Professional Documents
Culture Documents
A New Competency Model For General Practice - Implication For Selection
Uploaded by
Anonymous GOUaH7FOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A New Competency Model For General Practice - Implication For Selection
Uploaded by
Anonymous GOUaH7FCopyright:
Available Formats
Research
Fiona Patterson, Abdol Tavabie, MeiLing Denney, Máire Kerrin, Vicki Ashworth,
Anna Koczwara and Sheona MacLeod
A new competency model for general practice:
implications for selection, training, and careers
Introduction The primary purpose of this study is to
Under the UK government’s plans for evaluate the current selection criteria for
NHS reform, expectations of policymakers those entering general practice training.
regarding the future role of the GP are a However, the results also offer important
Abstract topic of significant debate.1,2,3 With major information regarding content of training,
Background structural changes in the UK NHS,4 there career development and aspects of workforce
Recent structural and policy changes in the UK is now more emphasis on exploring the planning. Previous research has largely
health service have significantly changed the job skills and capabilities of GPs outside of the focused on doctor–patient consultations
responsibilities for the GP role. consulting room, relating to leadership, (such as measuring determinants of patient
Aim
professionalism5,6 and engagement in satisfaction).9,10 Relatively little research
To replicate a previous job analysis study to commissioning activities.4,7 These skills has explored aspects of GP performance
examine the relevance of current competency are in addition to designing services for outside of the consulting room, relating to
domains and selection criteria for doctors their registered patients, with an increasing planning services, financial management,
entering training.
shift of patient care from hospitals into the and running a practice.11 Similarly, previous
Design and method community. This suggests that there is a research in GP selection has tended to
A multisource, multimethod approach broadening of the UK GP job role from that focus on indicators of clinical judgement,
comprising three phases: (1) stakeholder
consultation (n = 205) using interviews, centred on a ‘helping model’ in doctor– reasoning and patient communication9,12,13
focus groups and behavioural observation of patient consultations to a role that also rather than skills associated with working
practising GPs; (2) a validation questionnaire emphasises a ‘business model’, where GPs in multiprofessional teams and practice
based on results from phase 1 (n = 1082); are increasingly required to consider how management.
followed by (3) an expert panel (n = 6) to review
and confirm the final competency domains. their work impacts at a community level and The current UK GP selection system
how this fits within the health system as a is reliable, valid, and generates positive
Results whole.4 Furthermore, a recent policy report candidate reactions,14,15,16,17 and uses
Eleven competency domains were identified, on the career path of GPs advocates the selection criteria derived from a job analysis
which extends previous research findings.
A new domain was identified called Leading
future importance of generalism as opposed study published over 12 years ago in this
for Continuing Improvement. Results show to specialty development.8 However, there journal.9 Although the selection criteria
that, Empathy and Perspective Taking, is limited research available to inform the were reviewed using a nationwide survey
Communication Skills, Clinical Knowledge skills and professional attributes required of in 2005,18 there is a now an urgent need to
and Expertise, and Professional Integrity are
currently rated the most important domains. GPs in future for their expanded role outside ensure continued relevance given recent
Results indicate a significant increase in ratings of the consulting room. This paper reports changes in practice.4 Research consistently
of importance for each domain in the future on a multisource, multimethod job analysis shows that the cornerstone of effective
(P<0.001), except for Communication Skills study of the GP role, replicating a previous selection is identifying selection criteria
and Empathy and Perspective Taking, which
consistently remain high. job analysis conducted over 12 years ago.9 through job analysis studies.19 Job analysis
Conclusion
The breadth of competencies required for F Patterson, BSc, MSc, PhD, CPsychol, Board, University of Nottingham, Nottingham.
GPs has increased significantly. GPs are now AcSS, FRCGP (Hon), professor and principal Address for correspondence
required to resolve competing tensions to be researcher, Department of Psychology, University
effective in their role, such as maintaining a Fiona Patterson, Department of Psychology,
of Cambridge, Cambridge. A Tavabie, deputy
patient focus while overseeing commissioning, University of Cambridge, Downing Street,
dean director and GP dean for Health Education
with a potential ethical conflict between these Kent, Surrey Sussex, London. M Denney, DCH, Cambridge, CB2 3EB.
aspects. Selection criteria remain largely DRCOG, FRCGP, PCME, ILTM, MMedSci (Clin E-mail: F.patterson@workpsychologygroup.com
unchanged but with increased priority in some Ed), interim MRCGP research and development Submitted: 22 November 2012; Editor’s
domains (for example, Effective Teamworking). lead for the MRCGP, Edinburgh. M Kerrin, BSc, response: 15 January 2013; final acceptance: 28
However, there is an urgent need to review the MSc, PhD, CPsychol, director; V Ashworth, BSc, February 2013.
training provision arrangements to reflect the MSc, CPsychol, senior consultant; A Koczwara,
greater breadth of competencies now required. ©British Journal of General Practice
BA, MSc, PhD, CPsychol, associate director, Work
Psychology Group Ltd, Derby. S MacLeod, FRCGP, This is the full-length article (published online
Keywords 29 Apr 2013) of an abridged version published in
MMEd, FAoME, DOccMed, DCH, DRCOG, director
clinical competence; education; knowledge;
of education and quality and postgraduate dean, print. Cite this article as: Br J Gen Pract 2013;
personnel recruitment; personnel selection;
East Midlands Local Education and Training DOI: 10.3399/bjgp13X667196
professional competence; training.
e331 British Journal of General Practice, May 2013
with patient representatives, 23 with allied
healthcare professionals/health managers/
How this fits in administrators, and three with trainees (see
A job analysis study conducted over Table 1 for a description). A total of eight
12 years ago was used to inform focus groups were conducted, comprising
development of selection criteria and GP trainers (n = 58), Royal College patient
training interventions. A revised model representatives (n = 9), and trainee
comprising 11 competency domains was
representatives (n = 29). A total of 32 hours
identified, including a new domain labelled
Leading for Continuing Improvement. of behavioural observations of practising
Results indicate that the GP role has GPs (n = 6) were conducted across five sites
significantly increased in breadth and there in a range of locations (at least one in each
is increasing potential for role conflict in of the UK nations and a mix of urban and
the job design. Some updates are required rural areas).
to the current selection criteria but these Data arising from the interviews, focus
remain largely unchanged. There are
groups and behavioural observations were
however, serious concerns about the level
of preparedness after training as several transcribed and analysed over a 3-day period
domains are not adequately covered at by a panel of six independent researchers
present to provide sufficient support to experienced in job analysis. The initial process
equip trainees in future. of coding was conducted using a two-level
card sort method,21 whereby behavioural
descriptions were grouped according to
similarity. For example, all behavioural
is a systematic process for the collection
descriptions relating to ‘clear and concise
and analysis of job-related information
in written and verbal communication’ were
to provide a framework with which role-
grouped together to form a behavioural
specific selection criteria can be identified
indicator. Next, behavioural indicators were
and prioritised. Results are used to develop
classified into higher-order competency
behavioural indicators for use in assessment
domains, and assigned a label to reflect the
when operationalising a selection method.20
domain content, such as Communication
Method Skills and Professional Integrity.
