Professional Documents
Culture Documents
Lanjutan Strengtening
Uploaded by
'fanny Quenhita'Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lanjutan Strengtening
Uploaded by
'fanny Quenhita'Copyright:
Available Formats
1 Bennie
Bennie et alet/ al
Am / Am J Prev
J Prev MedMed 2018;55(6):864
2018;55(6):864 − 874
− 874 1
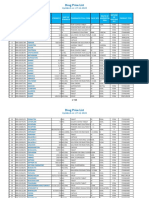
Table 2. Proportions Reporting MSE ≥ 2 Times/Week and AORs a for Meeting the Recommendations ( continued)
Met MSE recommendations ( ≥ 2 times/week) Weighted % b ( 95%
Characteristics n CI) AOR a( 95 % CI)
Fair 52,953 18.3 (17.6, 19.0) 0.50 (0.46, 0.53)
Poor 20,664 14.7 (13.8, 15.7) 0.45 (0.41, 0.50)
Smoking status
Current (daily) 40,236 21.1 (20.3, 21.9) 0.72 (0.68, 0.76)
Current (some days) 16,440 30.5 (29.1, 31.8) 0.99 (0.91, 1.07)
Former smoker 114,649 28.5 (28.0, 29.1) 1.03 (0.99, 1.07)
Never smoked 223,858 32.6 (29.9, 30.5) 1.00 (ref)
Note: Boldface indicates statistical signi fi cance ( p< 0.05).
a Adjusted for all other explanatory variables in the table.
bData weighted using stratum weight provided by the Centers for Disease Control and Prevention. 57 c To meet the aerobic recommendations a respondent had to report ≥ 150 moderate-intensity
minutes/week or ≥ 75 vigorous-intensity minutes/week or an equivalent combination of both.
MSE, muscle-strengthening exercise.
The ORs ranged from 0.70 (95% CI=0.67,0.73) for very good to DISCUSSION
0.45 (95% CI=0.41, 0.50) among those reporting poor health. The key fi nding is that among approximately 400,000
Compared with never smokers, current daily smokers had 28% lower U.S. adults, more than half do not engage in MSE. Considering the independent
odds of meeting the MSE recommendations. health bene fi ts associated with MSE, 58 the current fi ndings are concerning from
a public health perspective. Another key fi nding
After adjusting for potential confounders (e.g., age, sex, aerobic is that MSE was independently associated with lower odds of
MVPA, smoking, BMI), compared with those who did no MSE, no prevalent diabetes, obesity, and cancer (non-skin), although dose − response was not
frequencies were associated with a lower risk of coronary heart disease ( always evident.
Figure 1 ). For diabetes, there was a U-shaped association, with the
lowest odds among those reporting MSE This study showed a similar MSE prevalence to previous U.S. data.
three to four times/week (OR=0.69, 95% CI=0.63, 0.76). Only those Data from BRFSS 2011 estimated that
reporting MSE either one (OR=0.91, 95% CI=0.83, 0.99) or two 29.3% of U.S. adults met the MSE recommendations, 44
times/week (OR=0.89, 95% CI=0.81, 0.98) had lower odds of a cancer (0.9% lower than prevalence estimates), suggesting that MSE levels among
(non-skin) diagnosis (data are shown in U.S. adults appear to be stable over 4 years (2011 − 2015).
Similar MSE levels have been observed in the United Kingdom, 45 whereas lower
levels are reported among Australian 28,43 and Finnish adults 42
Appendix Table 1 , available online).
Compared with those who did no MSE, there were reduced odds of
(range, 10% − 20%). Interestingly, one study in the U.S. estimated
reporting poor self-rated health across all MSE frequencies (Table 3). The
approximately 6% of the population met the MSE recommendations. 59 In this
ORs showed a Ushaped association, with a relative increase in
study, among 4,000 adults, not only was frequency of MSE assessed, but in
the odds among those reporting the highest MSE frequency ( fi ve or more
accordance with the U.S. guidelines, 7 all seven major muscle groups had to be
times/week). There was a linear decrease in the odds of being classi fi ed
targeted (i.e., shoulders, arms, back, chest, abdomen, legs, and hips). 59
obese across all MSE frequencies. This ranged from 24% among those
Discordance in prevalence estimates suggest the need to test the validity of MSE
reporting MSE one time/week to 44% among those reporting fi ve or more
instruments used in surveillance studies.
times/week.
The sociodemographic and lifestyle-related MSE correlates observed in
the present study were generally consistent with previous studies. Others
For stroke, there was no signi fi cant change in odds among those
identify that females, older adults, not meeting the aerobic
reporting lower MSE frequencies. However, among the
recommendations, being obese/overweight, lower income/education, and
highest frequency there were 19% increased odds. When strati fi ed by sex,
smoking are inversely associated with
age, and BMI, the increased odds remained signi fi cant only for those with
meeting MSE recommendations. 28,42 , 43,45 These fi ndings underscore the
a BMI classi fi ed as obese (OR=1.30, 95% CI=1.03,
importance of targeting these population
1.63; Appendix Table 2 , available online).
December 2018 www.ajpmonline.org
2 Bennie
Bennie et alet/ al
Am / Am J Prev
J Prev MedMed 2018;55(6):864
2018;55(6):864 − 874
− 874 2
Figure 1. AORs for adverse health outcomes according to muscle-strengthening exercise (times/week) (reference=0 times/week) among 2015 Behavioral Risk Factor
Surveillance System sample ( n= 397,423). Bars, 95% CI.
Note: Data are shown in Appendix 1 (available online).
a Adjusted for sex, age, race/ethnicity, employment, education, income, moderate-to-vigorous intensity aerobic activity, smoking, and BMI.
b Adjusted for sex, age, race/ethnicity, employment, education, income, moderate-to-vigorous intensity aerobic activity, and smoking.
c To be classi fi ed as being diagnosed with coronary heart disease, diabetes, stroke, or cancer (non-skin) a respondent had to report having a “ doctor, nurse or other health professional ” diagnose
each condition.
d Self-rated health and BMI based on self-report.
