Professional Documents
Culture Documents
Pat Hop Harm Ology
Uploaded by
Noel BaluCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pat Hop Harm Ology
Uploaded by
Noel BaluCopyright:
Available Formats
Abu zaid nada
Group 352
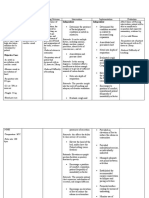
1. Edema. Definition. Mechanisms of edema formation. Morphology.
Edema occurs when an excessive volume of fluid accumulates in the tissues, either within
cells (cellular edema) or within the collagen-mucopolysaccharide matrix distributed in the
interstitial spaces (interstitial edema).
Our focus is on swelling of the extracellular matrix or interstitial edema, which may occur as
a result of aberrant changes in the pressures (hydrostatic and oncotic) acting across the
microvascular walls, alterations in the molecular structures that comprise the barrier to fluid
and solute flux in the endothelial wall that are manifest as changes in hydraulic conductivity
and the osmotic reflection coefficient for plasma proteins, or alterations in the lymphatic
outflow system, as predicted by examination of the Starling equation.
Excessive accumulation of interstitial fluid is generally viewed as detrimental to tissue
function because edema formation increases the diffusion distance for oxygen and other
nutrients, which may compromise cellular metabolism in the swollen tissue. For the same
reason, edema formation also limits the diffusional removal of potentially toxic byproducts of
cellular metabolism. These are especially important problems in the lungs, where pulmonary
edema can significantly impair gas exchange. In some tissues, certain anatomical structures
limit the expansion of the tissue spaces in response to edemagenic stress. For example, the
kidneys are enveloped by a tough fibrous capsule, the brain is surrounded by the cranial
vault, and skeletal muscles in the volar and anterior tibial compartments are encased in tight
fascial sheaths. As a consequence of the inability of these tissues to readily expand their
interstitial volume, relatively small increments in transcapillary fluid filtration induce large
increases in interstitial fluid pressure. This, in turn, reduces the vascular transmural pressure
gradient and physically compresses capillaries, thereby reducing nutritive tissue perfusion .
In the intestine, unrestrained transcapillary filtration leads to exudation of interstitial fluid into
the gut lumen, a phenomenon referred to as filtration-secretion or secretory filtration .
Filtration-secretion may compromise the absorptive function of the delicate intestinal mucosa
and appears to occur as a result of the formation of large channels between mucosal cells in
the villous tips when interstitial fluid pressure increases by greater than 5 mmHg . Ascites, or
the pathologic accumulation of fluid in the peritoneal cavity, occurs in cirrhosis and is caused
by fluid weeping from congested hepatic sinusoids secondary to elevated portal venous
pressure. Ascites can predispose afflicted individuals to peritoneal infections, hepatic
hydrothorax, and abdominal wall hernias.
You might also like
- Edema: Pendrik Tandean Internal Medicine, Medical Faculty of Hasanuddin University, MakassarDocument31 pagesEdema: Pendrik Tandean Internal Medicine, Medical Faculty of Hasanuddin University, MakassarLIEBERKHUNNo ratings yet
