Professional Documents
Culture Documents
Ventolin
Uploaded by
Taka0 ratings0% found this document useful (0 votes)
2 views4 pagesventolin
Original Title
ventolin
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentventolin
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
2 views4 pagesVentolin
Uploaded by
Takaventolin
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/273066274
Supraventricular tachycardia after nebulized salbutamol therapy in a neonate:
Case report
Article in Archivos Argentinos de Pediatría · April 2015
DOI: 10.1590/S0325-00752015000200018 · Source: PubMed
CITATIONS READS
4 1,170
5 authors, including:
Birgul Say Halil Degirmencioglu
Dr. Zekai Tahir Burak Women's Health Research and Education Hospital Dr. Zekai Tahir Burak Women's Health Research and Education Hospital
12 PUBLICATIONS 69 CITATIONS 32 PUBLICATIONS 341 CITATIONS
SEE PROFILE SEE PROFILE
Gozde Hayriye Kutman Nurdan Uras
Dr. Zekai Tahir Burak Women's Health Research and Education Hospital 229 PUBLICATIONS 2,636 CITATIONS
68 PUBLICATIONS 432 CITATIONS
SEE PROFILE
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
case report View project
Zekai Tahir Burak Women’s Health Education and Research Hospital newborn hearing screening results and assessment of the patients View project
All content following this page was uploaded by Birgul Say on 30 July 2018.
The user has requested enhancement of the downloaded file.
Case report Arch Argent Pediatr 2015;113(2):e98-e100 / e98
Supraventricular tachycardia after nebulized salbutamol
therapy in a neonate: Case report
Birgul Say MDa, Halil Degirmencioglu MDa, Hayriye Gozde Kanmaz Kutman MDa, Nurdan Uras MDa and
Ugur Dilmen MDa,b
ABSTRACT intervals, and absent P waves or an abnormal P
Supraventricular tachycardia (SVT) is the most common
wave axis. Salbutamol, which has been used as
sustained arrhythmia in neonates and infants. Presentation of
SVT in the neonate is usually subtle and frequently complicated bronchodilators for the prevention and treatment
by congestive heart failure. Despite the widespread use of of chronic lung disease in preterm infants, for
β2-agonists, their safety has been questioned. Several studies emergency treatment of hyperkalemia, and
have reported an increased incidence of cardiac arrhythmias in
transient tachypnea of the newborn (TTN),2-4 is a
patients treated with these agents, and other studies have found
increased rates of cardiovascular death associated with the use direct-acting sympathomimetic agent that has a
of oral and nebulized β2-agonists such as salbutamol, which is selective β-adrenergic effect. Because β-receptors
used to treat bronchospasm in newborns with several diseases. in the heart are mainly the β-1 type, it is believed
Herein, we report a case of SVT following administration of
that salbutamol has minimal cardiovascular
nebulized salbutamol in a neonate.
Keywords: tachycardia supraventricular, salbutamol, newborn. effects; however, tachycardia and cardiac
arrhythmias have been reported as complications
http://dx.doi.org/10.5546/aap.2015.eng.e98 of salbutamol administration. 5 Although well
documented in adults, cardiac arrhythmias have
INTRODUCTION not been widely reported in pediatric patients as
Supraventricular tachycardia (SVT) includes a complication of salbutamol therapy.
all forms of tachycardia originated above This paper presents the case of an infant who
the bifurcation of the bundle of His or have was admitted to the neonatal intensive care unit
mechanisms dependent on the bundle of His. (NICU) with a diagnosis of meconium aspiration
SVT is the most common sustained arrhythmia syndrome and who developed multiple SVTs
in neonates and infants. Predisposing factors such following administration of salbutamol during
as congenital heart disease, drug administration, the recovery phase of her underlying illness.
illness, and fever occur only in 15% of cases.1 The
presentation of SVT in the neonate is frequently CASE REPORT
subtle and it may include pallor, cyanosis, The patient was a girl born to a 28-year-old
restlessness, irritability, feeding difficulty, mother via a spontaneous vaginal delivery after
tachypnea, diaphoresis and grunting. SVT in a term gestation; the birth weight was 3600 g.
newborns is frequently complicated by congestive The mother was healthy and had an uneventful
heart failure, characterized by a fixed heart pregnancy. The baby was delivered through thick
rate usually greater than 230 beats per minute. meconium and she was cyanotic. Her mouth was
Typical electrocardiogram (ECG) findings of suctioned and she was intubated and suctioned
SVT include narrow QRS complexes, regular R-R for thick, particulate meconium. Her pulse fell
below 100 beats per minute (bpm) and positive-
pressure ventilation (PPV) was initiated. The
patient’s first and fifth Apgar scores were 5 and 6,
respectively and she was transferred to the NICU.
a. Division of Neonatology, Zekai Tahir Burak Maternity On admission to the NICU, the infant had a pulse
Teaching Hospital. of 157 (bpm), a respiration rate of 72 per minute,
b. Department of Pediatrics, Yıldırım Beyazıt University
School of Medicine and a mean arterial blood pressure of 34 mmHg.
