Professional Documents
Culture Documents
OSTEOPROSIS
Uploaded by
HANNAH MICOLE GAERLAN0 ratings0% found this document useful (0 votes)
11 views2 pagesOsteoporosis is a systemic skeletal disease characterized by low bone mass and deterioration of bone tissue, leading to fragile bones that break easily. It is categorized based on bone mineral density measurements compared to young adults. Symptoms include severe back pain from collapsed vertebrae fractures, loss of height, and bone deformities. Diagnosis involves bone density scans. Risk factors include hereditary factors, menopause, lack of exercise, low calcium/vitamin D, smoking, medications, and medical conditions. Nursing priorities are mobility impairment, nutritional imbalances, and knowledge deficits. Management includes education, exercise, nutrition, fall prevention, and drug therapies like bisphosphonates, monoclonal antibodies, hormones, and bone building medications
Original Description:
Nursing process
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOsteoporosis is a systemic skeletal disease characterized by low bone mass and deterioration of bone tissue, leading to fragile bones that break easily. It is categorized based on bone mineral density measurements compared to young adults. Symptoms include severe back pain from collapsed vertebrae fractures, loss of height, and bone deformities. Diagnosis involves bone density scans. Risk factors include hereditary factors, menopause, lack of exercise, low calcium/vitamin D, smoking, medications, and medical conditions. Nursing priorities are mobility impairment, nutritional imbalances, and knowledge deficits. Management includes education, exercise, nutrition, fall prevention, and drug therapies like bisphosphonates, monoclonal antibodies, hormones, and bone building medications
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views2 pagesOSTEOPROSIS
Uploaded by
HANNAH MICOLE GAERLANOsteoporosis is a systemic skeletal disease characterized by low bone mass and deterioration of bone tissue, leading to fragile bones that break easily. It is categorized based on bone mineral density measurements compared to young adults. Symptoms include severe back pain from collapsed vertebrae fractures, loss of height, and bone deformities. Diagnosis involves bone density scans. Risk factors include hereditary factors, menopause, lack of exercise, low calcium/vitamin D, smoking, medications, and medical conditions. Nursing priorities are mobility impairment, nutritional imbalances, and knowledge deficits. Management includes education, exercise, nutrition, fall prevention, and drug therapies like bisphosphonates, monoclonal antibodies, hormones, and bone building medications
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
OSTEOPOROSIS
DESCRIPTION NURSING DIAGNOSES BY PRIORITY
● Systemic skeletal disease characterized by low bone 1. Impaired physical mobility related to bone loss
mass and microachriectual deterioration of bone tissue 2. Imbalanced nutrition: less than body requirement
that leads to increased bone fragility and susceptibility related to inadequate calcium and vitamin D
to fracture 3. Deficient knowledge related to lack of exposure to
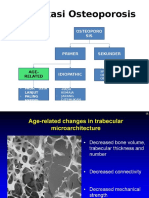
● Categories of osteoporosis: information regarding medication, dietary
○ Normal modifications and safe activity program
■ Value for bone mineral content
(BMC) is not more than 1.0 standard NURSING MANAGEMENT/ INTERVENTION
deviation (SD) below young adult ● Promote understanding of osteoporosis and the