- Appendicitis PathophysiologyDocument4 pagesAppendicitis PathophysiologyAngelica Cassandra VillenaNo ratings yet
- Ecg ReadingDocument6 pagesEcg ReadingMarianette CainongNo ratings yet
- 2022 Serous Fluid Cytology AmaDocument75 pages2022 Serous Fluid Cytology Amareuben kwotaNo ratings yet
- A Level Biology NotesDocument6 pagesA Level Biology NotesMira AluedeNo ratings yet
- Hypovolemic Shock Nursing Care Management and Study GuideDocument1 pageHypovolemic Shock Nursing Care Management and Study GuideRoselyn VelascoNo ratings yet
- Pathophysiology ARDSDocument2 pagesPathophysiology ARDSKim AmboyaNo ratings yet
- Patofisiologi Ileus Obstruktif Ec Adhesi Dengan Fistula EnterokutanDocument1 pagePatofisiologi Ileus Obstruktif Ec Adhesi Dengan Fistula EnterokutanEfiran N S WandaNo ratings yet
- Starling ForcesDocument1 pageStarling ForcesbernieNo ratings yet
- Fluid Therapy Options and Rational SelectionDocument13 pagesFluid Therapy Options and Rational SelectionRoberto López MataNo ratings yet
- Chapter 036. Edema: PathogenesisDocument5 pagesChapter 036. Edema: PathogenesisJane GutierrezNo ratings yet
- Congestive Cardiac FalureDocument57 pagesCongestive Cardiac FalurelightningiceNo ratings yet
- Hydrostatic Pressure and Colloid Osmotic Pressure QuestionsDocument2 pagesHydrostatic Pressure and Colloid Osmotic Pressure QuestionsCorinneNo ratings yet
- Fenestración y Transporte Endotelial: EndotelioDocument5 pagesFenestración y Transporte Endotelial: EndotelioYANDIRA JANET SOSA IBAÑEZNo ratings yet
- Edema Hyperemia & Congestion: Miriam Al Battal, MDDocument20 pagesEdema Hyperemia & Congestion: Miriam Al Battal, MDHassoun hassounNo ratings yet
- Aubf FluidsDocument1 pageAubf FluidsMaryNo ratings yet
- OEDEMADocument4 pagesOEDEMAambiliNo ratings yet
- Pleural Effusion MechanismsDocument20 pagesPleural Effusion MechanismsAlienNo ratings yet
- CF NotesDocument24 pagesCF NotesKyle WindsorNo ratings yet
- Mechanism: Interstitium Swelling Interstitial Fluid HomeostasisDocument3 pagesMechanism: Interstitium Swelling Interstitial Fluid HomeostasisBryan MahendraNo ratings yet
- Renal Physiology IIDocument22 pagesRenal Physiology IIسمية صالحNo ratings yet
- PathophysiologyDocument13 pagesPathophysiologybobygannyNo ratings yet
- Celulas Müller EdemaDocument10 pagesCelulas Müller EdemaOrielle RocioNo ratings yet
- Kinesiología y Sus AlcancesDocument16 pagesKinesiología y Sus AlcancesEzequiel SosaNo ratings yet
- Diuretics: Dr. Ashley M. StokesDocument26 pagesDiuretics: Dr. Ashley M. StokesDhaif dhaifNo ratings yet
- Fluid MechanicsDocument6 pagesFluid MechanicszanitoreaddisonNo ratings yet
- MY GROUP Edema - Report2010Document5 pagesMY GROUP Edema - Report2010Nadhirah Mohamad NohNo ratings yet
- Pathophy Narrative (Final)Document9 pagesPathophy Narrative (Final)JANIELA RITCHEL DANIELNo ratings yet
- Lectura Adicional. Módulo 2. EfusionesDocument9 pagesLectura Adicional. Módulo 2. EfusionescarlosNo ratings yet
- Diskusi Topik EdemaDocument1 pageDiskusi Topik EdemaIustitia Septuaginta SambenNo ratings yet
- Atherosklerosis: DR Budi Enoch SPPDDocument56 pagesAtherosklerosis: DR Budi Enoch SPPDLia pramitaNo ratings yet
- Physiology, Body Fluids - StatPearls - NCBI BookshelfDocument5 pagesPhysiology, Body Fluids - StatPearls - NCBI Bookshelfpilar gabriela hernandez fernandezNo ratings yet
