Professional Documents
Culture Documents
A Game Plan: Gamification Design Principles in Mhealth Applications For Chronic Disease Management
Uploaded by
MichaelaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Game Plan: Gamification Design Principles in Mhealth Applications For Chronic Disease Management
Uploaded by
MichaelaCopyright:
Available Formats
Viewpoint
Page 1 of 4
Do mental health mobile apps work: evidence and
recommendations for designing high-efficacy mental health
mobile apps
Pooja Chandrashekar
School of Engineering and Applied Sciences, Harvard University, Cambridge, MA, USA
Correspondence to: Pooja Chandrashekar. School of Engineering and Applied Sciences, Harvard University, 29 Oxford Street, Cambridge, MA 02138,
USA. Email: pchandrashekar@college.harvard.edu.
Received: 19 February 2018; Accepted: 28 February 2018; Published: 23 March 2018.
doi: 10.21037/mhealth.2018.03.02
View this article at: http://dx.doi.org/10.21037/mhealth.2018.03.02
Smartphone-based apps may expand access to classifies mental health apps into six categories based on
mental health treatment functionality: self-management, cognition improvement,
skills-training, social support, symptom tracking, and
Smartphone-based mental health apps represent a unique
passive data collection (3). Mental health apps span all
opportunity to expand the availability and quality of mental
stages of clinical care provision, including immediate crisis
health treatment. The number of mobile health (mHealth)
intervention, prevention, diagnosis, primary treatment,
apps focused on mental health has rapidly increased;
supplement to in-person therapy, and post-treatment
a 2015 World Health Organization (WHO) survey of
condition management (4). Mobile apps are a good choice
15,000 mHealth apps revealed that 29% focus on mental
for psychological treatment delivery compared to other
health diagnosis, treatment, or support (1). Additionally, platforms due to (I) ease of habit, (II) low effort expectancy,
public health organizations like the UK’s National Health and (III) high hedonic motivation (2,5).
Service (NHS) and the U.S. National Institute of Mental
Health (NIMH) have pointed to mental health apps as
cost-effective and scalable solutions to addressing the Do they work: evidence for using mental health
mental health treatment gap. But though the ubiquity of apps for treatment
smartphones is well-poised to address the mental health Though evidence supports the use of smartphone-based
provider shortage, the efficacy of mental health apps apps as a vehicle for mental health treatment delivery,
remains contested (2). As mental health apps are increasingly there remains debate around whether these apps have
prescribed to supplement psychiatric treatment and help demonstrated high efficacy (3). This is due to both the lack
patients self-manage their mental health conditions, it is key of evidence-based mobile apps available on the market,
to understand (I) whether, and which, mental health apps and the lack of studies that bring together the disorder-
have proved effective, and (II) what makes a mental health specific silos of evidence that do exist. To show that the
app effective. Here, we argue that mental health apps do have efficacy of evidence-based mobile apps is comparable to
value in providing psychological treatment, and present four traditional psychiatric treatment, we analyze the efficacy
recommendations for high-efficacy mental health apps. of smartphone-based treatments for three psychological
disorders with high 12-month global prevalence rates:
depression, anxiety, and schizophrenia.
Why apps: the utility of mental health apps for
psychological treatment
Depression
Mental health apps target a broad range of psychological
disorders and vary in design and functionality. NIMH Depression treatment options may not result in complete
© mHealth. All rights reserved. mhealth.amegroups.com mHealth 2018;4:6
Page 2 of 4 mHealth, 2018
alleviation of symptoms, and often fail to address post- focused on using smartphone apps for treating symptoms
treatment subclinical or residual depression symptoms. of schizophrenia demonstrated app retention was 92%, and
Mobile apps that use cognitive behavioral therapy (CBT), approximately 3.95 patient-app interactions took place each
mindfulness training, mood monitoring, and cognitive day. Self-reported patient experience survey results revealed
skills training to treat depressive symptoms are gaining high adherence, positive user experience, and broad-ranging
momentum. A meta-analysis of 18 randomized controlled clinical benefits (11).
trials (RCTs) covering 22 mobile apps revealed that using
apps to alleviate symptoms and self-manage depression
What makes them work: characteristics of high-
significantly reduced patients’ depressive symptoms
efficacy apps
compared to control conditions (g=0.38, P<0.001). They
also found that smartphone-based therapies yield the It is important to acknowledge the challenges of using apps
greatest benefits for individuals with mild to moderate, for mental health treatment. These challenges can broadly
rather than major, depression (6). be divided into the following categories: (I) poor regulation
of quality and privacy; (II) inconsistencies in engagement;
(III) narrow focus on one disorder per app (12,13). To be
Anxiety
effective and address these challenges, mental health apps
Though clinical evidence suggests that relaxation training, must be evidence-based and carefully designed. Developers
CBT, and mindfulness can reduce anxiety symptoms, access should integrate the following four characteristics of high-
to these interventions is limited by cost and availability. efficacy mental health apps.
