Professional Documents
Culture Documents
617 911 1 SM
Uploaded by
mehakOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
617 911 1 SM
Uploaded by
mehakCopyright:
Available Formats
Indonesian J. Pharm. Vol. 24 No.
4 : 245 – 252
ISSN-p : 2338-9427
DOI: 10.14499/indonesianjpharm24iss4pp245
Research Article
DESIGN AND OPTIMIZATION OF SOLID LIPID
NANOPARTICLES (SLNs) OF ZOLMITRIPTAN FOR THE
MANAGEMENT OF MIGRAINE
Deepti Singh1, Navneet Garud2, Akanksha Garud1,*
1Dept of Pharmaceutics ABSTRACT
Institute of Professional Solid lipid nanoparticles (SLNs) of zolmitriptan were
Studies-College of produced by solvent emulsification-diffusion technique. Soya
Pharmacy, Gwalior - lecithin and poloxamer 188 were used as surfactants and
474001, India stabilizers of the particles. The formulations were optimized for
2School of Studies in
independent variables (amount of stearic acid, amount of lecithin
Pharmaceutical Sciences, and homogenization time) in order to achieve desired particle size
Jiwaji University, Gwalior, with maximum percent entrapment efficiency (% EE). Prepared
India
SLNs were characterized by transmission electron microscopy
(TEM), atomic force microscopy (AFM) and zeta potential
Submitted: 23-04-2013
measurements. To achieve our goal, eight formulations (F1–F8) of
Revised: 22-06-2013
SLNs were prepared by solvent injection technique and optimized
Accepted: 04-07-2013
by 23 full-factorial design. The responses of the design were
*Corresponding author analyzed using Minitab 15. On the basis of software analysis,
Akanksha Garud formulation F8 was selected as optimized formulation and was
evaluated for the independent parameters. Optimized formulation
Email : showed particle size of 340nm, percent entrapment efficiency (EE)
akanksha.garud@gmail.com of 81.36 and 79.11% of in-vitro drug release after 24h. The
release kinetics of the optimized formulation best fitted the
Higuchi model.
Key words: solid lipid nanoparticles, zolmitriptan, solvent emulsification-
diffusion technique, in-vitro release.
INTRODUCTION migraine symptoms, including pain, nausea, and
Migraine is a common and frequently photo-or phonophobia (Gayathri, et al., 2000).
disabling headache disorder characterized by Patients with migraine generally suffer from
recurrent episodic attacks of moderate to nausea and vomiting; oral treatment can
severe headache variably accompanied by therefore be inconvenient or could fail (Kolsure,
neurological, gastrointestinal and/or autonomic et al., 2012). The inherent shortcomings of
symptoms (Goadsby et al., 2002). There are two conventional drug delivery and the potential of
major forms of migraine: migraine without aura nanoparticles as drug delivery systems have
and migraine with aura. The aura consists of offered tremendous scope for researchers in
focal neurologic symptoms (usually visual this field and are fast moving from concept to
symptoms) that precede or accompany reality.
headache, and it appears in 15-25% of migraine Nanoparticles based on solid lipids have
sufferers. Migraine affects approximately 18% been proposed as a promising alternative to
of women and 6% of men in western countries, colloidal drug delivery system, polymeric
and 20-40% of patients experience an attack nanoparticles, and liposomes. Compared to
frequency of greater than one per month traditional carriers, the solid lipid nanoparticles
(Belvis et al., 2009). (SLNs) combine the advantages of polymeric
Zolmitriptan, 4S-4-({3-[2-(dimethylamino) nanoparticles and o/w fat emulsions for
ethyl]-1H-indol-5-yl} methyl)-1, 3-oxazolidin - drug administration such as good tolerability,
2-one, is a second generation triptan prescribed lower cytotoxicity (Muller, et al., 1996), higher
for patients with migraine attacks, with or bioavailability by oral administration (Yang, et
without an aura, and cluster headaches. It has a al., 1999), and increase in the drug stability
selective action on serotonin (5-HT1B/1D) (Mehnert and Mader, 2001). Other advantages
receptors and is very effective in reducing of lipid excipients, such as biodegradability and
Volume 24 Issue 4 (2013) 245
Design and Optimization of Solid Lipid Nanoparticles
cost effectiveness (Mukherjee, et al., 2007), and % entrapment efficiency (EE) were taken
promote their use as novel drug carriers. as response parameters.
