• Acidosis—pH below 7.35
• Physiological acidosis—pH between 7.0 and 7.35
Maintaining Acid-Base Balance of Blood
• Kidneys play greatest role in maintaining acid-base balance
• Other acid-base controlling systems
• Blood buffers
10 © 2018 Pearson Education, Ltd.
• Respiration
Maintaining Acid-Base Balance of Blood
• Blood buffers
• Acids are proton (H+) donors
• Strong acids dissociate completely and liberate all of their H + in water
• Weak acids, such as carbonic acid, dissociate only partially
• Bases are proton (H+) acceptors
• Strong bases dissociate easily in water and tie up H +
• Weak bases, such as bicarbonate ion and ammonia, are slower to
accept H+
Maintaining Acid-Base Balance of Blood
• Molecules react to prevent dramatic changes in hydrogen ion (H +) concentrations
• Bind to H+ when pH drops
• Release H+ when pH rises
• Three major chemical buffer systems
1. Bicarbonate buffer system
2. Phosphate buffer system
3. Protein buffer system
Maintaining Acid-Base Balance of Blood
• The bicarbonate buffer system
• Mixture of carbonic acid (H2CO3) and sodium bicarbonate (NaHCO3)
• Carbonic acid is a weak acid that does not dissociate much in neutral
or acid solutions
• Bicarbonate ions (HCO3−) react with strong acids to change them to
weak acids
HCl + NaHCO3 → H2CO3 + NaCl
strong acid weak base weak acid salt
Maintaining Acid-Base Balance of Blood
• The bicarbonate buffer system (continued)
• Carbonic acid dissociates in the presence of a strong base to form a weak
base and water
NaOH + H2CO3 → NaHCO3 + H2O
strong base weak acid weak base water
Maintaining Acid-Base Balance of Blood
• Respiratory mechanisms
• Respiratory rate can rise and fall depending on changing blood pH to retain
© 2018 Pearson Education, Ltd. 11
CO2 (decreasing the blood pH) or remove CO2 (increasing the blood pH)
12 © 2018 Pearson Education, Ltd.
Maintaining Acid-Base Balance of Blood
• Renal mechanisms
• When blood pH rises:
• Bicarbonate ions are excreted
• Hydrogen ions are retained by kidney tubules
• When blood pH falls:
• Bicarbonate ions are reabsorbed
• Hydrogen ions are secreted
• Urine pH varies from 4.5 to 8.0
Developmental Aspects of the Urinary System
• The kidneys begin to develop in the first few weeks of embryonic life and are
excreting urine by the third month of fetal life
• Common congenital abnormalities include polycystic kidney and hypospadias
• Common urinary system problems in children and young to middle-aged adults
include infections caused by fecal microorganisms, microorganisms causing sexually
transmitted infections, and Streptococcus
Developmental Aspects of the Urinary System
• Control of the voluntary urethral sphincter does not start until age 18 months
• Complete nighttime control may not occur until the child is 4 years old
• Urinary tract infections (UTIs) are the only common problems before old age
• Escherichia coli (E. coli), a bacterium, accounts for 80 percent of UTIs
Developmental Aspects of the Urinary System
• Renal failure is an uncommon but serious problem in which the kidneys are unable
to concentrate urine, and dialysis must be done to maintain chemical homeostasis of
blood
• With age, filtration rate decreases and tubule cells become less efficient at
concentrating urine, leading to urgency, frequency, and incontinence
• In men, urinary retention is another common problem
Developmental Aspects of the Urinary System
• Problems associated with aging
• Urgency—feeling that it is necessary to void
• Frequency—frequent voiding of small amounts of urine
• Nocturia—need to get up during the night to urinate
• Incontinence—loss of control
• Urinary retention—common in males, often the result of hypertrophy of the
prostate gland
© 2018 Pearson Education, Ltd. 13
You might also like
- PhysioEx Exercise 9 Activity 1Document4 pagesPhysioEx Exercise 9 Activity 1MARILYN MARIANA HERNANDEZ MENDOZANo ratings yet
