Professional Documents
Culture Documents
Robust Neutralizing Antibodies To Sars-Cov-2 Infection Persist For Months
Uploaded by
Jared Michael BergerOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Robust Neutralizing Antibodies To Sars-Cov-2 Infection Persist For Months
Uploaded by
Jared Michael BergerCopyright:
Available Formats
RES EARCH
CORONAVIRUS of 30,082 individuals testing positive (defined
as detectable antibodies to the spike protein
Robust neutralizing antibodies to SARS-CoV-2 at a titer of 1:80 or higher) and 42,319 testing
negative. The clinical laboratory ELISA set up
infection persist for months results in discrete titers of either 1:80, 1:160,
1:320, 1:960, or ≥1:2880. Titers of 1:80 and
Ania Wajnberg1*, Fatima Amanat2,3, Adolfo Firpo4, Deena R. Altman5, Mark J. Bailey1, 1:160 were categorized as low titers, 1:320 as
Mayce Mansour1, Meagan McMahon2, Philip Meade2,3, Damodara Rao Mendu4, Kimberly Muellers1, moderate, and 1:960 and ≥1:2880 as high
Daniel Stadlbauer2, Kimberly Stone1, Shirin Strohmeier2, Viviana Simon2, Judith Aberg5, titers. For plasma therapy, titers of 1:320 or
David L. Reich6, Florian Krammer2*, Carlos Cordon-Cardo4* higher were initially deemed eligible. Of the
30,082 positive samples, 690 (2.29%) had a
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused a global pandemic with titer of 1:80; 1453 (4.83%), 1:160; 6765 (22.49%),
millions infected and more than 1 million fatalities. Questions regarding the robustness, functionality, and 1:320; 9564 (31.79%), 1:960; and 11,610 (38.60%),
longevity of the antibody response to the virus remain unanswered. Here, on the basis of a dataset of ≥1:2880 (Fig. 1). Thus, we conclude that the vast
30,082 individuals screened at Mount Sinai Health System in New York City, we report that the vast majority of positive individuals have moderate-
majority of infected individuals with mild-to-moderate COVID-19 experience robust immunoglobulin G to-high titers of anti-spike antibodies. Of course,
antibody responses against the viral spike protein. We also show that titers are relatively stable for at least the argument could be made that we could be
a period of about 5 months and that anti-spike binding titers significantly correlate with neutralization missing a number of individuals who had been
of authentic SARS-CoV-2. Our data suggest that more than 90% of seroconverters make detectable infected with SARS-CoV-2 and did not produce
neutralizing antibody responses. These titers remain relatively stable for several months after infection. antibodies, given that many individuals in-
Downloaded from http://science.sciencemag.org/ on December 4, 2020
cluded in our dataset had never been tested
S
by a nucleic acid amplification test for the
evere acute respiratory syndrome coro- for characterizing the immune response to virus. An earlier analysis performed with a
navirus 2 (SARS-CoV-2) has infected SARS-CoV-2 is the spike protein. The spike is a smaller subset of 568 PCR-confirmed indi-
millions of individuals globally and, as large trimeric glycoprotein that contains the viduals using the same ELISA showed that
of October 2020, has led to the death of receptor binding domain, which the virus uses >99% developed an anti-spike antibody re-
>1 million individuals. Although the anti- to dock to its cellular receptor, angiotensin- sponse (8). In a later dataset of 2347 patients
body responses in severe COVID-19 cases have converting enzyme 2, and for fusion of viral who self-reported positive PCR, 95% had
been relatively well characterized (1, 2), assess- and cellular membranes (4, 5). It is known positive antibody titers, which indicates that
ing the response in mild and asymptomatic from other coronaviruses—and it holds true we did not miss large numbers of patients
cases is of great importance because they con- for SARS-CoV-2—that the spike is the main, and confirms our prior sensitivity findings.
stitute most infections. It will be critical to and potentially the only, target for neutral- Thus, the rate of individuals who do not
understand the robustness of the antibody izing antibodies (6). Therefore, the assay seroconvert after SARS-CoV-2 infection is
response in these mild cases, including its used in this study to characterize the anti- low, although such individuals may exist,
longevity and functionality, so as to inform body response to SARS-CoV-2 is based on and the majority of responders mount titers
serosurveys and to determine levels and du- the trimerized, stabilized ectodomain of the of 1:320 or higher.