Consisting of physiological and biodegradable
lipids, lipid nanoparticles are suitable for the Preparation of SLNs
incorporation of lipophilic, hydrophilic, and Solvent emulsification-diffusion technique
poorly water-soluble drugs within the lipid Solid lipid nanoparticles of zolmitriptan
matrix in considerable amounts (Bunjes, et al., were prepared by the solvent emulsification-
2001). Lipidic carriers used to prepare SLNs diffusion technique. The solvent (ethyl acetate)
can be highly purified lipids such as tristearin or and water were mutually saturated for 10min at
tripalmitin, hard fats such as stearic acid or room temperature in order to generate
behenic acid, waxes such as cetylpalmitate, and equilibrium between the two liquids. Heating
acylglycerol mixtures such as compritol or up to 70°C was required to solubilize the lipid,
glycerylmonostearate (GMS) (Souto, 2006). the saturation step was performed at this
In the present study, stearic acid has temperature. Typically, specified amount of
been used to formulate SLNs. The selection of lipid, 10mg of drug zolmitriptan were dissolved
stearic acid was its lipid matrix is made from in 10mL of water-saturated solvent and
physiological lipids that decrease the danger of this organic phase (internal phase) was
acute and chronic toxicity in epidemiologic and emulsified with 20mL of the solvent-
clinical studies. Stearic acid was associated with saturated aqueous solution containing 10% w/v
lowered LDL cholesterol in comparison with of stabilizer(dispersion medium) using a
other saturated fatty acids indicating it less mechanical stirrer at 3000rpm for 15min. After
unhealthy than other saturated fatty acids. formation of an oil in-water emulsion, 80mL of
water (dilution medium) was added to the
MATERIAL AND METHODS system in order to allow solvent diffusion into
Zolmitriptan was a gift from Zydus the continuous phase thus causing the
Cadila Health Care Limited, Ahmedabad. aggregation of the lipid in nanoparticles. When
Stearic acid (Molar mass 284.48g mol−1, melting heating was required to dissolve the lipid, both
point 69.6°C, density 0.84g/cm3 at 70°C) was phases were maintained at 70°C and the
purchased from Clearsynth Labs, Andheri, diffusion step was performed either at RT or at
Mumbai, India. Soya lecithin (Epikuron, 200) the temperature under which the lipid was
was purchased from LeciImpex, Indore, M.P. dissolved. Throughout the process constant
PoloxamerF 68 (molecular weight 12 kDa) was stirring was maintained. Thereafter, the
purchased from Balaji Drugs, Surat. Dialysis dispersion was centrifuged to 10,000rpm for
bag (molecular weight cut off (MWCO) 12- 30min at 10°C in Remi cooling centrifuge
14kDa; pore size 2.4nm) was supplied by Hi (Model C-24BL, VCAO-779, Vasai, India), and
Media, Mumbai, India. Other chemicals used aggregates were purified by dialysis bag and
were of analytical grade. resuspended to 10mL distilled water containing
4% poloxamer F68 (by weight) as stabilizer
Experimental design of SLNs with stirring at 1,000rpm for 10min.
In this study, a 23 full-factorial expe-
rimenttal design was used to optimize SLNs. In Purification of zolmitriptan-loaded SLNs
this ‘2’ indicates levels i.e. higher and lower and Purification of zolmitriptan-loaded SLNs
‘n’ is factor i.e. concentration of stearic acid, was done by using dialysis technique.
concentration of soya lecithin and time for Sedimented soft pellet was taken in the
homogenization. Eight formulations of SLNs dialysis bag and sealed at both ends. The
(F1 to F8) were designed. In order to optimize, dialysis bag was then immersed into 100mL of
the amount of stearic acid (X1), amount of distilled water containing 0.2% w/v sodium
lecithin (X2) and homogenization time (X3) lauryl sulphate and stirred at 100 rpm for
were selected as independent variables. Each 30min. Five milliliter of sample was withdrawn
factor was set at a high level and low level. The at different time intervals of 5, 10, 15, and
actual values and coded values of different 30min. The samples were diluted appropriately
variables are given in table I. The particle size and analyzed for amount of drug by UV/
246 Volume 24 Issue 4 (2013)
Deepti Singh
visible spectrophotometer (JASCO V-30 UV Drug loading capacity
Spectrophotometer) at 283nm (Shah and The drug loading (DL) capacity of
Pathak, 2010). Zolmitriptan was also calculated using the
formula:
Characterization of zolmitriptan SLNs DL (%)=(Winitial – Wfree)/ Wlipid X 100
Transmission electron microscopy where, Winitial is the total amount of
Structure of the SLNs were studied zolmitriptan used in preparation of solid lipid
using Morgagni 268D transmission electron nanoparticles, Wfree is the amount of
microscopy (TEM) FEI, Netherland operating zolmitriptan detected in the supernatant, and
at 70KV and capable of point to point Wlipid is the amount of lipid in the preparation
resolution. Combination of bright field imaging of solid lipid nanoparticles, respectively (Lv et
at increasing magnification and diffraction al., 2009).
