Professional Documents
Culture Documents
Conditions of The Accessory Organs
Conditions of The Accessory Organs
Uploaded by
Cake Man0 ratings0% found this document useful (0 votes)
18 views3 pagesThe pancreas functions as both an exocrine and endocrine gland. As an exocrine gland, it produces enzymes that aid digestion. Inflammation of the pancreas is called pancreatitis, which can be acute or chronic. Acute pancreatitis has a sudden onset and risks life-threatening complications, while chronic pancreatitis is long-lasting and causes progressive pancreatic damage over time. Chronic pancreatitis is often due to alcohol abuse or malnutrition and management focuses on pain relief. Pancreatic cancer typically develops late symptoms and has a very low 5-year survival rate.
Original Description:
Original Title
Conditions of the Accessory Organs
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe pancreas functions as both an exocrine and endocrine gland. As an exocrine gland, it produces enzymes that aid digestion. Inflammation of the pancreas is called pancreatitis, which can be acute or chronic. Acute pancreatitis has a sudden onset and risks life-threatening complications, while chronic pancreatitis is long-lasting and causes progressive pancreatic damage over time. Chronic pancreatitis is often due to alcohol abuse or malnutrition and management focuses on pain relief. Pancreatic cancer typically develops late symptoms and has a very low 5-year survival rate.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views3 pagesConditions of The Accessory Organs
Conditions of The Accessory Organs
Uploaded by
Cake ManThe pancreas functions as both an exocrine and endocrine gland. As an exocrine gland, it produces enzymes that aid digestion. Inflammation of the pancreas is called pancreatitis, which can be acute or chronic. Acute pancreatitis has a sudden onset and risks life-threatening complications, while chronic pancreatitis is long-lasting and causes progressive pancreatic damage over time. Chronic pancreatitis is often due to alcohol abuse or malnutrition and management focuses on pain relief. Pancreatic cancer typically develops late symptoms and has a very low 5-year survival rate.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 3
Conditions of the Accessory Organs
Chronic - onset is gradual; symptoms may
3. The Pancreas: appear late - when almost 80 - 90% of the
pancreas are already destroyed.
Exocrine Dysfunction
Etiology factors and predisposing
Pancreas
Alcoholism
A pistol-shaped organ; endocrine and /
exocrine gland Hypercalcemia
Parts: head, body and tail /
Trauma
Ducts: /
Wirsung's duct Hyperlipidemia
Santorini's duct /
Biliary tract disease - cholelithiasis
As an endocrine gland, it produces the /
hormones: Bacterial disease
/
1. Insulin - beta cells PUD
2 Glucagon - alpha cells /
3. Somatostatin - delta cells Mumps
/
As an exocrine gland it produces the Acute Pancreatitis
enzymes necessary for digestion:
PATHOPHYSIOLOGY
1. Amylase - Self-digestion of the pancreas by its own
2. Lipase digestive enzymes principally TRYPSIN
3. Trypsin
PATHOPHYSIOLOGY of acute
Pancreatic Secretions pancreatitis
1. Bicarbonate- to neutralize the acidic
chyme from the stomach Spasm, edema or block in the Ampulla of
2. Pancreatic amylase- for carbohydrate Vater
digestion /
reflux of proteolytic enzymes auto digestion
Pancreatitis - Inflammation of the of the pancreas
pancreas /
inflammation
Can be acute or chronic /
Inflammation, Hemorrhage, Necrosis
ACUTE VS CHRONIC PANCREATITIS /
ACTIVATION of KININ (induce
Acute - may range from mild to severe acute vasodilation and
(a medical emergency); high risk for life - /
threatening complications; onset is sudden. contraction of smooth muscle
12. Manage shock and other complications
increased permeability (in portal vessels and
pancreatic cells) Chronic Pancreatitis
/ Is an inflammatory condition
Loss of Protein-rich fluid into the characterized by progressive anatomic and
peritoneum functional destruction of the pancreas.
/
HYPOVOLEMIA with ASCITES Pathophysiology
ASSESSMENT findings Repeated attacks of pancreatitis
1. Abdominal pain- acute onset, attacks /
occurring after a heavy meal or alcohol Pancreatic cells are replaced by fibrous
intake tissues
2 Abdominal guarding /
3. Bruising on the flanks and umbilicus Pressure within the pancreas increases
4. N/V, jaundice /
5.Hypotension and hypovolemia Obstruction of the pancreatic and common
6.HYPERGLYCEMIA bile ducts and the duodenum
7. HYPOCALCEMIA /
8. Signs of shock Atrophy, inflammation and destruction of
the secreting cells of
DIAGNOSTIC TESTS /
1. Serum amylase and serum lipase elevated the pancreas
2. Ultrasound
3. WBC
4. Serum calcium 4 Major Causes
5. CT scan Alcohol(70 - 80% of all cases)
6. Hemoglobin and hematocrit Malnutrition (protein defičiency and
high fat)
NURSING INTERVENTIONS
1. Assist in pain management. Usually, Diagnostic Exams
Demerol is given. Morphine is AVOIDED ERCP
2. Assist in correction of Fluid and Blood CT scans, MRI, USG
loss Glucose Tolerance Test
3. Place patient on NPO to inhibit pancreatic Stool Exams
stimulation
Blood exams
4. NGT insertion to decompress distention
others
and remove gastric secretions
5. Maintain on bed rest
Management
7. Position patient in SEMI-FOWLER's
Treatment is aimed towards
decrease pressure on the diaphragm
preventing and managing acute attacks,
8. Deep breathing and coughing exercises
relieving pain and discomfort and managing
9. Provide parenteral nutrition
endocrine and docrine insufficiency.
