Professional Documents
Culture Documents
Brain Infections
Uploaded by
Samuel kuria0 ratings0% found this document useful (0 votes)
7 views28 pagesmedicine
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentmedicine
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views28 pagesBrain Infections
Uploaded by
Samuel kuriamedicine
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 28
Brain infections
Acute bacterial meningitis
• is an acute purulent infection within the sub-arachnoid
space.
• The meninges, the subarachnoid space, and the brain
parenchyma are all frequently involved in the
inflammatory reaction (meningoencephalitis).
• Etiology
– Strptococcus pneumoniae 30-60%
– Haemophylus influenzae <10%
– Neisseria meningitidis 10-35%
– Listeria monocyytogenes
– Gram negative organisms
– Staphlococcus-VP shunt,trauma or surgery
• Risk factors for pneumococcal meningitis
– Pneumococcal pneumonia
– acute or chronic pneumococcal sinusitis or otitis
media,
– alcoholism,
– diabetes,
– splenectomy,
– hypogammaglobulinemia, complement deficiency
– head trauma with basilar skull fracture and CSF
rhinorrhea
pathophysiology
• Microorganism and virus reach the nervous
through many routes main route is blood
stream and bacteria in URTI
• Microrganism in the csf in the subarachnoid
space becomes infected
• Infection spreads through meninges and
invades the ventricles
• Inflammatory response to infection tends to
increase the CSF production with moderate
increase in pressure .
Continuation of pathophysiology
• If the process extends into the brain ,parencyma
or if concurrent encephalitis is present ,cerebral
oedema and increased intracranial pressure
• Pathological alteration includes hyperaemia of
meningeal vessels,edema of brain tissues ,and
generalized inflammatory reactions with the
exudation of WBC into subarachnoid .
• Hydrocephalus may be caused by exudates
blocking the small passage between ventricles.
Clinical features
• Fever
• Headache
• Stiff neck
• Photosensitivity
• Altered mental status
• 2 of 4 found in 95% of patients
• Examination
– Kernig sign passive resistance to extension of
flexed knee at 90 degree
– Nuchal rigidity
– Brudzinski sign-flexion of knee and hip when neck
passively flexed
– Focal neurological sign-hemiparesis,aphasia etc
– Fundoscopy-papiloedema
– Rash-maculopapular,petechia etc
• Investigation
– Blood culture before antibiotics
– White cell count >10,000
– CT SCAN brain prior to lumbar puncture if
immunosuppressed,seizure,focal deficit,altered
mental status
– Lumbar puncture CSF
• turbid
• Gram stain and culture
• White cell >20
• Protein >0.45g/l or 45mg/dl
• Glucose <2.5mmol
Types of meningitis glucose protein cells
Acute bacterial low high PMNS often >300/mm
Acute viral low Normal or high Mononuclear
<300mm
tuberculous low high Mononuclear and
PMNs,<300/mm
Fungal low high <300/mm
malignant Low high Usually mononuclear
treatment
• Normal adult-ceftriaxone 2gm BD for two
weeks in pneumococcal.if resistance
suspected then add vancomycin
• Crytsalline penicillin 24mu/day every 4-6
hours
Complications
• Brain damage
• Build up of fluid between skull and
brain(subdural effusion)
• Hearing loss
• Hydrocephalus
• seizures
VIRAL MENINGITIS
• headache, fever, and signs of meningeal
irritation coupled with an inflammatory CSF
profile
• Constitutional signs can include malaise,
myalgia, anorexia, nausea and vomiting etc
• Drowsiness and lethargy
• Alteration in mental status,marked stupor or
confusion suggest encephalitis
• Etiology-enterovirus,HSV2,HIV are common
diagnosis
• CSF
– lymphocytic pleocytosis (25–500 cells/L),
– a normal or slightly elevated protein
concentration [0.2–0.8 g/L (20–80 mg/dL)],
– a normal glucose concentration,
– and a normal or mildly elevated opening pressure
(100–350 mmH2O)
VIRAL ENCEPHALITIS
• Viral infection of the brain parenchyma with
evidence of neurologic dysfunction
• Etiology
– HSV
– HZV
– Arbovirus
– Enterovirus
– Others HIV/CMV/JC virus
– mumps
• Fever,Headache Mental status change
seizures and focal neurological findings
• Diagnostic
– Lumbar puncture:
• lymphocytic pleocytosis;
• PCR for Human herpes virus
• Treatment of viral meningitis/encephalitis
– Acyclovir 15-30mg/kg TID
Subacute and chronic meningitis
• Tuberculosis meningitis-
– Index of suspicion- combination of
unrelenting headache, stiff neck, fatigue,
night sweats, and fever
– PLUS
– with a CSF lymphocytic pleocytosis and a mildly
decreased glucose concentration is highly
suspicious for tuberculous meningitis.