- The Cardiovascular System: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical CollegeDocument124 pagesThe Cardiovascular System: Lecture Presentation by Patty Bostwick-Taylor Florence-Darlington Technical Collegelourd nabNo ratings yet
- Anatomy and Physiology of The Female Reproductive SystemDocument34 pagesAnatomy and Physiology of The Female Reproductive Systemruthpebbles100% (2)
- The Urinary System Functions of The Urinary System: © 2018 Pearson Education, Inc. 1Document13 pagesThe Urinary System Functions of The Urinary System: © 2018 Pearson Education, Inc. 1Stef FieNo ratings yet
- Bio 208 Urinary SystemDocument121 pagesBio 208 Urinary SystemNazir RabiuNo ratings yet
- Anatomy and Physiology RenalDocument5 pagesAnatomy and Physiology RenalMaryGeneville Opeña AbitNo ratings yet
- Life Sciences Grade 11 Term 3 Week 5 - 2020Document12 pagesLife Sciences Grade 11 Term 3 Week 5 - 2020YONDELA MbandezeloNo ratings yet
- 5 Renal SystemDocument7 pages5 Renal SystemHajar ObeidatNo ratings yet
- Urinary SystemDocument68 pagesUrinary SystemWilson chumpukaNo ratings yet
- Urinary SystemDocument16 pagesUrinary SystemDragan KankarasNo ratings yet
- Urogenital Guide Notes PDFDocument26 pagesUrogenital Guide Notes PDFJoryn LimNo ratings yet
- Excretory SystemDocument42 pagesExcretory Systemadedayoadeboye0107No ratings yet
- Urinary SystemDocument55 pagesUrinary SystemChristian UdaundoNo ratings yet
- Excretory SystemDocument37 pagesExcretory SystemBlister CountNo ratings yet
- Kidneys and ExcretionDocument28 pagesKidneys and ExcretionD-Cristen OrlandoNo ratings yet
- KidneyDocument85 pagesKidneyIshita SinghNo ratings yet
- Excretion and KidneysDocument39 pagesExcretion and KidneyselizabethNo ratings yet
- Urinary SystemDocument34 pagesUrinary SystemJULIANNE ANACTANo ratings yet
- 2304 UrinaryDocument31 pages2304 UrinaryAliyah Tofani PawelloiNo ratings yet
- CH 26 The Urinary SystemDocument95 pagesCH 26 The Urinary SystemnunungNo ratings yet
- Urinary System: Kidney Ureter BladderDocument12 pagesUrinary System: Kidney Ureter BladderAshwini Harwale SonwaneNo ratings yet
- The Urinary SystemDocument34 pagesThe Urinary Systemaarti HingeNo ratings yet
- Anatomy and Histology of Urinary System: Amina Arshad LecturerDocument33 pagesAnatomy and Histology of Urinary System: Amina Arshad LecturerMuhammad TahirNo ratings yet
- Lecture 8 Urinary SystemDocument46 pagesLecture 8 Urinary SystemKang MonNo ratings yet
- Urinary SystemDocument32 pagesUrinary SystemDr Anais AsimNo ratings yet
- The Excretory/ Urinary System: Lecture By: Marri Jmelou M. Roldan, MSCDocument29 pagesThe Excretory/ Urinary System: Lecture By: Marri Jmelou M. Roldan, MSCHeaven SolNo ratings yet
- Parmann Notes 16 17 TeacherDocument20 pagesParmann Notes 16 17 Teacherapi-305436791No ratings yet
- Part 7 - Human Urinary SystemDocument18 pagesPart 7 - Human Urinary SystemAmal Naeem JHNo ratings yet
- Urinary System: Bela Sartina Evita Rossa Futti Hatum MunawarohDocument10 pagesUrinary System: Bela Sartina Evita Rossa Futti Hatum MunawarohBelaNo ratings yet
- 3 - Urinary SystemDocument19 pages3 - Urinary Systemvgf58jsq6cNo ratings yet
- Kidney PhysiologyDocument144 pagesKidney PhysiologySilasNo ratings yet
- Chapter 11 - ExcretionDocument46 pagesChapter 11 - Excretionapi-372850875% (4)
- Urinary SystemDocument29 pagesUrinary SystemTrisha AmitNo ratings yet
- Excretory System in Human LecDocument20 pagesExcretory System in Human LecUnza WaqarNo ratings yet
- Part 9 - Human Urinary System Anatomy - UpdatedDocument29 pagesPart 9 - Human Urinary System Anatomy - UpdatedمحمدالسلمانNo ratings yet
- Excretory SystemDocument39 pagesExcretory SystemTajXNo ratings yet
- The Urinary System: DR P VijayalakshmiDocument79 pagesThe Urinary System: DR P VijayalakshmiVijaya LakshmiNo ratings yet
- Urinary SystemDocument36 pagesUrinary SystemguintogeorgetteNo ratings yet
- Urogenital SystemDocument106 pagesUrogenital SystemBen MasungcadNo ratings yet
- Jigjiga University College of Veterinary Medicine: by DR Mahamud A. (DVM, MSC)Document56 pagesJigjiga University College of Veterinary Medicine: by DR Mahamud A. (DVM, MSC)Shemsu LoveNo ratings yet
