Professional Documents
Culture Documents
Process Analysis For A Hospital Emergency Department
Uploaded by
EponleeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Process Analysis For A Hospital Emergency Department
Uploaded by
EponleeCopyright:
Available Formats
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
Process analysis for a hospital Emergency Department
ANTONIO DI LEVA EMILIO SULIS
University of Turin University of Turin
Department of Computer Science Department of Computer Science
Corso Svizzera, 185 - Torino Corso Svizzera, 185 - Torino
ITALY ITALY
dileva@di.unito.it sulis@di.unito.it
Abstract: This paper provides an application of the BP-M* methodology to care pathway for patients in a health-
care Emergency Department. On the basis of an analysis of the context, a decision support framework made of
several Key Performance Indicators is performed. By using the model, managers were able to run different sce-
narios, to identify bottlenecks and to explore solutions that can lead to better performance. The model takes into
account not only the flow of patients but also: a) the timing of the activities and resources used (both personnel and
equipment), b) the severity of the patient’s pathology, c) the distribution in time of arrivals of patients. By running
several experiments with different configurations, the analysis of these scenarios has provided useful information
for management of the department and for the re-engineering of the process.
Key–Words: Business Process Management, Business Process Modeling, Process Analysis, Emergency Depart-
ment, Simulation
1 Introduction i.e. the emergency field. An aim of this paper is to
demonstrate the usefulness of our approach to analyze
In this paper we apply a methodology called BP-M* EDs.
(Business Process Methodology*) [6] to an Emer- EDs are facing to lack of resources, long wait
gency Department (ED) of a public hospital1 . A fea- times, overuse of emergency services. Workers often
ture of BP-M* concerns the use of simulation during complain dissatisfaction in an high stress work envi-
the analysis and the restructuring of processes. While ronment. Some patients could decide to leave without
several studies have shown the usefulness of computer being seen. These problems can lead to well-known
simulations, real case applications are still lacking, es- situations of inefficiency, medical risk, and financial
pecially in the field of public administration. At the loss [14].
same time the public sector is increasingly required
Several indicators coming from real data are ini-
to provide better services at lower cost, strengthen its
tially collected. With this information, we document
customer focus and monitor control processes.
the current situation as it is (As-Is model). Then, sim-
A core area for governments is healthcare, as ulation can be used to see how entities flow through
the topmost agenda includes providing and improving the system and to detect and understand inefficien-
healthcare facilities to the population. Nevertheless, cies, bottlenecks, constraints, and risks. Finally, the
in many countries costs are increasing in a resource- analysis of the As-Is model in different scenarios may
limited setting and improving performance become a suggest changes in the model and the effects can be
key element. For instance, the pre-crisis growth of studied without the commitment of any physical re-
OECD countries resulted in average public expendi- sources or interruption of the real system.
ture on health increasing at an annual rate of almost
The current work includes at least three main
4%. After 2010, growth in spending came almost to a
point of interests:
halt overall with reductions in many cases2 .
In this context, tools and techniques to help the
re-engineering process are urgently needed. We focus i. Real Data: we based the simulation on real
on one of the more complex area in a public hospital, data coming from the department under analysis.
Similar relevant works considered patient arrival
1
The case relates to a medium sized city (about 40,000 inhab- pattern based on the average of data collected
itants) located in northern Italy. from other hospitals [7], or adopted a constant
2
Cfr. OECD Health Statistics 2016, at pattern due to the unavailability of detailed data
http://www.oecd.org/els/health-systems/health-data.htm from the real system [15].
ISSN: 2367-8925 34 Volume 2, 2017
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
ii. Set of KPIs: a relatively high number of KPIs The validation of the simulation model includes
can be taken into account, in comparison with the comparison between indicators given by the model
similar works which include only a small subset, with real data. To evaluate simulation results, most
i.e. waiting time and/or length of stay. ED studies consider basic performance indicators as
the Length-of-Stay (the time from patient arrival to
iii. Costs: the simulation of the ED process includes patient’s discharge, shortened in LoS), the Door-To-
an analysis of ED staff and hospital services Doctor-Time (from patient arrival to seeing a doc-
based on real costs. Expenses for doctors, nurses tor or a mid-level provider, shortened in DTDT) and
and operators can be covered, as well as charges the amount of patients who Left Without Being Seen
for laboratory analysis, blood tests and radiolog- (LWBS).
ical examinations. A recent review identifies at least 202 indicators
The paper is organized as follows. Section 1.1 in- from 127 articles that belongs to main four typolo-
troduces a review of related work. In Section 2 we gies: satisfaction, process, structural, and outcome
briefly describe our methodology. Sections 3 focuses [18]. A wide set of Time intervals is detailed in [29].
on the simulation model, presenting the results of tests The most studied categories are process-related per-
with different scenarios. Section 4 discusses our re- formance indicators, as length of wait/stay or ED oc-
sults. cupancy/crowding. Nevertheless, most works include
only few indicators (an average of 1.6 KPIs per arti-
cle).