10. Introduce oral feedings gradually HIGH
carbo, LOW FAT
11. Maintain skin integrity Endoscopy-to remove stones
Non opioid medication to pain Diagnostic Exams
Meperidine (Demerol) CT scan
Insulin (for DM) MRI, x- rays
Pancreatic enzyme replacement USG
ERCP with biopsy and histology
Surgery: Tissue diagnosis is made at the time
1. Pancreato jejunostomy of surgery for surgical patients
2 Pancreato - duodenostomy Management:
Surgery
• Use of MULTIPLE SUMP TUBES after Chemotherapy (Fluorouracil,
surgery to drain and irrigate Leucovorin, gemcitabine)
Radiation therapy
CA of the Pancreas
- The tumor may develop in the head Trend: Famesyl transferase inhibitors
(common), the body or the tail of the monoclonal antibodies and are under study
pancreas for pancreatic CA treatment (Choti, 2004).
- Clinical manifestations depend on the
location of the tumor
- If the beta cells are involved, then
syndrome of hyperinsulinism could develop
In most cases, diagnosis is made when 80 -
85% of the case is in the advanced stage
because symptoms arise late.
. Pancreatic carcinoma has only 4% survival
rate at 5 years regardless of the stage of the
disease or treatment (ACA, 2005).
Clinical Manifestations:
Vague upper mid abdominal pain
Jaundice
Weight loss
Vague upper abdominal discomfort
resulting to boring mid back pain
that will require opioids Ascites,
glycosuria, hyperglycemia and
glucose intolerance develop later
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5808)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Antibiotics Summary - Flattened PDFDocument3 pagesAntibiotics Summary - Flattened PDFmicheal1960100% (6)
- Circus Cat Alley Cat: Lesson - 3Document1 pageCircus Cat Alley Cat: Lesson - 3sukavasi1973100% (1)
- AntiCancer Drugs MCQsDocument25 pagesAntiCancer Drugs MCQssk90% (10)
- MenopauseDocument49 pagesMenopauseKaruna Kumari100% (3)
- 2010 FulltextDocument410 pages2010 FulltextNajam Din SahitoNo ratings yet
- Literacy Prop Box DentistDocument5 pagesLiteracy Prop Box Dentistapi-251432137No ratings yet
- Clipp Case 30Document9 pagesClipp Case 30manzooradilNo ratings yet
- IB Psychology Option: Abnormal - Revision NotesDocument4 pagesIB Psychology Option: Abnormal - Revision NotesNoor MohsinNo ratings yet
- Final Coaching - PalmrDocument55 pagesFinal Coaching - PalmrCake ManNo ratings yet
- Module PrelimDocument5 pagesModule PrelimCake ManNo ratings yet
- No Pregnancy Is Safe For Any WomanDocument2 pagesNo Pregnancy Is Safe For Any WomanCake ManNo ratings yet
- FC - CDDocument27 pagesFC - CDCake ManNo ratings yet
- Bitashdsadsa Lkwwa Daw Guide To The DSMDocument4 pagesBitashdsadsa Lkwwa Daw Guide To The DSMCake ManNo ratings yet
- Universal Emotions: GAMBARE! What Is Sadness?Document5 pagesUniversal Emotions: GAMBARE! What Is Sadness?Cake ManNo ratings yet
- Typoon KetsanaDocument2 pagesTypoon KetsanaCake ManNo ratings yet
- YOWAI NA That Is DepressionDocument4 pagesYOWAI NA That Is DepressionCake ManNo ratings yet
- 2 AspectsDocument4 pages2 AspectsCake ManNo ratings yet
- Depressusion Desu SymptomsDocument3 pagesDepressusion Desu SymptomsCake ManNo ratings yet
- SHIMATA SadnessDocument2 pagesSHIMATA SadnessCake ManNo ratings yet
- NASO and ORO-Tracheal SuctioningDocument4 pagesNASO and ORO-Tracheal SuctioningCake ManNo ratings yet
- What Is Gastritis?Document8 pagesWhat Is Gastritis?Cake ManNo ratings yet
- What Is Gastritis?Document13 pagesWhat Is Gastritis?Cake ManNo ratings yet
- Related Lit Case StudyDocument3 pagesRelated Lit Case StudyCake ManNo ratings yet
- Activity 1. EssayDocument4 pagesActivity 1. EssayCake ManNo ratings yet
