Professional Documents
Culture Documents
Guide During AEFI Investigation
Uploaded by
Fret Ramirez Coronia RNOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Guide During AEFI Investigation
Uploaded by
Fret Ramirez Coronia RNCopyright:
Available Formats
Guide during AEFI Investigation
We recommend the following actions for a comprehensive clinical investigation to aid in determining the valid
diagnosis to launch the step 1 of the causality assessment by the RAEFIC:
1. Post-mortem RT-PCR swab - If this is not possible, please cite or explain the reasons in the case
investigation form and during the causality assessment (i.e. not a protocol in the clinic nor hospital)
2. Medical autopsy - If this is not possible, please cite or explain the reasons in the case investigation form
and during the causality assessment (i.e. no consent, no available pathologist in the nearest hospital,
NBI, or PNP availability)
3. Verbal autopsy from the patient's relatives particularly on:
A. Physical look of the patient - was he emaciated / nangangayayat, obese
B. Level of control of hypertension, if any - Was the patient compliant on taking medications.
Indicate how long has he started medications, usual BP and highest BP
C. Level of control of diabetes mellitus, if any - Was he insulin-requiring, what are the medications,
latest FBS or HbA1C
D. Level of control of chronic kidney disease, if any.
E. Previous hospitalizations, medical records, laboratory, imaging or pathologic findings,
particularly 12-L ECG, Chest X-ray, 2D-Echo, CBC w/ quantitative platelet count with or without
peripheral blood smear, electrolytes (Na, K, Cl BUN, Crea), metabolic panel (TG HDL, LDL,
vLDL), FBS, HbA1c
F. Family medical history - hypertension, diabetes, early cardiac death (<50 y/o) in 1st generation
members of the family -- parents, siblings, children of the patient, allergies, asthma or allergic
rhinitis, previous COVID-19 exposure or diagnosis
G. Personal social history
Was the patient a smoker? how many pack-years or how many sticks of cigarettes does
he use in a day, and around how many years has s/he been smoking?
Alcohol drinking and frequency and usual beverage and quantity (ex. beer drinker,
consumes ~2L every other night
Occupation/line of work - ex. farmer, kaingin, miner
Recent COVID Exposure in the past 14 days prior to death
H. Baseline functional status - was the patient ambulatory without assistance? what is his body
habitus? does he look generally emaciated?
I. Did the patient experience the following symptoms that may pertain to organic causes of death:
Neuro: Focal neurologic no matter how mild (seizures, slurring of speech, facial
asymmetry, dragging of feet, numbness, of extremities, hands/feet)
Cardio: cardiac (chest pain- -- characterize the pain, even in the vernacular --- point
tenderness, heaviness, tightness, radiation to the back or left upper shoulder; heart
failure symptoms -- hinihingal pagkatapos maglakad o magbuhat o pagkatapos nang
malalapit na tinatakbuhan, nalulunod kung matulog na walang unan)
Pulmonary: if any (DOB, Cough, Colds, shortness of breath or respiratory symptoms)
GU: Genitourinary (weak stream, urinary incontinence or hindi ma-kontrol ang pag-
ihi, difficulty in urination, nocturia bumabangon sa tulog para umihi))
GI: Gastrointestinal (nausea, vomiting, abdominal pain, diarrhea, constipation, loss of
appetite / walang ganang kumain, early satiety / madaling mabusog)
Extremities (pallor, edema, jaundice naninilaw)
HEENT (Head, Ears, Eyes, Nose & Throat): if any significant findings: Sudden-onset
blindness, tinnitus, anosmia nawalan ng pang-amoy, ageusia nawalan ng panlasa,
hirap lumunok
J. Provide a day-by-day to hour-by-hour narrative of events prior to death
4. Retrieval of other medical records, laboratory tests. Please take note that if the retrieval of these
records is difficult from the patient or previous attending physicians, the investigation team may opt to ask
for a written summary asking the contents of these records and tests, provided as a detailed medical