1.1 Related Work
The Process Modeling usually refers to methods, tech-
niques, and software used to analyse and support busi- 2 The BP-M* Methodology
ness processes. Typical procedures concern design, The BP-M* methodology analyses functional, behav-
control, and analysis of operational tasks which in- ioral, and organizational aspects of the object system,
volve humans, documents, organizations or applica- and it strongly enforces an event-driven process-based
tions [31]. A standard notation called Business Pro- approach as opposed to traditional function-based ap-
cess Modeling and Notation (BPMN) was created to proaches.
present business processes [3, 28]. BP-M* was briefly described in [6] and consists
Business Process simulation was already applied of four logically successive phases:
in industrial reengineering [27, 24]. The more com-
mon simulation modeling methods are System Dy- 1. Context Analysis
namics (SD) [9], Discrete Event Simulation (DES) The context analysis phase aims to fix the overall
[15], and Agent-Based Modeling (ABM) [11]. Sim- strategic scenario of the enterprise and to deter-
ulations demonstrated their utility in modeling public mine the organizational components which will
services [12], as in the cases of public administration be investigated.
process [17], political decision-making [25], contact
information for public health and social care services 2. Organizational Analysis and Process Engi-
[32]. In the Health sector, some applications include neering
the simulation of the functioning of healthcare clinics The purpose of this phase is the determination
[8], spreading of diseases [20], assessing costs of care of the activities that constitute the process and of
[21], planning radiation therapy treatment [33]. the causal relationships existing between them.
In addition to more traditional statistical ap- The process is then reconstructed starting from
proaches [19], DES emerged as an alternative method external input/output events and/or objects. A
to model EDs [2, 6, 23]. DES was already applied process must be validated with stakeholders in-
to improve the patient throughput time [26] or the volved in the process, using animation and simu-
scheduling of staff members [13], as well as to reduce lation of its specification, obtaining the so called
patient waiting times [7]. Other works deal with the As-Is model. This model provides managers and
impact of staff scheduling on overall utilization and engineers with an accurate model of the enter-
burnout issues [30]. Moreover, a simulation-based op- prise as it stands, out of which they can make: a)
timization to staff levels can be performed [10]. Some a good assessment of its current status and b) an
systems focused on the trade-offs between different accurate estimation of available capabilities.
alternatives such as adding more beds or altering the
admission rate [16]. Few studies deal with costs of 3. Process Diagnosis and Reorganization
personnel and equipment, as in [4] where personnel The purpose of this phase is to trace back from
costs and hospital total charges are considered. the problems highlighted in the previous phase
ISSN: 2367-8925 35 Volume 2, 2017
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
to possible solutions to be taken in order to re- Connecting Objects. Connecting objects are used
structure the As-Is model generating in this way to specify how flow objects interacts. A connector can
the new To-Be version. be a sequence, a message or an association. Sequence
and message flows are represented by arcs which im-
4. Information System and Workflow Imple- pose temporal constraints between flow objects. An
mentation association connects artifact objects to activities and
When the To-Be model has been approved, it has is represented by a dotted line.
to be transmitted to engineers for implementa- Swimlanes. Pools and lanes are used to group the
tion. In the BP-M* methodology, two implemen- primary modeling elements related to functional ca-
tation aspects are considered: 1) the specification pabilities or responsibilities. A Pool represents a par-
of the Information System environment, and 2) ticipant in a Process, it acts as a graphical container
the specification of the Workflow execution en- for partitioning a set of activities from other Pools. A
vironment. Lane is a sub-partition within a Pool which is used to
organize and categorize activities.
Because the aim of this paper is the analysis of a In our approach, BPMN was extended by insert-
real process, the treatment of patients in an emergency ing the possibility of introducing descriptors for each
department, we will deal primarily with Phase 2 of the element of the diagram in order to specify the seman-
BP-M* methodology and Phases 3 and 4 will not be tics of process execution and to introduce all the quan-
discussed. titative parameters of the process, i.e. the duration of
In the following, we describe the specification activities. In fact, the standard version of BPMN only
language used in the methodology and the set of KPIs allows the specification of the flow of activities but
adopted in our work. this is only one aspect of the system, it is also neces-
sary to take into account resources that the company
allocates to the process and workload characteristics
2.1 BPMN in order to proceed with the process simulation on a
discrete event simulator. The simulator used in our
A key element of BP-M* is the Process Diagram (PD), article is iGrafxProcess2015 [1] and its use and the
which is used to describe the process. The diagram BPMN language extensions will be illustrated with
is specified by the BPMN language [19] which is a the help of our case study.
graphical notation that describes the steps in a busi-
ness process. BPMN describes the end to end flow of
a business process. The notation has been specifically 2.2 Key Performance Indicators
designed to coordinate the sequence of processes and
the messages that flow between different process par- Key performance indicators (KPI) are measurements
ticipants in a related set of activities. used to identify and quantify business performance.
BPMN consists of four basic categories of graph- As illustrated in Table 1, we identified, for the ED,
ical elements: Flow Objects, Connecting Objects, three main categories of KPI: Outcome, Process/Time
Swimlanes and Artifacts. and Structural.
Flow Objects are events, activities, and gate- Among the outcome indicators, Mortality (Mor),
ways. An event is something that “happens” during Hospitalization (Hos) and Transfer (Tra) respectively
the course of a business process. Events affect the represent patients who die in the ED, are hospitalized
flow of the process in different moments: Start, In- in the wards or are transferred to other facilities (eg
termediate, and End. Events are simply represented other specialized hospitals). The rate of patients who
by circles with open centers to allow internal mark- abandon (LWBS) can be related to quality and patient
ers to differentiate them. Activities are single task satisfaction.
or sub-processes. The representation of an activity is The Process/Time category is related to total
a rounded-corner rectangle. A sub-process is distin- times the patient spends in the ED (Length of stay -
guished by a small plus sign in the bottom center of LoS, Length of work - LoWo and Length of Wait -
the shape. Finally, gateways are elements that control LoWa) and to the intervals between the crucial events
the flow of execution of the process. Internal Markers in the treatment like the arrival, the beginning and the
will indicate the type of behavior control. A gateway end of the triage, the pre-visit and the visit, and so on.
is represented by a diamond shape. Structural indicators describe the amount of pa-
Artifacts are used to provide additional informa- tients admitted in the ED (Adm), with their re-
tion about the process, such as data, text, inputs and lated Type of disease (Dis) and Severity of illness
outputs of activities. (Sev). Moreover, Resources allocated to activities
ISSN: 2367-8925 36 Volume 2, 2017
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
Table 1: KPIs by categories. Table 2: Staff in the ED model by lane, number of
Cat. KPI Abbr. workers and hourly labour costs per capita.