ration of antibody titers that may be protec- spike protein (7). An enzyme-linked immuno- Determining the neutralizing effects of SARS-
tive against reinfection (3). sorbent assay (ELISA) initially developed CoV-2 spike antibodies is critical to understand-
Antibodies to SARS-CoV-2 can target many in early 2020 has been extensively used in ing possible protective effects of the immune
of its encoded proteins, including structural research (7–10). This so-called Mount Sinai response. Therefore, we performed a well-
and nonstructural antigens. Thus far, two struc- ELISA has high sensitivity (92.5%) and speci- established quantitative microneutralization
tural proteins have been used as target antigens ficity (100%), as determined with an initial assay (12) based on authentic SARS-CoV-2
for serological assays. One is the abundant validation panel of samples (table S1). Fur- with 120 samples of known ELISA titers rang-
nucleoprotein (NP), which is found inside the thermore, it has a positive predictive value ing from negative to ≥1:2880. Neutralization
virus or inside infected cells. However, because (PPV) of 100%, with a negative predictive val- titers significantly correlated (Spearman r =
of the biological function of NP and because it ue (NPV) of 99.6%. 0.87, P < 0.0001) with spike-binding titers
is shielded from antibodies by viral or cellular In March 2020, the Mount Sinai Health Sys- (Fig. 2A). Although there was some variability,
membranes, it is unlikely that NP antibodies tem began screening individuals for antibodies sera with 1:320, 1:960, and ≥1:2880 ELISA
can directly neutralize SARS-CoV-2. The sec- to SARS-CoV-2 to recruit volunteers as donors titers had geometric mean 50% inhibitory
ond structural protein often used as a target for convalescent plasma therapy (11). Screened dilutions (ID50) of about 1:30, 1:75, and 1:550,
patients had either polymerase chain reaction respectively. If any and all neutralizing ac-
1
(PCR)–confirmed SARS-CoV-2 infections or tivity above background is considered, then
Department of General Internal Medicine, Icahn School of
Medicine at Mount Sinai, New York, NY 10029, USA.
suspected disease, which is defined as being ~50% of sera in the 1:80 to 1:160 titer range,
2
Department of Microbiology, Icahn School of Medicine at told by a physician that symptoms may be 90% in the 1:320 range, and all sera in the
Mount Sinai, New York, NY 10029, USA. 3Graduate School of related to SARS-CoV-2 or exposure to some- 1:960 to ≥1:2880 range had neutralizing ac-
Biomedical Sciences, Icahn School of Medicine at Mount
Sinai, New York, NY 10029, USA. 4Clinical Microbiology
one with confirmed SARS-CoV-2 infection. tivity (Fig. 2B). Only one of the negative samples
Laboratory, Department of Pathology, Icahn School of Most of the symptomatic patients who were showed activity slightly above background,
Medicine at Mount Sinai, New York, NY 10029, USA.
5
screened experienced mild-to-moderate dis- which was potentially an ELISA false negative.
Division of Infectious Diseases, Department of Medicine,
ease, with <5% requiring emergency depart- Another important question is longevity of
Icahn School of Medicine at Mount Sinai, New York, NY
10029, USA. 6Department of Anesthesiology, Perioperative ment evaluation or hospitalization. Mount the antibody response to the spike. To assess
and Pain Medicine, Icahn School of Medicine at Mount Sinai, Sinai also offered the antibody test to all the medium-range stability of serum antibody
New York, NY 10029, USA. employees in its health system on a volun- titers against the spike protein, we recalled 121
*Corresponding author. Email: ania.wajnberg@mountsinai.org
(A.W.); florian.krammer@mssm.edu (F.K.); carlos. tary basis. By 6 October 2020, Mount Sinai plasma donors at a variety of titer levels who
cordon-cardo@mssm.edu (C.C.-C.) had screened 72,401 individuals, with a total had initially been screened at around day 30
Wajnberg et al., Science 370, 1227–1230 (2020) 4 December 2020 1 of 4
RES EARCH | R E P O R T
Fig. 1. SARS-CoV-2 spike antibody titers in 30,082 individuals. (A) The percentage of individuals with antibody titers of 1:80 (low), 1:160 (low), 1:320 (moderate),
1:960 (high), and ≥1:2880 (high). (B) Absolute numbers of individuals testing positive and percent of individuals with titers of 1:320 over time. Testing of each
sample was performed once in a Clinical Laboratory Improvement Amendments (CLIA)–certified laboratory using an assay that received emergency use authorization
(EUA) from the U.S. Food and Drug Administration (FDA).
Downloaded from http://science.sciencemag.org/ on December 4, 2020
Fig. 2. Neutralizing activity of serum
samples in relation to ELISA titers. (A) A
correlation analysis between ELISA titers on
the x axis and neutralization titers in a micro-
neutralization assay on the y axis. The
Spearman r was determined. Red bars indicate
the geometric mean. (B) The proportion of
sera that exert any neutralizing activity in each
of the ELISA titer categories. Testing was
performed once, using an FDA EUA ELISA in a
CLIA laboratory, or twice, following a stand-
ardized neutralization protocol.