subgroups in future MSE public health interventions. In particular, related activities (e.g., push-ups, squats, sit-ups, and lunges). 60 Last,
because the lowest odds for meeting the MSE recommendations were negative social norms associated with MSE might be impeding its uptake,
observed among older adults, community-based interventions should speci fi as this activity might be associated with excessive muscle
cally target this population subgroup. The fi ndings on MSE levels across gain, risk of injury, and hyper-masculine settings (e.g., gymnasiums). 57
, 60 − 62
different racial groups was somewhat surprising. For example, in contrast to
research on correlates of aerobic MVPA, this study showed that black, non- To address these complex MSE promotion issues, a coordinated social
23 ecologic approach is warranted. 63
Hispanics and multiracial,
Potential concurrent public health strategies based on limited research may
non-Hispanics were more likely to meet the MSE guidelines, when
include some of the following approaches: increasing the availability of
compared with white adults. These fi ndings are suggestive that MSE
MSE equipment for home-based activity (e.g., resistance bands, barbells),
might be a particularly popular activity among non-white population
64 establishing affordable/attractive spaces to perform MSE (e.g., fi tness
subgroups. This could be important for future MSE interventions that
centers, apparatuses in open community spaces), 65,66 use of behavior-
target currently inactive black and multiracial populations.
change science techniques to understand how different activities suit
different groups, 67 public access to professionals who have skills in
prescribing and teaching MSE (e.g., strength coaches/ fi tness instructors),
Compared with BRFSS 2015 respondents who reported no aerobic MVPA
68 mass media campaigns endorsing MSE as important for overall physical
(24.6%), more than twice as many respondents reported no MSE (57.8%).
activity and health, and challenging the negative social norms sometimes
Public health action is warranted to support MSE uptake/adherence.
associated with this activity. 69
However, contrasted with MVPA, MSE has unique health promotion
challenges. First, MSE requires a rudimentary understanding of speci fi c
nomenclature (e.g., sets, repetitions, large muscle groups) and access to some
basic equipment (e.g., resistance bands, dumbbells). 10 Second, this behavior Strengths of this study include the use of a large, nationally
requires self-ef fi cacy to perform MSE- representative sample of U.S. adults. Moreover, MSE levels were
examined across a wide variety of sociodemographic and
lifestyle-related categories.
Additionally, the use of standardized data collection makes it
possible to compare fi ndings to future BRFSS results.
Limitations
December 2018 www.ajpmonline.org
3 Bennie
Bennie et alet/ al
Am / Am J Prev
J Prev MedMed 2018;55(6):864
2018;55(6):864 − 874
− 874 3
Given the cross-sectional design, the authors are cautious in drawing
are now needed to con fi rm the preliminary fi ndings on the
strong inferences from the associations observed between MSE and
association between weekly frequency of MSE and health
adverse health conditions. Notwithstanding this limitation, apart from
outcomes. Another limitation was the use of a single self-report item
stroke, when compared with those who did none, any MSE participation
assessing weekly MSE frequency. Although the item has
was generally associated with lower odds for a set of common adverse
acceptable reliability, 51 the
health outcomes. However, the U-shape association for diabetes, cancer,
authors are unable to eliminate the possibility of selfreport bias, which
and poor self-rated heath suggests that low-to-moderate MSE frequencies
may have led to overestimation of MSE in the present study. Because
might be more effective in reducing the risk of these
MSE duration and intensity were not assessed, the authors are unable
adverse health conditions. Potential explanations may be the
to determine how these might have in fl uenced the adverse health
pathophysiologic consequences associated with chronic MSE
conditions. Last, MSE was unlikely to be captured during gardening,
overtraining (e.g., chronic in fl ammation, immunosuppression, and
yard work, or laboring. However, given that over the past 50 years
musculoskeletal discomfort/pain). 70 For obesity, there was an inverse
technologic advancements have resulted in a decline in energy
linear association between this outcome and MSE. Longitudinal
expenditure within household/occupational domains, 71 it is unlikely
evidence has shown a linear dose
that many adults engage in suf fi cient MSE within these contexts.
− repose relationship between minutes per week spent in MSE and
reduction in gain in waist circumference among approximately 10,000
healthy males. 36
CONCLUSIONS
Somewhat surprising were the fi ndings that the highest MSE
frequency ( fi ve or more times/week) was associated with an More than half of U.S. adults do not engage in MSE. For maximal
increased odds of stroke. This might be explained by the increased public health bene fi ts, effort should be made to enable greater
risk of arterial stiffness 40 and hypertension among speci fi c populations proportions of the population to increase their involvement in MSE.
who engage in high levels/intensity of MSE (e.g., athletes). 41 Moreover, a Comprehensive public health strategies are needed to promote
recent prospective study of approximately 30,000 older women showed a population-level MSE uptake/adherence. Future MSE public health
reverse J-shaped nonlinear association between MSE and interventions should target older adults, females, and those with low
all-cause mortality. 37 In the strati fi ed analyses, the increased risk of education/income.
stroke remained solely among the obese, suggesting caution in
encouraging high levels of MSE among this group. Nevertheless, because
most adults do no MSE, it is unlikely that too much MSE poses a signi fi ACKNOWLEDGMENTS
cant public health risk. Regardless, future interventions should promote We thank all 2015 Behavioral Risk Factor Surveillance System participants for their
generous contributions. We thank Taryn Axelsen from USQ Statistical Consulting
low-to-moderate MSE participation levels, as Unit for her initial advice on the data analysis.
opposed to high levels.
No fi nancial disclosures were reported by the authors of this paper.
A key limitation was the cross-sectional design restricting the SUPPLEMENTAL MATERIAL
possibility of inferring causality. The authors are unable to rule out
Supplemental materials associated with this article can be found in the online
reverse causality, for example, the reduced odds of adverse health
version at https://doi.org/10.1016/j. amepre.2018.07.022 .
outcomes may be because of the fact that individuals with health
conditions are less likely to participate in exercise, including MSE.
Alternatively, it might be possible that those with existing health
conditions could engage in MSE more frequently than those REFERENCES
without such conditions, potentially because their health 1. WHO. Global Status Report on Noncommunicable Diseases. Geneva,
Switzerland: WHO, 2014.
complications motivate them to do so (e.g., rehabilitation for 2. National Center for Health Statistics. Health, United States, 2016: With
Chartbook on Long-term Trends in Health. Hyattsville, MD: National Center for Health
diabetes, cancer, stroke). Future studies with prospective designs Statistics, 2017.
3. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical
inactivity on major non-communicable diseases worldwide: an analysis of burden of
disease and life expectancy. Lancet. 2012;380(9838):219 – 229. https://doi.org/10.1016/S0140-6736(12)
61031-9 .