Left Without Being Seen LWBS Lane Staff Num Cost
Outcome
Mortality Mor ED Doctors 3 50
Hospitalisation Hos ED+TA Nurses (generic) 2 27
Transfer Tra TR+WA Nurses (specialized) 3 30
Length of stay LoS RA+EF Employee 2 25
Length of work LoWo IC+OB+EF Generic operators 4 20
Process/Time Intervals
Length of wait LoWa
Arrival – Init. triage A-I
Arrival – Visit DTDT 3 The Case Study
Arrival – Cl-dec (diagnosis) A-C The ED under study serves about 55,000 patients an-
Init.Triage – Triage completed ED Tri nually. Patients move through various sections of the
Pre-visit – Visit v-V department depending on the type of care they require.
Pre-visit – Cl-dec (diagnosis) v-C The main sections are the Registration area, the Triage
Pre-visit – Discharge v-Dis area and the ED (Visit area) which consists of 3 basic
Cl-dec (diagnosis)– Discharge C-Dis ambulatories (Medical, Orthopedic and Surgical).
Pre-visit – Hospitalization v-Hos Patients access to ED in the Registration Area.
Cl-dec (diagnosis)– Hospitalization C-Hos Then, a qualified nurse evaluates the Emergency
ED Admissions Adm Severity Index (ESI) and provides a pre-visit (Triage
Structural
Resources Res area). There are four classes of severity ranging from
“very high” (level 1) to “very low” (level 4). An em-
Types of Disease Dis
pirical data analysis shows a larger presence of “low”
Severity of illness Sev severity (73.5%), followed by “very low” (18.8%),
“high” (7.3%) and “very high” (0.4%) cases.
While some patients could decide to leave the ED
(only in not urgent cases, as for 3 and 4 ESI level
(Res) must be described in terms of types and num- cases) others continue in their path.
bers. Most cases are visited in the three basic ambu-
latories of the ED: orthopedics, surgery and general
In our approach, the initial setting of the As-Is medicine, but a smaller number of cases, however, is
model includes both Outcome and Structural KPIs. transferred in others internal clinics (ic). While most
This data can easily be obtained from the hospital in- patients are discharged (dis), some ones can be hos-
formation system. pitalized (hos) or transferred to external healthcare
structures (ef). Finally, very few patients die in the
By performing the process simulation, the sim- ED (dea). Immediately after triage or after the visit
ulator provides a complete set of results from which some patients may be moved to specialized internal
is easy to derive the simulated values of Process/Time clinics.
type KPIs. Comparing the simulated values with those Following interviews with managers, doctors and
detected experimentally in the department it is possi- nurses, and through an accurate quantitative analysis,
ble to evaluate the accuracy with which the As-Is pro- we were able to build the As-Is process model of the
cess model approximates what actually happens in the ED which is illustrated in Figure 1.
real world. The visit is a complex task, which is detailed in
the sub-process of Figure 2. It includes the collection
Once the As-Is model has been validated, it is of patient history (anamnesis), a preliminary diagno-
simple to run on the model several types of “What- sis and the assignment of a therapy. During the visit
If” analysis by changing the values of Structural KPIs. it is possible to request exams (i.e. blood test) and/or
For example, we can change the resources assigned to radiological tests.
the activities and the simulation allows us to see how
the values of Process/Time KPIs are changed. This 3.1 Human Resources
type of data is particularly useful in deciding how to
restructure the As-Is model, but the restructuring step The ED process includes several kinds of human re-
will not be considered in this paper. sources, from doctors to generic operators. To provide
ISSN: 2367-8925 37 Volume 2, 2017
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
Figure 2: The Visit sub-process.
Figure 3: Patient arrival in ED by hour.
walk-in and ambulance patients. The average arrival
pattern is modeled with a hourly distribution as de-
tailed in Figure 3.
Quantitative information on patients concerns as-
pects related to different categories or diagnosis:
Figure 1: The ED As-Is model. - Diagnosis correspond to four different kinds of
medical care. The main three ambulatories involved
are orthopedics (ort) with the 31,5% of all cases,
24-hour services, the ED requires operators working surgery (sur) with the 15,7%, and general medicine
in different shifts (8 hours a shift including a meal (med) with the 21,8%. The remaining patients (31%)
break). Basically, there are three shifts starting at are sent directly to the internal specialist clinics.
6 a.m., at 2 p.m. and at 10 p.m.. A total amount - Patients can exit the process in different ways.
of 14 workers are modeled accordingly to table 2 in 86% of patients are dismissed (shortened in “dis”
which staff costs have been introduced. The night in Figure 1), 12% are hospitalized to a ward (hos),
shift which starts at 10 p.m., involves 2 doctors, 2 0,2% are transferred to other clinics (ic) and few cases
generic nurses, 1 specialized nurse in the TA and 1 (0,03%) are moved to the morgue. In addition, some
generic operator. (1.7%) patients may choose to leave the ED due to,
for example, of excessive delays.This results in a loss
3.2 Patient Arrival of revenue for the hospital and potential risks for the
patient.
The arrival of patients is driven by three main charac-
teristics. First, it depends on seasonal illness or inci- 3.3 Activities
dents. Second, the flow fluctuates depending on days
of the week: more arrivals are observed on Mondays An ED includes both well standardized activities and
and Fridays than the rest of the week [5]. Third, two more complex ones. In the BP-M* methodology ac-
peaks are observed in morning/afternoon with a break tivities are characterized by their duration and the re-
during lunch time [22]. As we are interested in aggre- sources used to implement them. Moreover, some ac-
gated patient flow data, we do not distinguish between tivities depend also from the kind of disease. For in-
ISSN: 2367-8925 38 Volume 2, 2017
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
Table 3: Duration of activities (minutes) by level of Table 4: Simulated and real values of activities.