modes were used to reveal the form and
size of SLNs. In order to perform the Particle size distribution, zeta potential and
TEM observations, a drop of SLN polydispersity index (PDI)
dispersion was applied on carbon coated The zeta potential and size distribution
grid with 2% phosphotungstic acid (PTA) of SLNs were measured in triplicates in
and was left for 30sec. The dried coated grid multimodal move (Doijad et al., 2008). The
was taken on a slide and covered with a cover particle size distribution and polydispersity
slip. The slide was observed under the electron index were determined using computerized
microscope (Garcia-Fuentes et al., 2003). Malvern instrument particle size analyser v2.0
(Malvern UK) and zeta potential was
Atomic force microscopy (AFM) determined by using Malvern zetasizer
By using AFM one can not only image inspection system v2.2 (Malvern UK) at 25°C.
the surface in atomic resolution but also Prior to the measurement, SLNs were diluted
measure the force at nano-newton scale. The with distilled water and the measurements were
sample preparation for AFM is simple and taken in triplicate (n=3).
quick and it allows the material to be preserved
in its original form. For AFM study, one In-vitro release
drop of formulation was spread out In vitro release was evaluated by using a
homogenously on separate mica piece (5mm × dialysis membrane diffusion technique (Reddy
5mm) and the sample was then allowed to dry et al., 2005). The drug release from Zolmitriptan
at room temperature for one day before SLNs (ZOL-SLNs) was performed in PBS (pH
imaging at a scan speed of 2Hz (Dubes et al., 7.4) using dialysis membrane. A dialysis
2003). membrane (Himedia, Mumbai) weight cut off
between 12.000 and 14.000 was used. The
Entrapment efficiency membrane was soaked in distilled water for 12
Entrapment efficiency (EE) of SLNs hours before the release study. Two mL ZOL-
was determined by centrifugation method SLNs suspension was placed in dialysis
with rotor at 10,000rpm for 30min. The membrane tied at both ends to form dialysis
supernatant was collected. The quantity of drug bags and these dialysis bags were subsequently
present in the supernatant was determined by placed in flasks containing 50mL dissolution
the UV Spectrophotometer. The entrapment medium at 100rpm at 37°C. Aliquots of the
efficiency was calculated using the following dissolution medium were withdrawn at each
equation. time interval and the same volume of fresh
EE(%)=(Winitial-Wfree)/Winitial X 100 dissolution medium was added to the flask to
where, Winitial is the total amount of maintain a constant volume. Drug
zolmitriptan used in preparation of solid lipid concentration in the dissolution medium was
nanoparticles and Wfree is the amount of determined.The absorbance was used to
zolmitriptan detected in the supernatant, calculate concentration using calibration curve.
respectively (Bhaskar et al., 2009, Sarmento et The experiments were performed in triplicate.
al., 2007).
Volume 24 Issue 4 (2013) 247
Design and Optimization of Solid Lipid Nanoparticles
Table I. Formulations of zolmitriptan SLNs
Code Experiment Factor Factor Factor Particle size Entrapment
A B C (nm) efficiency (%)
F1 1 - - - 410 57.12
F2 A + - - 450 76.42
F3 B - + - 320 58.36
F4 Ab + + - 390 75.48
F5 C - - + 360 60.14
F6 Ac + - + 430 77.81
F7 Bc - + + 250 59.16
F8 Abc + + + 340 81.36
Coded values
Factor A = Amount of stearic acid (low level 200mg, high level 600mg)
Factor B = Amount of soya lecithin (low level 200mg, high level 800mg)
Factor C = Stirring time (low level 15min, high level 30min)
- denotes lower and + denotes higher limit, respectively.