Having produced an initial framework, the
The job analysis method adopted here
label for each domain with a corresponding
follows a previously validated approach9,20
definition was used to create items for a
comprising three phases:
questionnaire. The questionnaire comprised
11 domains with four items per domain.
• stakeholder consultation (n = 205) Responders were asked to indicate the
using a combination of semi-structured importance of each domain:
interviews (n = 103), focus groups (n = 96)
and behavioural observation (n = 6) of GPs
(in a range of practices across the UK over • currently in the GP role;
30 hours); • in the future GP role;
• validation questionnaire based on phase 1 • for assessment at point of selection; and
results administered to a further sample • for addressing during training.
of stakeholders within the GP community Each item was based on a 6-point Likert-
to examine the initial competency type scale where 1 = ‘not at all important’
framework (n = 1082); followed by and 6 = ‘very important’. The questionnaire
• expert panel to review all available was administered electronically. It was
evidence from phases 1 and 2 to confirm accessible for online completion for 1 month
the competency framework and identify via 15 regional websites. Wilcoxon signed-
core themes arising from the results (n = 6 rank tests were used to examine differences
experts). This three-phase method was between mean ratings of importance for
designed to triangulate results consistent the current and future GP role for each
with previous job analysis studies.9,20 competency domain, and between mean
For phase 1, a convenience sample of rating of importance for selection and
205 stakeholders participated either in training.
an interview, focus group, or behavioural In phase 3, a panel of six independent
observation. A total of 103 semi-structured experts with no previous involvement in the
interviews were conducted, either face- analysis reviewed the results arising from
to-face or by telephone, each lasting phases 1 and 2. The panel comprised two
approximately 45 minutes. Of these, 32 senior GPs and four senior occupational
interviews were conducted with GPs, 38 psychologists. The panel met during a 1-day
British Journal of General Practice, May 2013 e332
workshop to agree the final competency
Table 1. Summary of stakeholder interviews domains. This review included identifying
areas of similarity to, and divergence from
Interviews Organisation Roles n
the previously published competency
GPs RCGP Assessment and Curriculum Leads 7 framework.9
Elected Representatives for the Panel of Examiners 1
Chair of Assessment Committee 1 Results
R&D Lead for MRCGP and Deputy Chief Examiner 1
Phase 1. Stakeholder consultation
Advisor to MRCGP 1
A total of 4168 behavioural descriptions
RCGP Council Chair, RCGP Council 1
were extracted from the interviews, focus
Chair Postgraduate Training Committee 1
groups and observations. Using the card
COPMeD Chair 1 sort procedure described above, 266 were
COGPED Chair 1 identified as unique and these formed the
GPNRO Chair 1 basis of the initial framework. A total of
Deaneries GP Recruitment Leads 3 11 independent competency domains were
Commissioning Leads 2 identified: (1) Empathy and Perspective
National Association of Chief Executive 1
Taking; (2) Communication Skills; (3)
Sessional GPs Clinical Knowledge and Expertise; (4)
Conceptual Thinking and Problem-
British International Chair 1
Solving; (5) Organisation and Management
Doctors Association
of Resources; (6) Professional Integrity;
General Practitioners Chair 1
(7) Coping with Pressure; (8) Effective
Committee
Teamworking; (9) Respect for Diversity and
Medical Schools GP Deans/Senior Educators 3 the Law; (10) Learning and Development
UK Association of Chair 1 of Self and Others; and (11) Leading for
Programme Directors Continuing Improvement (Table 2).
National Association of Chair 1 When compared to the original competency
Primary Care Educators framework,9 the expert panel judged 10 of
UKCEA Chair 1 the domains to align closely with the existing
AiT Subcommittee Chair 1 domains (such as Communication Skills
and Professional Integrity). However, the
First5 representatives Chair 1
definition for each of these domains has
Department of Health Department of Health Director General of Workforce 1 expanded, which reflects a broadening of
and Medical Deputy Director of Workforce Capacity 1
the role. For example, Organisation and
Education England Academia/ research — Society for Academic 1
Planning is now defined as Organisation
Primary Care
NHS Management/Workforce Planning 1
and Management of Resources, and has
a greater emphasis on management of
Medical Education Director of Medical Education 1
external resources within and outside the
England (MEE) Dean Advisor 1
Clinical Advisor 1
GP practice, rather than solely personal
resources. The previously delineated domain
Patients and Patient Picker Institute Chief Executive 1
Personal Attributes was not identified as an
Representatives RCGP Patient Chair 1
independent domain this time. Instead, an
Partnership Group
National Association for President 1
additional domain was identified, defined
Patient Participation as Leading for Continuing Improvement,
East Midlands Deanery Patient representatives 35 reflecting the new requirement of the job
Allied Professionals Allied healthcare Practice Managers, Patient Services Manager, 18
role.
and healthcare professionals Dispenser Manager, Receptionists, Practice
professionals Nurses, District Nurses, Community Counsellor Phase 2. Validation questionnaire
A total of 1082 individuals completed the
Other healthcare Presidents/Medical Directors from Royal College of 5
professionals Physicians, Royal Collage of Paediatrics and Child
questionnaire (demographic characteristics
Health, Royal College of Obstetricians and of the responder sample are displayed
Gynaecologists, Royal College of Psychiatry, in Table 3). The descriptive statistics for
Faculty of Public Health the rated importance of each competency
Trainees Derbyshire, England 3 domain is shown in Table 4. Results indicate
Glasgow, Scotland that all 11 competency domains were
Llandrindod, Wales perceived as currently highly important for
Total 103 the GP role, with Empathy and Perspective
Taking, Communication Skills, Clinical
AiT = Associate in Training. COGPED = Committee of General Practice Education Directors of the UK. COPMeD =
Knowledge and Expertise, and Professional
Conference of Postgraduate Medical Deans of the UK. GPNRO = National Recruitment Office for GP Training. MRCGP
= Membership of the Royal College of General Practitioners. RCGP = Royal College of General Practitioners.