abstract to the investigation team. If these are not possible, please document the efforts done for
transparency purposes
5. This is a general advice and may be supplemented by the respective RESU and/or RAEFIC
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Assessment of Adult ADHDDocument24 pagesAssessment of Adult ADHDPsydoc100% (4)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Gender & Mental HealthDocument25 pagesGender & Mental HealthMarcNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Clinical Practice Guideline For Schizophrenia and Incipient Psychotic DisorderDocument9 pagesClinical Practice Guideline For Schizophrenia and Incipient Psychotic DisorderFranco MascayanoNo ratings yet
- Brain Cancer (Tumors) : Jinu Janet Varghese Group: 4 Year: 5 Tbilisi State Medical UniversityDocument35 pagesBrain Cancer (Tumors) : Jinu Janet Varghese Group: 4 Year: 5 Tbilisi State Medical UniversityPPDSNeuroUnsri RSMHNo ratings yet
- Introduction To Nursing EthicsDocument23 pagesIntroduction To Nursing EthicsAzra Baloch67% (3)
- ERP Bridging Document Rev 00Document21 pagesERP Bridging Document Rev 00herisusantoNo ratings yet
- To Err Is Human A Case Study of Error Prevention in Process IsolationsDocument6 pagesTo Err Is Human A Case Study of Error Prevention in Process Isolationsairbuk doeingNo ratings yet
- Dialysis Flow SheetDocument1 pageDialysis Flow SheetFret Ramirez Coronia RNNo ratings yet
- Dokument - Pub DRRM H Planning Guide Content Module 3 Flipbook PDFDocument9 pagesDokument - Pub DRRM H Planning Guide Content Module 3 Flipbook PDFFret Ramirez Coronia RNNo ratings yet
- PhilHealth Konsulta Provider Self-Assessment ToolDocument8 pagesPhilHealth Konsulta Provider Self-Assessment ToolFret Ramirez Coronia RNNo ratings yet
- Rabies Policies and ProceduresDocument19 pagesRabies Policies and ProceduresFret Ramirez Coronia RNNo ratings yet
- Sosialisasi E-Report IKP RS Eksternal - 2021Document32 pagesSosialisasi E-Report IKP RS Eksternal - 2021Putri Arum PermatasariNo ratings yet
- Comm 1010 Informative Full-Sentence Speech Outline InstructionsDocument2 pagesComm 1010 Informative Full-Sentence Speech Outline Instructionsapi-270505782No ratings yet
- Network and IT Assessment Form 1Document1 pageNetwork and IT Assessment Form 1Fret Ramirez Coronia RNNo ratings yet
- DRRMH Monitoring and Assessment ChecklistDocument3 pagesDRRMH Monitoring and Assessment ChecklistFret Ramirez Coronia RNNo ratings yet
- Chikiting Ligtas Certificate TemplateDocument2 pagesChikiting Ligtas Certificate TemplateRhu Pugo, La UnionNo ratings yet
- Network and IT Assessment Form 3Document1 pageNetwork and IT Assessment Form 3Fret Ramirez Coronia RNNo ratings yet
- Network and IT Assessment Form 2Document1 pageNetwork and IT Assessment Form 2Fret Ramirez Coronia RNNo ratings yet
- Training Rules and Regulations: Rizal ChapterDocument1 pageTraining Rules and Regulations: Rizal ChapterFret Ramirez Coronia RNNo ratings yet
- Social Change1Document9 pagesSocial Change1Fret Ramirez Coronia RNNo ratings yet
- Republic The Philippines Health: ClarifyDocument12 pagesRepublic The Philippines Health: ClarifyFret Ramirez Coronia RNNo ratings yet
- National Vaccination Operation Center: COVID-19 VACCINE HAYAT-VAX (Sinopharm)Document9 pagesNational Vaccination Operation Center: COVID-19 VACCINE HAYAT-VAX (Sinopharm)Fret Ramirez Coronia RNNo ratings yet
- DOH 2020-0258-A Amended GuidelinesDocument7 pagesDOH 2020-0258-A Amended GuidelinesCathy LopezNo ratings yet
- Advisory No. 15Document9 pagesAdvisory No. 15Fret Ramirez Coronia RNNo ratings yet
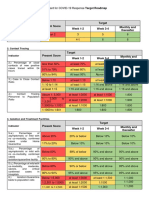
- Present Score Target Week 1-2 Week 3-4 Monthly and ThereafterDocument2 pagesPresent Score Target Week 1-2 Week 3-4 Monthly and ThereafterFret Ramirez Coronia RNNo ratings yet
- Product Information of Sinopharm Covid-19 Vaccine (Vero Cell), Inactivated CoviloDocument7 pagesProduct Information of Sinopharm Covid-19 Vaccine (Vero Cell), Inactivated CoviloFret Ramirez Coronia RNNo ratings yet
