Professional Documents
Culture Documents
Espino STD Rle
Uploaded by
Emi EspinoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Espino STD Rle
Uploaded by
Emi EspinoCopyright:
Available Formats
Espino, Emilyn
BSN-III
UNIVERSITY OF LUZON
College of Nursing and Midwifery
INFECTIOUS AND INFLAMMATORY DISORDERS
CASE STUDY: THE PATIENT WITH A SEXUALLY TRANSMITTED DISEASE
A young woman comes to the STD clinic. She is defensive and seems disgusted as She
explains to the nurse that she believes she was exposed to an STD. She bases her belief
on something a friend told her, but she is reluctant to be more forth- coming about the
details, she currently denies symptoms.
She is also very angry about false accusations that people are making. The nurse
validates her decision to come in for examination and diagnosis.
1. The nurse explains that women have more health problems associated with STDs
than men. What should the nurse tell the patient? What are the health problems?
(tabulate)
Infertility and increased risk of ectopic pregnancy
Congenital infections
Neurosyphilis
Gonococcal meningitis
Gonococcal arthritis
Syphilis aortitis
Human Immune Deficiency Virus-Related Complications
2. Explain why the patient could present with this angry and defensive behavior.
What can the nurse do?
STD is a very sensitive topic and maybe the patient does not want to disclose the
information because it might spread.
Assure the patient that you will keep the information confidential
Encourage the patient to be calm by doing first deep breathing exercises
De-escalate client with a calm voice.
Avoid arguing to the client
Document incidents in an objective manner, stating factual information only.
3. What should be included in a nursing assessment of the patient with symptoms of
an STD? List and differentiate the STD and its symptoms (tabulate)
Syphilis is a bacterial infection usually spread by sexual contact. The disease starts as a
painless sore, typically on genitals, rectum, or mouth. Syphilis spreads from person to
person via skin or mucous membrane contact with these sores.
In primary syphilis, chancre
Secondary syphilis, chancre to generalized infection which includes
lymphadenopathy, arthritis, meningitis, hair loss, fever, malaise, and weight loss.
Rashes occur to the trunk, the extremities, palms of the hand and soles of the feet
In tertiary syphilis, 20% to 40% of patients with syphilis does not exhibit signs and
symptoms. Most common manifestations include aortitis and neurosyphilis as
evidenced by dementia, psychosis, paresis, stroke, or meningitis.
Chlamydia Trachomatis and Neisseria Gonorrhoeae Infections- Coinfection with C.
Trachomatis often occurs in patients infected with N. gonorrhoeae.
The patient is assessed for:
Fever
Discharge (urethral, vaginal, or rectal)
Signs of arthritis
UTI
Vaginitis
Trichomoniasis is a common sexually transmitted infection caused by a flagellated
protozoon.
Signs and symptoms include:
Vaginal discharge that is thin, yellow to yellow-green, malodorous, and very
irritating
Vulvitis which results to vulvovaginal burning and itching
Assess for odor of discharge
Human Papillomavirus is a type of virus that can cause abnormal tissue growth (for
example, warts) and other changes to cells. Infection for a long time with certain types
of human papillomavirus can cause cervical cancer.
Genital warts (condylomata) grows on the skin of vulva, vagina, cervix, or anus.
Herpes Virus Type 2 Infection is a recurrent and lifelong viral infection that can cause
herpetic lesions on the external genitalia and occasionally the vagina and cervix.
Itching and pain
Red and edematous (infected area)
Macules and papules at first and may progress to vesicles and blisters mostly in
the labia. Although cervix, vagina and perianal skin may be affected
Inguinal nodes are enlarged
Human Immune Deficiency Virus and Acquired Immune Deficiency Syndrome
After contracting HIV, the immune system mounts a response to the virus.
Signs and symptoms may include:
Fatigue
Headaches
A low-grade fever
Coughing
Sneezing
A runny nose or congestion
The symptoms above usually appear 2–6 weeks after contracting HIV, and they can last
anywhere from a week to a month.
These symptoms can resemble those of a cold or flu, so a person may not initially
associate them with HIV.
Many symptoms of an acute HIV infection are common in males and females. However,
some women may experience other symptoms, including:
Swollen lymph nodes- Can be one of the earliest symptoms of HIV, after those of
an acute infection.