Integrity rated as the most important
R&D = Research and Development. UKCEA = UK Conference of Postgraduate Education Advisors in General Practice. currently. Respect for Diversity and the Law
and Leading for Continuing Improvement
e333 British Journal of General Practice, May 2013
Table 2. Identified competency domains for general practice with example behavioural indicators
1. Empathy and Perspective Taking • Capacity and motivation to view situations from the patient and/or colleague perspective; acts in an open
and non-judgemental manner.
• Takes a holistic approach to patient care and considers social, psychological and emotional factors as well
as the wider healthcare system.
• Takes a patient-centred approach, treating patients as individuals; empowers patients through involvement
in their own care.
2. Communication Skills • Demonstrates an ability to listen attentively and actively.
• Tailors language to suit the individual and the situation; provides explanations using non-technical
language; builds rapport with others.
• Communicates clearly both written and verbally with team members and others (patients, colleagues,
allied healthcare professionals).
3. Clinical Knowledge and Expertise • Capacity to apply sound clinical knowledge and awareness to full investigation of problems, reflecting good
clinical judgement.
• Proficient in information gathering and history taking; applies knowledge effectively to make clear and
proactive decisions.
• Able to anticipate rather than just react; maintains knowledge of current research and practice.
4. Conceptual Thinking and Problem-Solving • Thinks conceptually, using critical analysis to think around issues to help formulate solutions; open to ideas
and suggestions from others.
• Recognises inconsistencies in information; able to assimilate information quickly; identifies key issues/
details and understand data.
• Able to synthesise multiple streams of evidence to make effective judgements; makes decisions confidently
and in a timely way.
5. Organisation and Management of Resources • Efficient and organised; employs effective processes to manage own workload.
• Able to prioritise and shift demands to fulfil tasks; demonstrates attention to detail.
• Is aware of resources available and manages these appropriately, considers implications of actions and/or
activities on available resources.
6. Professional Integrity • Open and honest with others; willing to admit own mistakes; treats others with respect and knows where
personal and professional boundaries lie.
• Able to balance ethical tensions in relation to demand, resources and expectations.
• Demonstrates a commitment to equality of care for all and strives to act in the patient’s best interests.
7. Coping with Pressure • Willing to admit when experiencing difficulties and seek assistance where needed; readily employs tactics
for managing own stress and pursues a healthy work and life balance.
• Remains calm under pressure; demonstrates self-awareness; understands own limitations, manages
own emotions and is resilient.
• Able to take on multiple complex roles and balance differing responsibilities and commitments, capable of
modifying behaviour to adapt to differing roles; accepts and manages uncertainty and change, responding
flexibly when required.
8. Effective Teamworking • Able to effectively influence and negotiate with others; promotes an inclusive approach; motivates others
to achieve goals.
• Supportive of colleagues; offers advice and assistance as required; understands and respects others’ roles
within the wider multiprofessional team.
• Is open to sharing information; collaborative with other professionals; acknowledges and appreciates
others’ expertise; willing to learn from others.
9. Respect for Diversity and the Law • Demonstrates awareness and is compliant with nationally or locally agreed policies; works to protocol,
guidelines, and legislation.
• Recognises prejudice and works with, and learns from, others’ prejudices; appreciates values, and sees
the strength of diversity.
• Recognises and takes into account own and others’ moral and religious codes.
10. Learning and Development of Self and Others • Committed to the learning and development of self and others; able to self-manage; actively promotes
self-directed learning.
• Proactively seeks feedback; motivated to learn; supports others to learn through engaging in peer support
and teaching.
• Demonstrates lifelong desire to develop skills and abilities to enable effective fulfilment of role responsibilities.
11. Leading for Continuing Improvement • Shows leadership skills and organisational awareness within and outside of the practice; is an ambassador
for the profession; inspires and empowers others and is positive about the future of general practice.
• Commitment to quality improvement in care; understands the needs of the local community; manages
healthcare pathways effectively.
• Considers multiple agendas (for patient, practitioner, higher clinician); understands implications of
decisions on the health of the wider population.
• Understands and demonstrates business, finance and budget management and skills; is aware of the cost
and value of services.
British Journal of General Practice, May 2013 e334
most important currently (Empathy and
Table 3. Demographic data for Perspective Taking and Communications
the validation questionnaire Skills) were still perceived as the most
(n = 1082) important in the future, as they were in the
previous job analysis study.9 However, the
Sex %
most significant increases in perceptions
Male 47.3
Female 51.9 of importance for the future were (in order
Undisclosed 0.8 of magnitude of increasing importance in
future), Leading for Continuing Improvement
Ethnic group
White 85.7
(t = 4429, P<0.001, r = –0.54), Organisation
Black 1.2 and Management of Resources (t = 3927.5,
Asian 10.1 P<0.001, r = –0.50), and Effective
Mixed 1.6 Teamworking (t = 3552.5, P<0.001, r = –0.30).
Other 1.4 Regarding perceived importance for
Role selection into training, Communication
GP/Allied health professionals 92.8 Skills, Empathy and Perspective Taking,
Trainees 6.5 and Professional Integrity were rated as
Undisclosed 0.8 the most important domains, broadly
Involved in medical education reflecting the current selection criteria.
Yes 84.5 However, compared to the previous job
No 14.6 analysis study,9 results show other domains
Undisclosed 1.0 are also important for selection, including,
Effective Teamworking (mean = 4.63)
and Learning and Development of Self
and Others (mean = 4.59). By contrast,
were rated as less important for the role Leading for Continuing Improvement and
currently (although all domains were rated Organisation and Management of Resources
>4 on a 6-point Likert scale; indicating that were perceived as less important at the
all domains were considered important). point of selection (mean = 3.48 and 4.08
For the relative importance of the respectively). All competency domains were
competency domains now and in the seen as increasingly important to address
future, there was a significant increase in during the training pathway, with Leading
nine of the 11 domains (P<0.001; Table for Continuing Improvement showing the
4), with the exception of Communications greatest increase in importance rating
Skills and Empathy and Perspective Taking (t = 1989.50, P<0.001, r = –0.76), followed by
as these domains were both rated highly Organisation and Management of Resources
important now and in the future. In absolute (t = 1320, P<0.001, r = –0.77).