- AO2021-0043 Omnibus Guidelines On The Minimum Public Health Standards For The Safe Reopening of Institutions (08-31)Document44 pagesAO2021-0043 Omnibus Guidelines On The Minimum Public Health Standards For The Safe Reopening of Institutions (08-31)Fret Ramirez Coronia RN100% (1)
- Burns Management PDFDocument7 pagesBurns Management PDFRoh Bungaria N Garingging100% (1)
- Skill Mapping20210531 - 19132706Document4 pagesSkill Mapping20210531 - 19132706Fret Ramirez Coronia RNNo ratings yet
- Index Case Name Age Sex Contact Generation Date of Birth (Mm/dd/yr)Document5 pagesIndex Case Name Age Sex Contact Generation Date of Birth (Mm/dd/yr)Fret Ramirez Coronia RNNo ratings yet
- NVOC Advisory 41 Reiteration On The Scheduling For Vaccination of Individuals With COVID-19 InfectionDocument1 pageNVOC Advisory 41 Reiteration On The Scheduling For Vaccination of Individuals With COVID-19 InfectionFret Ramirez Coronia RNNo ratings yet
- QAQI - Policy On QAPDocument5 pagesQAQI - Policy On QAPFret Ramirez Coronia RNNo ratings yet
- Vital Signs Flow SheetDocument1 pageVital Signs Flow SheetFret Ramirez Coronia RNNo ratings yet
- ANTIGEN TEST KIT UTILIZATION REPORT - Preliminary FormDocument1 pageANTIGEN TEST KIT UTILIZATION REPORT - Preliminary FormFret Ramirez Coronia RNNo ratings yet
- Medication LogDocument1 pageMedication LogFret Ramirez Coronia RNNo ratings yet
- Regulatory Board's Guide to Registering Housing ProjectsDocument16 pagesRegulatory Board's Guide to Registering Housing ProjectsLgu SikatunaNo ratings yet
- LGU Specimen Submission GuidelinesDocument3 pagesLGU Specimen Submission GuidelinesFret Ramirez Coronia RNNo ratings yet
- Cstms Registry CalabarzonDocument11 pagesCstms Registry CalabarzonFret Ramirez Coronia RNNo ratings yet
- There and Back AgainDocument113 pagesThere and Back AgainsantjiejdNo ratings yet
- Cancer: Causes, Diagnosis & TreatmentDocument2 pagesCancer: Causes, Diagnosis & TreatmentNitesh kuraheNo ratings yet
- Case Study on ADHD Nursing Diagnoses and InterventionsDocument2 pagesCase Study on ADHD Nursing Diagnoses and InterventionsKeeshia Mae100% (1)
- Flyer IDDW 2022 Updt 28.07.22Document2 pagesFlyer IDDW 2022 Updt 28.07.22Krisna ChandraNo ratings yet
- Syllabus Foodservice-2Document15 pagesSyllabus Foodservice-2Arienda RKNo ratings yet
- Capaian Mutu Respon Time Igd-2Document1,536 pagesCapaian Mutu Respon Time Igd-2Arsyad AkmatulNo ratings yet
- Zinc Deficiency in ChickensDocument6 pagesZinc Deficiency in ChickensShah NawazNo ratings yet
- OSH With GAD 2Document5 pagesOSH With GAD 2JanrayBernalNo ratings yet
- LASIXDocument2 pagesLASIXMill Jan CruzNo ratings yet
- Sika Monotop®-614 HS: Safety Data SheetDocument10 pagesSika Monotop®-614 HS: Safety Data SheetMuhammad Farhan SetyawanNo ratings yet
- Mukt Shabd JournalDocument9 pagesMukt Shabd JournalJustin SebastianNo ratings yet
- Student Exploration: Disease Spread: Vocabulary: Disease, Epidemic, Infect, Infectious Disease, PathogenDocument5 pagesStudent Exploration: Disease Spread: Vocabulary: Disease, Epidemic, Infect, Infectious Disease, PathogenVijay Shankar PrasadNo ratings yet
- Practice Test: Ielts UsaDocument11 pagesPractice Test: Ielts UsajoseNo ratings yet
- Dializer Hollow FiberDocument6 pagesDializer Hollow FiberdinamariaNo ratings yet
- 1 The Philippines Sam Guidelines 2015 Final Print Ready PDFDocument111 pages1 The Philippines Sam Guidelines 2015 Final Print Ready PDFFar SultanNo ratings yet
- Everyday Health Is ImportantDocument2 pagesEveryday Health Is ImportantEllen WrightNo ratings yet
- Minister of Health V TreatmentDocument82 pagesMinister of Health V TreatmentABDOULIENo ratings yet
- MD Community MedicineDocument14 pagesMD Community MedicineAshwini DongreNo ratings yet
- Hridayrog Sarvangi AbhigamDocument286 pagesHridayrog Sarvangi AbhigamMaheshNo ratings yet
- Public Health Internship: Environmental Health and Safety Intern at Berry Global Summer ScottDocument17 pagesPublic Health Internship: Environmental Health and Safety Intern at Berry Global Summer Scottapi-677941383No ratings yet
- Hope 3 Q1 M6Document12 pagesHope 3 Q1 M6Angelo Jess TorrevillaNo ratings yet