ESI. Simulation Real data
Activity ESI 3-4 ESI 1-2 value % value %
Register patients Tri(2,6,3) 0-2 Dismission 46,557 81.47 46,047 81.21
Evaluate urgency Tri(1,4,2) 0 Transfer to IC 3,064 5.36 2,977 5.25
Provide pre-visit 3-10 1-3 Hospitalize in ward 6,572 11.54 6,640 11.71
Manage outcome 7-15 2-4 Abandon 893 1.56 973 1.72
Hospitalize in ward 15 15 Transfer to EF 44 0.08 49 0.09
Transfer to morgue 7 7 Transfer to morgue 19 0.03 15 0.03
Search external facility 60-480 60-480 Total 57,148 100 56,701 100
Transfer to external facility 10 10
Collect history 1-4 1-2
Hypothesize diagnosis Tri(1,5,2) 1-2 Table 5: Simulation results for several scenarios.
b-D b+D b+N i10% i20% Em.
Take Blood Sample 3-8 1-2
Laboratory (delay) 5-15 3-5 Time +137.2 -3.7 -1.2 +2.8 +7.9 +70.7
Transfer to radiology Tri(5,15,8) 2-4 Costs -0.25 +0.2 +0.1 +2.6 +5.4 +12.7
Radiological exams (delay) 10-20 7-12
Establish diagnosis [med] 5-25 3-5 one year of activity of the department. As can be seen,
Establish diagnosis [sur] 3-12 3-5 results are in good agreement with the experimental
Establish diagnosis [ort] 3-7 3-5 values;
Define therapy 2-5 5-10 2) compare real and simulated data regarding
some critical KPIs. The LoS (Length of Stay), i.e.
the patient’s average time spent in the department, is
stance, to establish diagnosis is faster for orthopedic the most used metric. In our case the value obtained
or surgery patients, while others may require addi- with the simulation, about 82 min, is in good agree-
tional consultancy which increase the whole average ment with the real value, 82.8 min, derived from data
time. Table 3 summarizes different duration depend- in the information system.
ing on severity. In this Table two different probabil-
ity distributions are used, the triangular distribution
Tri(min,max,mode), and the uniform distribution in 3.5 What-If analysis
the remaining cases.
In the model, the execution order of activities (pa- In our experimental setting, several different scenarios
tient pathways) is controlled through the gateways. As are compared. Starting from the basic As-Is model,
in the case of the duration of the activities, the per- variables related to resources (adding or removing
centage of activation of the different pathways may some professionals) as well as to patient diseases have
depend on the patient’s severity. For example, in the been changed, obtaining the scenarios that will be dis-
Visit sub-process, requests for blood and/or radiolog- cussed below with reference to Table 5 which contains
ical exams are modeled accordingly to the type of pa- results of the simulations. For each scenario we indi-
tient’s disease. Abandons are modeled as a probabilis- cate the percentage difference from the value of the
tic function only for not urgent patients, having an ESI As-Is model, both for time and costs (costs are related
levels of 3 or 4 (0.7 and 3.5 percent probability, re- to personnel expenses, to medical consumables and to
spectively). physical examinations).
3.4 Validation of the model 3.5.1 Resource scenarios
As discussed before, the As-Is model includes both The variation of the staff is one of the most interest-
Outcome and Structural KPIs values obtained from ing experiment for an organization. We carried out
the hospital information system. In the BP-M* ap- three different scenarios, adding or removing a Doc-
proach, the validation of the As-Is model involves two tor (“b+D” and “b-D”), as well as adding a Nurse
steps: (“b+N”). Due to the small size of the ED, removing
1) verify that data concerning the Outcome and even one nurse is not possible as it cause a block in the
Structural KPIs had been properly considered in the model. The results show that an increment of a doc-
model. Table 4 shows the simulation results relative to tor increases performance times of about 4%, while
ISSN: 2367-8925 39 Volume 2, 2017
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
the increment of a nurse improves of 1%. Decreas- References:
ing a doctor have dramatic impact with a worsening
of about 130% of time. This justifies the fact that a [1] iGrafxProcess 2015. http://www.igrafx.com.
doctor is removed only in the night shift.
[2] W. Abo-Hamad and A. Arisha. Simulation-
based framework to improve patient experience
3.5.2 Patient scenarios in an emergency department. European Jour-
nal of Operational Research, 224(1):154–166,
By this experiment, we simulate an increment of some 2013.
kinds of patients’ disease. For instance, the spread
of influenza virus infection in winter time will in- [3] T. Allweyer. BPMN 2.0: introduction to the
crease the arrival of patients having specific needs. We standard for business process modeling. BoD–
slightly increase of 10 percentage points (“i+10%”) Books on Demand, 2016.
and 20% (“i+20%”) the arrival of patients’ directed to
the general medicine ambulatory, i.e. instead of or- [4] J. G. Anderson, W. Harshbarger, H. Weng, S. J.
thopedic or surgery. Finally, a last scenario (“Em”) Jay, and M. M. Anderson. Modeling the costs
simulates an emergency, where urgent cases increases and outcomes of cardiovascular surgery. Health
(10% for the ESI level 2 and 5% for the ESI 1). As ex- Care Management Science, 5(2):103–111, 2002.
pected, in both cases there is an impact over ED time
performances. [5] F. Chetouane and K. Barker. Integrating simula-
tion and risk-based sensitivity analysis methods
in hospital emergency department design, pages
3.5.3 Impact on operational costs 67–82. Springer Milan, Milano, 2012.
The analysis of results presented in Table 5 suggests [6] A. Di Leva, S. Femiano, et al. The bp-m*
that the impact of the changes is significant especially methodology for process analysis in the health
for what concerns the increase of patients (for exam- sector. Intelligent Information Management,
ple, in the case of epidemics). 3(02):56, 2011.