terms, the competency domains rated as
Phase 3. Expert panel review
A final framework of 11 competency domains
and corresponding behavioural indicators
Table 4. Mean ratings of importancea for each competency domain was confirmed through a review by an expert
panel. The expert panel identified three core
Current Future Importance Importance
importance importance in selection in training
themes arising from the study relating to:
Competency domains Mean SD Mean SD Mean SD Mean SD
• significantly increased role breadth for
1. Empathy and Perspective Taking 5.77 0.54 5.76 0.58 5.04 0.92 5.79 0.53
GPs in the future;
2. Communication Skills 5.83 0.48 5.83 0.52 5.21 0.84 5.84 0.50
• increased potential for role conflict
3. Clinical Knowledge and Expertise 5.61 0.63 5.64 0.63 4.55 1.0 5.63 0.63
through balancing patient care and
4. Conceptual Thinking and Problem-Solving 5.33 0.77 5.41 0.78 4.63 0.93 5.41 0.71 financial responsibilities; and
5. Organisation and Management of Resources 5.12 0.80 5.51 0.72 4.08 1.0 5.35 0.72 • concerns around the level of preparedness
6. Professional Integrity 5.66 0.61 5.73 0.59 5.24 0.92 5.62 0.67 for practice after training.
7. Coping with Pressure 5.43 0.70 5.54 0.69 4.72 0.91 5.48 0.69 Table 5 summarises the core themes
8. Effective Teamworking 5.30 0.76 5.47 0.72 4.63 0.93 5.46 0.69 identified with illustrative quotations from
9. Respect for Diversity and the Law 5.05 0.86 5.16 0.85 4.46 1.1 5.16 0.83 the stakeholder interviews (from phase 1).
10. Learning and Development of Self 5.26 0.73 5.37 0.73 4.59 1.0 5.40 0.74
Regarding an increased role breadth,
and Others results show an enhanced emphasis for
GPs to consider multiple agendas beyond
11. Leading for Continuing Improvement 4.47 0.95 4.99 0.96 3.48 1.2 4.94 0.92
the patient and their practice in future,
a
1= not at all important and 6 =very important. to include the health of their registered
population, the broader community, and
e335 British Journal of General Practice, May 2013
towards patient care but this demand
Table 5. Key themes identified by the expert panel with quotations could at times be at odds with maintaining
to illustrate findings professional boundaries.
1. Significantly increased role breadth for general practice in the future A third theme identified was the level
• Considering multiple agendas ‘I’ve got to consider the patient’s agenda(s), I’ve got of trainee preparedness for practice given
to consider the practitioner’s agenda … of course new job role requirements. For example,
there’s the higher clinician agenda that I need to there are gaps in training provision relating
to bring into this.’ to dealing with challenging psychosocial
• Balancing local and ‘bigger-picture’ thinking ‘GPs will have to see the patient in front of them in issues facing patients. In future a significant
the context of the whole healthcare system.’ proportion of the role will involve an
‘GPs have to learn to balance their working week increasingly broad range of non-clinical
between face-to-face contact with individual patients duties. Capabilities relating to Leading
and involvement as clinician in the wider sense, for Continuing Improvement, leadership,
delivering healthcare processes for the locality to innovation, and financial awareness are
which they are working.’ not currently assessed in training or tested
• Taking on multiple complex roles ‘I think the future GPs are going to have to be much directly in the current MRCGP licensure
more than what they are now; part social worker, exams.
public health person, part commissioner, part GP ...’
2. Increased potential for increased role conflict Discussion
• Commitment to patient care versus ‘There will be an increasing pressure to make Summary
managing resources difficult decisions as GPs have to decide between This study extends previous research by
cases of funding versus patient care — there is more conducting a comprehensive job analysis to
pressure to consider money and funding.’ develop a model of 11 competency domains
• Maintaining patient trust versus professional ‘GPs don’t like saying “no”, they like to be able to say required for effective practice, now and in the
integrity relating to resources “yes” ... but this isn’t going to be possible with finite future. Compared to a previous job analysis
resource.’ study9 results here show substantial
• Holistic patient care versus negotiating the ‘In deprived areas some doctors are shocked by the alignment. However, some important
boundary between illness and disease conditions people live in and find themselves wanting changes were clearly identified, such as
management within their professional identity to “fix” the overall situation ... are they only there for a significantly increased role breadth,
the treatment of medical conditions?’ where several domains are now broader
3. Level of preparedness for practice after training in their definition to reflect contemporary
• Some elements of the future GP role are not ‘Trainees will need greater support during training in practice. For example, Empathy and
currently addressed in training developing their business acumen. The need to know Perspective Taking replaces Empathy and
about budget management, employment law, PR, Sensitivity identified in the previous study
HR ... not just clinical’ (which focused more on behaviours within
• Effective training in how to treat medical ‘Trainees are often unprepared to deal with difficult the consulting room), whereas the present
ailments but less in how to deal with difficult situations involving child protection issues, domestic study shows an increased emphasis on
psychological or social issues facing patients violence or relationship issues and bereavement etc teamworking within multiprofessional
as they are unlikely to have encountered this to a units, reflecting additional skills outside
great extent during training.’ of the consulting room. Furthermore, a
• Training focuses on the clinical role — ‘Managing paperwork is a critical skill to be an new competency domain was identified:
a significant proportion of the role will involve an effective GP but the non-clinical administration side Leading for Continuing Improvement
increasingly broad range of non-clinical duties is not taught in training.’ relating to population (registered patients)
HR = human resources. PR = public relations. health needs, business acumen, finance,
and budget management (in addition to
managing healthcare pathways effectively).
the NHS. GPs will be required to focus Participants perceived Leading for
Continuing Improvement, Organisation and
on balancing individual (local) needs versus
Management of Resources and Effective
their registered population’s health (‘bigger-
Teamworking as significantly more important
picture’ thinking), and will need to take on
for being a GP in the future compared to
multiple complex roles in future.
current perceived importance. However, of
Results show an increased potential for these, Leading for Continuing Improvement
role conflict in relation to ethical values, and Organisation and Management of
whereby GPs are required to demonstrate Resources were judged less important as
commitment to patient care, which may selection criteria, with more emphasis on
at times conflict with managing limited these domains being addressed within the
resources. Similarly, GPs need to maintain education curriculum and training pathway.
patient trust, which may also conflict with
ensuring Professional Integrity relating to Strengths and limitations
resource management. GPs are required A previously validated method was employed
to adopt an increasingly holistic approach and an extended sample of GPs and patient
British Journal of General Practice, May 2013 e336
representatives were recruited from across These two components have consistently
the UK, including observation in practices been shown to be linked to work-related
in both urban and rural locations. For stress, reduced job satisfaction and
practical reasons, a convenience sample burnout.27 Results show an increased
was recruited, the majority of whom potential for role conflict, especially relating
were from the GP community. It was not to ethical values, where there is increased
feasible to administer the questionnaire emphasis on GPs taking responsibility for
to patient representatives, for example. balancing what is good for individuals versus
It is conceivable that patients would rate what is good for the broader community in
the relative importance of competency a climate of heavily restricted resources.