December 2018 www.ajpmonline.org
4 Bennie
Bennie et alet/ al
Am / Am J Prev
J Prev MedMed 2018;55(6):864
2018;55(6):864 − 874
− 874 4
4. WHO. Global Health Risks: Mortality and Burden of Disease Attribut- 23. Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW. Correlates of physical
able to Selected Major Risks. Geneva, Switzerland: WHO, 2009. activity: why are some people physically active and others not? Lancet. 2012;380(9838):258
5. Oja P, Titze S. Physical activity recommendations for public health: development and policy context. – 271. https://doi.org/10.1016/ S0140-6736(12)60735-1 .
EPMA J. 2011;2(3):253 – 259. https:// doi.org/10.1007/s13167-011-0090-1 .
24. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity
6. Australian Government Department of Health. Australia ’ s Physical Activ- levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247 – 257. https://doi.org/10
ity & Sedentary Behaviour Guidelines for Adults (18 − 64 years). Canberra, Australia: .
Australian Government Department of Health, 2014.
7. HHS. 2008 Physical Activity Guidelines for Americans. Washington, DC:
25. Sallis J, Owen N. Physical Activity and Behavioral Medicine. Thousand
HHS, 2008.
8. UKK Institute. UKK Institute ’ s Physical Activity Pie. www.ukkinsti- Oaks, CA: Sage Publications, 1999.
tuutti. fi/fi lebank/64-physical_activity_pie.pdf . Published 2016. 26. Sallis JF, Hovell MF. Determinants of exercise behavior. Exerc Sport
Accessed September 20, 2018. Sci Rev. 1990;18(1):307 – 330. https://doi.org/10.1249/00003677-
199001000-00014 .
9. WHO. Global Recommendations on Physical Activity for Health.
Geneva, Switzerland: WHO, 2010. 27. Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults ’ participation in
physical activity: review and update. Med Sci Sports
10. American College of Sports Medicine. American College of Sports Medicine position stand.
Exerc. 2002;34(12):1996 – 2001. https://doi.org/10.1097/
Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2009;41(3):687 00005768-200212000-00020 .
− 708. https://doi. org/10.1249/MSS.0b013e3181915670 . 28. Bennie JA, Pedisic Z, van Uffelen JGZ, et al. Pumping iron in Australia: prevalence, trends and
sociodemographic correlates of muscle strengthening activity participation from a
11. Lavie CJ, Arena R, Swift DL, et al. Exercise and the cardiovascular system: clinical science national sample of 195,926 adults. PLoS One. 2016;11(4):e0153225. https://doi.org/10.1371/journal.pone
and cardiovascular outcomes. Circ Res. 2015;117 (2):207 – 219. https://doi.org/10.1161/CIRCRESAHA..117.305205
.
12. Hardee JP, Porter RR, Sui X, et al. The effect of resistance exercise on all-cause mortality 29. Brown WJ, Bauman AE, Bull FC, Burton NW. Development of evidence-based physical
in cancer survivors. Mayo Clin Proc. 2014;89 (8):1108 – 1115. https://doi.org/10.1016/j.mayocp.2014.03a.c0t1iv8ity recommendations for adults (18 − 64 years): report prepared for the Australian
. Government Department of Health, August 2012. https://www.health.gov.au/internet/main/publishing.nsf/c
13. IR Lemes, PH Ferreira, Linares SN, Machado AF, Pastre CM, Netto J. Resistance training reduces DEB-PAR-Adults-18-64years.pdf . Published 2013. Accessed September 20, 2018.
systolic blood pressure in metabolic syndrome: a systematic review and
meta-analysis of randomised controlled trials. Br J Sports Med. 2016;50(23):1438 – 1442. https://doi.org/
10.1136/bjsports-2015-094715 . 30. Artero EG, D-c Lee, Lavie CJ, et al. Effects of muscular strength on cardiovascular risk
14. Schoenfeld BJ, Ogborn D, Krieger JW. Dose-response relationship between weekly resistance factors and prognosis. J Cardiopulm Rehabil Prev.
training volume and increases in muscle mass: a systematic review and
2012;32(6):351 – 358. https://doi.org/10.1097/HCR.0b013e3182642688 .
meta-analysis. J Sports Sci. 2017;35 (11):1073 – 1082. https://doi.org/10.1080/02640414.2016.123110.1D9a7nkel SJ, Loenneke JP, Loprinzi PD. Dose-dependent association between
. muscle-strengthening activities and all-cause mortality: prospective cohort study among a national
15. Strasser B, Siebert U, Schobersberger W. Resistance training in the treatment of the metabolic sample of adults in the USA.
syndrome: a systematic review and metaanalysis of the effect of resistance training on Arch Cardiovasc Dis. 2016;109(11):626 – 633. https://doi.org/10.1016/j. acvd.2016.04.005 .
metabolic clustering in patients with abnormal glucose metabolism. Sports Med. 2010;40
(5):397 – 415. https://doi.org/10.2165/11531380-000000000-00000 .
32. Kraschnewski JL, Sciamanna CN, Poger JM, et al. Is strength training associated with
mortality bene fi ts? A 15 year cohort study of U.S. older adults. Prev Med. 2016;87:121 – 127.
16. Bakker EA, Lee DC, Sui X, et al. Association of resistance exercise with the incidence of https://doi.org/10.1016/j.
hypercholesterolemia in men. Mayo Clin Proc. ypmed.2016.02.038 .
2018;93(4):419 – 428. https://doi.org/10.1016/j.mayocp.2017.11.024 . 33. Stamatakis E, Lee I-M, Bennie JA, et al. Does strength promoting exercise confer unique health
17. Martyn-St James M, Carroll S. A meta-analysis of impact exercise on postmenopausal bone bene fi ts? A pooled analysis of eleven population cohorts with all-cause, cancer,
loss: the case for mixed loading exercise programmes. Br J Sports Med. 2009;43(12):898 – 908. and cardiovascular mortality endpoints. Am J Epidemiol. 2018;187(5):1102 – 1112. https://doi.org/
https://doi.org/
10.1136/bjsm.2008.052704 .
18. Martyn-St James M, Carroll S. Effects of different impact exercise modalities on bone 10.1093/aje/kwx345 .
mineral density in premenopausal women: a meta-analysis. J Bone Metab. 2010;28(3):251 34. Grontved A, Rimm EB, Willett WC, Andersen LB, Hu FB. A prospective study of weight
– 267. https://doi.org/ training and risk of type 2 diabetes mellitus in men. Arch Intern Med. 2012;172(17):1306 – 1312.
10.1007/s00774-009-0139-6 . https://doi.org/
10.1001/archinternmed.2012.3138 .