Characteristic of CSF
• elevated opening pressure,
• lymphocytic pleocytosis (10–500 cells/L),
• elevated protein concentration in the
range of 1–5 g/L, and
• decreased glucose concentration in the
range of 1.1–2.2 mmol/L (20–40 mg/dL).
• Diagnosis of TBM is via culture or PCR plus the
biochemistry of high protein and low glucose
and lymphocytic pleocytosis
• Treatment
– isoniazid,rifampcin,pyrazinamide,ethambutol
– Pyridoxine 50mg/day
– Dexamethasone 12-16mg tapered after three
weeks
• Cryptococcal meningitis
– Caused by cryptococcus neoformans almost
exclusively in HIV postive individuals
– CSF –
• mononuclear or lymphocytic pleocytosis, an increased
protein concentration, and a decreased glucose
concentration.
• Indian ink stains the fungi
• Cryptococcal antigen test is highly sensitive
• Treatment
– Induction phase of two weeks
• Amphotericin B 0.7-1mg/kg
– Plus
• Fluconazole 1200mg/day
– Consolidation for 8 weeks
• Fluconazole at 400-800mg/day
– Maintenance
• Fluconazole 200mg/day for minimum one year and
CD4 >100 on at least two occasion 6 months apart
Brain abscess
• Focal, suppurative infection within the brain
parenchyma, typically surrounded by a
vascularized capsule.
• Develop from
– direct spread from a contiguous cranial site of
infection, such as paranasal sinusitis, otitis media,
mastoiditis, or dental infection;
– following head trauma or a neurosurgical procedure
– (3) as a result of hematogenous spread from a remote
site of infection
– Cryptogenic in 25%,source unknown
• Etiology
– streptococci,
– Bacteroides spp.,
– Pseudomonas spp.,
– Haemophilus spp
– Enterobacteriaceae.
– staphylococci,
– Bacteroides spp.
– , Fusobacterium spp.,
• Clinical features-presents as an expanding intracranial
mass lesion rather than as an infectious process
• Median hospital presentation is 11–12 days following
onset of symptoms.
• The classic clinical triad of headache, fever, and a focal
neurologic deficit in <50%
• Others-focal or generalised seizure
• Focal deficit-hemiparesis,aphasia,visual field
defects,ataxia
• Signs of ICP-vomiting,nausea,vomiting,drowsiness
• Diagnosis-MRI or CT SCAN head.MRI is superior
moreso at earl stage
• Treatment
– third- or fourth-generation cephalosporin (e.g.,
cefotaxime, ceftriaxone, or cefepime) and
metronidazole
– Duration 6-8 weeks
– Intravenous dexamethasone therapy (10 mg every 6
h) is usually reserved for patients with substantial
periabscess edema and associated mass effect and
increased ICP and tapered rapidly
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Peripheral Nerve and Muscular WeaknessDocument17 pagesPeripheral Nerve and Muscular WeaknessSamuel kuriaNo ratings yet
- Leukamia and Transfusion MedicineDocument26 pagesLeukamia and Transfusion MedicineSamuel kuriaNo ratings yet
- Disorders of The PancreaseDocument14 pagesDisorders of The PancreaseSamuel kuriaNo ratings yet
- Haematological DisordersDocument28 pagesHaematological DisordersSamuel kuriaNo ratings yet
- Glomerular DiseasesDocument16 pagesGlomerular DiseasesSamuel kuriaNo ratings yet
- Disorders of Small IntestineDocument41 pagesDisorders of Small IntestineSamuel kuriaNo ratings yet
- Acute and Chronic Kidney DiseaseDocument17 pagesAcute and Chronic Kidney DiseaseSamuel kuriaNo ratings yet
- DementiaDocument11 pagesDementiaSamuel kuriaNo ratings yet
- Disorders of Esophagus and StomachDocument29 pagesDisorders of Esophagus and StomachSamuel kuriaNo ratings yet
- Acute Liver FailureDocument29 pagesAcute Liver FailureSamuel kuriaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
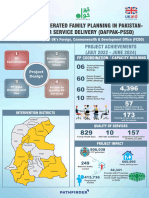
- Poster Sindh 2-01-2024Document11 pagesPoster Sindh 2-01-2024FM Printers111No ratings yet