Using mobile apps to deliver these interventions has thus
garnered attention as a supplement to in-person therapy
High patient engagement
and a mechanism to treat sub-clinical anxiety conditions
that may lie below the threshold for anxiety disorder Because patients typically use apps on their own time
treatment (7). A meta-analysis of nine RCTs that evaluated without clinical oversight, they must be intrinsically
the effects of smartphone-delivered interventions on motivated to engage with the app. Evidence from the
symptoms of subclinical and diagnosed anxiety disorders literature suggest that patient engagement can be improved
revealed that users experienced reductions in total anxiety through: (I) real-time engagement; (II) usage reminders; (III)
after using anxiety treatment apps (g=0.33, P<0.001). gamified interactions (14-16).
Additionally, anxiety-focused mobile apps delivered the
greatest reductions in anxiety symptoms when paired with
Simple user interface (UI) and experience
face-to-face or internet-based therapies. In fact, replacing
outpatient patient-therapist sessions with a mobile app Models of technology-based behavior change emphasize
resulted in no significant loss of treatment efficacy (8). the importance of simple, intuitive UIs for driving faster
behavior change through reduced cognitive demands. For
patients suffering from depression or anxiety, working
Schizophrenia
memory is often impaired. Apps serving these population
Antipsychotic medications can relieve schizophrenic must be designed to generate a low cognitive load, the total
hallucinations, delusions, and disorganization, but fail to mental activity imposed on working memory. A simple UI
address its behavioral symptoms. Though psychosocial reduces cognitive load and increases capacity for learning.
interventions (e.g., social skills training, cognitive training, Features that reduce cognitive load include: (I) the use of
and education on illness management) can alleviate pictures rather than text; (II) reduced sentence lengths; (III)
behavioral symptoms, these interventions are rarely inclusive, nonclinical language (14).
integrated into clinical treatment due to limited funding
and adequately trained staff. Mobile apps may present an
Transdiagnostic capabilities
opportunity to deliver these services directly to patients,
especially given evidence of little difference between Psychological disorders are highly comorbid; however,
how schizophrenic patients and healthy controls use few mental health apps explicitly harness transdiagnostic
technology (9,10). A systematic review of five studies methods to treat symptoms shared among disorders. Since
© mHealth. All rights reserved. mhealth.amegroups.com mHealth 2018;4:6
mHealth, 2018 Page 3 of 4
interventions for comorbid disorders are typically similar 4. Price M, Yuen EK, Goetter EM, et al. mHealth:
in delivery and content, transdiagnostic apps can increase a mechanism to deliver more accessible, more
patient engagement and treatment efficacy by reducing effective mental health care. Clin Psychol Psychother
the commitment needed to interact with multiple apps for 2014;21:427-36.
comorbid disorders (14,17,18). 5. Yuan S, Ma W, Kanthawala S, et al. Keep Using My
Health Apps: Discover Users Perception of Health and
Fitness Apps with the UTAUT2 Model. Telemed J E
Self-monitoring features
Health 2015;21:735-41.
App-based features that enable users to self-monitor their 6. Firth J, Torous J, Nicholas J, et al. The efficacy of
mood by periodically reporting their thoughts, behaviors, smartphone-based mental health interventions for
and actions can increase emotional self-awareness depressive symptoms: a meta-analysis of randomized
(ESA), which has been found to be implicated in anxiety, controlled trials. World Psychiatry 2017;16:287-98.
depression, and substance abuse (14). Increasing ESA, 7. Firth J, Torous J, Nicholas J, et al. Can smartphone mental
defined as the ability to identify and understand one’s own health interventions reduce symptoms of anxiety? A meta-
emotions, has been shown to reduce symptoms of mental analysis of randomized controlled trials. J Affect Disord
illness and improve coping skills (19-22). 2017;218:15-22.