after symptom onset for two additional time cating that very low initial titers might drop to Correlates of protection have been estab-
points. The mean interval between the initial undetectable levels over time. Neutralizing lished for many different viral infections. These
titer measurement and the second was 52 days antibody titers followed titers measured by correlates are usually based on a specific level
(range: 33 to 67 days). This set the second time ELISA (Fig. 3G), and a good correlation be- of antibody acquired through vaccination or
point at a mean of 82 days after symptom tween neutralization and ELISA titers was natural infection that substantially reduces
onset (range: 52 to 104 days) and the third still observed on day 148 (Fig. 3H). The initial the risk of (re)infection. One example is the
time point at 148 days after symptom onset serum antibody titer was likely produced by hemagglutination inhibition titer for the in-
(range: 113 to 186 days). In comparing overall plasmablasts, and plasmablast-derived anti- fluenza virus, where a 1:40 titer reduces the
titers, we observed a slight drop from a geo- bodies peak 2 to 3 weeks after symptom onset. risk of getting infected by 50% (14). Similar
metric mean titer (GMT) of 764 to a GMT of Given an immunoglobulin G half-life of ~21 days, titers have been established for the measles
690 from the first to the second time point the sustained antibody titers observed here virus (an ID50 titer of 1:120), hepatitis A virus,
and another drop to a GMT of 404 for the over time are likely produced by long-lived hepatitis B virus, and many others (15). These
last time point (Fig. 3A). In the higher titer plasma cells in the bone marrow. Note that titers have facilitated vaccine development con-
range of ≥1:2880 and 1:960, we also observed our observations contrast with a recent report siderably. For some viruses and vaccines, the
a slow decline in titer over time (Fig. 3, B and that found waning titers at 8 weeks after virus kinetics of the antibody response is also known,
C). Unexpectedly, but in agreement with infection (13). Especially in asymptomatic cases, allowing for an accurate prediction of how
earlier observations that seroconversion in antibody responses disappeared after 8 weeks long protection will last (16).
mild COVID-19 cases might take a longer time in 40% of individuals in that study. However, It is still unclear whether infection with
to mount (8), we saw an increase in individuals the antibodies measured in that paper targeted SARS-CoV-2 in humans protects from rein-
who had an initial titer of 1:320, 1:160, or 1:80 the NP plus a single linear spike epitope. The fection and, if it does, for how long. We know
(Fig. 3, D to F) from day 30 to day 82. Titers in same paper also reported relatively stable from work with common human coronaviruses
these groups declined to about day 30 levels on (slightly declining) neutralizing antibody that neutralizing antibodies are induced and
day 148. Notably, one individual in the initial titers, which shows much higher concordance that these antibodies can last for years and
1:80 group dropped from a 1:80 titer to being with our present findings. Thus, the stability provide protection from reinfection or, in
negative at the day 82 time point, and two others of the antibody response over time may also the event of reinfection, attenuate disease (17).
lost reactivity at the day 148 time point, indi- depend on the target antigen. Furthermore, we now know from nonhuman
Wajnberg et al., Science 370, 1227–1230 (2020) 4 December 2020 2 of 4
RES EARCH | R E P O R T
Downloaded from http://science.sciencemag.org/ on December 4, 2020
Fig. 3. Antibody titer stability over time. (A) Titers of 121 volunteers whose analysis of variance corrected for multiple comparison was used to determine
blood was initially drawn ~30 days after COVID-19 symptom onset and who were statistical significance. (H) A correlation analysis between ELISA titers on the
then recalled for additional blood draws at ~82 days and 148 days after symptom x axis and neutralization titers in a microneutralization assay on the y axis
onset. (B to F) The same data as in (A), but stratified by the initial (day 30) titer. at day 148. Red bars indicate the geometric mean. The Spearman r was
Titers are graphed as geometric mean titers (GMT) with geometric standard determined. Testing was performed once, using an FDA EUA ELISA in a CLIA-
error. (G) Neutralization titers of 36 individuals over time. A paired one-way certified laboratory, or twice, following a standardized neutralization protocol.
primate models that infection with SARS- antibody titers of 1:320 or higher show neu- tion, combined with a better understanding of
CoV-2 does protect from reinfection for at tralizing activity in their serum. We also find antibody kinetics to the spike protein, would
least some time (18, 19). We also know that stable antibody titers over a period of at least inform policy regarding the COVID-19 pan-
transferring serum of convalescent animals 3 months and only modest declines at the demic and would be beneficial to vaccine de-
or neutralizing monoclonal antibodies to naïve 5-month time point, which is consistent with velopment efforts.
animals can be protective and reduces virus data for the human coronaviruses SARS-CoV-1
REFERENCES AND NOTES
replication significantly (20, 21). Finally, vaccine- and Middle East respiratory syndrome–related
1. L. Liu et al., Emerg. Microbes Infect. 9, 1664–1670 (2020).
induced neutralizing antibody titers have been coronavirus (MERS-CoV) (17). We plan to follow 2. Q. X. Long et al., Nat. Med. 26, 845–848 (2020).
established as a correlate of protection in non- this cohort over longer intervals of time. Al- 3. F. Krammer, V. Simon, Science 368, 1060–1061 (2020).
4. D. Wrapp et al., Science 367, 1260–1263 (2020).
human primates (22). Notably, these vaccine- though we cannot provide conclusive evidence 5. M. Letko, A. Marzi, V. Munster, Nat. Microbiol. 5, 562–569 (2020).
induced titers were relatively low and in the that these antibody responses protect from re- 6. F. Amanat, F. Krammer, Immunity 52, 583–589 (2020).
lower range of the titers observed in this study. infection, we believe it is very likely that they 7. F. Amanat et al., Nat. Med. 26, 1033–1036 (2020).