19. Cj Liu, NK Latham. Progressive resistance strength training for improving physical function in older
adults. Cochrane Database Syst Rev. 35. Grontved A, Pan A, Mekary RA, et al. Muscle-strengthening and conditioning activities and
risk of type 2 diabetes: a prospective study in two cohorts of U.S. women. PLoS Med. 2014;11(1):e10015 https://
2009;3:CD002759. https://doi.org/10.1002/14651858.CD002759.pub2 .
doi.org/10.1371/journal.pmed.1001587 .
20. Mangione KK, Miller AH, Naughton IV. Cochrane review: improving physical function and
performance with progressive resistance strength training in older adults. Phys Ther. 2010;90(12):3167.1M1ekary RA, Grùntved A, Despres J-P, et al. Weight training, aerobic physical activities, and
– 1715. long-term waist circumference change in men.
https://doi.org/10.2522/ptj.20100270 . Obesity. 2015;23(2):461 – 467. https://doi.org/10.1002/oby.20949 .
21. Gordon BR, McDowell CP, Lyons M, Herring MP. The effects of resistance exercise training 37. Kamada M, Shiroma EJ, Buring JE, Miyachi M, Lee IM. Strength training and all-cause,
on anxiety: a meta-analysis and meta-regression analysis of randomized controlled trials. Sports cardiovascular disease, and cancer mortality in older women: a cohort study. J Am Heart Assoc.
Med. 2017;47 (12):2521 – 2532. https://doi.org/10.1007/s40279-017-0769-0 . 2017;6(11):e007677. https:// doi.org/10.1161/JAHA.117.007677 .
22. O ’ Connor PJ, Herring MP, Caravalho A. Mental health bene fi ts of strength 38. Shiroma EJ, Cook NR, Manson JE, et al. Strength training and the risk of type 2 diabetes and
training in adults. Am J Lifestyle Med. 2010;4(5):377 – 396. cardiovascular disease. Med Sci Sports Exerc.
https://doi.org/10.1177/1559827610368771 . 2017;49(1):40 – 46. https://doi.org/10.1249/MSS.0000000000001063 .
December 2018 www.ajpmonline.org
5 Bennie
Bennie et alet/ al
Am / Am J Prev
J Prev MedMed 2018;55(6):864
2018;55(6):864 − 874
− 874 5
39. Bakker EA, Lee DC, Sui X, et al. Association of resistance exercise, independent of and 56. Ng SP, Korda R, Clements M, et al. Validity of self-reported height and weight and derived
combined with aerobic exercise, with the incidence of metabolic syndrome. Mayo Clin body mass index in middle-aged and elderly individuals in Australia. Aust N Z J Public
Proc. 2017;92(8):1214 – 1222. Health. 2011;35(6):557 – 563.
https://doi.org/10.1016/j.mayocp.2017.02.018 . https://doi.org/10.1111/j.1753-6405.2011.00742.x .
40. Miyachi M. Effects of resistance training on arterial stiffness: a metaanalysis. Br J Sports 57. Dworkin SL. “ Holding back ”: negotiating a glass ceiling on women ’ s
Med. 2013;47(6):393 – 396. https://doi.org/10.1136/ bjsports-2012-090488 . muscular strength. Sociol Perspect. 2001;44(3):333 – 350. https://doi.
org/10.1525/sop.2001.44.3.333 .
58. Westcott WL. Resistance training is medicine: effects of strength training on health. Curr
41. Karpinos AR, Roumie CL, Nian H, Diamond AB, Rothman RL. High prevalence of
Sports Med Rep. 2012;11(4):209 – 216. https://doi. org/10.1249/JSR.0b013e31825dabb8 .
hypertension among collegiate football athletes. Circ Cardiovasc Qual Outcomes. 2013;6(6):716
– 723. https://doi.org/
10.1161/CIRCOUTCOMES.113.000463 . 59. Loustalot F, Carlson SA, Kruger J, Buchner DM, Fulton JE. Musclestrengthening activities
42. Bennie JA, Pedisic Z, Suni JH, et al. Self-reported health-enhancing physical activity and participation among adults in the United States. Res Q Exerc Sport. 2013;84(1):30 – 38.
recommendation adherence among 64,380 Finnish adults. Scand J Med Sci Sports. 2017;27(12):1842 https://doi.org/10.1080/
– 1853. https://doi.org/ 02701367.2013.762289 .
10.1111/sms.12863 . 60. Rhodes RE, Lubans DR, Karunamuni N, Kennedy S, Plotnikoff R. Factors associated with
43. Bennie JA, Pedisic Z, Van Uffelen JG, et al. The descriptive epidemiology of total physical activity, participation in resistance training: a systematic review. Br J Sports Med. 2017;51(20):1466
muscle-strengthening exercises and sedentary behaviour among Australian adults — results from the – 1472. https://doi.org/
National Nutrition and Physical Activity Survey. BMC Public Health. 10.1136/bjsports-2016-096950 .
61. Phillips SM, Winett RA. Uncomplicated resistance training and health-related outcomes:
2016;16:73. https://doi.org/10.1186/s12889-016-2736-3 . evidence for a public health mandate. Curr Sports Med Rep. 2010;9(4):208 – 213. https://doi.org/10.1249/
44. CDC. Adult participation in aerobic and muscle-strengthening physical activities − United
States, 2011. MMWR Morb Mortal Wkly Rep. JSR.0b013e3181e7da73 .
2013;62(17):326 − 330. 62. Howe HS, Welsh TN, Sabiston CM. The association between gender role stereotypes,
45. Strain T, Fitzsimons C, Kelly P, Mutrie N. The forgotten guidelines: cross-sectional analysis of resistance training motivation, and participation. Psychol Sport Exerc. 2017;33:123 – 130. https://doi.org/10.1
participation in muscle strengthening and balance & co-ordination activities by adults
and older adults in Scotland. BMC Public Health. 2016;16(1):1108. https://doi.org/10.1186/
s12889-016-3774-6 . chsport.2017.08.006 .
63. Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach
to creating active living communities. Annu Rev Public Health. 2006;27:297 – 322. https://doi.org/10.1146/ann
46. CDC. 2015 BRFSS Survey Data and Documentation. www.cdc.gov/
brfss/annual_data/annual_2015.html . Accessed 2017.