8. Ly KH, Topooco N, Cederlund H, et al. Smartphone-
Supported versus Full Behavioural Activation for
Conclusions
Depression: A Randomised Controlled Trial. PLoS One
Mobile apps have significant potential to deliver high- 2015;10:e0126559.
efficacy mental health interventions. Given the global 9. Ben-Zeev D, Brenner CJ, Begale M, et al. Feasibility,
shortage of psychiatrists and the lack of mental health care Acceptability, and Preliminary Efficacy of a Smartphone
access in rural regions, apps have emerged as a viable tool Intervention for Schizophrenia. Schizophr Bull
to bridge the mental health treatment gap. Technology is 2014;40:1244-53.
well-poised to transform how mental health treatment is 10. Abdel-Baki A, Lal S, D-Charron O, et al. Understanding
delivered and accessed, but this transformation requires the access and use of technology among youth with first-
combined mobilization of science, regulation, and design. episode psychosis to inform the development of
technology-enabled therapeutic interventions. Early Interv
Psychiatry 2017;11:72-6.
Acknowledgements
11. Firth J, Torous J. Smartphone Apps for Schizophrenia: A
None. Systematic Review. JMIR Mhealth Uhealth 2015;3:e102.
12. Marley J, Farooq S. Mobile telephone apps in mental
health practice: uses, opportunities and challenges.
Footnote
BJPsych Bull 2015;39:288-90.
Conflicts of Interest: The author has no conflicts of interest to 13. Dennison L, Morrison L, Conway G, et al. Opportunities
declare. and Challenges for Smartphone Applications in Supporting
Health Behavior change: Qualitative Study. J Med Internet
Res 2013;15:e86.
References
14. Bakker D, Kazantzis N, Rickwood D, et al. Mental
1. Anthes E. Mental health: There’s an app for that. Nature Health Smartphone Apps: Review and Evidence-Based
2016;532:20-3. Recommendations for Future Developments. JMIR Ment
2. East ML, Havard BC. Mental Health Mobile Apps: From Health 2016;3:e7.
Infusion to Diffusion in the Mental Health Social System. 15. Chan S, Godwin H, Gonzalez A, et al. Review of Use and
JMIR Ment Health 2015;2:e10. Integration of Mobile Apps Into Psychiatric Treatments.
3. Technology and the Future of Mental Health Treatment. Curr Psychiatry Rep 2017;19:96.
National Institute of Mental Health 2017. Available online: 16. Fleming TM, Bavin L, Stasiak K, et al. Serious Games
https://www.nimh.nih.gov/health/topics/technology-and- and Gamification for Mental Health: Current Status and
the-future-of-mental-health-treatment/index.shtml Promising Directions. Front Psychiatry 2017;7:215.
© mHealth. All rights reserved. mhealth.amegroups.com mHealth 2018;4:6
Page 4 of 4 mHealth, 2018
17. Johnston L, Titov N, Andrews G, et al. Comorbidity and 20. Kauer SD, Reid SC, Crooke AH, et al. Self-monitoring
Internet-Delivered Transdiagnostic Cognitive Behavioural Using Mobile Phones in the Early Stages of Adolescent
Therapy for Anxiety Disorders. Cogn Behav Ther Depression: Randomized Controlled Trial. J Med Internet
2013;42:180-92. Res 2012;14:e67.
18. Rozbroj T, Lyons A, Pitts M, et al. Assessing the 21. Morris ME, Kathawala Q, Leen TK, et al. Mobile
Applicability of E-Therapies for Depression, Anxiety, and Therapy: Case Study Evaluations of a Cell Phone
Other Mood Disorders among Lesbians and Gay Men: Application for Emotional Self-Awareness. J Med Internet
Analysis of 24 Web- and Mobile Phone-Based Self-Help Res 2010;12:e10.
Interventions. J Med Internet Res 2014;16:e166. 22. Rickard N, Arjmand HA, Bakker D, et al. Development
19. Heron KE, Smyth JM. Ecological momentary of a Mobile Phone App to Support Self-Monitoring
interventions: Incorporating mobile technology into of Emotional Well-Being: A Mental Health Digital
psychosocial and health behaviour treatments. Br J Health Innovation. JMIR Ment Health 2016;3:e49.
Psychol 2010;15:1-39.
doi: 10.21037/mhealth.2018.03.02
Cite this article as: Chandrashekar P. Do mental health mobile
apps work: evidence and recommendations for designing high-
efficacy mental health mobile apps. mHealth 2018;4:6.