Statistical analysis removed from the sediment of SLNs by
Statistical analysis was performed with purification by dialysis technique. Dialysis
Minitab 15 software. Results were expressed as technique was considered suitable, as
mean ± standard deviation (SD). Statistical zolmitriptan with a low molecular weight could
significance was determined using analysis of be efficiently removed using dialysis bag made
variance (ANOVA) with P≤0.05 as a minimal of Himedia membrane. Consequently,
level of significance. purification was accomplished by monitoring
percent free drug removed after 5, 10, 15, and
RESULTS AND DISCUSSION 30min, respectively. Initially, the percent free
Formulation considerations drug removed increased with time and reached
SLNs were prepared by solvent plateau levels by 30min. Slowest% drug release
emulsification-diffusion technique that relies on using dialysis technique after 30 min was
the rapid diffusion of the solvent across the observed by formulation F8 (2.40%) and
solvent-lipid interface with the aqueous phase. highest % drug release was observed by
Thus, the diffusion rate of the organic solvent formulation F4 (20.66%).
through the interface seems to be a critical ANOVA was used to check any
parameter for particle size determination significant difference between the percent free
(Schubert et al., 2003). The major problem with drug removed at 15 and at 30 min. It was
the formulation of SLNs is its separation. observed that although the extent of free drug
Owing to their small size and low density of in various SLN formulations was significantly
lipids, SLNs present difficulty in settling upon different (p < 0.05), there was no significant
centrifugation. To overcome this problem, in difference in percent free drug removed after
the present study, the pH of the dispersion was purification time of 15 and 30min (p > 0.05).
reduced to 2-3 to adjust the zeta potential for Thus, free zolmitriptan from sediment of SLNs
aggregation of SLNs (Hu et al., 2002) and could be efficiently removed after purification
facilitate centrifugation and consequently for 15min and hence was used throughout the
separation. experiment.
A possibility of presence of zolmitriptan
particles in the sediment of zolmitriptan-loaded Statistical analysis of experimental data
SLNs was explored. It is suggested that these by minitab 15 software
particles can potentially interfere in the in The results of the experimental design
vitro and in vivo behavior of zolmitriptan-loaded were analyzed using Minitab software that
SLNs. Therefore, free drug particles were provided considerable useful information and
248 Volume 24 Issue 4 (2013)
Deepti Singh
Figure 1. In-vitro drug release of prepared SLN formulations
Figure 2. Response surface plots showing particle size as dependent variables plotted against two
independent parameters (stearic acid and homogenization time) taking one parameter (lecithin
amount) as constant of the prepared SLN formulations.
reaffirmed the utility of statistical design for Particle size
conduct of experiments. The selected Particle size (nm) = 546 + 0.215 Stearic
independent variables like the amount of stearic acid (mg) - 0.136 Lecithin (mg) - 3.93 Stirring
acid, amount of lecithin, and stirring time time (min)
significantly influenced the particle size, % EE, S = 10.8167 R-Sq = 99.0% R-Sq(adj) =
and % cumulative drug release (CDR) that is 98.2%
very much evident from the results in table I.
The in vitro drug release profiles of F1 to F8 are Entrapment efficiency (EE)
shown in figure 1. EE (%) = 47.0 + 0.0444 Stearic acid
Based on the results obtained for particle (mg) - 0.000347 Lecithin (mg) + 0.0978 Stirring
size, % EE, the response polynomial time (min)S = 0.836324 R-Sq = 99.6% R-
coefficients were determined in order to Sq(adj) = 99.2%.
evaluate each response. Each response These equations were utilized for
coefficient was studied for its statistical validation of the experimental design. The
significance. The non-significant response response surface plots generated using
coefficients were deleted, and the following polynomial equations represent simultaneous
significant polynomial response equation(s) for effect of any two variables on response
particle size, % EE, were generated. parameter taking one variable at constant level.
Volume 24 Issue 4 (2013) 249
Design and Optimization of Solid Lipid Nanoparticles
Figure 3. Transmission electron microscopy (TEM), with magnification
150 KX.
Figure 4. Atomic force microscopy (AFM) images of SLNs on 1µm scale.