domains differently, which is an important This presents competing job demands, for
consideration for further research. The example, where there is a need to balance
patient representatives who took part in the a commitment towards patient care versus
interviews were also a convenience sample managing limited resources effectively. The
from a single Deanery. results also demonstrate a significantly
increased emphasis on management and
Comparisons with existing literature business skills within the GP role, reflecting
The issue of increased role breadth is a topic the requirement for UK GPs to take a closer
not unique to medicine, as research shows account of cost-effectiveness and be more
that a common challenge for many high closely involved in managing commissioning
stakes job roles is in how best to train and activities, which may be at odds with their
develop individuals to perform in new and identity as clinicians.
more complex ways.22 Research consistently
shows that effective performance of high Implications for future practice
stakes job roles requires employees who are Results indicate that all areas of the
sufficiently confident in their abilities to take previously published competency model
on broader duties, and here, the concept continue to be perceived as important
of self-efficacy is an increasingly important and the key priorities for selection criteria
construct to evaluate.23 Self-efficacy refers are largely unchanged, with empathy,
to people’s judgements about their capability communication skills, and integrity being
to perform particular tasks, and evidence rated as most important in selection. Hence,
shows that job holders who feel capable of relatively light-touch updates are required
performing particular tasks will perform to the selection criteria in future, but these
them better,24 will persist at them in the face updates must reflect the increased role
of adversity,25 and will cope more effectively breadth of GPs. Selectors should also place
with change.26 Therefore, this study more weighting on some domains, such as
proposes that self-efficacy is an important teamwork and leadership capabilities.
motivational construct to be considered in A more pressing need is to determine
the future education and training of GPs, how the greater breadth of capabilities can
as it influences individual goals, emotional be addressed during training to support and
reactions, effort, coping, well-being and equip future GPs. Results show the need
persistence. In future, research could to educate trainees in new domains such
evaluate a trainee’s role breadth self-efficacy as Leading for Continuing Improvement,
as part of the training evaluation process. which is not yet addressed within training.
This concerns the extent to which people Given the extensive and broad range of
feel confident that they are able to carry out responsibilities and capabilities required,
Funding
a broader and more proactive role, beyond there are now important implications for the
Not applicable.
traditionally prescribed requirements, and future configuration and potential extension
Ethical approval would allow training interventions to be of GP education and training. Further work
Ethics Committee at the Department of tailored accordingly. is urgently required to explore the optimal
Psychology, City University, London. Of perhaps more immediate concern for construction of the education, training and
trainers and employers is the increased career pathway to support trainees (and thus
Provenance
potential for role conflict and role ambiguity. patients) appropriately in the future.
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing
interests.
Discuss this article
Contribute and read comments about
this article on the Discussion Forum:
http://www.rcgp.org.uk/bjgp-discuss
e337 British Journal of General Practice, May 2013
REFERENCES 96(5): 927–940.
1. Buckman L. Changes to the GP contract threaten general practice in the UK. 15. Plint S, Patterson F. Identifying critical success factors for designing selection
BMJ 2012; 345: e7343. processes into postgraduate specialty training: the case of UK general practice.
Postgrad Med J 2010; 86(1016): 323–327.
2. Trumble S, Naccarella L, Brooks P. The future of the primary medical
workforce. BMJ 2011; 343: d5006. 16. Patterson F, Zibarras L, Carr V, et al. Evaluating candidate reactions to selection
practices using organizational justice theory. Med Educ 2011; 45(3): 289–297.
3. Toynbee P. GPs have reasons not to be so cheerful over commissioning plans.
BMJ 2010; 341: c3839. 17. Irish B, Patterson F. Selecting general practice specialty trainees: where next?
4. Department of Health. Equity and excellence: liberating the NHS. London: DoH, Br J Gen Pract 2010; 60(580): 849–852.
2010. 18. Patterson F, Carr V, Plint S. General practice competency validation exercise:
5. NHS (Institute for Improvement and Innovation). Medical Leadership technical report to GP National Recruitment Office. Sollihull: National
Competency Framework. 3rd edn. NHS Leadership Academy, 2010. Recruitment Office for GP Training, 2005.
6. Clark J, Armit K. Leadership competency for doctors: a framework. Leadersh 19. Ash RA. Job analysis in the world of work. In: S Gael (ed.). The job analysis
Health Serv 2010; 23(2): 115–29. handbook. New York: John Wiley and Sons, 1998: 3–13.
7. Department of Health. The functions of GP commissioning consortia: a working 20. Patterson F, Ferguson E, Thomas S. Using job analyses to identify core and
document. London: DoH, 2011. specific competencies for three secondary care specialties: Implications for
8. Royal College of General Practitioners. Medical generalism. Why expertise selection and recruitment. Med Educ 2008; 42(12): 1195–1204.
in whole person medicine matters. London: RCGP, 2012. http://www.rcgp. 21. Miles MB, Huberman AM. Qualitative data analysis: a sourcebook of new
org.uk/policy/rcgp-policy-areas/~/media/Files/Policy/A-Z%20policy/Medical- methods. Beverly Hills, CA: Sage, 1984.
Generalism-Why_expertise_in_whole_person_medicine_matters.ashx
22. Parker S. Enhancing role breadth self-efficacy: the roles of job enrichment and
(accessed 6 Mar 2013).
other organizational interventions. J Appl Psychol 1998; 83(6): 835–852.
9. Patterson F, Ferguson E, Lane P, et al. A competency model for General
Practice: implications for selection and development. Br J Gen Pract 2000; 23. Gist ME, Mitchell TR. Self-efficacy: a theoretical analysis of its determinants and
50(452): 188–193. malleability. Acad Manage Rev 1992; 17(2): 183–211.
10. Saultz JW, Albedaiwi W. Interpersonal continuity of care and patient satisfaction: 24. Barling J, Beattie R. Self-efficacy beliefs and job performance. J Organ Behav
a critical review. Ann Fam Med 2004; 2(5): 445–451. Manage 1983; 5(1): 41–51.
11. Smits A, Meyboom W, Mokkink H, et al. Medical versus behavioural skills: an 25. Lent RW, Brown SD, Larkin KC. Comparison of three theoretically derived
observation study of 75 general practitioners. Fam Pract 1991; 8(1): 14–18. variables in predicting career and academic behavior: Self-efficacy, interest
12. Ham C. Health care commissioning in the international context: lessons from congruence, and consequence thinking. J Couns Psychol 1987; 34: 293–298.
experience and evidence. Birmingham: University of Birmingham, 2007. 26. Hill T, Smith ND, Mann ME. Role of efficacy expectations in predicting the
13. Goodwin N, Ross S, Smith A. The quality of care in general practice capturing decision to use advanced technologies: The case of computers. J Appl Psychol
opinions from the front line. A King’s Fund report. London: King’s Fund, 2010. 1987; 72(2): 307–313.