[7] C. Duguay and F. Chetouane. Modeling and
4 Conclusions improving emergency department systems us-
ing discrete event simulation. Simulation,
This paper shows how simulation techniques allow a 83(4):311–320, 2007.
quantitative analysis of the emergency department in
the public hospital of a medium-size Italian city. [8] R. B. Fetter and J. D. Thompson. The simula-
The article has demonstrated the validity of the tion of hospital systems. Operations Research,
BP-M* methodology for what concerns the construc- 13(5):689–711, 1965.
tion of an As-Is model of the process that describes the
patient care pathway in the department. The key fea- [9] J. W. Forrester. Industrial dynamics. Journal of
ture of the model is the ability to run the model with the Operational Research Society, 48(10):1037–
a discrete event simulator thereby obtaining an esti- 1041, 1997.
mate of the main indicators of the model to be com-
[10] K. Ghanes, O. Jouini, M. Wargon, and Z. Je-
pared with real values. In this way the model is a very
mai. Modeling and analysis of triage nurse or-
helpful environment for studying the behavior of the
dering in emergency departments. In Industrial
system in different working conditions obtaining use-
Engineering and Systems Management (IESM),
ful tips for management of the department and for the
2015 International Conference on, pages 228–
re-engineering of the process.
235. IEEE, 2015.
[11] G. N. Gilbert. Agent-based models. Number
5 Acknowledgments 153. Sage, 2008.
The Cittá della Salute e della Scienza of Turin (Italy) [12] T. R. Gulledge Jr and R. A. Sommer. Busi-
has funded the working group on the analysis of busi- ness process management: public sector impli-
ness processes, including the research work of Emilio cations. Business Process Management Journal,
Sulis. 8(4):364–376, 2002.
ISSN: 2367-8925 40 Volume 2, 2017
International Journal of Economics and Management Systems
Antonio Di Leva, Emilio Sulis http://www.iaras.org/iaras/journals/ijems
[13] W. M. Hancock and P. F. Walter. The use of com- [24] H. A. Reijers. Design and control of workflow
puter simulation to develop hospital systems. processes: business process management for the
ACM SIGSIM Simulation Digest, 10(4):28–32, service industry. Springer-Verlag, 2003.
1979.
[25] J. Rouchier and S. Thoyer. Votes and lobbying in
[14] N. R. Hoot and D. Aronsky. Systematic review the european decision-making process: applica-
of emergency department crowding: causes, tion to the european regulation on gmo release.
effects, and solutions. Annals of emergency Journal of Artificial Societies and Social Simu-
medicine, 52(2):126–136, 2008. lation, 9(3), 2006.
[15] J. Jun, S. H. Jacobson, and J. Swisher. Appli- [26] C. E. Saunders, P. K. Makens, and L. J. Leblanc.
cation of discrete-event simulation in health care Modeling emergency department operations us-
clinics: A survey. Journal of the operational re- ing advanced computer simulation systems. An-
search society, 50(2):109–123, 1999. nals of emergency medicine, 18(2):134–140,
1989.
[16] R. K. Khare, E. S. Powell, G. Reinhardt, and
M. Lucenti. Adding more beds to the emergency [27] A. W. Scheer and M. Nüttgens. Aris architec-
department or reducing admitted patient board- ture and reference models for business process
ing times: which has a more significant influence management. In Business Process Management,
on emergency department congestion? Annals of pages 376–389. Springer, 2000.
emergency medicine, 53(5):575–585, 2009.
[28] H. Smith and P. Fingar. Business process man-
[17] A. Kovacic and B. Pecek. Use of simulation agement: the third wave, volume 1. Meghan-
in a public administration process. Simulation, Kiffer Press Tampa, 2003.
83(12):851–861, 2007. [29] C. M. Sørup, P. Jacobsen, and J. L. For-
[18] M. Madsen, S. Kiuru, M. Castrèn, and L. Kur- berg. Evaluation of emergency department
land. The level of evidence for emergency de- performance–a systematic review on recom-
partment performance indicators: systematic re- mended performance and quality-in-care mea-
view. European Journal of Emergency Medicine, sures. Scandinavian journal of trauma, resus-
22(5):298–305, 2015. citation and emergency medicine, 21(1):1, 2013.
[30] M. Thorwarth, A. Arisha, and P. Harper. Sim-
[19] B. P. Model. Notation (bpmn) version 2.0. OMG
ulation model to investigate flexible workload
Specification, Object Management Group, 2011.
management for healthcare and servicescape en-
[20] M. E. Newman. Spread of epidemic disease vironment. In Proceedings of the 2009 Win-
on networks. Physical review E, 66(1):016128, ter Simulation Conference (WSC), pages 1946–
2002. 1956. IEEE, 2009.
[21] M. Pitt, T. Monks, S. Crowe, and C. Vasilakis. [31] W. M. Van der Aalst, J. Nakatumba, A. Rozinat,
Systems modelling and simulation in health ser- and N. Russell. Business process simulation. In
vice design, delivery and decision making. BMJ Handbook on Business Process Management 1,
quality & safety, 25(1):38–45, 2016. pages 313–338. Springer, 2010.