On carefully observing these plots, the The release kinetics was evaluated by
qualitative effect of each variable on each fitting the data into first order (r2 = 0.7421),
response parameter can be visualized. Figure 2 zero order (r2 = 0.9428), Higuchi (r2 = 0.9747)
shows response surface plots with particle size and Peppas equations (r2 = 0.9330). Based on
as dependent variables plotted against two the results, the release of zolmitriptan from
independent parameters (stearic acid and SLNs best-fitted Higuchi equation
homogenization time) taking one parameter (r2 = 0.9747) and the possible mechanisms
(lecithin amount) as constant. for the drug release from F8 might be
Response graph shows the variation in diffusion of the drug from the matrix and
independent variables strongly affect the matrix erosion resulting from degradation of
dependent variable. The wavy surface show lipids. A similar report has been made by
more variations in dependent variable on other researchers as well (Souto, 2006 and
increasing or decreasing the value of Lai et al., 2009). Thus, the in-vitro release
independent variable and almost straight data indicated that the optimized SLNs were
surface denote less variation in dependent capable of sustaining the release of
variable for same condition. zolmitriptan.
250 Volume 24 Issue 4 (2013)
Deepti Singh
Selection of optimized formulation Attack Therapy. Recent Pat. CNS Drug
Optimized formulation (F8) was selected Discov. 4: 70-81.
on the basis of small particle size, higher Bhaskar K., Anbu J., Ravichandiran V.,
entrapmentefficiency,andhigher in- Vankateswarlu V., Rao YM. 2009. Lipid
vitro cumulative drug release after 24 h. The nanoparticles for transdermal delivery of
optimized formulation was then subjected to flurbiprofen: formulation, in vitro ex
Zeta potential, TEM and AFM. vivo and in vivo studies. Lipids Health
Dis. 8: 1-15.
Zeta potential and Polydispersity Index Bunjes H., Drechsler M., Koch MH., Westesen
(PDI) K. 2001. Incorporation of the model
The zeta potential was determined to be drug ubidecarenone into solid lipid
-35.3 ± 0.02 mV (n=3). The polydispersity nanoparticles. Pharm. Res. 18: 287-293.
index of 0.131 ± 0.12 (n=3) indicated a Doijad RC., Manvi FV., Godhwani DM.,
polydisperse colloidal dispersion. Joseph R., Deshmukh NV. 2008.
Formulation and targeting efficiency of
Transmission Electron Microscopy (TEM)
cisplatin engineered solid lipid
TEM showed that the particles had
nanoparticles, Indian J. Pharm. Sci. 70:
round and uniform shapes. The means
203-207.
diameters of SLNs were in the range of
Dubes A., Parrot LH., Abdelwahed W.,
approximately 260-290nm (Figure 3).
Degobert G., Fessi H., Shahgaldian P.,
Atomic force microscopy
Coleman AW. 2003. Scanning electron
The AFM tapping mode images of microscopy and atomic force
ZOL-SLNs were observed. Both the planner microscopy imaging of solid lipid
and three-dimensional images are presented. nanoparticles derived from amphiphilic
The imaging showed that ZOL-SLNs had a cyclodextrins. Eur. J. Pharm. Biopharm. 55:
spherical shape. The obtained images showed a 279-282.
clear topography of particles (Figure 4). Garcia-FM., Torres D., Alonso MJ. 2003.
Design of lipid nanoparticles for the oral
CONCLUSION delivery of hydrophilic macromolecules.
The present investigation demonstrated Colloids and Surfaces B: Biointerfaces. 27:
that particle size of the nanoparticles can be 159-168.
controlled by varying process variables such as Gayathri DS., Venkatesh P., Udupa, N. 2000.
homogenization time, amount of stearic acid Niosomal sumatriptan succinate for
used and the amount of lecithin. Solid lipid nasal administration. Indian J. Pharm. Sci.
nanoparticles of zolmitriptan were successfully 62: 479-481.
developed to yield an optimized formulation Goadsby PJ., Lipton RB., Ferrari MD. 2002.
with least nanometeric particle size and highest Migraine-current understanding and
possible entrapment efficiency that could treatment. N. Engl. J. Med. 346: 257- 270.
sustain the release of drug for over 24h. Use of Hu FQ., Yuan H., Zhang HH., Fang M. 2002.