14. Lievens F, Patterson F. The validity and incremental validity of knowledge 27. Jackson SE, Schuler RS. A meta-analysis and conceptual critique of research
tests, low-fidelity simulations, and high-fidelity simulations for predicting job on role ambiguity and role conflict in work settings. Organ Behav Hum Dec
performance in advanced-level high-stakes selection. J Appl Psychol 2011; Processes 1985; 26: 16–28.
British Journal of General Practice, May 2013 e338
You might also like
- 5 Signs Showing You May Suffer From Mental Slavery' by Dr. Amos WilsonDocument4 pages5 Signs Showing You May Suffer From Mental Slavery' by Dr. Amos Wilsonebitechukwudi100% (3)
- Jean Genet - Deathwatch-Faber & Faber (1961) PDFDocument38 pagesJean Genet - Deathwatch-Faber & Faber (1961) PDFValentin MarcosNo ratings yet
- Pastor. The History of The Popes, From The Close of The Middle Ages. 1891. Vol. 31Document540 pagesPastor. The History of The Popes, From The Close of The Middle Ages. 1891. Vol. 31Patrologia Latina, Graeca et Orientalis100% (1)
- Short Answer Questions CHCCSM004Document14 pagesShort Answer Questions CHCCSM004Tmg Preity100% (2)
- RTCDocument27 pagesRTCMaple De los SantosNo ratings yet
- AHP Calculator - Example in The Lecture - 1Document24 pagesAHP Calculator - Example in The Lecture - 1Afranur ErenNo ratings yet
- NCMB 419 Week 11 CU10Document23 pagesNCMB 419 Week 11 CU10GERALDINE GONZALESNo ratings yet
- Blending Online Asynchronous and Synchronous Learning PDFDocument24 pagesBlending Online Asynchronous and Synchronous Learning PDFAnonymous GOUaH7FNo ratings yet
- Assessment of Critical Success Factors For Construction Projects in PakistanDocument13 pagesAssessment of Critical Success Factors For Construction Projects in PakistanAbdul Qayoom Memon100% (1)
- Nurse Education Today: Carole Irwin, Julie Bliss, Karen PooleDocument12 pagesNurse Education Today: Carole Irwin, Julie Bliss, Karen PooleAndi Fajrin PermanaNo ratings yet
- Education and Training of Clinical and Translational Study Investigators and Research Coordinators A Competency-Based Approach.Document10 pagesEducation and Training of Clinical and Translational Study Investigators and Research Coordinators A Competency-Based Approach.Luis FelipeNo ratings yet
- 2020 1830048 PDFDocument14 pages2020 1830048 PDFMarietou SidibeNo ratings yet
- Facilitating Case Studies in Massage Therapy CliniDocument5 pagesFacilitating Case Studies in Massage Therapy ClinijorgenovachrolloNo ratings yet
- The Effectiveness of A Short Cognitive Behavioural TrainingDocument27 pagesThe Effectiveness of A Short Cognitive Behavioural TrainingArinze7No ratings yet
- The Implementation of Mindfulness-Based Cognitive Therapy: Learning From The UK Health Service ExperienceDocument9 pagesThe Implementation of Mindfulness-Based Cognitive Therapy: Learning From The UK Health Service ExperienceRutekNo ratings yet
- Wrightetal Acad Med GMC2012Document11 pagesWrightetal Acad Med GMC2012d_kourkoutasNo ratings yet
- Apn IcnDocument42 pagesApn IcnJohn Mark LingconNo ratings yet
- Clarkson 2004Document4 pagesClarkson 2004Claudia SilveraNo ratings yet
- 4-Global Leadership in IPECP Research An Intro To Co-Creation of BestDocument8 pages4-Global Leadership in IPECP Research An Intro To Co-Creation of BestodetNo ratings yet
- 1734 13 7495 2 10 20180324Document11 pages1734 13 7495 2 10 20180324Lieven VermeulenNo ratings yet
- 10005038measuringprofessionalismasamulti Dimensionalconstruct PDFDocument102 pages10005038measuringprofessionalismasamulti Dimensionalconstruct PDFJanry SimanungkalitNo ratings yet
- Oup Accepted Manuscript 2020Document8 pagesOup Accepted Manuscript 2020Yusril AhmadNo ratings yet
- The Effects of Pay-for-Performance Programs On Health, Health Care Use, and Processes of CareDocument14 pagesThe Effects of Pay-for-Performance Programs On Health, Health Care Use, and Processes of CareMasrun FatanahNo ratings yet
- E013318 FullDocument25 pagesE013318 FullKarina Mejía EscobarNo ratings yet
- How Effect Size Practical Significance Misleads Clinical Practice The Case For Switching To Practical Benefit To Assess Applied Research FindingsDocument13 pagesHow Effect Size Practical Significance Misleads Clinical Practice The Case For Switching To Practical Benefit To Assess Applied Research FindingsDami TepedeNo ratings yet
- Which Patients Miss Appointments With General Practice and The Reasons WhyDocument7 pagesWhich Patients Miss Appointments With General Practice and The Reasons WhyR. H.No ratings yet
- Interpersonal SkillsDocument3 pagesInterpersonal Skillsluciana fardilaNo ratings yet
- Interpersonal SkillsDocument2 pagesInterpersonal SkillsUmarameshKNo ratings yet
- Nurs FPX 4010 Assessment 2 Interview and Interdisciplinary Issue IdentificationDocument4 pagesNurs FPX 4010 Assessment 2 Interview and Interdisciplinary Issue Identificationalicecullen3No ratings yet
- NRSG 7200 EmilyharamesdnpprojectpaperDocument14 pagesNRSG 7200 Emilyharamesdnpprojectpaperapi-582004140No ratings yet
- Acp Led Therapeutic Parenthesis: Advanced Clinical Practice MSCDocument35 pagesAcp Led Therapeutic Parenthesis: Advanced Clinical Practice MSCJoana SilvaNo ratings yet
- Using Field Notes To Evaluate Competencies in Family Medicine Training: A Study of Predictors of IntentionDocument10 pagesUsing Field Notes To Evaluate Competencies in Family Medicine Training: A Study of Predictors of IntentionMirna Liliana Carmona GarciaNo ratings yet