Ankara,Turkey. She remained with 100% oxygen. A capillary
blood gas test showed a pH of 7.31, a PCO 2 of
E-mail Address:
Halil Degirmencioglu MD: hdegirmencioglu@gmail.com 43 mmHg, and a SpO 2 of 94% at 20 minutes
of life, and she was severely tachypneic. After
Conflict of Interest: None. intubation, a blood culture was taken, a sepsis
Received: 7-14-2014 evaluation was performed, and intravenous
Accepted: 11-3-2014 (IV) antibiotics (crystalline penicilline; 50,000
Case report / Arch Argent Pediatr 2015;113(2):e98-e100 / e99
units/kg/day in divided doses every 12 hours, administrations of adenosine treatment and
and gentamicine 4 mg/kg/day every 24 hours) electrical cardioversion was performed, which
were begun. Chest radiography revealed terminated the SVT. Salbutamol treatment was
dense bilateral infiltrates with prominent air ceased and SVT was never observed again. The
bronchograms. An echocardiogram at 10 hours of patient was doing well and was discharged from
life revealed septal hypertrophy with flattening of the hospital on day 15 of life.
the ventricular septum, consistent with persistent
pulmonary hypertension of the neonate (PPHN). DISCUSSION
Treatment was aimed at interrupting the cycle Despite the widespread use of β2-agonists,
of pulmonary vasoconstriction and hypoxia. their safety has been questioned. Existing data
Her chest radiographs started to demonstrate a on the effects of these agents, especially those
reticulogranular pattern, and there was concern administered in an inhaled form, on myocardial
that she might have an element of surfactant electrophysiological properties are rare. 6
deficiency. Pharmacologically, however, inhaled salbutamol
Over the next several days, the need to can result in significant changes in cardiac
ventilate and oxygenate the patient gradually electrophysiological properties.6 Salbutamol has
decreased, and on day 7 of life, she was extubated been found to enhance atrioventricular nodal
to a nasal cannula. She had coarse bilateral breath conduction and to decrease atrioventricular nodal,
sounds with marked expiratory wheezing. The atrial, and ventricular refractoriness in addition to
cardiovascular examination was unremarkable, its positive chronotropic effects. b2-agonists also
the echocardiographic examination was normal, increase QT dispersion. All of these alterations
and serum potassium and the other electrolytes theoretically could contribute to the generation
were in the normal ranges at this time. Inhaled of tachycardia and tachyarrhythmias. Several
salbutamol therapy was initiated at a dose of studies have reported an increased incidence
0.15 mg/kg (0.45mg) every 4 hours. Following of cardiac arrhythmias in patients treated with
the inhalation of salbutamol solution (Ventolin the use of oral and nebulized β2-agonists. 5-7
nebules® 50, Glaxo Wellcome; Greenford, UK), A recent human study demonstrated that
the infant’s heart rate increased suddenly to salbutamol, a selective β2-agonist, administered
314 bpm. The ECG showed a narrow complex by nebulizer has significant electrophysiological
tachycardia at a heart rate of 310 bpm and effects on the atrium, nodes, and ventricle.
retrograde conducted P waves buried in the ST Some studies found that salbutamol produced
segment at an RP interval (Figure 1). Adenosine more evident changes on the electrophysiologic
was administered via IV rapid bolus at a dose of properties of the sinus node compared with
100 mcg/kg which was repeated twice. However, the atrioventricular node.6,8 The cardiac effects
we were not able to obtain sinus rhythm of β2-agonists include tachycardia, atrial and
despite the raised dose for the two subsequent ventricular ectopic complexes, and atrial and
ventricular arrhythmias.6,9
Although adverse drug reactions including
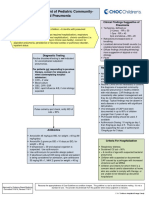
Figure 1. Electrocardiogram indicative of supraventricular tremor (90%), hypokalaemia (45.5%), and
tachycardia, with no visible P wave and normal QRS supraventricular tachycardia (21%) were reported
morphology. to be common, especially after administration of
continuous intravenous infusion of salbutamol,10
the estimated SVT rate in children treated
with inhaled β2-agonists remains unknown.