[32] M. Vinai and E. Sulis. Health and social
[22] O. Rado, B. Lupia, J. M. Y. Leung, Y.-H. Kuo,
public information office (spun) simula-
and C. A. Graham. Using Simulation to Analyze
tion, 2015 (accessed September 15, 2016).
Patient Flows in a Hospital Emergency Depart-
https://www.openabm.org/model/4778/version/2.
ment in Hong Kong, pages 289–301. Springer
International Publishing, Cham, 2014. [33] G. Werker, A. Sauré, J. French, and S. Shechter.
The use of discrete-event simulation modelling
[23] M. Raunak, L. Osterweil, A. Wise, L. Clarke, to improve radiation therapy planning pro-
and P. Henneman. Simulating patient flow cesses. Radiotherapy and Oncology, 92(1):76–
through an emergency department using 82, 2009.
process-driven discrete event simulation. In
Proceedings of the 2009 ICSE Workshop on
Software Engineering in Health Care, pages
73–83. IEEE Computer Society, 2009.
ISSN: 2367-8925 41 Volume 2, 2017
You might also like
- Procascamc00003 0526Document6 pagesProcascamc00003 0526Eduardo MonteiroNo ratings yet
- Articulo Lean Thinking en InglesDocument10 pagesArticulo Lean Thinking en InglesAntonella ParentiniNo ratings yet
- ADAPT@AGENT - HOSPITAL: Agent-Based Optimization and Management of Clinical ProcessesDocument23 pagesADAPT@AGENT - HOSPITAL: Agent-Based Optimization and Management of Clinical Processeswalaba06No ratings yet
- A Dimensional Data Model For Healthcare Revenue Cycle Analytics and Business Intelligence Joseph George A1Document6 pagesA Dimensional Data Model For Healthcare Revenue Cycle Analytics and Business Intelligence Joseph George A1Harsh WaghelaNo ratings yet
- Covid-19 Hospital Management SystemDocument74 pagesCovid-19 Hospital Management SystemMuhammed Ajmal67% (3)
- Systematic Mapping of Process Mining Studies in HealthcareDocument25 pagesSystematic Mapping of Process Mining Studies in HealthcareMiftachul IndrianiNo ratings yet
- Mast Et Al-2011-Quality and Reliability Engineering InternationalDocument12 pagesMast Et Al-2011-Quality and Reliability Engineering InternationalAnonymous 3O0J2YYNo ratings yet
- Literature Review On Hospital Management System ProjectDocument6 pagesLiterature Review On Hospital Management System Projectea46krj6No ratings yet
- Process Improvement in A Radiology Department: Hatice Camgoz-Akdag and Tu Ğçe BeldekDocument12 pagesProcess Improvement in A Radiology Department: Hatice Camgoz-Akdag and Tu Ğçe BeldekAditya ShuklaNo ratings yet
- DMAIC For Process Digitalization: A Hospital Case StudyDocument17 pagesDMAIC For Process Digitalization: A Hospital Case StudyGuillermo Luis AcostaNo ratings yet
- McConnel, Brendon and Vera-Hernandez (2015)Document53 pagesMcConnel, Brendon and Vera-Hernandez (2015)María Ignacia Valenzuela NavarroNo ratings yet
- Lean Six Sigma in HospitalDocument10 pagesLean Six Sigma in Hospitalterrac3211No ratings yet
- Master Thesis Rutger Van BreugelDocument83 pagesMaster Thesis Rutger Van BreugelTrần Tôn Phương TrâmNo ratings yet
- Hospital Operations Management: An Exploratory Study From Brazil and PortugalDocument10 pagesHospital Operations Management: An Exploratory Study From Brazil and PortugalQuality SaketNo ratings yet
- Process Modeling of The Health Sector Using BPMN: A Case StudyDocument6 pagesProcess Modeling of The Health Sector Using BPMN: A Case StudyIndra GunawanNo ratings yet
- Muito BomDocument3 pagesMuito BomSantos OliveiraNo ratings yet
- Critical Analysis of a Community Nursing Information SystemDocument5 pagesCritical Analysis of a Community Nursing Information SystemAgboola Ayobami AbiolaNo ratings yet
- Hospital Management SystemDocument23 pagesHospital Management SystemKhadiza ShakilaNo ratings yet
- Agile Six Sigma in Healthcare: Case Study at Santobono Pediatric HospitalDocument17 pagesAgile Six Sigma in Healthcare: Case Study at Santobono Pediatric HospitalGuillermo Luis AcostaNo ratings yet
- Simulation Modelling and Lean Management in HcareDocument20 pagesSimulation Modelling and Lean Management in HcareAtharva GaikwadNo ratings yet
- 14-Application of Process Mining in Healthcare - A Case Study in A Dutch Hospital - Mans - 2008Document14 pages14-Application of Process Mining in Healthcare - A Case Study in A Dutch Hospital - Mans - 2008Paul EncisoNo ratings yet
- Patient Care Information System and Health Care Work - A Sociotechnical ApproachDocument15 pagesPatient Care Information System and Health Care Work - A Sociotechnical ApproachPUSKESMAS JERUKNo ratings yet
- Medical Device Management SoftwareDocument6 pagesMedical Device Management SoftwareMuhammad IzzuddinNo ratings yet
- Information Systems For Public Sector Management: Working Paper SeriesDocument24 pagesInformation Systems For Public Sector Management: Working Paper SeriesMahesh ChaudhariNo ratings yet
- Public Sector Management Information SystemsDocument26 pagesPublic Sector Management Information SystemswisewastelmiracleNo ratings yet