- Liver CirrhosisDocument12 pagesLiver CirrhosisOm Pratap KurmiNo ratings yet
- Nervous Disorder Circulation, Body Liquids and Acid BasesDocument33 pagesNervous Disorder Circulation, Body Liquids and Acid BasesHeru TriasNo ratings yet
- Shock Hypoxia and Perforated Duodenal UlcerDocument4 pagesShock Hypoxia and Perforated Duodenal UlceradaGodNo ratings yet
- Edema: Causes of Edema Are Described BelowDocument6 pagesEdema: Causes of Edema Are Described BelowrinirhynNo ratings yet
- MK Hemodynamics PathologyDocument27 pagesMK Hemodynamics PathologyMoses Jr Kazevu100% (1)
- Disorders of EsophagusDocument27 pagesDisorders of EsophagusFranci Kay SichuNo ratings yet
- GENITO URINARY SYSTEM 2nd Year BSC NursingDocument8 pagesGENITO URINARY SYSTEM 2nd Year BSC NursingShreyas WalvekarNo ratings yet
- Merlo Panoramic p20 6sc Drive Train Hydraulic Electrical Manual enDocument22 pagesMerlo Panoramic p20 6sc Drive Train Hydraulic Electrical Manual enkidixarov100% (37)
- Edema ParuDocument4 pagesEdema ParuSri BayaniNo ratings yet
- Disorders of Water-Salt MetabolismDocument3 pagesDisorders of Water-Salt MetabolismDr. NateqNo ratings yet
- Third SpacingDocument4 pagesThird SpacingJelly BeanNo ratings yet
- EdemaDocument4 pagesEdemaWanchung ZienNo ratings yet
- Disorders of The GallbladderDocument67 pagesDisorders of The GallbladderGeofry OdhiamboNo ratings yet
- Physiology of The LiverDocument43 pagesPhysiology of The LiverbeliskmncNo ratings yet
- Aqueous Humor Production 1Document7 pagesAqueous Humor Production 1yesi eka molitaNo ratings yet
- Melena, Diarrhea, NauseaDocument5 pagesMelena, Diarrhea, Nauseakelompok 6B IDIKNo ratings yet
- 24circulation Part 2Document11 pages24circulation Part 2Jaydave PatelNo ratings yet
- Excretion (Continued)Document9 pagesExcretion (Continued)t0000123No ratings yet
- Chapter 17Document6 pagesChapter 17g_komolafe100% (1)
- Disorders of The PulpDocument7 pagesDisorders of The Pulpابو الجودNo ratings yet
- Presentation1 (Ductal System)Document20 pagesPresentation1 (Ductal System)Sounak BanerjeeNo ratings yet
- Urogenital Development & Associated AnomaliesDocument114 pagesUrogenital Development & Associated AnomaliesvictorNo ratings yet
- PathologyDocument30 pagesPathologyTenorski baritonNo ratings yet
- Pathophysiology of Body Fluids: Mansyur Arif, MD, PHDDocument14 pagesPathophysiology of Body Fluids: Mansyur Arif, MD, PHDLIEBERKHUNNo ratings yet
- Lection 6. Acute PeritonitisDocument12 pagesLection 6. Acute PeritonitisOussama ANo ratings yet
- 1 EdemaDocument33 pages1 EdemaSawera RaheemNo ratings yet
- Drago Rogic - Seminarski !Document18 pagesDrago Rogic - Seminarski !Drago RogicNo ratings yet
- Williams 03 - Implantation, Embryogenesis, Placental DevelopmentDocument14 pagesWilliams 03 - Implantation, Embryogenesis, Placental DevelopmentAhmed Abou SeifNo ratings yet
- Hemodynamics ModifiedDocument175 pagesHemodynamics ModifiedAyele AsefaNo ratings yet
- Microcirculation of Blood 101: The Next Generation of HealthcareFrom EverandMicrocirculation of Blood 101: The Next Generation of HealthcareNo ratings yet
- 1 Klöppel Vortrag GEP NET The NE System 120217Document32 pages1 Klöppel Vortrag GEP NET The NE System 120217soledad88No ratings yet
- BIO101 Handouts by Hanzla Full 130 LessonsDocument225 pagesBIO101 Handouts by Hanzla Full 130 LessonsZeeshan NazarNo ratings yet