mean value treatment regimen
○ Low bone mass (osteopenia) ● Advise patient to rest in bed in a supine or side lying
■ Value for BMC lied between 1.0 to position several times a day to relieve pain
2.5 SD below young adult mean ● Encourage the patient to intake adequate calcium and
value vitamin d
○ Osteoporosis ● Encourage walking and regular weight bearing
■ BMC is more than 2.5 SD below the exercises to enhance the production of vitamin D
young adult value ● Encourage the patient to avoid tobacco and alcohol
○ Severe osteoporosis ● Instruct the patient regarding estrogen replacement
■ BMC is more than 2.5 SD below the therapy
young adult value and presence of ● Inform the patient regarding dietary calcium and
one or more fragility fracture vitamin D
● Administer food high in fiber and increase fluids to
FOCUS ASSESSMENT (SIGNS AND SYMPTOMS) prevent constipation
● Severe back pain caused by fractures of collapsed
vertebra MEDICAL/ SURGICAL INTERVENTION
● Loss of height ● Joint replacement
● Progressive vertebral deformities ○ Replace all or part of a joint with a prosthesis
● Changes in appearance ● Closed or open reduction with internal fixation
○ Open- implants to guide the healing process of
DIAGNOSTIC AND LABORATORY TEST a bone
● Bone density scan ○ Closed- to set or reduce a broken bone without
○ Used to measure bone mineral density surgery
○ Commonly performed using dual energy x-
ray absorptiometry (DXA) DRUG ANALYSIS
● Calcium and vitamin D supplements
RISK FACTORS ● Bisphosphonates
● Hereditary ○ Increase bone mass and decrease bone loss by
● Low body weight (<127 lbs) inhibiting osteoclast function
● Prolonged premenopausal amenorrhea or early ■ Alendronate, risedronate,
menopause ibandronate, zoledronic
● Inadequate physical activity ● Monoclonal antibody medications
● Low intake of dietary calcium ○ Decrease bone resorption, increase BMD and
● Suboptimal level of vitamin D reduce the risk of fracture
● Smoking and alcohol intake ○ Administered intradermally every 6 months
○ Suppress osteoblast activity ■ Denosumab
● Certain medication such as: ● Hormone related therapy
○ Steroids, thyroid hormone, anti- convulsants, ○ Help maintain bone density in menopausal
calcium channel blockers, NSAIDS women
● Certain medical conditions such as: ■ Estrogen, raloxifene
○ Celiac disease, IBD, cancer, rheumatoid ● Calcitonin
arthritis ○ Inhibits osteoclasts thereby reducing bone loss
● Fragility fracture resulting from low trauma and increasing bone mineral density
● Osteopenia ● Bone building medication
○ Used when other common treatment cannot be
tolerated
■ Teriparatide- stimulates new bone
growth
■ Abaloparatide
■ Romosozumab
You might also like
- Panalpina 7-Point Container Inspection ChecklistDocument1 pagePanalpina 7-Point Container Inspection ChecklistNisma NilamNo ratings yet
- NCP For Gouty ArthritisDocument3 pagesNCP For Gouty ArthritisMolly HollyNo ratings yet
- Meas - Lecture Note Substructure Note 3Document14 pagesMeas - Lecture Note Substructure Note 3LokuliyanaNNo ratings yet
- Biology Subject For Pre-K: Bones by SlidesgoDocument18 pagesBiology Subject For Pre-K: Bones by Slidesgomalar kumuthaNo ratings yet
- Drugs For Bone Disorders CompleteDocument18 pagesDrugs For Bone Disorders CompleteOmar AbdullahiNo ratings yet
- 7 Treatment of OsteoporosisDocument23 pages7 Treatment of OsteoporosisIlham KurniawanNo ratings yet
- Tara's CH. 64 Arthritis and Connective Tissue DisordersDocument34 pagesTara's CH. 64 Arthritis and Connective Tissue DisordersTara McNeillNo ratings yet