Following an acute HIV infection, the virus continues to multiply, but at a slower rate. A
person may or may not have symptoms.
4. What are six nursing responsibilities associated with the management of a patient
who is newly diagnosed with an STD?
Increasing knowledge of the patient
Preventing spread of disease
Reducing anxiety
Increasing adherence
Monitoring potential complications
Managing potential complications
5. The patient is reluctant to disclose the names of sexual partners or talk about
partners. What could the nurse do?
By individualizing education, factual information applied to specific needs may
offer reassurance
Explain that patient may need help in planning discussion with partner
If the patient is especially apprehensive about this aspect, referral to a social
worker or other specialist may be appropriate
6. The patient is diagnosed with Gonorrhea. What should be included in the patient
education material? What are your nursing interventions?
Discuss feelings and concerns about the diagnosis of gonorrhea. Stress that such a
diagnosis does not reflect on one’s self-worth as a person
Directions for taking medication and what to do about potential side
effects.
Reinforce the importance of abstinence
Educate limiting the number of sexual partners
Educate patient on how to talk with a future sexual partner about condom use
7. What should the nurse include in the patient teaching for a patient who was
prescribed oral antibiotics?
It is important to take all of the medication prescribed to cure gonorrhea.
Do not stop antibiotic unless told by the physician
Finish all course of antibiotic prescribed by the physician
If there is reoccurrence, mostly it is not associated with failure of the medicine
but a reinfection.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Chronic Kidney Disease Case PresentationDocument14 pagesChronic Kidney Disease Case PresentationEmi EspinoNo ratings yet
- Assessment of Digestive and Gi FunctionDocument3 pagesAssessment of Digestive and Gi FunctionEmi EspinoNo ratings yet
- Conceptual Phase: Presented byDocument16 pagesConceptual Phase: Presented byEmi EspinoNo ratings yet
- Chapter 47-48Document6 pagesChapter 47-48Emi EspinoNo ratings yet
- Espino-Self Expression ExercisesDocument2 pagesEspino-Self Expression ExercisesEmi EspinoNo ratings yet
- Workbook-Chap 43-46Document11 pagesWorkbook-Chap 43-46Emi EspinoNo ratings yet
- NCP - Drug Study - Peptic UlcerDocument18 pagesNCP - Drug Study - Peptic UlcerEmi EspinoNo ratings yet
- Espino-Renal Replacement TherapyDocument5 pagesEspino-Renal Replacement TherapyEmi EspinoNo ratings yet
- Espino Rle Discussion TopicsDocument7 pagesEspino Rle Discussion TopicsEmi EspinoNo ratings yet
- Conceptual LiteratureDocument3 pagesConceptual LiteratureEmi EspinoNo ratings yet
- ESPINO RESEACH My Personal EvaluationDocument2 pagesESPINO RESEACH My Personal EvaluationEmi EspinoNo ratings yet
- Case ReadingDocument3 pagesCase ReadingEmi EspinoNo ratings yet
- Participants Risk and BenefitsDocument4 pagesParticipants Risk and BenefitsLester DananNo ratings yet
- Respondents InstrumentationDocument1 pageRespondents InstrumentationEmi EspinoNo ratings yet
- The Role of Technology in The Medication Use ProcessDocument20 pagesThe Role of Technology in The Medication Use ProcessEmi EspinoNo ratings yet
- Aplastic AnemiaDocument14 pagesAplastic AnemiaEmi EspinoNo ratings yet
- TonsillitisDocument8 pagesTonsillitisEmi EspinoNo ratings yet