- 4.1 Photosynthesis QPDocument33 pages4.1 Photosynthesis QPNirashaNo ratings yet
- Pulmonary Pathology: Maria Sarah L. Lenon, MD, DPSPDocument32 pagesPulmonary Pathology: Maria Sarah L. Lenon, MD, DPSPKATREEYA ELEONOR LIMSINo ratings yet
- Institute of Dentistry, CMH Lahore Medical College Curriculum & Study Guide First Year BDS Deaniod@cmhlahore - Edu.pkDocument160 pagesInstitute of Dentistry, CMH Lahore Medical College Curriculum & Study Guide First Year BDS Deaniod@cmhlahore - Edu.pkSR Creations.No ratings yet
- OMM Block 1 Lab Study GuideDocument18 pagesOMM Block 1 Lab Study Guidejoe doweNo ratings yet
- Systemic Acquired Resistance (SAR)Document38 pagesSystemic Acquired Resistance (SAR)Arulsia ANo ratings yet
- Endocrinology PhysiologyDocument2 pagesEndocrinology PhysiologyzeeshanNo ratings yet
- 1st SST Science Mock TestDocument15 pages1st SST Science Mock TestJunaid SaqibNo ratings yet
- Lesson 4: Anatomy and Physiology of Reproduction: Gee 2 - Gender & Society Dr. Teri Marie P. Laude Et. AlDocument1 pageLesson 4: Anatomy and Physiology of Reproduction: Gee 2 - Gender & Society Dr. Teri Marie P. Laude Et. AlRexson Dela Cruz TagubaNo ratings yet
- Normal Test ReportDocument2 pagesNormal Test ReportBilal RashidNo ratings yet
- snpwp97,+2376 2581 1 PBDocument4 pagessnpwp97,+2376 2581 1 PBChristalie Bea FernandezNo ratings yet
- Xi. Biology. Revision Work.-Ch.3,4,&5. 3. Plant Kingdom. 1.what Do You Mean by ? 3.why Is Algae Grouped Under Thllophyta? 4. Write TheDocument2 pagesXi. Biology. Revision Work.-Ch.3,4,&5. 3. Plant Kingdom. 1.what Do You Mean by ? 3.why Is Algae Grouped Under Thllophyta? 4. Write TheOwasisNo ratings yet
- ABG (Arterial Blood Gas) : DR Sudhir Kumar SinghDocument30 pagesABG (Arterial Blood Gas) : DR Sudhir Kumar SinghVaso BalakhashviliNo ratings yet
- Revise Nursing Care PlanDocument5 pagesRevise Nursing Care PlanNur SetsuNo ratings yet
- Chapter Nine - Isolation, Culture and Propagation of Natural Killer CellsDocument11 pagesChapter Nine - Isolation, Culture and Propagation of Natural Killer CellsManoj Kumar pandreNo ratings yet
- Module 2: Biology and PsychologyDocument23 pagesModule 2: Biology and Psychologyshain aldovinoNo ratings yet
- Pashu Prahari April To June MagzineDocument129 pagesPashu Prahari April To June MagzinesumNo ratings yet
- ORDONEZ ERALAINE G. Photosynthesis Reading and Questions PDFDocument3 pagesORDONEZ ERALAINE G. Photosynthesis Reading and Questions PDFRaine OrdonezNo ratings yet
- Modelo Respondido Quiz InglesDocument4 pagesModelo Respondido Quiz InglesCaro RiosNo ratings yet
- Gastritis An Update in 2020Document17 pagesGastritis An Update in 2020adri20121989No ratings yet
- Sensory OrgansDocument11 pagesSensory OrgansVictoria VintuNo ratings yet
- Study Guide For Bio 101 Final ExamDocument2 pagesStudy Guide For Bio 101 Final ExamJinnyCakes100% (1)
- Rapidchem National Dealers Plist April 2023Document2 pagesRapidchem National Dealers Plist April 2023lifesaviourdyenNo ratings yet
- Mcqs On Excretory SystemDocument3 pagesMcqs On Excretory SystemIshfaq LoneNo ratings yet
- Mtle - Hema 1Document50 pagesMtle - Hema 1Leogene Earl FranciaNo ratings yet
- Accessory Respiratory Organ-FishDocument63 pagesAccessory Respiratory Organ-Fishkaushik mallickNo ratings yet
- Castor Oil Packs ImmunomodulationDocument6 pagesCastor Oil Packs ImmunomodulationCiprian AlexandruNo ratings yet