47. CDC. Behavioral Risk Factor Surveillance System. www.cdc.gov/brfss/ publhealth.27.021405.102100 .
index.html . Accessed 2017. 64. Harada K, Oka K, Shibata A, et al. Strength-training behavior and perceived environment among
48. CDC. Overview: BRFSS 2015. www.cdc.gov/brfss/annual_data/2015/ Japanese older adults. J Aging Phys Act.
pdf/overview_2015.pdf . Published 2016. Accessed 2017. 2011;19(3):262 – 272. https://doi.org/10.1123/japa.19.3.262 .
49. CDC. 2015 Summary Data Quality Report. www.cdc.gov/brfss/annu- 65. Beedie C, Mann S, Jimenez A. Community fi tness center-based physi-
al_data/2015/pdf/2015-sdqr.pdf . Published 2015. Accessed 2017. cal activity interventions: a brief review. Curr Sports Med Rep. 2014;13 (4):267 – 274. https://doi.org/10.1249/J
50. CDC. 2015 Codebook Report. www.cdc.gov/brfss/annual_data/2015/ .
pdf/codebook15_llcp.pdf . Published 2016. Accessed 2017. 66. Schroeder EC, Welk GJ, Franke WD, Lee D-c. Associations of health club membership with physical
activity and cardiovascular health.
51. Yore MM, Ham SA, Ainsworth BE, et al. Reliability and validity of the instrument used in
PLoS One. 2017;12(1):e0170471. https://doi.org/10.1371/journal.
BRFSS to assess physical activity. Med Sci Sports Exerc. 2007;39(8):1267 – 1274. https://doi.org/10.12p4o9n/e.0170471 .
mss.0b013e3180618bbe . 67. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for
characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. https://doi.org/10.11
52. Dankel SJ, Loenneke JP, Loprinzi PD. The individual, joint, and additive interaction associations 1748-5908-6-42 .
of aerobic-based physical activity and muscle strengthening activities on
metabolic syndrome. Int J Behav Med. 2016;23(6):707 – 713. https://doi.org/10.1007/s12529016-96587. 0M-yazzetti SA, Kraemer WJ, Volek JS, et al. The in fl uence of direct
. supervision of resistance training on strength performance. Med Sci Sports
Exerc. 2000;32(6):1175 – 1184. https://doi.org/10.1097/
53. Cheng YJ, Gregg EW, De Rekeneire N, et al. Muscle-strengthening activity and its 00005768-200006000-00023 .
association with insulin sensitivity. Diabetes Care. 69. Abioye AI, Hajifathalian K, Danaei G. Do mass media campaigns improve physical activity?
2007;30(9):2264 – 2270. https://doi.org/10.2337/dc07-0372 . A systematic review and meta-analysis. Arch Public Health. 2013;71(1):20. https://doi.org/10.1186/0778-7367
54. Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and .
non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 70. Lavallee ME, Balam T. An overview of strength training injuries: acute and chronic. Curr
30.3 million participants. BMJ. Sports Med Rep. 2010;9(5):307 – 313. https://doi.org/
2016;353:i2156. https://doi.org/10.1136/bmj.i2156 . 10.1249/JSR.0b013e3181f3ed6d .
55. Gander J, D-c Lee, Sui X, Hebert JR, Hooker SP, Blair SN. Self-rated health status and cardiorespiratory 71. Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 decades in U.S.
fi tness as predictors of mortality in men. Br J Sports Med. 2011;45(14):1095 occupation-related physical activity and their associations with obesity. PLoS One. 2011;6(5):e19657.
– 1100. https://doi.org/ https://doi.org/10.1371/journal. pone.0019657 .
10.1136/bjsm.2010.079855 .
December 2018 www.ajpmonline.org
You might also like
- The Management of Metastatic Triple-Negative Breast Cancer: An Integrated and Expeditionary ApproachFrom EverandThe Management of Metastatic Triple-Negative Breast Cancer: An Integrated and Expeditionary ApproachNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 3: CardiologyFrom EverandComplementary and Alternative Medical Lab Testing Part 3: CardiologyRating: 1 out of 5 stars1/5 (1)
- Samuthpongtorn 2023 LD 230182 1694535872.81978Document4 pagesSamuthpongtorn 2023 LD 230182 1694535872.81978bgx67nnnkgNo ratings yet
- Nut Screening Assess FELANPE 2012Document35 pagesNut Screening Assess FELANPE 2012Marcio BatistaNo ratings yet
- Oncotarget 08 16755Document10 pagesOncotarget 08 16755Ruang GiriNo ratings yet
- Associations of Physical Activity and Depression Results From The IrishDocument8 pagesAssociations of Physical Activity and Depression Results From The IrishHargo PsyNo ratings yet
- Food Habits of Age GroupsDocument9 pagesFood Habits of Age GroupsMuhammad MujtabaNo ratings yet
- Research ArticleDocument7 pagesResearch ArticlentnquynhproNo ratings yet
- Cognitive Function Following Breast Cancer TreatmentDocument4 pagesCognitive Function Following Breast Cancer TreatmentFrancisco MartinezNo ratings yet
- Fueling The Obesity Epidemic Artificially Sweetened BeveragesDocument7 pagesFueling The Obesity Epidemic Artificially Sweetened BeveragesJOCELYN ACEVEDONo ratings yet
- Cancer-Related Fatigue: A Systematic and Meta-Analytic Review of Non-Pharmacological Therapies For Cancer PatientsDocument43 pagesCancer-Related Fatigue: A Systematic and Meta-Analytic Review of Non-Pharmacological Therapies For Cancer Patientsjohn chinNo ratings yet
- Predictors of Long-Term Weight Loss in Adults With Modest Initial Weight Loss, by Sex and RaceDocument9 pagesPredictors of Long-Term Weight Loss in Adults With Modest Initial Weight Loss, by Sex and RaceindilaNo ratings yet
- A New Predictive Equation For Resting Energy Expenditure in Healthy IndividualsıDocument7 pagesA New Predictive Equation For Resting Energy Expenditure in Healthy IndividualsıJames McVeighNo ratings yet