Tachycardia and tachyarrhythmias are very
common in critically ill adult patients with
various conditions. 11 Predisposing factors for
SVT include congenital heart disease, fever, and
sympathomimetics.8,12 Our patient had no history
of congenital heart disease or fever. Although
she required brief PPV in the delivery room and
respiratory support and she suffered from mild
PPHN, her myocardial functions and cardiac
output were always within normal limits, and
e100 / Arch Argent Pediatr 2015;113(2):e98-e100 / Case report
no signs were observed of myocardial ischemia, REFERENCES
which could cause a tendency toward arrhythmia. 1. Moak JP. Supraventricular tachycardia in the neonate and
infant. Prog Pediatr Cardiol 2000;11(81):25-38.
Acute management of SVT in children involves
2. Armangil D, Yurdakök M, Korkmaz A, Yigit S, et al. Inhaled
the use of vagal maneuvers or IV adenosine. IV beta-2 agonist salbutamol for the treatment of transient
adenosine has been found to be safe and highly tachypnea of the newborn. J Pediatr 2011;159(3):398-403.
effective in the management of SVT in infants and 3. Ng G, da Silva O, Ohlsson A. Bronchodilators for the
prevention and treatment of chronic lung disease in preterm
children.5
infants. Cochrane Database Syst Rev 2012;6:CD003214.
Two previous patient reports have described 4. Vemgal P, Ohlsson A. Interventions for non-oliguric
salbutamol-induced SVT in children. In the hyperkalaemia in preterm neonates. Cochrane Database
first report, SVT in a 19-month-old baby was Syst Rev 2012;5:CD005257.
5. Duane M, Chandran L, Morelli PJ. Recurrent supraventricular
converted by applying facial ice, and in the
tachycardia as a complication of nebulized albuterol
second case, a 4-year-old patient recovered with treatment. Clin Pediatr (Phila) 2000;39(11):673-7.
IV adenosine. 5,6 We initially administered a 6. Kallergis EM, Manios EG, Kanoupakis EM, Schiza SE, et
100 mcg/kg dose of IV adenosine, and despite al. Acute electrophysiologic effects of inhaled salbutamol
in humans. Chest 2005;127(6):2057-63.
two repeated doses of 200 mcg/kg, we could
7. Salpeter SR, Ormiston TM, Salpeter EE. Cardiovascular
not obtain sinus rhythm. Cardioversion was effects of b-agonists in patients with asthma and COPD:
performed with 2j/kg followed by 4j/kg, and this a meta-analysis. Chest 2004;125(6):2309-21.
treatment was successful. 8. Lowe MD, Rowland E, Brown MJ, Grace AA. Beta(2)
adrenergic receptors mediate important electrophysiological
Although nebulized, short-acting β2-agonists
effects in human ventricular myocardium. Heart
are effective bronchodilator drugs that are widely 2001;86(1):45-51.
prescribed for the treatment of airflow obstruction 9. Keller KA, Bhisitkul DM. Supraventricular tachycardia:
and increasingly for TTN and hyperkalemia in a complication of nebulized albuterol. Pediatr Emerg Care
1995;11(2):98-9.
NICUs, there is considerable concern about their
10. Habashy D, Lam LT, Browne GJ. The administration
potential side effects, particularly those pertaining of beta2-agonists for paediatric asthma and its adverse
to heart rate and arrhythmias. In addition, β2 reaction in Australian and New Zealand emergency
agonists are widely used to treat neonates with departments: a cross-sectional survey. Eur J Emerg Med
2003;10(3):219-24.
bronchopulmonary dysplasia, but there is no
11. Khorfan FM, Smith P, Watt S, Barber KR. Effects of nebulized
evidence of their efficacy. bronchodilator therapy on heart rate and arrhythmias in
Therefore, we suggest that all infants should critically ill adult patients. Chest 2011;140(6):1466-72.
be carefully monitored for tachycardia which 12. Flatt A, Crane J, Purdie G, Kwong T, et al. The cardiovascular
effects of beta adrenergic agonist drugs administered by
requires urgent treatment after nebulized
nebulisation. Postgrad Med J 1990;66(772):98-101.
salbutamol in both ambulatory and inpatient
care, even if there are no underlying causes.