- Are Physiotherapy Students Adequately Prepared To Successfully Gain Employment? Mandy Jones, Judith Mcintyre, Sandra NaylorDocument13 pagesAre Physiotherapy Students Adequately Prepared To Successfully Gain Employment? Mandy Jones, Judith Mcintyre, Sandra NaylorMilan AnandNo ratings yet
- Capability Beliefs On, and Use of Evidence-Based Practice Among Four Health Professional and Student Groups in Geriatric Care: A Cross Sectional StudyDocument16 pagesCapability Beliefs On, and Use of Evidence-Based Practice Among Four Health Professional and Student Groups in Geriatric Care: A Cross Sectional StudynofitaNo ratings yet
- Addington Et Al-2018-Early Intervention in PsychiatryDocument8 pagesAddington Et Al-2018-Early Intervention in PsychiatryLink079No ratings yet
- PDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateDocument5 pagesPDSA Improvement Plan - Kingston General Hospital: Name Institution Course Professor DateNilanjana ChakrabortyNo ratings yet
- 10th Biennial Monash Pharmacy Education Symposium 2019Document68 pages10th Biennial Monash Pharmacy Education Symposium 2019muveszsziNo ratings yet
- 10 1111@jhn 12756Document10 pages10 1111@jhn 12756Federico CilloNo ratings yet
- Career Goals and Student Perceptions of A Post-ProDocument20 pagesCareer Goals and Student Perceptions of A Post-ProCarlos Miguel SumagueNo ratings yet
- Workplace CounsellingDocument5 pagesWorkplace CounsellingUmi AfidaNo ratings yet
- Health Coaching in Pharmacy Practice: A Systematic ReviewDocument14 pagesHealth Coaching in Pharmacy Practice: A Systematic ReviewrujaklutisNo ratings yet
- The Barrier To Implementation of Evidence-Based Practice Among Novice TherapistsDocument11 pagesThe Barrier To Implementation of Evidence-Based Practice Among Novice TherapistsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1-S2.0-S1939865422000315-MainDocument8 pages1-S2.0-S1939865422000315-MainnersrosdianaNo ratings yet
- Competency-Based Medical Education and Continuing Professional Development: A Conceptualization For ChangeDocument8 pagesCompetency-Based Medical Education and Continuing Professional Development: A Conceptualization For ChangeNader Elbokle100% (1)
- Hee Kim, Yeon. Effects of A Work-Based Critical Reflection Program For Novice NursesDocument6 pagesHee Kim, Yeon. Effects of A Work-Based Critical Reflection Program For Novice Nursescantoni1No ratings yet
- Using Staffing Ratios For Workforce Planning: Evidence On Nine Allied Health ProfessionsDocument8 pagesUsing Staffing Ratios For Workforce Planning: Evidence On Nine Allied Health ProfessionstikamdxNo ratings yet
- Py For Qualitu AMJDocument12 pagesPy For Qualitu AMJsunnyNo ratings yet
- Developing A Theory-Based Instrument To Assess The Impact of Continuing Professional Development Activities On Clinical Practice: A Study ProtocolDocument6 pagesDeveloping A Theory-Based Instrument To Assess The Impact of Continuing Professional Development Activities On Clinical Practice: A Study ProtocolSjktraub PahangNo ratings yet
- tmp7BD7 TMPDocument25 pagestmp7BD7 TMPFrontiersNo ratings yet
- 1.evidencebased Practices in Cognitive Behaviour Therapy CBT Case Formulation What Do Practitioners Believe Is Important and What Do They DoDocument21 pages1.evidencebased Practices in Cognitive Behaviour Therapy CBT Case Formulation What Do Practitioners Believe Is Important and What Do They DoGabriela RodriguezNo ratings yet
- Estudio Cualitativo Del Portafolio Que Explora Las Recomendaciones de Los Funcionarios ResponsablesDocument9 pagesEstudio Cualitativo Del Portafolio Que Explora Las Recomendaciones de Los Funcionarios ResponsablesFalconSerfinNo ratings yet
- 2014 Eberhart DNP Final Project PDFDocument81 pages2014 Eberhart DNP Final Project PDFaya PermatasariNo ratings yet
- Participatory Action ResearchDocument9 pagesParticipatory Action ResearchGilbert BaltazarNo ratings yet
- ACGME Outcome ProjectDocument8 pagesACGME Outcome ProjectsrisetyaNo ratings yet
- Graduate Radiographers' Expectations For Role Development e The Potential Impact of Misalignment of Expectation and Valence On Staff Retention and Service ProvisionDocument8 pagesGraduate Radiographers' Expectations For Role Development e The Potential Impact of Misalignment of Expectation and Valence On Staff Retention and Service ProvisionVincent OkekeNo ratings yet
- Evid Based Pract Final Feb 05Document41 pagesEvid Based Pract Final Feb 05Mus OubNo ratings yet
- The Right Place at The Right TimeDocument4 pagesThe Right Place at The Right TimeNian S KoNo ratings yet
- cg6 - Bmjopen-2016-012591Document7 pagescg6 - Bmjopen-2016-012591Mihalache Dan StefanNo ratings yet
- Comms Skills ReportDocument37 pagesComms Skills ReportbrendaNo ratings yet
- IPE Interprofessional EducationDocument10 pagesIPE Interprofessional EducationdewaNo ratings yet
- Jurnal Triad of Concern 2 PDFDocument10 pagesJurnal Triad of Concern 2 PDFKharina AreeistyNo ratings yet
- Education and Professional Development Strategy PDFDocument25 pagesEducation and Professional Development Strategy PDFColeen Ann BagasolNo ratings yet
- Stages of Milestones Implementation: A Template Analysis of 16 Programs Across 4 SpecialtiesDocument32 pagesStages of Milestones Implementation: A Template Analysis of 16 Programs Across 4 Specialtiesjustin76No ratings yet
- InternshipDocument8 pagesInternshipmahmoudNo ratings yet
- Factors Influencing Advanced Practitioners' Ability To Enact Leadership: A Case Study Within Irish HealthcareDocument12 pagesFactors Influencing Advanced Practitioners' Ability To Enact Leadership: A Case Study Within Irish HealthcareKarymeow1No ratings yet