- Vaccine effectiveness case-control studyDocument4 pagesVaccine effectiveness case-control studyAdin RamadhanNo ratings yet
- Relationship Between Low Maternal Vitamin D Status and The Risk of Severe Preeclampsia: A Case Control StudyDocument10 pagesRelationship Between Low Maternal Vitamin D Status and The Risk of Severe Preeclampsia: A Case Control StudyCindy DelapazNo ratings yet
- Asmaa Resullt MD1Document31 pagesAsmaa Resullt MD1yasmenelsherif55No ratings yet
- MoroDocument5 pagesMoroRadom MicoNo ratings yet
- Nejmoa 2206038Document12 pagesNejmoa 2206038Juan David Arboleda LopezNo ratings yet
- Tirzepatide Once Weekly For The Treatment of Obesity Nejmoa2206038Document12 pagesTirzepatide Once Weekly For The Treatment of Obesity Nejmoa2206038Salah ArafehNo ratings yet
- Pergamon 0005-7967 (94) 00070-0: (Received 29 June 1994)Document5 pagesPergamon 0005-7967 (94) 00070-0: (Received 29 June 1994)Aggelou MayaNo ratings yet
- BDI Scores and Risk of Breast Disease and CancerDocument6 pagesBDI Scores and Risk of Breast Disease and CancerRenz MacionNo ratings yet
- A Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfilesDocument4 pagesA Comparative Analysis of Three Methods of Contraception: Effects On Blood Glucose and Serum Lipid ProfileshectorNo ratings yet
- Harrington 2012Document5 pagesHarrington 2012atleticar1No ratings yet
- JOURNAL OBGYN Management - of - Chronic - Hepatitis - B - During - PregnancyDocument7 pagesJOURNAL OBGYN Management - of - Chronic - Hepatitis - B - During - PregnancyLina UkagoNo ratings yet
- Antenatal 20steroids 20 E2 80 93 20saga 20continues 20finalDocument22 pagesAntenatal 20steroids 20 E2 80 93 20saga 20continues 20finalRahul BadhyaNo ratings yet
- A Descriptive Study To Assess The Morbidity Pattern Among Nurses With Special Reference To ObesityDocument9 pagesA Descriptive Study To Assess The Morbidity Pattern Among Nurses With Special Reference To ObesityEditor IJTSRDNo ratings yet
- Aspartamo y Obesidad PDFDocument7 pagesAspartamo y Obesidad PDFdocneiraNo ratings yet
- Examining The Associations Among Fibrocystic Breast Change, Total Lean Mass, and Percent Body FatDocument6 pagesExamining The Associations Among Fibrocystic Breast Change, Total Lean Mass, and Percent Body FatMichiko MeritasariNo ratings yet
- Analysis On Psychology Status of Patients With Diabetic Retinopathy During Preoperative Period and Its Influencing FactorsDocument4 pagesAnalysis On Psychology Status of Patients With Diabetic Retinopathy During Preoperative Period and Its Influencing FactorsChindy PutriNo ratings yet
- Comparing VariablesDocument82 pagesComparing VariablesSA NodeNo ratings yet
- Non-Specific Low Back PainDocument12 pagesNon-Specific Low Back PainSarah Naura IrbahNo ratings yet
- A Review of Basic BiostatisticsDocument7 pagesA Review of Basic BiostatisticsMadhav V UpadhyeNo ratings yet
- (60-3) Peer-Facilitated Cognitive Dissonance Versus Healthy Weight EatinDocument39 pages(60-3) Peer-Facilitated Cognitive Dissonance Versus Healthy Weight Eatin陳銑鈞No ratings yet
- ABC Fizicke Aktivnosti I ZdravljaDocument40 pagesABC Fizicke Aktivnosti I ZdravljaMirjana VanovicNo ratings yet
- Harrer 2019Document21 pagesHarrer 2019Leslie DuarteNo ratings yet
- Examen 2 2223 PDFDocument3 pagesExamen 2 2223 PDFAnelisse DominicciNo ratings yet
- EJCM - Volume 36 - Issue 3 - Pages 93-102Document10 pagesEJCM - Volume 36 - Issue 3 - Pages 93-102Shaikh AyyubNo ratings yet
- MoCATest Fitness PresentationDocument26 pagesMoCATest Fitness PresentationSNo ratings yet
- United Responses To The Clarion-Ledger With 2016 Performance DataDocument3 pagesUnited Responses To The Clarion-Ledger With 2016 Performance DataAnna WolfeNo ratings yet
- Obese + DM SR MADocument10 pagesObese + DM SR MAnatneednutNo ratings yet
- Ageing Research Reviews: Annabel P. Matison, Karen A. Mather, Victoria M. Flood, Simone ReppermundDocument18 pagesAgeing Research Reviews: Annabel P. Matison, Karen A. Mather, Victoria M. Flood, Simone ReppermundMasithaNo ratings yet
- Progesterone-Receptor Index in Meningiomas: Correlation With Clinico-Pathological Parameters and Review of The LiteratureDocument8 pagesProgesterone-Receptor Index in Meningiomas: Correlation With Clinico-Pathological Parameters and Review of The LiteratureSaputro AbdiNo ratings yet
- Effectiveness Manual Therapy & Kinesio Tape, Versus Dry Needling & Exercise Stabilization, On Patient Low Back Pain Due To Hernia Nucleus PulposusDocument5 pagesEffectiveness Manual Therapy & Kinesio Tape, Versus Dry Needling & Exercise Stabilization, On Patient Low Back Pain Due To Hernia Nucleus PulposusMuhammad Ridha Al JinaniNo ratings yet
- Depression and Obesity - Evidence of Shared Biological Mechanisms PDFDocument16 pagesDepression and Obesity - Evidence of Shared Biological Mechanisms PDFWesley RicardoNo ratings yet
- Prevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation - United States, 2007-2009Document36 pagesPrevalence of Doctor-Diagnosed Arthritis and Arthritis-Attributable Activity Limitation - United States, 2007-2009worksheetbookNo ratings yet
- Risk Factors For Pelvic Organ Prolapse: C.M. Kim, M.J. Jeon, D.J. Chung, S.K. Kim, J.W. Kim, S.W. BaiDocument4 pagesRisk Factors For Pelvic Organ Prolapse: C.M. Kim, M.J. Jeon, D.J. Chung, S.K. Kim, J.W. Kim, S.W. BaiAkame No IDNo ratings yet
- Nutritional Anthropometry - Part 2 of 4Document74 pagesNutritional Anthropometry - Part 2 of 4CARYL CLAIRE GALOCGOCNo ratings yet