- Osteoporosis: Mohd Fikri Bin MustapaDocument54 pagesOsteoporosis: Mohd Fikri Bin MustapaiqiessesNo ratings yet
- Focused ReviewDocument6 pagesFocused ReviewGina GiammalvoNo ratings yet
- NCMB 314 - GERIATRICS (CARE OF THE OLDER ADULT) - Physical and Physiological Changes of AgingDocument3 pagesNCMB 314 - GERIATRICS (CARE OF THE OLDER ADULT) - Physical and Physiological Changes of AgingSofia LiNo ratings yet
- OsteoporosisDocument5 pagesOsteoporosisjsdlzjNo ratings yet
- Fracture Prevention Treatments Postmenopausal Women OsteoporosisDocument4 pagesFracture Prevention Treatments Postmenopausal Women Osteoporosisroby6No ratings yet
- Vitamin D Benefits and RisksDocument60 pagesVitamin D Benefits and Risksapi-393403647No ratings yet
- NDR Vivlodex Project DP 1Document7 pagesNDR Vivlodex Project DP 1api-665600383No ratings yet
- OsteoporosisDocument7 pagesOsteoporosisLorebell100% (2)
- Osteoarthritis of Knee: Vinod NaneriaDocument96 pagesOsteoarthritis of Knee: Vinod Naneriaagrawal29071989No ratings yet
- Pharmacotherapy Handbook 7th Edition-1-31-43Document13 pagesPharmacotherapy Handbook 7th Edition-1-31-43Erfin NingoNo ratings yet
- UK Guideline 2020 220709Document8 pagesUK Guideline 2020 220709rnwkrnrnNo ratings yet
- OsteoporosisDocument78 pagesOsteoporosisapi-324305863No ratings yet
- Pathophysiology of OsteoarthritisDocument41 pagesPathophysiology of OsteoarthritisghaziaNo ratings yet
- Kelompok 6 OsteoporosisDocument10 pagesKelompok 6 OsteoporosisNur Indah FitrianaDewiNo ratings yet
- Treatment Protocol Acute GoutDocument2 pagesTreatment Protocol Acute Goutapi-456313554No ratings yet
- Muscular Dystrophy-Olivia (Autosaved)Document14 pagesMuscular Dystrophy-Olivia (Autosaved)Aaron James GrayNo ratings yet
- OP ملونة كاملةDocument27 pagesOP ملونة كاملةArcangela QuaintrelleNo ratings yet
- Osteoarthritisknee: DR - Ketan Pandey Attending Consultant Joint Replacement Unit BLK Superspeciality HospitalDocument49 pagesOsteoarthritisknee: DR - Ketan Pandey Attending Consultant Joint Replacement Unit BLK Superspeciality HospitalPankaj VatsaNo ratings yet
- OsteoporosisDocument47 pagesOsteoporosisSasha VaidyaNo ratings yet
- Osteoporosis Medical ManagementDocument15 pagesOsteoporosis Medical ManagementKeina Arranz MolinaNo ratings yet
- Muskuloskeletal 2012 NaufalDocument53 pagesMuskuloskeletal 2012 Naufaldahlia kharisma wardhaniNo ratings yet
- Osteoporosis, Rickets and OsteomalaciaDocument43 pagesOsteoporosis, Rickets and OsteomalaciahasNo ratings yet
- Musculoskeletal DisordersDocument158 pagesMusculoskeletal DisordersJona Kristin EnclunaNo ratings yet
- Osteoporosis Clinical Case by SlidesgoDocument30 pagesOsteoporosis Clinical Case by SlidesgoHussein Al-jmrawiNo ratings yet
- Acid PamidronicDocument2 pagesAcid PamidronicAyanSeryNo ratings yet
- Musculoskeletal System GeriatricsDocument4 pagesMusculoskeletal System GeriatricsKathleen Ellize BetchaydaNo ratings yet
- FSHN 398 - Spring Project JaDocument20 pagesFSHN 398 - Spring Project Jaapi-529966007No ratings yet
- ScreeningDocument31 pagesScreeningBenny Chris TantoNo ratings yet
- Drugs Effecting On Osteoporosis: Abdullaev Dzhumadil, Pharmd International Medical UniversityDocument25 pagesDrugs Effecting On Osteoporosis: Abdullaev Dzhumadil, Pharmd International Medical UniversityRtxGaming Zone 73No ratings yet
- 16 Integ - Group 4 ReportingDocument5 pages16 Integ - Group 4 ReportingDump AccNo ratings yet