8. A. Wajnberg et al., Lancet 1, e283–e289 (2020).
Our data reveal that individuals who have re- will decrease the odds ratio of reinfection and 9. D. Stadlbauer et al., medRxiv 2020.06.2028.20142190
covered from mild COVID-19 experience rela- may attenuate disease in the case of break- [Preprint]. 29 June 2020. https://doi.org/10.1101/
tively robust antibody responses to the spike through infection. We believe that it is impera- 2020.06.28.20142190.
10. D. Stadlbauer et al., Curr. Protoc. Microbiol. 57, e100 (2020).
protein, which correlate significantly with neu- tive to swiftly perform studies to investigate 11. S. T. H. Liu et al., Nat. Med. 10.1038/s41591-020-1088-9 (2020).
tralization of authentic SARS-CoV-2 virus. Fur- and establish a correlate of protection from 12. F. Amanat et al., Curr. Protoc. Microbiol. 58, e108 (2020).
thermore, the vast majority of individuals with SARS-CoV-2 infection. A correlate of protec- 13. Q. X. Long et al., Nat. Med. 26, 1200–1204 (2020).
Wajnberg et al., Science 370, 1227–1230 (2020) 4 December 2020 3 of 4
RES EARCH | R E P O R T
14. F. Krammer, J. P. Weir, O. Engelhardt, J. M. Katz, R. J. Cox, institutional support of our work. Funding: This work was partially (COVID and HIV), Merck (HIV), Pfizer (COVID), Regeneron (COVID),
Influenza Other Respir. Viruses 14, 237–243 (2020). supported by NIAID Centers of Excellence for Influenza Research and and Viiv (HIV). J.A. has received personal fees for serving on the HIV
15. S. A. Plotkin, Clin. Vaccine Immunol. 17, 1055–1065 (2010). Surveillance (CEIRS) contract HHSN272201400008C (F.K.) and by scientific advisory boards of Gilead, Janssen, Merck, Theratechnology,
16. K. Van Herck, P. Van Damme, J. Med. Virol. 63, 1–7 (2001). Collaborative Influenza Vaccine Innovation Centers (CIVIC) contract and Viiv. Data and materials availability: All data are available in
17. A. T. Huang et al., Nat. Commun. 11, 4704 (2020). 75N93019C00051 (F.K.). Support was also provided by the JPB the manuscript or the supplementary materials. This work is licensed
18. W. Deng et al., Science 369, 818–823 (2020). Foundation, the Open Philanthropy Project (#2020-215611), and other under a Creative Commons Attribution 4.0 International (CC BY 4.0)
19. A. Chandrashekar et al., Science 369, 812–817 (2020). philanthropic donations. This effort was deliberated with Leidos license, which permits unrestricted use, distribution, and reproduction
20. R. Shi et al., Nature 584, 120–124 (2020). Biomedical Research Inc./NCI over the last several months and is now in any medium, provided the original work is properly cited. To view
21. M. Imai et al., Proc. Natl. Acad. Sci. U.S.A. 117, 16587–16595 going to be supported by the Serological Sciences Network (SeroNet). a copy of this license, visit https://creativecommons.org/licenses/by/
(2020). This project will be funded in whole or in part with federal funds 4.0/. This license does not apply to figures/photos/artwork or other
from the National Cancer Institute, National Institutes of Health, under content included in the article that is credited to a third party; obtain
22. J. Yu et al., Science 369, 806–811 (2020).
contract 75N91019D00024, task order 75N91020F00003, as well authorization from the rights holder before using such material.
as U54 CA260560. The content of this publication does not necessarily
ACKN OW LEDG MEN TS reflect the views or policies of the Department of Health and Human SUPPLEMENTARY MATERIALS
We are grateful for the continuous expert guidance provided by the Services, nor does mention of trade names, commercial products,
science.sciencemag.org/content/370/6521/1227/suppl/DC1
ISMMS Program for the Protection of Human Subjects (PPHS). We also or organizations imply endorsement by the U.S. government. Author
Materials and Methods
thank R. A. Albrecht for oversight of the conventional Biosafety Level 3 contributions: A.W., D.R.A., M.J.B., M.Ma., K.M., K.S., and J.A.
Table S1
biocontainment facility, the medical students involved in the plasma performed clinical activities. A.W., J.A., D.L.R., F.K., and C.C.-C.
References
convalescence program, and D. Adhimoolam for invaluable help with designed the study. A.W. and F.K. analyzed the data. A.F., M.Mc., P.M.,
MDAR Reproducibility Checklist
data curation. Furthermore, we thank E. Lium and team at Mount Sinai D.R.M., D.S., and S.S. performed experiments. A.W., C.C.-C., and F.K.
Innovation Partners for continuous support and V. Sarić and team at wrote the manuscript. All authors edited and approved the manuscript. View/request a protocol for this paper from Bio-protocol.