- The Associations of Weekend Warrior Activity Patterns With The Visceral Adiposity Index in US Adults: Repeated Cross-Sectional StudyDocument11 pagesThe Associations of Weekend Warrior Activity Patterns With The Visceral Adiposity Index in US Adults: Repeated Cross-Sectional StudyAli HNo ratings yet
- Depression and Obesity - Evidence of Shared Biological MechanismsDocument16 pagesDepression and Obesity - Evidence of Shared Biological MechanismsAlexandreNo ratings yet
- Waist Hip Ratio or CV RiskDocument1 pageWaist Hip Ratio or CV RiskTony LeeNo ratings yet
- Phelan Pediatric MalnutritionDocument76 pagesPhelan Pediatric MalnutritionErna MiraniNo ratings yet
- Leitzmann Et Al., (2007) Physical Activity RecommendationsDocument8 pagesLeitzmann Et Al., (2007) Physical Activity RecommendationsAna Flávia SordiNo ratings yet
- Tambahan Tabel JurnalDocument1 pageTambahan Tabel JurnalBungaNo ratings yet
- The Influence of Body Mass Index On The Long-Term Survival of Patients With Renal Cell Carcinoma After Tumour NephrectomyDocument6 pagesThe Influence of Body Mass Index On The Long-Term Survival of Patients With Renal Cell Carcinoma After Tumour NephrectomyRania AnisNo ratings yet
- Chapter Four Data Analysis and Presentation of The ResultDocument12 pagesChapter Four Data Analysis and Presentation of The ResultAHMAD SAHRIL HUSSINNo ratings yet
- Abstract Pregnancy Outcomes of In-Vitro Fertilization On Infertile Women With Adenomyosis-Retrospective Cohort StudyDocument6 pagesAbstract Pregnancy Outcomes of In-Vitro Fertilization On Infertile Women With Adenomyosis-Retrospective Cohort StudyLouis ReganNo ratings yet
- Prospective, Controlled Study of Acyclovir Pharmacokinetics in Obese PatientsDocument4 pagesProspective, Controlled Study of Acyclovir Pharmacokinetics in Obese PatientsnnNo ratings yet
- Management Issues for Elderly Esophagogastric Cancer PatientsDocument12 pagesManagement Issues for Elderly Esophagogastric Cancer Patientscnarvaez5No ratings yet
- Taxotere Docetaxel 80 mg/4 ML Concentrate For Solution For InfusionDocument52 pagesTaxotere Docetaxel 80 mg/4 ML Concentrate For Solution For InfusionArbiati Rahman100% (1)
- Diacerein Cochrane Review 26 Jan 2006 - StoppressDocument9 pagesDiacerein Cochrane Review 26 Jan 2006 - StoppressYunus AmmarieNo ratings yet
- Riginal Research: LucasDocument11 pagesRiginal Research: Lucas'fanny Quenhita'No ratings yet
- Artikel Dies BingDocument6 pagesArtikel Dies Bing'fanny Quenhita'No ratings yet
- 2020-Cerebral Palsy in Children-A Clinical Overview PDFDocument11 pages2020-Cerebral Palsy in Children-A Clinical Overview PDFCarolina LilloNo ratings yet
- Fransen Et Al-2015-Cochrane Database of Systematic ReviewsDocument128 pagesFransen Et Al-2015-Cochrane Database of Systematic Reviews'fanny Quenhita'No ratings yet
- Elementary Digital Choice Boards by SlidesgoDocument53 pagesElementary Digital Choice Boards by SlidesgoJeRi RojasNo ratings yet
- Exercise For Type 2 Diabetes MellitusDocument34 pagesExercise For Type 2 Diabetes MellitusAnonymous SMLzNANo ratings yet
- In Search of The Definitive Brodmann's Map of Cortical Areas in HumanDocument11 pagesIn Search of The Definitive Brodmann's Map of Cortical Areas in HumanAndi rabitha Tenri YolaNo ratings yet
- Journal 2 - Fani Yuanita PratiwiDocument6 pagesJournal 2 - Fani Yuanita Pratiwi'fanny Quenhita'No ratings yet
- 01tango Therapy For ParkinsonDocument8 pages01tango Therapy For Parkinson'fanny Quenhita'No ratings yet
- jpts-28-685 1Document4 pagesjpts-28-685 1DidikPrasetyoSuliNo ratings yet
- Young Ari Kusworo, Agus Kristiyanto, Muchsin Doewes: Afiliasi PenulisDocument6 pagesYoung Ari Kusworo, Agus Kristiyanto, Muchsin Doewes: Afiliasi Penulis'fanny Quenhita'No ratings yet
- 02outcome Evaluation of Highly Challenging Balance.3Document8 pages02outcome Evaluation of Highly Challenging Balance.3'fanny Quenhita'No ratings yet
- Exercise For Type 2 Diabetes MellitusDocument34 pagesExercise For Type 2 Diabetes MellitusAnonymous SMLzNANo ratings yet
- Walking and breathing exercises relieve insomnia in pregnant womenDocument9 pagesWalking and breathing exercises relieve insomnia in pregnant women'fanny Quenhita'No ratings yet
- Relationship Between Socioeconomic Status and Physical Fitness in Junior High School StudentsDocument6 pagesRelationship Between Socioeconomic Status and Physical Fitness in Junior High School Students'fanny Quenhita'No ratings yet
- Physical Activity During Pregnancy and Its Influence On Delivery Time: A Randomized Clinical TrialDocument14 pagesPhysical Activity During Pregnancy and Its Influence On Delivery Time: A Randomized Clinical TrialZaray EspinosaNo ratings yet
- Racial/Ethnic and Socioeconomic Status Differences in Overweight and Health-Related Behaviors Among American Students: National Trends 1986 - 2003Document10 pagesRacial/Ethnic and Socioeconomic Status Differences in Overweight and Health-Related Behaviors Among American Students: National Trends 1986 - 2003'fanny Quenhita'No ratings yet
- Ffect of Static and Dynamic Stretching Exercises: The E On Sprint Ability of Recreational Male Volleyball PlayersDocument10 pagesFfect of Static and Dynamic Stretching Exercises: The E On Sprint Ability of Recreational Male Volleyball Players'fanny Quenhita'No ratings yet
- Pre Start Movement The Evidence For and Against DYNAMIC WARM UP THE ONLY PRE TRAINING AND PRE MATCH ROUTINEDocument6 pagesPre Start Movement The Evidence For and Against DYNAMIC WARM UP THE ONLY PRE TRAINING AND PRE MATCH ROUTINE'fanny Quenhita'No ratings yet