- Musculoskeletal SystemDocument60 pagesMusculoskeletal Systempetite_chien15No ratings yet
- Presented By: Safa Riaz Presented To: Sir Ahmed Watoo Sap Id: 70095869 Topic: OsteoporosisDocument31 pagesPresented By: Safa Riaz Presented To: Sir Ahmed Watoo Sap Id: 70095869 Topic: OsteoporosisSafa RiazNo ratings yet
- OsteoporosisDocument11 pagesOsteoporosis906 SoNo ratings yet
- NCMB316 OsteoporosisDocument11 pagesNCMB316 Osteoporosis3-B-4 NAVIA, Kyle Bless V.No ratings yet
- Slide Materi Dr. Nelfi, SPKFR - Osteoporosis and Fracture Prevention - PMR4GP 2022Document32 pagesSlide Materi Dr. Nelfi, SPKFR - Osteoporosis and Fracture Prevention - PMR4GP 2022Maulia Wisda Era ChresiaNo ratings yet
- OsteoporosisDocument33 pagesOsteoporosisNadya LiemNo ratings yet
- Drugs For OsteoporosisDocument4 pagesDrugs For OsteoporosisJanine Castro SuguitanNo ratings yet
- Degenerative Disease in OrthopaedicDocument30 pagesDegenerative Disease in Orthopaedichelen kususma wardaniNo ratings yet
- OsteoporosisDocument35 pagesOsteoporosisNadya Magfira0% (1)
- Curriculum Vitae: Nama: Natsir Akil Riwayat PendidikanDocument50 pagesCurriculum Vitae: Nama: Natsir Akil Riwayat PendidikanSelica ErlindiNo ratings yet
- Drugs For Bone MetabolismDocument15 pagesDrugs For Bone MetabolismkwennybiangNo ratings yet
- 10256393Document31 pages10256393Diah PramuditaNo ratings yet
- Bone Healing 1Document42 pagesBone Healing 1bran makmornNo ratings yet
- Drug Induced OsteoporosisDocument8 pagesDrug Induced OsteoporosislueglemeNo ratings yet
- Management of Muscle Cramps in Patients With Chronic Kidney DiseaseDocument3 pagesManagement of Muscle Cramps in Patients With Chronic Kidney DiseaseSubhajit MaitraNo ratings yet
- OsteoporosisDocument13 pagesOsteoporosisRuaa MalekNo ratings yet
- Penyakit Sendi Degeneratif & Patologi TulangDocument38 pagesPenyakit Sendi Degeneratif & Patologi Tulangnaufal ihsanNo ratings yet
- 1-12 Osteoporosis in Childern - Dr. Hesham A GhanyDocument43 pages1-12 Osteoporosis in Childern - Dr. Hesham A GhanytarikeopsNo ratings yet
- Paget'S Disease: Presented By-Riya Kumari Basic BSC 2 Year College of NursingDocument20 pagesPaget'S Disease: Presented By-Riya Kumari Basic BSC 2 Year College of NursingRashi SinghNo ratings yet
- Strength of Osteoporotic Bone Is Impaired By:: Name: Johne Vincent V. Sarian Year/Section/Group: BSN 4-6 Group 4Document9 pagesStrength of Osteoporotic Bone Is Impaired By:: Name: Johne Vincent V. Sarian Year/Section/Group: BSN 4-6 Group 4Dodong GalitNo ratings yet
- B Is Phospho NatesDocument34 pagesB Is Phospho NatesGayathri RaveendranNo ratings yet
- Osteoprosis Presentation 2Document38 pagesOsteoprosis Presentation 2Shaz RizwanNo ratings yet
- RDU Case On Bone & Joint DisordersDocument22 pagesRDU Case On Bone & Joint DisordersATHENA MINERVA MORDENONo ratings yet
- Degenerative Disc Disease: A Beginner's 3-Step Plan to Managing DDD Through Diet and Other Natural Methods, with Sample Curated RecipesFrom EverandDegenerative Disc Disease: A Beginner's 3-Step Plan to Managing DDD Through Diet and Other Natural Methods, with Sample Curated RecipesNo ratings yet
- Ramon Magsaysay Memorial Medical Center, Inc.: University of The EastDocument7 pagesRamon Magsaysay Memorial Medical Center, Inc.: University of The EastHANNAH MICOLE GAERLANNo ratings yet
- University of The EastDocument4 pagesUniversity of The EastHANNAH MICOLE GAERLANNo ratings yet
- Ecg & BTDocument68 pagesEcg & BTHANNAH MICOLE GAERLANNo ratings yet
- NCM117 NCPDocument2 pagesNCM117 NCPHANNAH MICOLE GAERLANNo ratings yet