Mount Sinai’s Development Office for fundraising and for taking many Competing interests: Mount Sinai has licensed serological assays
little things off our shoulders during this difficult time. Finally, we thank to commercial entities and has filed for patent protection for serological 10 July 2020; accepted 26 October 2020
P. Palese and the Department of Microbiology and D. Charney and assays. J.A. reports grants for multicenter clinical trials: Atea (COVID), Published online 28 October 2020
the Icahn School of Medicine at Mount Sinai’s Dean’s Office for strong Frontier Technology (HIV), Gilead Sciences (COVID and HIV), Janssen 10.1126/science.abd7728
Downloaded from http://science.sciencemag.org/ on December 4, 2020
Wajnberg et al., Science 370, 1227–1230 (2020) 4 December 2020 4 of 4
Robust neutralizing antibodies to SARS-CoV-2 infection persist for months
Ania Wajnberg, Fatima Amanat, Adolfo Firpo, Deena R. Altman, Mark J. Bailey, Mayce Mansour, Meagan McMahon, Philip
Meade, Damodara Rao Mendu, Kimberly Muellers, Daniel Stadlbauer, Kimberly Stone, Shirin Strohmeier, Viviana Simon,
Judith Aberg, David L. Reich, Florian Krammer and Carlos Cordon-Cardo
Science 370 (6521), 1227-1230.
DOI: 10.1126/science.abd7728originally published online October 28, 2020
SARS-CoV-2 antibodies persist
As the number of daily COVID-19 cases continues to mount worldwide, the nature of the humoral immune
response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) remains uncertain. Wajnberg et al. used a
Downloaded from http://science.sciencemag.org/ on December 4, 2020
cohort of more than 30,000 infected individuals with mild to moderate COVID-19 symptoms to determine the robustness
and longevity of the anti−SARS-CoV-2 antibody response. They found that neutralizing antibody titers against the
SARS-CoV-2 spike protein persisted for at least 5 months after infection. Although continued monitoring of this cohort will
be needed to confirm the longevity and potency of this response, these preliminary results suggest that the chance of
reinfection may be lower than is currently feared.
Science, this issue p. 1227
ARTICLE TOOLS http://science.sciencemag.org/content/370/6521/1227
SUPPLEMENTARY http://science.sciencemag.org/content/suppl/2020/10/27/science.abd7728.DC1
MATERIALS
RELATED http://stm.sciencemag.org/content/scitransmed/12/550/eabc3539.full
CONTENT
http://stm.sciencemag.org/content/scitransmed/12/559/eabc3103.full
http://stm.sciencemag.org/content/scitransmed/12/556/eabc7075.full
http://stm.sciencemag.org/content/scitransmed/12/555/eabc9396.full
REFERENCES This article cites 22 articles, 8 of which you can access for free
http://science.sciencemag.org/content/370/6521/1227#BIBL
PERMISSIONS http://www.sciencemag.org/help/reprints-and-permissions
Use of this article is subject to the Terms of Service
Science (print ISSN 0036-8075; online ISSN 1095-9203) is published by the American Association for the Advancement of
Science, 1200 New York Avenue NW, Washington, DC 20005. The title Science is a registered trademark of AAAS.
Copyright © 2020 The Authors, some rights reserved; exclusive licensee American Association for the Advancement of
Science. No claim to original U.S. Government Works
You might also like
- How Does Hypnosis Work Ebook Uncommon KnowledgeDocument12 pagesHow Does Hypnosis Work Ebook Uncommon KnowledgeHarsh TripathiNo ratings yet
- As A General Goal, Aim For at Least 30 Minutes of Moderate Physical Activity Every Specific Fitness Goals, You May Need To Exercise MoreDocument5 pagesAs A General Goal, Aim For at Least 30 Minutes of Moderate Physical Activity Every Specific Fitness Goals, You May Need To Exercise MoreJessa Briones100% (1)
- Pedo 2016-18 PDFDocument4 pagesPedo 2016-18 PDFJude Aldo PaulNo ratings yet
- 2021 NATURE Neutralizing Antibody Titres in SARS-CoV-2Document7 pages2021 NATURE Neutralizing Antibody Titres in SARS-CoV-2Yuna SaspitaNo ratings yet
- Jurnal CT ValueDocument3 pagesJurnal CT ValueMetha AgustinaNo ratings yet
- Journal Pre-Proof: Kidney InternationalDocument22 pagesJournal Pre-Proof: Kidney InternationalMohammed Shuaib AhmedNo ratings yet