23 full-factorial design enabled to develop an Preparation of solid lipid nanoparticles
acceptable formulation using minimum raw with clobetasol propionate by a novel
materials and in minimum time. solvent diffusion method in aqueous
system and physicochemical
ACKNOWLEDGEMENT characterization. Int. J. Pharm. 239: 121-
Authors wish to thank ZydusCadila 128.
Health Care Limited, Ahmedabad for providing Kolsure PK., and Rajkapoor B. 2012.
the gift sample of Zolmitriptan. Development of zolmitriptan gel for
nasal administration. .Asian J. Pharm.
REFERENCES Clin. Res. 5: 88-94.
Belvís R., Pagonabarraga J., Kulisevsky J. 2009. Lai J., Chen J., Lu Y., Sun J., Hu F., Yin Z., Wu
Individual Triptan Selection in Migraine W. 2009. Glyceryl monooleate/
poloxamer 407 cubic nanoparticles as
Volume 24 Issue 4 (2013) 251
Design and Optimization of Solid Lipid Nanoparticles
oral drug delivery systems: I. In zation, in vitro drug release, and stability
vitro evaluation and enhanced oral evaluation. AAPS Pharm. Sci.Tech. 6: 158-
bioavailability of the poorly water- 166.
soluble drug simvastatin. AAPS Pharm. Sarmento B., Martins S., Ferreira D., Souto
Sci. Tech. 10: 960-966. EB. 2007. Oral insulin delivery by means
Lv Q., Yu A., Xi Y., Cui J., Cao F., Zhai G. of solid lipid nanoparticles. Int. J.
2009. Development and evaluation of Nanomedicine. 2: 743-749.
penciclovir-loaded solid lipid nano- Schubert MA., Muller-Goymann CC. 2003.
particles for topical delivery. Int. J. Pharm. Solvent injection as a new approach for
372: 191-198. manufacturing lipid nanoparticles-
Mehnert W., and Mader K. 2001. Solid lipid evaluation of the method and process
nanoparticles. Production, characteriza- parameters. Eur. J. Pharm. Biopharm. 55:
tion and applications. Adv. Drug Del. 125-131.
Rev. 47: 165-196. Shah M., Pathak K. 2010. Development and
Mukherjee S., Ray S., Thakur RS. 2007. The Statistical Optimization of Solid Lipid
current status of solid lipidnanoparticles Nanoparticles of Simvastatin by Using
.Pharmabit 1: 53-60. 23 Full-Factorial Design. AAPS Pharm.
Muller RH., Maaßen S., Weyhers H., Specht F., Sci. Tech. 11: 489-496.
Lucks JS. 1996. Cytotoxicity of Souto EB. 2006. Application of lipid
magnetite loaded polylactide, nanoparticles (SLN and NLC) in food
polylactide/glycolide particles and solid industry. J Food Tech. 4: 90-95.
lipid nanoparticles. Int. J. Pharm. 138: 85- Yang S., Zhu J., Lu Y., Liang B., Yang C. 1999.
94. Body distribution of camptothecin solid
Reddy LH., andMurthy RSR. 2005. Etoposide- lipid nanoparticles after oral
loaded nanoparticles made from administration. Pharm. Res. 16: 751-757.