- Analyzing Business Case and Feasibility of EMR SystemDocument3 pagesAnalyzing Business Case and Feasibility of EMR Systemchandini50% (4)
- Going Beyond Simple Sample Size Calculations: A Practitioner's GuideDocument56 pagesGoing Beyond Simple Sample Size Calculations: A Practitioner's GuideManuel BéjarNo ratings yet
- Improving Emergency Department Through Business PRDocument21 pagesImproving Emergency Department Through Business PRRares VasileNo ratings yet
- Process Mining Based Modeling and Analysis of W Orkflows in Clinical Care - A Case Study in A Chicago Outpatient ClinicDocument6 pagesProcess Mining Based Modeling and Analysis of W Orkflows in Clinical Care - A Case Study in A Chicago Outpatient ClinicNurFitrianti FahrudinNo ratings yet
- Case Study 3Document11 pagesCase Study 3sheilaNo ratings yet
- Integration of A Nationally Procured Electronic Health Record System Into User Work PracticesDocument12 pagesIntegration of A Nationally Procured Electronic Health Record System Into User Work PracticesPratiwi mongNo ratings yet
- A Financial Services OrganizationDocument11 pagesA Financial Services OrganizationMaritsa AmaliyahNo ratings yet
- Presentasi Big Data Analytics - Group 8Document32 pagesPresentasi Big Data Analytics - Group 8IloNo ratings yet
- What Is Operation Research? 2.what Is Production Management? 3.what Is The Difference Between Operation Research and Operational Research?Document6 pagesWhat Is Operation Research? 2.what Is Production Management? 3.what Is The Difference Between Operation Research and Operational Research?Justin ReyesNo ratings yet
- BPMN Process ModellingDocument3 pagesBPMN Process ModellingJane QuitonNo ratings yet
- 2 KijlDocument10 pages2 KijlZarah Alifani DzulhijjahNo ratings yet
- 10 1 1 126 788 PDFDocument31 pages10 1 1 126 788 PDFMahesh PradeepNo ratings yet
- Literature Review On Hospital Management SystemDocument7 pagesLiterature Review On Hospital Management SystemafdtsxuepNo ratings yet
- 5th Term - Operations ManagementDocument58 pages5th Term - Operations ManagementShreedharNo ratings yet
- HOSPITAL MANAGEMENT SYSTEMDocument30 pagesHOSPITAL MANAGEMENT SYSTEMDaniel braveNo ratings yet
- Semis Ni 2Document4 pagesSemis Ni 2Mel MelNo ratings yet
- Artículo Cirugía 1Document9 pagesArtículo Cirugía 1martinezli1533No ratings yet
- Towards Computer System-ValidationDocument16 pagesTowards Computer System-ValidationZaphod BeeblebroxNo ratings yet
- Resume Big Data Analytics - Group 8Document12 pagesResume Big Data Analytics - Group 8IloNo ratings yet
- Business Process Analytics A Dedicated Methodology Through A Case StudyDocument18 pagesBusiness Process Analytics A Dedicated Methodology Through A Case StudyelfowegoNo ratings yet
- Computers 11 00006Document21 pagesComputers 11 00006ThanujNo ratings yet
- Lean ManagmentDocument20 pagesLean Managmentفيصل الاعرجNo ratings yet
- MT AgapitosDocument43 pagesMT AgapitosYANNo ratings yet
- Towards Computer System-ValidationDocument16 pagesTowards Computer System-ValidationAnalista de ValidacionesNo ratings yet
- ABC in ServiceDocument6 pagesABC in ServiceCherrell LynchNo ratings yet
- Clinic DocumentsDocument17 pagesClinic Documentsanon_815273791No ratings yet
- PLANGKAT PROJECT WORK New YearDocument44 pagesPLANGKAT PROJECT WORK New YearAndrew OdoNo ratings yet
- Maintenance strategies overview focusing on concepts and approachesDocument14 pagesMaintenance strategies overview focusing on concepts and approachesThaierNo ratings yet
- The Balanced Scorecard: Innovative Performance Measurement and Management Control SystemDocument13 pagesThe Balanced Scorecard: Innovative Performance Measurement and Management Control Systemcok putriNo ratings yet
- J.2018. Using Six Sigma DMAIC Methodology and Discrete EventDocument18 pagesJ.2018. Using Six Sigma DMAIC Methodology and Discrete EventHadi P.No ratings yet
- Risk Management For Business Process Reengineering: The Case of A Public Sector OrganizationDocument11 pagesRisk Management For Business Process Reengineering: The Case of A Public Sector OrganizationMuhammad FirdianNo ratings yet
- Measuring Maintenance Performance) in Search For A Maintenance Productivity IndexDocument12 pagesMeasuring Maintenance Performance) in Search For A Maintenance Productivity Indexlospin1No ratings yet
- Data Analysis Algorithms For Revenue AssuranceDocument16 pagesData Analysis Algorithms For Revenue AssuranceHenry WishlyNo ratings yet
- B.1 Learning Objectives: System Life Cycle: at The End of The Lesson, The Student Should Be Able ToDocument73 pagesB.1 Learning Objectives: System Life Cycle: at The End of The Lesson, The Student Should Be Able ToPark Yoon AeNo ratings yet
- BKAN1013 Topik 2 Jahitan Ali business eventsDocument2 pagesBKAN1013 Topik 2 Jahitan Ali business eventsEponleeNo ratings yet
- Educational Attainment MapsDocument5 pagesEducational Attainment MapsEponleeNo ratings yet