- Antibody Status and Incidence of Sars-Cov-2 Infection in Health Care WorkersDocument8 pagesAntibody Status and Incidence of Sars-Cov-2 Infection in Health Care Workerscimedat524No ratings yet
- Sars C0V2 NucleoproteinsDocument20 pagesSars C0V2 NucleoproteinsFlorin CazanNo ratings yet
- Journal of Infection: Letter To The EditorDocument2 pagesJournal of Infection: Letter To The EditorJimmy A. Camones ObregonNo ratings yet
- Antibody Status and Incidence of Sars-Cov-2 Infection in Health Care WorkersDocument8 pagesAntibody Status and Incidence of Sars-Cov-2 Infection in Health Care WorkerskiranaNo ratings yet
- Serology Assays To Manage COVID-19Document3 pagesSerology Assays To Manage COVID-19Walid BoukhelkhalNo ratings yet
- Paper Grupo 5Document12 pagesPaper Grupo 5RobertoVeraNo ratings yet
- Ac and VaccineDocument15 pagesAc and VaccineMayaLunaNo ratings yet
- Journal Pre-Proof: Antiviral ResearchDocument16 pagesJournal Pre-Proof: Antiviral ResearchdipogoNo ratings yet
- Journal of Clinical Microbiology-2021-Higgins-JCM.03149-20.fullDocument20 pagesJournal of Clinical Microbiology-2021-Higgins-JCM.03149-20.fullOmar Cucho GamboaNo ratings yet
- 1 s2.0 S0166093420302767 MainDocument2 pages1 s2.0 S0166093420302767 MainbelaariyantiNo ratings yet
- Quantifying The Risk of Sars Cov 2 Reinfection Over TimeDocument11 pagesQuantifying The Risk of Sars Cov 2 Reinfection Over TimeJimmy A. Camones ObregonNo ratings yet
- Id Now NP Rna VLDocument5 pagesId Now NP Rna VLluis achaNo ratings yet
- Comparison of Four Sars-Cov-2 Neutralization AssaysDocument14 pagesComparison of Four Sars-Cov-2 Neutralization AssaysNandagopal PaneerselvamNo ratings yet
- 39 Dynamics of Antibody Response To CoronaVac VaccineDocument10 pages39 Dynamics of Antibody Response To CoronaVac Vaccinenadhia rahdaNo ratings yet
- Abstract 35867632Document1 pageAbstract 35867632elian nuñezNo ratings yet
- Presence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)Document12 pagesPresence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)azizk83No ratings yet
- Presence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)Document12 pagesPresence and Short-Term Persistence of SARS-CoV-2 (Ocak 2021)azizk83No ratings yet
- Fyhb 2 Pac 2 Ubuicrsjh 7 Z 6 FXVCCB 5 UkezDocument3 pagesFyhb 2 Pac 2 Ubuicrsjh 7 Z 6 FXVCCB 5 UkezLeonel RiveraNo ratings yet
- Sars-Cov-2 Cellular Immune Response in Uninfected Health Care Workers With Prolonged and Close Exposure To Covid-19 PatientsDocument14 pagesSars-Cov-2 Cellular Immune Response in Uninfected Health Care Workers With Prolonged and Close Exposure To Covid-19 PatientsAlexis Guevara QuijadaNo ratings yet
- Jurnal 1Document6 pagesJurnal 1Zha Zha Nurul ZahraNo ratings yet
- Research Letter: Lili Chan, Nicholas Fuca, Etti Zeldis, Kirk N. Campbell, and Aisha ShaikhDocument3 pagesResearch Letter: Lili Chan, Nicholas Fuca, Etti Zeldis, Kirk N. Campbell, and Aisha ShaikhBala MuraliNo ratings yet
- Lakshmanappa Et Al. - 2021 - SARS-CoV-2 Induces Robust Germinal Center CD4 T Follicular Helper Cell Responses in Rhesus Macaques - NaturDocument14 pagesLakshmanappa Et Al. - 2021 - SARS-CoV-2 Induces Robust Germinal Center CD4 T Follicular Helper Cell Responses in Rhesus Macaques - NaturCarlNo ratings yet
- Application of Real-Time PCR For Determination of Antiviral Drug Susceptibility of Herpes Simplex VirusDocument5 pagesApplication of Real-Time PCR For Determination of Antiviral Drug Susceptibility of Herpes Simplex VirusMinh TriếtNo ratings yet
- 32 165 1 PB PDFDocument5 pages32 165 1 PB PDFKennyShelva266No ratings yet
- Breakthrough COVID-19 Infections in HCWDocument11 pagesBreakthrough COVID-19 Infections in HCWPatrick Leonard G. CoNo ratings yet
- Neutralizing Antibody Responses To Sars-Cov-2 in A Covid-19 Recovered Patient Cohort and Their ImplicationsDocument20 pagesNeutralizing Antibody Responses To Sars-Cov-2 in A Covid-19 Recovered Patient Cohort and Their ImplicationsDiego MartinsNo ratings yet
- Covid-19 Breakthrough Infections in Vaccinated Health Care WorkersDocument11 pagesCovid-19 Breakthrough Infections in Vaccinated Health Care WorkerskajelchaNo ratings yet
- NEJMoa 2028436Document12 pagesNEJMoa 2028436arman ahdokhshNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesArum Rahmawatie VirgieNo ratings yet