- Urinary SystemDocument20 pagesUrinary SystemKelvin MallariNo ratings yet
- Urinary SystemDocument20 pagesUrinary SystemKelvin Mallari100% (1)
- Urinary System PresentationDocument29 pagesUrinary System PresentationDominic WamambaNo ratings yet
- Urinary System: Kidney Ureter BladderDocument35 pagesUrinary System: Kidney Ureter BladderNorilleJaneDequinaNo ratings yet
- Notes Life Processes (Excretion)Document2 pagesNotes Life Processes (Excretion)07.joycharlieNo ratings yet
- Anatomy and Physiology of The Urinary System: Dipali HarkhaniDocument43 pagesAnatomy and Physiology of The Urinary System: Dipali HarkhaniZala KarmitNo ratings yet
- Histology of The Urinary System: BY DR C.M. OkekeDocument62 pagesHistology of The Urinary System: BY DR C.M. OkekeonyekaNo ratings yet
- Topic 2b - Homeostasis-Student v2Document52 pagesTopic 2b - Homeostasis-Student v2Angel LimNo ratings yet
- Excretory Products AND Their EliminationDocument43 pagesExcretory Products AND Their EliminationBiju MylachalNo ratings yet
- Chap 09Document15 pagesChap 09Kenneth AldeguerNo ratings yet
- Structure and Function of Kidneys: HTC2-Physiology-26-10-21 DR CH LaiDocument4 pagesStructure and Function of Kidneys: HTC2-Physiology-26-10-21 DR CH LaiVienne Yuen Wing YanNo ratings yet
- Excretion in HumansDocument35 pagesExcretion in HumansHiba MoussaliNo ratings yet
- The Urinary SysemDocument20 pagesThe Urinary SysemAmber SharifNo ratings yet
- Urinary System ObjectivesDocument48 pagesUrinary System ObjectivesMubashir Ahmed MahesarNo ratings yet
- Urinary System: BS-Radiologic Technology 2-1Document47 pagesUrinary System: BS-Radiologic Technology 2-1Julia Stefanel PerezNo ratings yet
- Module ΙV Urinary systemDocument41 pagesModule ΙV Urinary systemkeerthi krishnaNo ratings yet
- Urinary TractDocument15 pagesUrinary TractYasmin MostafaNo ratings yet
- Md2011 HRM Is 2019 NotesDocument25 pagesMd2011 HRM Is 2019 NotesShiv SookunNo ratings yet
- Difficulty UrinatingDocument76 pagesDifficulty UrinatingHera Vinandika P100% (1)
- Excretory System: Ramesh Balayar (ZRB) IOM-2015Document26 pagesExcretory System: Ramesh Balayar (ZRB) IOM-2015AbhishekNo ratings yet
- Regulations of Body FluidsDocument26 pagesRegulations of Body FluidsMarcStep De GuzmanNo ratings yet
- Kidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKidney Diseases, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- BSN 3 ProceduresDocument128 pagesBSN 3 Procedureslourd nabNo ratings yet
- Guided Lecture Notes, Chapter 2, Community-Based Nursing PracticeDocument3 pagesGuided Lecture Notes, Chapter 2, Community-Based Nursing Practicelourd nabNo ratings yet
- The Respiratory System Organs of The Respiratory System: © 2018 Pearson Education, Ltd. 1Document13 pagesThe Respiratory System Organs of The Respiratory System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- The Reproductive System The Reproductive System: © 2018 Pearson Education, Ltd. 1Document19 pagesThe Reproductive System The Reproductive System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- The Muscular System The Muscular System: © 2018 Pearson Education, Ltd. 1Document14 pagesThe Muscular System The Muscular System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Guided Lecture Notes, Chapter 1, Health Care Delivery and Evidence-Based Nursing PracticeDocument3 pagesGuided Lecture Notes, Chapter 1, Health Care Delivery and Evidence-Based Nursing Practicelourd nabNo ratings yet
- The Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1Document12 pagesThe Endocrine System The Endocrine System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- The Cardiovascular System The Cardiovascular System: EpicardiumDocument17 pagesThe Cardiovascular System The Cardiovascular System: Epicardiumlourd nabNo ratings yet
- CH - 03 The CellDocument29 pagesCH - 03 The Celllourd nabNo ratings yet
- The Skeletal System The Skeletal System: © 2018 Pearson Education, Ltd. 1Document16 pagesThe Skeletal System The Skeletal System: © 2018 Pearson Education, Ltd. 1lourd nabNo ratings yet