- A192 BKAN1013 Summary Topik 1-3Document3 pagesA192 BKAN1013 Summary Topik 1-3EponleeNo ratings yet
- Scanned With Camscanner: Gym/If H 1Document3 pagesScanned With Camscanner: Gym/If H 1EponleeNo ratings yet
- Scanned With Camscanner: Gym/If H 1Document3 pagesScanned With Camscanner: Gym/If H 1EponleeNo ratings yet
- Process Analysis For A Hospital Emergency DepartmentDocument8 pagesProcess Analysis For A Hospital Emergency DepartmentEponleeNo ratings yet
- MathDocument2 pagesMathEponleeNo ratings yet
- Assessment Discrete Maths (A192 - Covid 19)Document1 pageAssessment Discrete Maths (A192 - Covid 19)EponleeNo ratings yet
- Asigment 1 (2c&3)Document2 pagesAsigment 1 (2c&3)EponleeNo ratings yet
- SQIT1013 IndividualDocument8 pagesSQIT1013 IndividualEponleeNo ratings yet
- Business Plan of Mineral Water PlantDocument27 pagesBusiness Plan of Mineral Water PlantHaytham FugahaNo ratings yet
- Group Assignment (5%) - (DUE DATE: 2 DECEMBER) : + 16t Feet. The Four Options To Be Provided by Buttons Are As FollowsDocument7 pagesGroup Assignment (5%) - (DUE DATE: 2 DECEMBER) : + 16t Feet. The Four Options To Be Provided by Buttons Are As FollowsEponleeNo ratings yet
- Hip ExaminationDocument7 pagesHip ExaminationWaqas Haleem100% (1)
- Highlights of key changes under the TRAIN LawDocument13 pagesHighlights of key changes under the TRAIN LawMiguel Anas Jr.No ratings yet
- Business DemographyDocument15 pagesBusiness DemographyNeha ShuklaNo ratings yet
- Dorothy JohnsonDocument9 pagesDorothy JohnsonMarianne Collantes BuendiaNo ratings yet
- Concure WB309 MSDSDocument7 pagesConcure WB309 MSDSAmeer KhanNo ratings yet
- How To Know If U Need Ortho TTDocument3 pagesHow To Know If U Need Ortho TTSubhajit SahaNo ratings yet
- Case Studies For PharmacyDocument3 pagesCase Studies For PharmacyMahima Sindhi50% (2)
- Introductory Lecture by DR Prafull VijayakarDocument139 pagesIntroductory Lecture by DR Prafull Vijayakarpredictive amar100% (1)
- ROO-ALL-HS-PRO-0025 REV 10 Ground Disturbance and Excavation Procedure - ...Document25 pagesROO-ALL-HS-PRO-0025 REV 10 Ground Disturbance and Excavation Procedure - ...Murtadda MohammedNo ratings yet
- Acutrak2 Radial Head Case StudyDocument2 pagesAcutrak2 Radial Head Case StudyDinesh KumarNo ratings yet
- Principles of Paragraph Writing IIIDocument15 pagesPrinciples of Paragraph Writing IIITitiek DwiNo ratings yet
- Ranah/ Domain D Iii KeperawatanDocument2 pagesRanah/ Domain D Iii KeperawatanMuhammad Moeharsah SNNo ratings yet
- Echo - Medical Supplies and Equipment For Primary Health CareDocument192 pagesEcho - Medical Supplies and Equipment For Primary Health CareKing Solomon CatralNo ratings yet
- Neurodegenerative Disease Among Male Elite Football (Soccer) Players in Sweden: A Cohort Study - TheDocument3 pagesNeurodegenerative Disease Among Male Elite Football (Soccer) Players in Sweden: A Cohort Study - Thepitufi11No ratings yet
- ABYIP-2023 TemplateDocument3 pagesABYIP-2023 Templatejomar88% (26)
- Anju Jose CV LatestDocument3 pagesAnju Jose CV LatestRafi Pk0% (1)
- NIOSH Hazardous DrugsDocument22 pagesNIOSH Hazardous DrugsjimstasonNo ratings yet
- Two Factor Theory Motivation-Hygiene Theory: Dual-Factor Theory/ Theory of Work Behavior byDocument16 pagesTwo Factor Theory Motivation-Hygiene Theory: Dual-Factor Theory/ Theory of Work Behavior byAngha0% (1)
- Kimberly Haynes, DMD - June 2016 Remedial Plan Issued by Texas State Board of Dental ExaminersDocument1 pageKimberly Haynes, DMD - June 2016 Remedial Plan Issued by Texas State Board of Dental ExaminersDentist The MenaceNo ratings yet
- H&PEDocument2 pagesH&PEDanielleNo ratings yet
- Mathematics in The Modern World: Introduction To LogicDocument17 pagesMathematics in The Modern World: Introduction To LogicOnecho Angelo Gabinete0% (1)
- Spa CuisineDocument11 pagesSpa CuisineNamanraj Singh JollyNo ratings yet
- Nur 111 Session 10 Sas 1Document9 pagesNur 111 Session 10 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- Soal Analytical ExpositionDocument17 pagesSoal Analytical ExpositionHilmi Muhammad AbduhNo ratings yet
- Chemical Restraint in The Horse: CommissionedDocument5 pagesChemical Restraint in The Horse: CommissionedKristoandi PoettingNo ratings yet
- 18 Min Workout PDFDocument12 pages18 Min Workout PDFdb0003No ratings yet
- Social Work ResearchDocument15 pagesSocial Work ResearchSuresh Murugan78% (9)
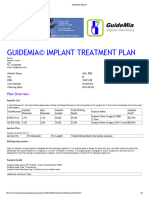
- GuideMia Sample Report - EnglishDocument9 pagesGuideMia Sample Report - Englishzhiao liuNo ratings yet
- OCP - 15 - GrindingDocument2 pagesOCP - 15 - GrindingNagendra Kumar SinghNo ratings yet
- The University of Melbourne Tuition Fees 2020: Tuition Fee Tables For International StudentsDocument32 pagesThe University of Melbourne Tuition Fees 2020: Tuition Fee Tables For International StudentsRuchi ChinfhaChinthaNo ratings yet