- Eurosurv 27 42 5Document13 pagesEurosurv 27 42 5Eben Leonel Albano MaiopueNo ratings yet
- Seroprevalence and Correlates of Sars-Cov-2 Neutralizing Antibodies From A Population-Based Study in Bonn, GermanyDocument10 pagesSeroprevalence and Correlates of Sars-Cov-2 Neutralizing Antibodies From A Population-Based Study in Bonn, GermanyLaurin LibudaNo ratings yet
- E601 FullDocument6 pagesE601 FullZakirNo ratings yet
- Ifcc Interim Guidelines On Serological Testing of Antibodies Against Sars Cov 2Document8 pagesIfcc Interim Guidelines On Serological Testing of Antibodies Against Sars Cov 2laboratorio clinico HPASNo ratings yet
- Reacao Cruzada SARSCOV Doencas AutoimunesDocument4 pagesReacao Cruzada SARSCOV Doencas AutoimunesEduardoNo ratings yet
- Supplement: Change in Saliva RT-PCR Sensitivity Over The Course of Sars-Cov-2 InfectionDocument3 pagesSupplement: Change in Saliva RT-PCR Sensitivity Over The Course of Sars-Cov-2 InfectionAdeline IntanNo ratings yet
- UntitledDocument1,450 pagesUntitledmikeNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesmeNo ratings yet
- 1 s2.0 S0264410X22005436 MainDocument5 pages1 s2.0 S0264410X22005436 MainSplitter IdNo ratings yet
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 SigalAme DNo ratings yet
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 Sigalenota15No ratings yet
- Rapid Evaluation of Covid-19 Vaccine Effectiveness Against Symptomatic Infection With Sars-Cov-2 Variants by Analysis of Genetic DistanceDocument16 pagesRapid Evaluation of Covid-19 Vaccine Effectiveness Against Symptomatic Infection With Sars-Cov-2 Variants by Analysis of Genetic DistancealinNo ratings yet
- Anti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsDocument6 pagesAnti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsdhairyasheelNo ratings yet
- Mm7003e3 HDocument6 pagesMm7003e3 HShuvo H AhmedNo ratings yet
- PIIS0085253821003483Document3 pagesPIIS0085253821003483Bala MuraliNo ratings yet
- Antecedentes Aqaa140Document10 pagesAntecedentes Aqaa140Omar Cucho GamboaNo ratings yet
- The Establishment of Reference Sequence For Sars Cov 2 and Variation AnalysisDocument8 pagesThe Establishment of Reference Sequence For Sars Cov 2 and Variation AnalysisYulaimy BatistaNo ratings yet
- Lung Ultrasonography For The Diagnosis of SARS-CoV-2 Pneumonia in The Emergency DepartmentDocument10 pagesLung Ultrasonography For The Diagnosis of SARS-CoV-2 Pneumonia in The Emergency DepartmentFannyRivera27No ratings yet
- Stroke in Two Children With Mycoplasma Pneumoniae Infection A Causal or Casual RelationshipDocument15 pagesStroke in Two Children With Mycoplasma Pneumoniae Infection A Causal or Casual Relationshipwawa chenNo ratings yet
- Aqac126 303Document2 pagesAqac126 303Starix UkrNo ratings yet
- Ijerph-18-11451 Meta Analysis StudyDocument14 pagesIjerph-18-11451 Meta Analysis StudySumit BediNo ratings yet
- Correspondence: Antibody Response To First Bnt162B2 Dose in Previously Sars-Cov-2-Infected IndividualsDocument2 pagesCorrespondence: Antibody Response To First Bnt162B2 Dose in Previously Sars-Cov-2-Infected IndividualsmujeebNo ratings yet
- Sars-Cov-2 Mrna Vaccines Induce Persistent Human Germinal Centre ResponsesDocument22 pagesSars-Cov-2 Mrna Vaccines Induce Persistent Human Germinal Centre ResponsesPedro Andrés R. SánchezNo ratings yet
- Sars-Cov-2 Evolution and Vaccines: Cause For Concern?: CommentDocument3 pagesSars-Cov-2 Evolution and Vaccines: Cause For Concern?: Commenthymen busterNo ratings yet
- Measuringtheserologic Responsetosevereacute Respiratorysyndrome Coronavirus2Document12 pagesMeasuringtheserologic Responsetosevereacute Respiratorysyndrome Coronavirus2Chris KontomarisNo ratings yet
- Diagnostics: Detection and Differentiation of Sars-Cov-2, Influenza, and Respiratory Syncytial Viruses by CrisprDocument11 pagesDiagnostics: Detection and Differentiation of Sars-Cov-2, Influenza, and Respiratory Syncytial Viruses by CrisprHuy Trần ThiệnNo ratings yet
- In Vivo Assessment of Antiviral Reactivity in Chronic HIV InfectionDocument7 pagesIn Vivo Assessment of Antiviral Reactivity in Chronic HIV InfectionFrontiersNo ratings yet
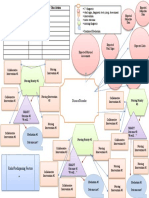