- The CardiacDocument7 pagesThe CardiacCake ManNo ratings yet
- Tuti, Rhidab. (Transculture)Document1 pageTuti, Rhidab. (Transculture)Cake ManNo ratings yet
- Assessment 2 1 0 CommentDocument2 pagesAssessment 2 1 0 CommentCake ManNo ratings yet
- Related Review of LiteratureDocument4 pagesRelated Review of LiteratureCake ManNo ratings yet
- Corneal Dystrophies: Retinal DetachmentDocument5 pagesCorneal Dystrophies: Retinal DetachmentCake ManNo ratings yet
- Checklist For Cardiac AssessmentDocument3 pagesChecklist For Cardiac AssessmentCake ManNo ratings yet
- Altered Neurovascular Status: FractureDocument3 pagesAltered Neurovascular Status: FractureCake ManNo ratings yet
- Precipitating FactorsDocument2 pagesPrecipitating FactorsCake ManNo ratings yet
- Post-Traumatic Stress DisorderDocument2 pagesPost-Traumatic Stress DisorderCake ManNo ratings yet
- Health Declaration Form: Applicant ProfileDocument1 pageHealth Declaration Form: Applicant ProfileOnyx XynoNo ratings yet
- IV. Dizoxia PDFDocument11 pagesIV. Dizoxia PDFIvanes IgorNo ratings yet
- RAD MS Nursing Long ExamDocument16 pagesRAD MS Nursing Long ExammiaaNo ratings yet
- Foreword - 2020 - Handbook of Clinical NeurologyDocument2 pagesForeword - 2020 - Handbook of Clinical NeurologyGlia Assessoria PedagógicaNo ratings yet
- Taken - Natasha KnightDocument168 pagesTaken - Natasha KnightAlo VidalNo ratings yet
- Everybody Loves A Good Drought - Palagummi SainathDocument282 pagesEverybody Loves A Good Drought - Palagummi Sainathsrivatsav60% (5)
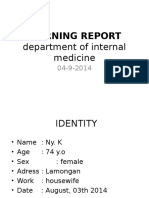
- MORNING REPORT Ipd 040914Document22 pagesMORNING REPORT Ipd 040914Teddy PrawiroNo ratings yet
- Nabel Point. The CentreDocument19 pagesNabel Point. The CentreveromoresNo ratings yet
- Cholecystectomy: Cholecystectomy (Pronounced / Kɒləsɪs Tɛktəmi/, Plural: Cholecystectomies) Is TheDocument3 pagesCholecystectomy: Cholecystectomy (Pronounced / Kɒləsɪs Tɛktəmi/, Plural: Cholecystectomies) Is Thejosias_jorgio1No ratings yet
- C8e 06 Test BankDocument20 pagesC8e 06 Test BankSpencer Martin50% (2)
- GAF - 2010 10 12 Homepage PDFDocument2 pagesGAF - 2010 10 12 Homepage PDFindahNo ratings yet
- Misdiagnosed Odontogenic Headache: Case Report and Review of LiteratureDocument2 pagesMisdiagnosed Odontogenic Headache: Case Report and Review of LiteratureAtul DwivediNo ratings yet
- Biofumigation: A Potential Aspect For Suppression of Plant-Parasitic NematodesDocument7 pagesBiofumigation: A Potential Aspect For Suppression of Plant-Parasitic NematodesIJEAB JournalNo ratings yet
- 4HB0 01 Que 20120307Document28 pages4HB0 01 Que 20120307AlaaNo ratings yet
- Appendicitis Introduction AppendicitisDocument4 pagesAppendicitis Introduction AppendicitisShiba AmpaNo ratings yet
- MCQ Haemato (DivC)Document6 pagesMCQ Haemato (DivC)Muhammad Nazif0% (2)
- DM No. 2020-0357 Guidance in Anticipation of Possible Increase in Cases of Infectious Diseases During The Rainy Season Amidst COVID-19Document9 pagesDM No. 2020-0357 Guidance in Anticipation of Possible Increase in Cases of Infectious Diseases During The Rainy Season Amidst COVID-19Zero Toribio MellaNo ratings yet
- Dermatofitosis FitzpatrickDocument28 pagesDermatofitosis FitzpatrickFadli IlhamNo ratings yet
- CosnsolesDocument228 pagesCosnsolesAnonymous pmVnncYJ100% (1)
- Review of Literature PivdDocument5 pagesReview of Literature PivdPankaj VatsaNo ratings yet
- 43 Adaptive Support Ventilation As VDocument5 pages43 Adaptive Support Ventilation As Vnanang criztaNo ratings yet
- MsdsDocument6 pagesMsdsWilliam GonzalesNo ratings yet