Underlying causes that might facilitate
arrhythmia should be evaluated.n
View publication stats
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Changes in Infectious Disease Mortality In.5Document5 pagesChanges in Infectious Disease Mortality In.5TakaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Tujuan Pembangunan Milenium: (Millenium Development Goals, MDGS)Document12 pagesTujuan Pembangunan Milenium: (Millenium Development Goals, MDGS)TakaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Erlen Rosance Faturaja. Tugas Farmasi KlinikDocument1 pageErlen Rosance Faturaja. Tugas Farmasi KlinikTakaNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Outpatient Management of Pediatric Community-Acquired PneumoniaDocument2 pagesOutpatient Management of Pediatric Community-Acquired PneumoniaTakaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Erlen Rosance Faturaja. Tugas Farmasi KlinikDocument1 pageErlen Rosance Faturaja. Tugas Farmasi KlinikTakaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Type 2 Diabetes Mellitus and Psychological Stress - A Modifiable Risk FactorDocument15 pagesType 2 Diabetes Mellitus and Psychological Stress - A Modifiable Risk FactorTakaNo ratings yet
- The Biopharmaceutical Anomaly: FeatureDocument8 pagesThe Biopharmaceutical Anomaly: FeatureTakaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- IFCCstd PDFDocument4 pagesIFCCstd PDFPaulina LizzethNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- GratitudeJournalingIntervention Schache2019Document5 pagesGratitudeJournalingIntervention Schache2019TakaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Glycated Hemoglobin.....Document9 pagesGlycated Hemoglobin.....TakaNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Use of Glycated Haemoglobin (Hba1C) in The Diagnosis of Diabetes MellitusDocument25 pagesUse of Glycated Haemoglobin (Hba1C) in The Diagnosis of Diabetes MellitusSiskawati Suparmin100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Therapies For Type 2 Diabetes: Lowering Hba1C and Associated Cardiovascular Risk FactorsDocument13 pagesTherapies For Type 2 Diabetes: Lowering Hba1C and Associated Cardiovascular Risk FactorsTakaNo ratings yet
- Hba Standardisation: History, Science and Politics: CommentaryDocument6 pagesHba Standardisation: History, Science and Politics: CommentaryTakaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Therapies For Type 2 Diabetes: Lowering Hba1C and Associated Cardiovascular Risk FactorsDocument13 pagesTherapies For Type 2 Diabetes: Lowering Hba1C and Associated Cardiovascular Risk FactorsTakaNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- HHS Public Access: Stress and A1c Among People With Diabetes Across The LifespanDocument16 pagesHHS Public Access: Stress and A1c Among People With Diabetes Across The LifespanTakaNo ratings yet
- The Role of A Community Pharmacist in Diabetes EducationDocument3 pagesThe Role of A Community Pharmacist in Diabetes EducationTakaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- PI e HBA1C - ONE 16 PDFDocument2 pagesPI e HBA1C - ONE 16 PDFTakaNo ratings yet
- Use of Glycated Haemoglobin (Hba1C) in The Diagnosis of Diabetes MellitusDocument25 pagesUse of Glycated Haemoglobin (Hba1C) in The Diagnosis of Diabetes MellitusSiskawati Suparmin100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- 2992 PDF PDFDocument4 pages2992 PDF PDFTakaNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Research in Social and Administrative Pharmacy: A B A ADocument11 pagesResearch in Social and Administrative Pharmacy: A B A AYusufAbdullahKhaidirNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Nihms 1044222 PDFDocument18 pagesNihms 1044222 PDFTakaNo ratings yet
- 2992 PDF PDFDocument4 pages2992 PDF PDFTakaNo ratings yet
- Pharmacists' Attitudes and Role in Diabetes Management in KuwaitDocument7 pagesPharmacists' Attitudes and Role in Diabetes Management in KuwaitTakaNo ratings yet
- Pharmacy 08 00193 v2 PDFDocument9 pagesPharmacy 08 00193 v2 PDFTakaNo ratings yet
- How Clinical Pharmacists Can Improve Outpatient Diabetes Care PDFDocument3 pagesHow Clinical Pharmacists Can Improve Outpatient Diabetes Care PDFTakaNo ratings yet