- TonsillitisDocument8 pagesTonsillitisEmi EspinoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Inherited Metabolic Disorders Are Genetic Conditions That Result in Metabolism ProblemsDocument10 pagesInherited Metabolic Disorders Are Genetic Conditions That Result in Metabolism ProblemsLance CornistaNo ratings yet
- Respiratory AlkalosisDocument4 pagesRespiratory Alkalosismardsz100% (1)
- Health and Illness: Lingua House Lingua HouseDocument4 pagesHealth and Illness: Lingua House Lingua Housemaria maltsevaNo ratings yet
- Mufrodat Fil MusytasyfaDocument3 pagesMufrodat Fil MusytasyfaNenazNaziahNo ratings yet
- Thalassaemia: Dr. Ruwanka de LiveraDocument30 pagesThalassaemia: Dr. Ruwanka de LiveraAshan BopitiyaNo ratings yet
- Long COVID19 Syndrome ADocument19 pagesLong COVID19 Syndrome Arbatjun576No ratings yet
- Drug-Induced Sleepiness and Insomnia: An Update: Sonolência e Insônia Causadas Por Drogas: Artigo de AtualizaçãoDocument8 pagesDrug-Induced Sleepiness and Insomnia: An Update: Sonolência e Insônia Causadas Por Drogas: Artigo de AtualizaçãoRene FernandesNo ratings yet
- 21 Facts About Vincent Van GoghDocument7 pages21 Facts About Vincent Van GoghSairah Quen AjenoNo ratings yet
- Imse Trans Lab 8Document7 pagesImse Trans Lab 8ela kikayNo ratings yet
- No. 6 Canuel vs. MagsaysayDocument2 pagesNo. 6 Canuel vs. Magsaysayapplegee liboonNo ratings yet
- Types of CancerDocument10 pagesTypes of CancerStudies 123No ratings yet
- Diseases Caused by MicroorganismsDocument9 pagesDiseases Caused by MicroorganismsKhushbuGuptaNo ratings yet
- BSBMED301: Assessment 1: What You Have To DoDocument8 pagesBSBMED301: Assessment 1: What You Have To DoPrayas AmatyaNo ratings yet
- Donning Doffing Dressing 1Document1 pageDonning Doffing Dressing 1api-556139355No ratings yet
- Review Paper Adenanthera Pavonina PavoninaDocument13 pagesReview Paper Adenanthera Pavonina PavoninaABDUL RUB NAAZNo ratings yet
- Infectious Diseases of The Dog and CatDocument329 pagesInfectious Diseases of The Dog and CatPetrisor GheorghiuNo ratings yet
- IMCIDocument15 pagesIMCIJoan MedinaNo ratings yet
- Fever in ICU ReviewDocument15 pagesFever in ICU ReviewAndrés Salazar MolinaNo ratings yet
- Candida Special ReportDocument12 pagesCandida Special ReportRxOuzo100% (1)
- Neurological Assessment PDFDocument52 pagesNeurological Assessment PDFJosephine George JojoNo ratings yet
- 8 - Autoimmune DiseasesDocument20 pages8 - Autoimmune Diseasesvirag.patilNo ratings yet
- Nursing 2020 1.3 Plasma ProteinsDocument20 pagesNursing 2020 1.3 Plasma ProteinsYogesh NerkarNo ratings yet
- Geriatric Otolaryngolo GY: DR Surya Prakash D R Associate Professor of Ent Ramaiah Medical CollegeDocument51 pagesGeriatric Otolaryngolo GY: DR Surya Prakash D R Associate Professor of Ent Ramaiah Medical CollegeSurya Prakash D RNo ratings yet
- Peta PWSDocument1 pagePeta PWSPUSKESMAS PLANTUNGAN KDLNo ratings yet
- 01 Jan IncompleteDocument123 pages01 Jan IncompleteDia DimayugaNo ratings yet
- By: Kinjal Banerjee SU-6Document40 pagesBy: Kinjal Banerjee SU-6Dr Ari SembiringNo ratings yet
- Physical, Ergonomic and Psychosocial HazardsDocument64 pagesPhysical, Ergonomic and Psychosocial HazardsPatricia GalorioNo ratings yet
- Hypertension HSE Presentation HSE FormatsDocument18 pagesHypertension HSE Presentation HSE FormatsasepNo ratings yet
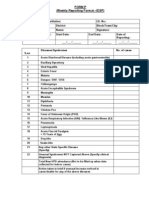
- IDSP P&L FormsDocument2 pagesIDSP P&L FormsKunal YadavNo ratings yet
- Multiple Mini-Stations Interviews: (Mmis) GuideDocument27 pagesMultiple Mini-Stations Interviews: (Mmis) Guidesandra abboudNo ratings yet