- Irritable Bowel SyndromeDocument6 pagesIrritable Bowel SyndromeHANNAH MICOLE GAERLANNo ratings yet
- Ramon Magsaysay Memorial Medical Center IncDocument2 pagesRamon Magsaysay Memorial Medical Center IncHANNAH MICOLE GAERLANNo ratings yet
- Rizal Critical EssayDocument2 pagesRizal Critical EssayHANNAH MICOLE GAERLANNo ratings yet
- Peptic Ulcer DiseaseDocument1 pagePeptic Ulcer DiseaseHANNAH MICOLE GAERLANNo ratings yet
- Cerebrovascular DiseaseDocument2 pagesCerebrovascular DiseaseHANNAH MICOLE GAERLANNo ratings yet
- Dar Administrative Order No. 04-03Document22 pagesDar Administrative Order No. 04-03Therese EspinosaNo ratings yet
- F1 Case IIM BangaloreDocument32 pagesF1 Case IIM Bangalorerishabh jainNo ratings yet
- Writers 39 Forum - 07 2018 PDFDocument68 pagesWriters 39 Forum - 07 2018 PDFGala Caesar AnugerahNo ratings yet
- 160649-Kanwal Saif - Critical EssayDocument4 pages160649-Kanwal Saif - Critical Essaykanwal afridiNo ratings yet
- YDRA/ YDRA 2009: Service ManualDocument359 pagesYDRA/ YDRA 2009: Service ManualJoaquim Filipe Ganhao100% (1)
- Marketing Revision BookletDocument18 pagesMarketing Revision BookletGodfreyFrankMwakalinga0% (1)
- Anaphy Possible ExamDocument7 pagesAnaphy Possible ExamZyra Kim ResareNo ratings yet
- Males Total Overall Reading Profile: Second SemesterDocument1 pageMales Total Overall Reading Profile: Second SemesterBernadette Manili LptNo ratings yet
- Multimedia Systems Lab Sheet 3 R.A.P.C.P Ranasinghe IT 14115394Document7 pagesMultimedia Systems Lab Sheet 3 R.A.P.C.P Ranasinghe IT 14115394M Naveed ShakirNo ratings yet
- InglesDocument5 pagesInglesDavid Quiñones PoloNo ratings yet
- Cisco Show CommandsDocument20 pagesCisco Show CommandsNorbert OngNo ratings yet
- A Short History of FirearmsDocument25 pagesA Short History of Firearmssveenl100% (10)
- 9th Bio Chapter 1 (1-32)Document32 pages9th Bio Chapter 1 (1-32)gmian9012No ratings yet
- Compilation of Academic PapersDocument27 pagesCompilation of Academic PapersGerald LandichoNo ratings yet
- Do Video Games Cause Violence - It's Complicated. - Rhetorical AnalysisDocument6 pagesDo Video Games Cause Violence - It's Complicated. - Rhetorical AnalysisGayTreeNo ratings yet
- Lesson 1 and 2 - Single Entry System, Correction of ErrorsDocument8 pagesLesson 1 and 2 - Single Entry System, Correction of ErrorsThe Brain Dump PHNo ratings yet
- Electro-Diesels v6Document14 pagesElectro-Diesels v6Nuh AinuhaNo ratings yet
- Examples of Geographic SegmentationDocument2 pagesExamples of Geographic SegmentationLucas satosNo ratings yet
- Nyaa Student Handbook PDFDocument63 pagesNyaa Student Handbook PDFAntonio UngureanNo ratings yet
- Pyramid of HateDocument8 pagesPyramid of Hateapi-263356428No ratings yet
- CONTOH Surat Lamaran Kerja Bhs EngDocument10 pagesCONTOH Surat Lamaran Kerja Bhs Engboy5mil3No ratings yet
- Cariño Vs CariñoDocument1 pageCariño Vs CariñoEmmanuel C. DumayasNo ratings yet
- French LiteratureDocument65 pagesFrench Literatureverlaine88No ratings yet
- Environment Culture and Cosmovision Roots of Farmers Natural Resource ManagementDocument13 pagesEnvironment Culture and Cosmovision Roots of Farmers Natural Resource Managementai_toch3685No ratings yet
- Group 1-Activity 4Document12 pagesGroup 1-Activity 4Dũng NguyễnNo ratings yet
- 2022 CiDocument22 pages2022 CiK60 Lâm Nguyễn Minh TấnNo ratings yet
- Nutrition Choice BingoDocument1 pageNutrition Choice BingoJenonymouslyNo ratings yet
- Lista Precios202107Document6 pagesLista Precios202107JoudynCold ZeroNo ratings yet