- The Journey To Becoming An Adult Learner: From Dependent To Self-Directed LearningDocument3 pagesThe Journey To Becoming An Adult Learner: From Dependent To Self-Directed LearningAnonymous GOUaH7FNo ratings yet
- Adult Learning in Health Professions Education: Laura L. BieremaDocument14 pagesAdult Learning in Health Professions Education: Laura L. BieremaAnonymous GOUaH7FNo ratings yet
- Emerging Pedagogies For Effective Adult Learning: From Andragogy To HeutagogyDocument6 pagesEmerging Pedagogies For Effective Adult Learning: From Andragogy To HeutagogyAnonymous GOUaH7FNo ratings yet
- Friedman - Medical Humanities in CurriculumDocument3 pagesFriedman - Medical Humanities in CurriculumAnonymous GOUaH7FNo ratings yet
- Contribution To Setting Up A Sustainable Learning in An Eco-Neighbourhood Development Plan Based On "Serious Game"Document16 pagesContribution To Setting Up A Sustainable Learning in An Eco-Neighbourhood Development Plan Based On "Serious Game"Anonymous GOUaH7FNo ratings yet
- 4CID Model in Communication Skills CourseDocument8 pages4CID Model in Communication Skills CourseAnonymous GOUaH7FNo ratings yet
- Koczwara - Et - Al-2012-Medical - Education - Dr. SyntiaDocument10 pagesKoczwara - Et - Al-2012-Medical - Education - Dr. SyntiaAnonymous GOUaH7FNo ratings yet
- Assessment of Professionalism A Consolidation of Current ThinkingDocument6 pagesAssessment of Professionalism A Consolidation of Current ThinkingAnonymous GOUaH7FNo ratings yet
- 4CID Model AMEE GuideDocument17 pages4CID Model AMEE GuideAnonymous GOUaH7FNo ratings yet
- Situational Judgement Tests in Medical Education and Training: Research, Theory and Practice: AMEE Guide No. 100Document16 pagesSituational Judgement Tests in Medical Education and Training: Research, Theory and Practice: AMEE Guide No. 100Anonymous GOUaH7FNo ratings yet
- Pengaruh Metode Kombinasi Jigsaw Dan Concept Mapping Terhadap Prestasi BelajarDocument12 pagesPengaruh Metode Kombinasi Jigsaw Dan Concept Mapping Terhadap Prestasi BelajarAnonymous GOUaH7FNo ratings yet
- Blended Learning' As An Effective Teaching and Learning Strategy in Clinical Medicine: A Comparative Cross-Sectional University-Based StudyDocument6 pagesBlended Learning' As An Effective Teaching and Learning Strategy in Clinical Medicine: A Comparative Cross-Sectional University-Based StudyAnonymous GOUaH7FNo ratings yet
- Blended Learning For PostgraduateDocument7 pagesBlended Learning For PostgraduateAnonymous GOUaH7FNo ratings yet
- CSL Lab PDFDocument8 pagesCSL Lab PDFAnonymous GOUaH7FNo ratings yet
- Ats Scholar.2020 0046psDocument10 pagesAts Scholar.2020 0046psAnonymous GOUaH7FNo ratings yet
- Blended Learning For Medical ProfessionalsDocument2 pagesBlended Learning For Medical ProfessionalsAnonymous GOUaH7FNo ratings yet
- 26Document7 pages26Rinandar MusliminNo ratings yet
- ARTS10 WEEK3 A10PL-Ih-1Document15 pagesARTS10 WEEK3 A10PL-Ih-1rene nonatoNo ratings yet
- Marketing Strategy of Pepsi AssaignmentDocument48 pagesMarketing Strategy of Pepsi AssaignmentZekria Noori AfghanNo ratings yet
- Role-Play #1: Saving Energy: WellDocument4 pagesRole-Play #1: Saving Energy: WellDaniel VasquezNo ratings yet
- Theatres: 2 HellDocument10 pagesTheatres: 2 HellmooolkaNo ratings yet
- A. Biblical Studies C. Systematic Theology: TH THDocument2 pagesA. Biblical Studies C. Systematic Theology: TH TH謝樂知No ratings yet
- Happy Orere-Amadu 7&17 Professional CVDocument4 pagesHappy Orere-Amadu 7&17 Professional CVapi-284326863No ratings yet
- PIL Lecture Notes - Week 1Document3 pagesPIL Lecture Notes - Week 1Yoshita SoodNo ratings yet
- Chinese DragonDocument2 pagesChinese DragonwaiNo ratings yet
- Rizal Report - 19TH CenturyDocument25 pagesRizal Report - 19TH CenturyNamja PyosiNo ratings yet
- Jaltarang Instruments ShreyaDocument24 pagesJaltarang Instruments ShreyaKaushal DidwaniaNo ratings yet
- CBSE Class 2 EVS Our FestivalsDocument3 pagesCBSE Class 2 EVS Our FestivalsRakesh Agarwal100% (1)
- Rahail's ResumeDocument3 pagesRahail's ResumeRahailSalamatNo ratings yet
- An Informational Guide To Young Children's Outdoor Play SpacesDocument59 pagesAn Informational Guide To Young Children's Outdoor Play SpacesCristian NiculitaNo ratings yet
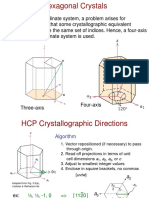
- Chap3.3 HexCrystal DirectionsDocument6 pagesChap3.3 HexCrystal DirectionsJeonghun LeeNo ratings yet
- Library Etymology - WiktionaryDocument4 pagesLibrary Etymology - WiktionarySamuel D. AdeyemiNo ratings yet
- Law437 Basic Features All PrintedDocument121 pagesLaw437 Basic Features All PrintedcfgqymsqdhNo ratings yet
- The Export Performance of Emerging Economy Firms The Influence of FirmDocument13 pagesThe Export Performance of Emerging Economy Firms The Influence of FirmJulio Jefrie Rojas SaraviaNo ratings yet
- Solution of IWTDocument6 pagesSolution of IWTreetikaNo ratings yet
- Mechanical Properties of Astm A572 Grade 65 SteelDocument123 pagesMechanical Properties of Astm A572 Grade 65 Steelcesarceron2003No ratings yet
- A Study On Customer Satisfaction Towards Parachute Hair Oil With Reference To Coimbatore CityDocument3 pagesA Study On Customer Satisfaction Towards Parachute Hair Oil With Reference To Coimbatore CityAbner Alexander Luiz86% (7)
- Chapter 1 To 3Document26 pagesChapter 1 To 3Hyman Jay Blanco100% (1)
- Tools Surveilans Hais Pencegahan & Pengendalian Infeksi 2021Document127 pagesTools Surveilans Hais Pencegahan & Pengendalian Infeksi 2021Yohana AnjaNo ratings yet
- Semi-Final NotesDocument6 pagesSemi-Final NotesRezel FuntilarNo ratings yet