- Relationship Between Depression and Stress With Blood Sugar Levels in Patients With Diabetes Melitus 7841 PDFDocument5 pagesRelationship Between Depression and Stress With Blood Sugar Levels in Patients With Diabetes Melitus 7841 PDFTakaNo ratings yet
- Circoutcomes 115 002184 PDFDocument9 pagesCircoutcomes 115 002184 PDFTakaNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Role of Clinical Pharmacist in The Management of Type II Diabetes Mellitus and Its Outcomes PDFDocument7 pagesRole of Clinical Pharmacist in The Management of Type II Diabetes Mellitus and Its Outcomes PDFTakaNo ratings yet
- PAE Sulistyorini PDFDocument17 pagesPAE Sulistyorini PDFTakaNo ratings yet
- What On Earth Is A MainframeDocument132 pagesWhat On Earth Is A MainframeCarlos DantasNo ratings yet
- Munchies BrochureDocument28 pagesMunchies BrochureIbrahim Diaz LazoNo ratings yet
- Talent-Olympiad 9 Science SampleDocument12 pagesTalent-Olympiad 9 Science SampleFire GamingNo ratings yet
- COSO DefinEDDocument21 pagesCOSO DefinEDRefdy AnugrahNo ratings yet
- Tip Sheet March 2017Document2 pagesTip Sheet March 2017hoangvubui4632No ratings yet
- VDRL - Press. GaugesDocument9 pagesVDRL - Press. GaugesSourav RayNo ratings yet
- AC MachinesDocument32 pagesAC Machinesjoeney guardiarioNo ratings yet
- Damask: by ChenoneDocument17 pagesDamask: by ChenoneYasir IjazNo ratings yet
- No Experience ResumeDocument2 pagesNo Experience ResumeNatalia PantojaNo ratings yet
- A Review On Different Yogas Used in The Management of Mandali Damsa Vrana W.S.R. To KriyakaumudiDocument11 pagesA Review On Different Yogas Used in The Management of Mandali Damsa Vrana W.S.R. To KriyakaumudiTiya TiwariNo ratings yet
- Audit Committee and Corporate Governance: CA Pragnesh Kanabar Sir's The Audit Academy-CA Final AuditDocument17 pagesAudit Committee and Corporate Governance: CA Pragnesh Kanabar Sir's The Audit Academy-CA Final AuditPULKIT MURARKANo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- ENGLISH 4 (General & Specific Sentence, Main Idea & Key Sentence) )Document3 pagesENGLISH 4 (General & Specific Sentence, Main Idea & Key Sentence) )Analiza Dequinto BalagosaNo ratings yet
- Advanced Packaging Polymers: Product Selection GuideDocument12 pagesAdvanced Packaging Polymers: Product Selection GuideDKNo ratings yet
- Kitchen Equipment Handling and Maintaining Standard Procedure and PoliciesDocument2 pagesKitchen Equipment Handling and Maintaining Standard Procedure and PoliciesChef Chef75% (4)
- No ApprovedDocument154 pagesNo ApprovedAnnaNo ratings yet
- L&T Motor CatalogDocument24 pagesL&T Motor CatalogSanjeev DhariwalNo ratings yet
- Lesson Plan Defining and Non Relative Clauses XII (I)Document3 pagesLesson Plan Defining and Non Relative Clauses XII (I)mariaalexeli0% (1)
- Augmentation of Labour: Nabhan A, Boulvain MDocument8 pagesAugmentation of Labour: Nabhan A, Boulvain MMade SuryaNo ratings yet
- JHS Integrated Science Preamble, Jan 2012 - FinalDocument15 pagesJHS Integrated Science Preamble, Jan 2012 - Finalfrank adamsNo ratings yet
- NCP81205Document1 pageNCP81205Tom TomNo ratings yet
- CS1 Entity Level Controls SolutionsDocument16 pagesCS1 Entity Level Controls SolutionsPakistan Breaking News100% (6)
- Machine DesignDocument627 pagesMachine DesignlucarNo ratings yet
- Individual Reflection ScribdDocument4 pagesIndividual Reflection ScribdJamie Chan JieminNo ratings yet
- Subsea Pipeline Job DescriptionDocument2 pagesSubsea Pipeline Job DescriptionVijay_DamamNo ratings yet
- Architecture of Neural NWDocument79 pagesArchitecture of Neural NWapi-3798769No ratings yet
- Daewoo SJ-210H DSJ-6000LHMDocument44 pagesDaewoo SJ-210H DSJ-6000LHMMarco Antonio100% (5)
- Syllabus - Building Rehabilitation Anfd Forensic en - 220825 - 181244Document3 pagesSyllabus - Building Rehabilitation Anfd Forensic en - 220825 - 181244M O H A N A V E LNo ratings yet
- 7 ApportionmentDocument46 pages7 Apportionmentsass sofNo ratings yet
- CfoDocument13 pagesCfocarmen pirvanNo ratings yet
- Autodesk Design Review: About DWF and DWFXDocument7 pagesAutodesk Design Review: About DWF and DWFXNesreNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (23)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)