- Test II Anatomy LabelingDocument7 pagesTest II Anatomy Labelinglourd nabNo ratings yet
- Cell JunctionsDocument11 pagesCell Junctionslourd nabNo ratings yet
- ABG Quiz by GroupDocument13 pagesABG Quiz by Grouplourd nabNo ratings yet
- Muscles in Alphabetical OrderDocument2 pagesMuscles in Alphabetical Orderlourd nabNo ratings yet
- Head, Face and NeckDocument50 pagesHead, Face and Necklourd nabNo ratings yet
- Anatomy and Physiology: The CellDocument8 pagesAnatomy and Physiology: The Celllourd nabNo ratings yet
- Health Education NotesDocument5 pagesHealth Education Noteslourd nab50% (2)
- Anatomical PrinciplesDocument4 pagesAnatomical Principleslourd nabNo ratings yet
- Anaphy Reviewer FINALSDocument4 pagesAnaphy Reviewer FINALSim. EliasNo ratings yet
- Patho FinalDocument2 pagesPatho FinalMichael EvanNo ratings yet
- Anatomy of MicturictionDocument19 pagesAnatomy of MicturictionsalomonmarinaNo ratings yet
- Health Assessment SAS Session 17Document5 pagesHealth Assessment SAS Session 17pw49cbqxnfNo ratings yet
- Section A: Jawab Semua SoalanDocument3 pagesSection A: Jawab Semua SoalanAzreen IzetNo ratings yet
- WORKSHEET 12. 7: Homeostasis in Humans: Name: - Chapter 12 Coordination and ResponseDocument2 pagesWORKSHEET 12. 7: Homeostasis in Humans: Name: - Chapter 12 Coordination and ResponseAzmaniza AdnanNo ratings yet
- Mini Cex 1 POP CTTDocument10 pagesMini Cex 1 POP CTTZAHRA RIZQIKA ALIYYA SAFITRI -No ratings yet
- HYDRONEPHROSISDocument43 pagesHYDRONEPHROSISEureka RathinamNo ratings yet
- Staged Urethroplasty: Indications and Techniques: Charles L. Secrest, MDDocument9 pagesStaged Urethroplasty: Indications and Techniques: Charles L. Secrest, MDDKANo ratings yet
- Radiology Imaging of Urinary TractDocument40 pagesRadiology Imaging of Urinary TractMuhammad Zaniar RamadhaniNo ratings yet
- Skripsi Tanpa Bab PembahasanDocument67 pagesSkripsi Tanpa Bab PembahasanUpitFlowNo ratings yet
- Pelvic Examination: Liezel B. Cauilan MSN, MSTDocument25 pagesPelvic Examination: Liezel B. Cauilan MSN, MSTSIR ONENo ratings yet
- The Structure of A Sperm Cell - WorksheetDocument2 pagesThe Structure of A Sperm Cell - WorksheetJustine Kylle AberinNo ratings yet
- Dapus Episode 1Document6 pagesDapus Episode 1leny suardiNo ratings yet
- The Urinary System: DR RNGT Amin Samiasih, SKP - Msi.MedDocument36 pagesThe Urinary System: DR RNGT Amin Samiasih, SKP - Msi.MedSura MaduNo ratings yet
- الجهاز البوليDocument2 pagesالجهاز البوليهدير محمدNo ratings yet
- Anomalies of The Penies ...Document6 pagesAnomalies of The Penies ...Firas Abu-SamraNo ratings yet
- 1 s2.0 S0302283822016013 MainDocument11 pages1 s2.0 S0302283822016013 MainJoan Marie S. FlorNo ratings yet
- Genito-Urinary Fistulas: Yashar Najiaghdam M.DDocument33 pagesGenito-Urinary Fistulas: Yashar Najiaghdam M.DyoghaNo ratings yet
- Urinary EliminationDocument101 pagesUrinary EliminationJade Giordano100% (1)
- Nursing Care of Urolithiasis: Nursing Faculty Chatolic University of Widya Mandala Surabaya 2014Document11 pagesNursing Care of Urolithiasis: Nursing Faculty Chatolic University of Widya Mandala Surabaya 2014victor zhefaNo ratings yet
- The Truth About 2014Document22 pagesThe Truth About 2014Drew B MrtnzNo ratings yet
- 07Document24 pages07Esteban CayuelasNo ratings yet
- (K4) Male Reproductive SystemDocument73 pages(K4) Male Reproductive SystemJane Andrea Christiano DjianzonieNo ratings yet
- 5 AnatomyPhysiologyHO SpermProdStoryDocument2 pages5 AnatomyPhysiologyHO SpermProdStorylili btsNo ratings yet
- Inserting A Straight or Indwelling Catheter Catheterization - Is TheDocument2 pagesInserting A Straight or Indwelling Catheter Catheterization - Is ThezjaneNo ratings yet
- Activity 6Document5 pagesActivity 6convekz100% (3)
- Quick and Easy Medical Terminology 8Th Edition Leonard Test Bank Full Chapter PDFDocument27 pagesQuick and Easy Medical Terminology 8Th Edition Leonard Test Bank Full Chapter PDFmathewsandersa13j100% (8)