- Pain Managementin TemporomandibularDocument10 pagesPain Managementin Temporomandibularirfanadil2006No ratings yet
- Borrescio-Higa Valenzuela - Gender Inequality and Mental Health.Document9 pagesBorrescio-Higa Valenzuela - Gender Inequality and Mental Health.Firdaus Silabi Al-AttarNo ratings yet
- HayalllDocument41 pagesHayalllchalie tarekegnNo ratings yet
- Can Your Baby Get Pregnant If You Have Sex While PregnantDocument6 pagesCan Your Baby Get Pregnant If You Have Sex While Pregnanteng-scribd100% (2)
- Mobile Phone Addiction Among YouthDocument10 pagesMobile Phone Addiction Among Youthda dadadfgNo ratings yet
- Niche and Sub-NicheDocument3 pagesNiche and Sub-NichehoneybeeNo ratings yet
- Universiti Kuala Lumpur Royal College of Medicine Perak: Year 3 Module Handbook (Medicine) 2014-2015Document15 pagesUniversiti Kuala Lumpur Royal College of Medicine Perak: Year 3 Module Handbook (Medicine) 2014-2015Codillia CheongNo ratings yet
- SOP-32-06 - Vendor Assessment (Oct 21)Document11 pagesSOP-32-06 - Vendor Assessment (Oct 21)parwana formuliNo ratings yet
- Crohn's Disease Seminar FinalDocument27 pagesCrohn's Disease Seminar Finalshahad alshareefNo ratings yet
- Addisons DiseaseDocument1 pageAddisons DiseaseAndreia Palade100% (1)
- q2 Grade 7 Health DLL Week 1Document8 pagesq2 Grade 7 Health DLL Week 1johann reyes0% (1)
- American Journal of Infection ControlDocument6 pagesAmerican Journal of Infection ControlfathimzahroNo ratings yet
- Paper 2 - Abisha AliDocument7 pagesPaper 2 - Abisha Aliapi-269596566No ratings yet
- DM No. 2022-0287 Updated Moa and Tor PRDPDocument8 pagesDM No. 2022-0287 Updated Moa and Tor PRDPDRMC Infirmary100% (1)
- PEBC Qualifying Exam References and Resources ListDocument5 pagesPEBC Qualifying Exam References and Resources ListAnkit ShahNo ratings yet
- Soal PAS BIG Xi, SMT 3, OnlineDocument10 pagesSoal PAS BIG Xi, SMT 3, OnlineRivaldi Lukman HakimNo ratings yet
- Cebu Technological University: Main CampusDocument2 pagesCebu Technological University: Main CampusLeonard Patrick Faunillan BaynoNo ratings yet
- Aggregates - Limestone Dolomite Safety Data SheetDocument8 pagesAggregates - Limestone Dolomite Safety Data SheetJEAN KATHLEEN SORIANONo ratings yet
- K5 - Sistem Informasi KesehatanDocument29 pagesK5 - Sistem Informasi KesehatanPusvaNurmalaSariNo ratings yet
- R.A. No. 6969 - Brown GroupDocument35 pagesR.A. No. 6969 - Brown GroupAngelNo ratings yet
- An Tropo Metri Status GiziDocument73 pagesAn Tropo Metri Status GiziMochammad Fariz AmsalNo ratings yet
- GL3655EDocument0 pagesGL3655EandyhrNo ratings yet
- The Sleep Doctor'S Diet Plan by Michael Breuss, PHD The Sleep Doctor'S Diet PlanDocument5 pagesThe Sleep Doctor'S Diet Plan by Michael Breuss, PHD The Sleep Doctor'S Diet PlanshubhangivsNo ratings yet
- Mindfulness Exercise 1: Attending To BreAthingDocument2 pagesMindfulness Exercise 1: Attending To BreAthingcruz210No ratings yet
- Chain of Hope Teams With Gift of LifeDocument1 pageChain of Hope Teams With Gift of LifeJonathan DanosNo ratings yet
- Veterans Affairs Presumptive Service Connection and Disability CompensationDocument33 pagesVeterans Affairs Presumptive Service Connection and Disability CompensationChuck Achberger100% (1)
- Biological Warfare Agents - AgronDocument129 pagesBiological Warfare Agents - AgronMARK ARQUE LACANARIANo ratings yet
- Professional Development Plan PPT 1Document10 pagesProfessional Development Plan PPT 1api-355484042No ratings yet
- Inpatient Management of Adolescents With Eating Disorders ToolkitDocument191 pagesInpatient Management of Adolescents With Eating Disorders ToolkitAjutor Anorexie-BulimieNo ratings yet