© mHealth. All rights reserved. mhealth.amegroups.com mHealth 2018;4:6
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Brief Interventions and Brief Therapy For Substance AbuseDocument254 pagesBrief Interventions and Brief Therapy For Substance AbuseSasu Nicoleta100% (5)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
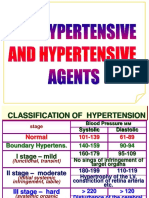
- Antihypertensive DrugsDocument29 pagesAntihypertensive Drugsmailforrandomuse100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Gamification in E-Mental Health: Development of A Digital Intervention Addressing Severe Mental Illness and Metabolic SyndromeDocument90 pagesGamification in E-Mental Health: Development of A Digital Intervention Addressing Severe Mental Illness and Metabolic SyndromeMichaelaNo ratings yet
- Hypnotherapy & PLR TherapyDocument14 pagesHypnotherapy & PLR TherapyReeshabhdev Gauttam100% (1)
- Management of The Dental Patient With Neurological Disease - Overview, Epilepsy, StrokeDocument5 pagesManagement of The Dental Patient With Neurological Disease - Overview, Epilepsy, StrokearindraNo ratings yet
- Colour TherapyDocument18 pagesColour Therapylily50% (2)
- Sports Medicine Introduction Day1Document16 pagesSports Medicine Introduction Day1Sharen Selvadurai100% (1)
- Test Bank For Fundamentals of Mental Health Nursing 4th Edition, LindaDocument23 pagesTest Bank For Fundamentals of Mental Health Nursing 4th Edition, LindaILL101100% (3)
- Lecture 3 History of Clinical PsychologyDocument49 pagesLecture 3 History of Clinical Psychologyumibrahim75% (8)
- Informed Consent For Porcelain VeneersDocument2 pagesInformed Consent For Porcelain VeneersEking In100% (1)
- The Challenger App For Social Anxiety Disorder - New Advances in Mobile Psychological TreatmentDocument30 pagesThe Challenger App For Social Anxiety Disorder - New Advances in Mobile Psychological TreatmentMichaelaNo ratings yet
- Assignment of Master'S Thesis: C T U P F I TDocument94 pagesAssignment of Master'S Thesis: C T U P F I TMichaelaNo ratings yet
- Czech Technical University in Prague Faculty of Information Technology Assignment of Master's ThesisDocument7 pagesCzech Technical University in Prague Faculty of Information Technology Assignment of Master's ThesisMichaelaNo ratings yet
- Play4fit: Enhancing Users' Engagement With Smartphone Health and Fitness Application Using Gamification Concept.Document6 pagesPlay4fit: Enhancing Users' Engagement With Smartphone Health and Fitness Application Using Gamification Concept.MichaelaNo ratings yet
- Technology and Mental Health The Role of A IDocument4 pagesTechnology and Mental Health The Role of A IMichaelaNo ratings yet
- An Android Based Medication Reminder System Based On OCR Using ANNDocument17 pagesAn Android Based Medication Reminder System Based On OCR Using ANNMichaelaNo ratings yet
- Journal of Promotional CommunicationsDocument11 pagesJournal of Promotional CommunicationsMichaelaNo ratings yet
- Journal of Promotional CommunicationsDocument17 pagesJournal of Promotional CommunicationsMichaelaNo ratings yet
- Do Mental Health Mobile Apps Work: Evidence and Recommendations For Designing High-Efficacy Mental Health Mobile AppsDocument26 pagesDo Mental Health Mobile Apps Work: Evidence and Recommendations For Designing High-Efficacy Mental Health Mobile AppsMichaelaNo ratings yet
- Technology and Mental Health: The Role of Artificial IntelligenceDocument2 pagesTechnology and Mental Health: The Role of Artificial IntelligenceMichaelaNo ratings yet
- Gameful Self-Regulation - A Study On How Gamified Self-Tracking Features Evoke Gameful ExperienceDocument10 pagesGameful Self-Regulation - A Study On How Gamified Self-Tracking Features Evoke Gameful ExperienceMichaelaNo ratings yet
- Medication Reminder and Healthcare - An Android ApplicationDocument8 pagesMedication Reminder and Healthcare - An Android ApplicationMichaelaNo ratings yet
- Creating A Digital Health Smartphone App and Digital Phenotyping Platform For Mental Health and Diverse Healthcare NeedsDocument13 pagesCreating A Digital Health Smartphone App and Digital Phenotyping Platform For Mental Health and Diverse Healthcare NeedsMichaelaNo ratings yet
- Developing and Implementing A Gamification Method User EngagementDocument33 pagesDeveloping and Implementing A Gamification Method User EngagementMichaelaNo ratings yet