- HAN - Graphic OrganizerDocument1 pageHAN - Graphic OrganizerJared Michael BergerNo ratings yet
- CH 1Document10 pagesCH 1Jared Michael BergerNo ratings yet
- Aripiprazole: A Novel Atypical Antipsychotic Drug With A Uniquely Robust PharmacologyDocument20 pagesAripiprazole: A Novel Atypical Antipsychotic Drug With A Uniquely Robust PharmacologyJared Michael BergerNo ratings yet
- Coronavirus 2019-nCoV Info TipsforRestaurantsDocument1 pageCoronavirus 2019-nCoV Info TipsforRestaurantsJared Michael BergerNo ratings yet
- A Systematic Review of SARS-CoV-2 VaccineDocument14 pagesA Systematic Review of SARS-CoV-2 VaccineJosé Luis García MezaNo ratings yet
- Title: Decreased Sars-Cov-2 Viral Load Following VaccinationDocument12 pagesTitle: Decreased Sars-Cov-2 Viral Load Following VaccinationJared Michael BergerNo ratings yet
- Immunogenicity of One-And Two-Dose Regimens of The Ad26.COV2.S COVID-19 Vaccine Candidate in Adult and Aged Rhesus MacaquesDocument36 pagesImmunogenicity of One-And Two-Dose Regimens of The Ad26.COV2.S COVID-19 Vaccine Candidate in Adult and Aged Rhesus MacaquesJared Michael BergerNo ratings yet
- Anemia, Acute Bronchitis and Adequate NutritionDocument39 pagesAnemia, Acute Bronchitis and Adequate NutritionSetiawan DanuNo ratings yet
- Reporte 2020 de La Oficina de Asuntos Globales de Estados UnidosDocument72 pagesReporte 2020 de La Oficina de Asuntos Globales de Estados UnidosAristegui NoticiasNo ratings yet
- Emt Schedule 2014-15 RVD 10-27-14Document3 pagesEmt Schedule 2014-15 RVD 10-27-14api-257829824No ratings yet
- Annotated Bibliography and SynthesisDocument6 pagesAnnotated Bibliography and SynthesismperezveNo ratings yet
- Peds EORDocument29 pagesPeds EORAndrew BowmanNo ratings yet
- The Story of Florence NightingaleDocument2 pagesThe Story of Florence NightingaleBella RettobNo ratings yet
- Isolation 2007Document219 pagesIsolation 2007Jorge CunhaNo ratings yet
- Mmha EcoDocument54 pagesMmha EcoAlfredo De Ocampo JrNo ratings yet
- RTI 17 Manual MOH R Central Ward-4Document55 pagesRTI 17 Manual MOH R Central Ward-4SwarupaNo ratings yet
- Hospital Case Study FlexsimDocument2 pagesHospital Case Study FlexsimMano KanthanathanNo ratings yet
- Testicular PainDocument16 pagesTesticular PainkdwazirNo ratings yet
- School StressDocument24 pagesSchool StressShaheen Khan WarsiNo ratings yet
- 2020 ISMP - Smart Infusion Pumps-FINALDocument38 pages2020 ISMP - Smart Infusion Pumps-FINALmochkurniawanNo ratings yet
- Suspected Adverse Drug Reaction Reporting Form: CdscoDocument2 pagesSuspected Adverse Drug Reaction Reporting Form: CdscoNaveen Kumar G TNo ratings yet
- IATA Covid-19 - GuidanceDocument2 pagesIATA Covid-19 - GuidanceMahashweta ChakrabortyNo ratings yet
- Practice Guidelines For Central Venous Access PDFDocument35 pagesPractice Guidelines For Central Venous Access PDFJulio AltamiranoNo ratings yet
- Best COVID 04-01-20 (Before Merger) 1Document16 pagesBest COVID 04-01-20 (Before Merger) 1Ron SchottNo ratings yet
- Aacn Critical CareDocument40 pagesAacn Critical Careapi-348346538No ratings yet
- Methodology of Seasonal Waves of Respiratory.2Document12 pagesMethodology of Seasonal Waves of Respiratory.2Shiwali SinghNo ratings yet
- Practical Cardio-Oncology (2019, CRC Press)Document261 pagesPractical Cardio-Oncology (2019, CRC Press)Anitei GabrielaNo ratings yet
- Jurnal Akk Pengadaan Bahan MakananDocument14 pagesJurnal Akk Pengadaan Bahan Makananmelisa yuniartiNo ratings yet
- Translation of Evidence Into Nursing PracticeDocument8 pagesTranslation of Evidence Into Nursing PracticeNica C. MatsusakiNo ratings yet
- ST Gallen 2017 - Early Breast CancerDocument13 pagesST Gallen 2017 - Early Breast CancerPaulo Cesar Castañeda RuizNo ratings yet
- Formula Masking 1Document111 pagesFormula Masking 1Caroline RochaNo ratings yet
- Case-Study-12 8 2Document16 pagesCase-Study-12 8 2Jaylen CayNo ratings yet
- Shimla Nursing College Annadale Bai BerbaiDocument17 pagesShimla Nursing College Annadale Bai Berbaigill priyaNo ratings yet
- Proposal For CSR Support of A Lifeline Express Project in The North-East or BiharDocument13 pagesProposal For CSR Support of A Lifeline Express Project in The North-East or BiharSaurabh GuravNo ratings yet