- 64-Articles Content-234-1-10-20190909Document5 pages64-Articles Content-234-1-10-20190909Selvira MarthingNo ratings yet
- Hamstring Flexibility PDFDocument5 pagesHamstring Flexibility PDFpradeep6288No ratings yet
- B R I E F: Aseline ISK Dentification of Rgonomic ActorsDocument1 pageB R I E F: Aseline ISK Dentification of Rgonomic Actors'fanny Quenhita'No ratings yet
- Nuci DapusDocument2 pagesNuci Dapus'fanny Quenhita'No ratings yet
- Naskah PublikasiDocument13 pagesNaskah PublikasisutianiNo ratings yet
- The Complete Guide To Core Stability - Matt Lawrence - Google BukuDocument1 pageThe Complete Guide To Core Stability - Matt Lawrence - Google Buku'fanny Quenhita'No ratings yet
- Beda Pengaruh Intervensi Peregangan Dan Mobilisasi Sendi Terhadap Perbaikan Keterbatasan Lingkup Gerak SendiDocument7 pagesBeda Pengaruh Intervensi Peregangan Dan Mobilisasi Sendi Terhadap Perbaikan Keterbatasan Lingkup Gerak SendiAbdRahmanDaudNasutionNo ratings yet
- Dapus Cicin 1Document1 pageDapus Cicin 1'fanny Quenhita'No ratings yet
- Physical Therapy & Rehabilitation: International Journal ofDocument6 pagesPhysical Therapy & Rehabilitation: International Journal of'fanny Quenhita'No ratings yet
- Muscle-Strengthening Exercise Among 397,423 U.S. Adults: Prevalence, Correlates, and Associations With Health ConditionsDocument11 pagesMuscle-Strengthening Exercise Among 397,423 U.S. Adults: Prevalence, Correlates, and Associations With Health Conditions'fanny Quenhita'No ratings yet
- Five Brothers and Their Mother's LoveDocument4 pagesFive Brothers and Their Mother's Lovevelo67% (3)
- SpamDocument2 pagesSpamAshutosh SinghNo ratings yet
- PPR - LISTS - Registered Medicine Price List - 20221127 BahrainDocument318 pagesPPR - LISTS - Registered Medicine Price List - 20221127 BahrainvdvedNo ratings yet
- Previews 2013360 PreDocument13 pagesPreviews 2013360 PreEko Setyo BudiNo ratings yet
- NURS 366 Exam 1 Study Guide and RubricDocument7 pagesNURS 366 Exam 1 Study Guide and RubriccmpNo ratings yet
- Sectors of The Indian EconomyDocument5 pagesSectors of The Indian EconomyhavejsnjNo ratings yet
- Practical 5.17 Protein MaterialsDocument2 pagesPractical 5.17 Protein MaterialsdeeyamullaNo ratings yet
- RP F107 PDFDocument45 pagesRP F107 PDFPriyam KmNo ratings yet
- 2018 Federal Income Tax Return PDFDocument8 pages2018 Federal Income Tax Return PDFBrandon BachNo ratings yet
- By Pass System in The Dry ProcessDocument34 pagesBy Pass System in The Dry Processfaheemqc100% (1)
- Space suit essentialsDocument6 pagesSpace suit essentialsAdam PaiggeNo ratings yet
- Research 1Document7 pagesResearch 1Rhea Mae ObligarNo ratings yet
- Chapter 18Document10 pagesChapter 18nehallakdawalaNo ratings yet
- Service Manual For High Efficiency High Ambient Amazon 20180726Document400 pagesService Manual For High Efficiency High Ambient Amazon 20180726Syedimam100% (1)
- The Morning Calm Korea Weekly - Oct. 14, 2005Document26 pagesThe Morning Calm Korea Weekly - Oct. 14, 2005Morning Calm Weekly NewspaperNo ratings yet
- A Review of Empathy Education in NursingDocument11 pagesA Review of Empathy Education in Nursinglora ardyaNo ratings yet
- Personal Development Course for Senior High StudentsDocument7 pagesPersonal Development Course for Senior High StudentsLucelle PalarisNo ratings yet
- Specification for Child MUAC Tape Quality ChecksDocument4 pagesSpecification for Child MUAC Tape Quality ChecksM HussainNo ratings yet
- Mandaya: Presented By: Cutad, Ray Dag-Uman, Ely Mae Cortes, MaikoDocument24 pagesMandaya: Presented By: Cutad, Ray Dag-Uman, Ely Mae Cortes, MaikoAPPLE MAE AGOSTONo ratings yet
- Buller, Paul F. - Schuler, Randall S - Managing Organizations and People - Cases in Management, Organizational Behavior and Human Resource Management-Thomson - South-Western (2006)Document530 pagesBuller, Paul F. - Schuler, Randall S - Managing Organizations and People - Cases in Management, Organizational Behavior and Human Resource Management-Thomson - South-Western (2006)ezekiel capuzNo ratings yet
- Let's Cook: Basic EnglishDocument6 pagesLet's Cook: Basic EnglishVincentNo ratings yet
- Principle of Economics Consolidated Assignements-2 - 10th February 22Document27 pagesPrinciple of Economics Consolidated Assignements-2 - 10th February 22Mani Bhushan SinghNo ratings yet
- 08 Ergonomics - 01Document35 pages08 Ergonomics - 01Cholan PillaiNo ratings yet
- 可汗语法48篇(明志教育推荐) PDFDocument163 pages可汗语法48篇(明志教育推荐) PDFtellmewhour100% (2)
- Fire Safety in Public BuildingDocument48 pagesFire Safety in Public BuildingSamirsinh ParmarNo ratings yet
- PT. Citilink Indonesia N P W P: 0 2 - 8 2 7 - 5 9 7 - 2 - 0 9 3 - 0 0 0 Jl. Raya Juanda Sawotratap Gedangan SidoarjoDocument2 pagesPT. Citilink Indonesia N P W P: 0 2 - 8 2 7 - 5 9 7 - 2 - 0 9 3 - 0 0 0 Jl. Raya Juanda Sawotratap Gedangan SidoarjoZemNo ratings yet
- Conversion Disorder in Childhood: James R. BrašićDocument8 pagesConversion Disorder in Childhood: James R. BrašićmasriffaNo ratings yet
- Pradhan Mantri Gram Sadak Yojana Pradhan Mantri Gram Sadak YojanaDocument19 pagesPradhan Mantri Gram Sadak Yojana Pradhan Mantri Gram Sadak Yojanapriyajaiswal428No ratings yet
- MA Only Notice Explains Coverage ChangeDocument2 pagesMA Only Notice Explains Coverage ChangeAnonymous Zp7kAtNo ratings yet
- Heavy Oil's Production ProblemsDocument22 pagesHeavy Oil's Production Problemsalfredo moran100% (1)