- App-Based Mindfulness Meditation For Psychological Distress and Adjustment To College in Incoming University StudentsDocument27 pagesApp-Based Mindfulness Meditation For Psychological Distress and Adjustment To College in Incoming University StudentsMichaelaNo ratings yet
- Developing and Evaluating MindMax - Promoting Mental Wellbeing Through An Australian Footbal League-Themed AppDocument229 pagesDeveloping and Evaluating MindMax - Promoting Mental Wellbeing Through An Australian Footbal League-Themed AppMichaelaNo ratings yet
- Watashi DekiruyoDocument15 pagesWatashi DekiruyoMichaelaNo ratings yet
- Development of A Mental Health Smartphone App - Perspectives of Mental Health Service UsersDocument8 pagesDevelopment of A Mental Health Smartphone App - Perspectives of Mental Health Service UsersMichaelaNo ratings yet
- Threats and AttacksDocument21 pagesThreats and AttacksMichaelaNo ratings yet
- Social Engineering and Identity TheftDocument14 pagesSocial Engineering and Identity TheftMichaelaNo ratings yet
- It Feels Different From Real Life' Users' Opinions of Mobile Applications For Mental Health (Doi 10.1145 - 2838739.2838806)Document5 pagesIt Feels Different From Real Life' Users' Opinions of Mobile Applications For Mental Health (Doi 10.1145 - 2838739.2838806)MichaelaNo ratings yet
- Introduction To CybersecurityDocument9 pagesIntroduction To CybersecurityMichaelaNo ratings yet
- Cia M1 2Document6 pagesCia M1 2MichaelaNo ratings yet
- Lecture 5 First Aid and Antidotes Against Pesticides PoisoningDocument45 pagesLecture 5 First Aid and Antidotes Against Pesticides PoisoningMuhammad Shahrooz NaseerNo ratings yet
- Peritoneal Dialysis Brochure US 401067001 A PDFDocument6 pagesPeritoneal Dialysis Brochure US 401067001 A PDFstaryk0% (1)
- Schizophrenia - Indian Psychiatry JournalDocument128 pagesSchizophrenia - Indian Psychiatry JournalLIDIYA MOL P VNo ratings yet
- List Obat Lasa/ Norum Berdasarkan Ucapan MiripDocument3 pagesList Obat Lasa/ Norum Berdasarkan Ucapan MiripYusufa Ibnu Sina SetiawanNo ratings yet
- Adapted Aquatics and RehabilitationDocument14 pagesAdapted Aquatics and RehabilitationCarlos Ernesto AriasNo ratings yet
- Report - 11 Jul 2020Document4 pagesReport - 11 Jul 2020Shreedhar KadkolNo ratings yet
- Therapeutic Alliance in Schizophrenia The Role of Recovery PDFDocument6 pagesTherapeutic Alliance in Schizophrenia The Role of Recovery PDFAndrei BrookNo ratings yet
- Dos When Taking Diclegis: Do Not Use Diclegis If You Have Used An (In The Past 14 DaysDocument2 pagesDos When Taking Diclegis: Do Not Use Diclegis If You Have Used An (In The Past 14 Daysadrian lozanoNo ratings yet
- HYPOSPADIUSDocument4 pagesHYPOSPADIUSODONG MARTINNo ratings yet
- The Influence of Altered Lower-Extremity Kinematics On Patellofemoral Joint Dysfunction - Powers 2003Document8 pagesThe Influence of Altered Lower-Extremity Kinematics On Patellofemoral Joint Dysfunction - Powers 2003shivnairNo ratings yet
- 2016 European Guidelines On Cardiovascular Disease Prevention in Clinical PracticeDocument78 pages2016 European Guidelines On Cardiovascular Disease Prevention in Clinical PracticeJose Ignacio Tarton SisimitNo ratings yet
- Jurnal BronchopneumoniaDocument5 pagesJurnal BronchopneumoniaBianti Nur'ainiNo ratings yet
- Subcutaneous MycosesDocument23 pagesSubcutaneous Mycosessarguss14100% (1)
- CelecoxibDocument1 pageCelecoxibJoover AquinoNo ratings yet
- Mental Health Program Cut AdriftDocument2 pagesMental Health Program Cut AdriftDominic KitchingNo ratings yet
- Introduction To MAX InternationalDocument48 pagesIntroduction To MAX InternationalDanieldoeNo ratings yet
- 2009 Article 9164Document170 pages2009 Article 9164Amir Surya HidayahNo ratings yet
- TB Alt CuresDocument2 pagesTB Alt Curessidadams2No ratings yet
- Gamiz Bermudez Et Al 2021 Corrective Exercise Based Therapy For Adolescent IdiopDocument12 pagesGamiz Bermudez Et Al 2021 Corrective Exercise Based Therapy For Adolescent IdiopalfianjuniorNo ratings yet
- RCEM Curriculum 05 03 15 For August 2015 FINAL AMENDED 05 06 15 .PDF 61270597Document392 pagesRCEM Curriculum 05 03 15 For August 2015 FINAL AMENDED 05 06 15 .PDF 61270597RaheelNo ratings yet
- Indikasi Skull XrayDocument9 pagesIndikasi Skull XrayHesti Nurmala RizqiNo ratings yet