glyceride lipids: formulation, characteri-
252 Volume 24 Issue 4 (2013)
You might also like
- 595-Article Text-2709-1-10-20201004Document7 pages595-Article Text-2709-1-10-20201004Ellie satrianiNo ratings yet
- Dissolution Enhancement and Formulation of Film CoDocument12 pagesDissolution Enhancement and Formulation of Film CobimaNo ratings yet
- 10 1 1 509 9662 PDFDocument5 pages10 1 1 509 9662 PDFRizky AdyaNo ratings yet
- Development and Characterization of Prednisolone Liposomal Gel For The Treatment of Rheumatoid ArthritisDocument5 pagesDevelopment and Characterization of Prednisolone Liposomal Gel For The Treatment of Rheumatoid Arthritismazahir razaNo ratings yet
- Solid Lipid Nano ParticlesDocument12 pagesSolid Lipid Nano ParticlesGunja ChaturvediNo ratings yet
- Formulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFDocument8 pagesFormulation Development of Ketoprofen Liposomal Gel (KELOMPOK V) PDFTreesna OuwpolyNo ratings yet
- Development and Evaluation of Nanoemulsion of RepaglinideDocument8 pagesDevelopment and Evaluation of Nanoemulsion of Repaglinidevikrantkadam12No ratings yet
- Formulation and Evaluation of Niosomal in Situ GelDocument14 pagesFormulation and Evaluation of Niosomal in Situ GelrandatagNo ratings yet
- Enkapsulasi KetoprofenDocument5 pagesEnkapsulasi KetoprofenFitria NugrahaeniNo ratings yet
- Controlling curcumin-loaded shea butter nanoparticles sizeDocument11 pagesControlling curcumin-loaded shea butter nanoparticles sizeIsabelle sandrine Bouelet NtsamaNo ratings yet
- My Research PaperDocument10 pagesMy Research PaperMamta AroraNo ratings yet
- P 021097104Document8 pagesP 021097104Aamir KhanNo ratings yet
- Patel Deepa R., Patel Laxmanbhai J., Patel Madhabhai M., Patel Advaita BDocument4 pagesPatel Deepa R., Patel Laxmanbhai J., Patel Madhabhai M., Patel Advaita Biabureid7460No ratings yet
- (Bom) Shazly2018Document8 pages(Bom) Shazly2018Eduardo Hösel MirandaNo ratings yet
- 2018 Article 99Document10 pages2018 Article 99IIrsandi JohanNo ratings yet
- Formulasi Sediaan FarmasiDocument11 pagesFormulasi Sediaan FarmasiKukuh PermadiNo ratings yet
- Effect of Pegylated Polypropylene Imine Dendrimers Loaded Imatinib For Anti-Tumor Activity: Synthesis, Characterization and Invivo Evaluation StudiesDocument9 pagesEffect of Pegylated Polypropylene Imine Dendrimers Loaded Imatinib For Anti-Tumor Activity: Synthesis, Characterization and Invivo Evaluation StudiesRAPPORTS DE PHARMACIENo ratings yet
- Project PPT YugeshDocument57 pagesProject PPT Yugeshyugesh shresthaNo ratings yet
- Formulation and Evaluation of Microemulsion Based Topical Hydrogel Containing LornoxicamDocument8 pagesFormulation and Evaluation of Microemulsion Based Topical Hydrogel Containing LornoxicamsafrinpujiNo ratings yet
- Formulation and Evaluation of Multiple Emulation of Diclofenac SodiumDocument7 pagesFormulation and Evaluation of Multiple Emulation of Diclofenac SodiumIJRASETPublicationsNo ratings yet
- FormulationDevelopment GemcitabineHCl DryPowder For IntravenousInfusionDocument16 pagesFormulationDevelopment GemcitabineHCl DryPowder For IntravenousInfusionDo Thanh HoanNo ratings yet
- JPSR 03110106Document9 pagesJPSR 03110106sunilpdNo ratings yet
- Self-Emulsifying Formulation of Indomethacin With Improved Dissolution and Oral AbsorptionDocument12 pagesSelf-Emulsifying Formulation of Indomethacin With Improved Dissolution and Oral AbsorptionKietNo ratings yet
- Gemcitabine Dry Powder Formulation DevelopmentDocument16 pagesGemcitabine Dry Powder Formulation DevelopmentFIRMAN MUHARAMNo ratings yet
- Karakterisasi Sediaan Dan Uji Pelepasan Natrium Diklofenak Dengan Sistem Mikroemulsi Dalam Basis Gel HPC-MDocument10 pagesKarakterisasi Sediaan Dan Uji Pelepasan Natrium Diklofenak Dengan Sistem Mikroemulsi Dalam Basis Gel HPC-MAndi SyahNo ratings yet
- Formulation and In-Vitro Evaluation of Glibenclamide Dry Emulsion in Vegetarian CapsulesDocument5 pagesFormulation and In-Vitro Evaluation of Glibenclamide Dry Emulsion in Vegetarian CapsulesBaru Chandrasekhar RaoNo ratings yet
- Hospital Training ReviewDocument12 pagesHospital Training ReviewMaheshvari VyavhareNo ratings yet
- Miconazole Nitrate From EmulgelDocument6 pagesMiconazole Nitrate From Emulgelasit_m100% (1)
- Glimepiride Sustained Release Tablets Compared to Immediate ReleaseDocument6 pagesGlimepiride Sustained Release Tablets Compared to Immediate ReleaseAnditapitalokaNo ratings yet
- Cellulose AcetaeDocument11 pagesCellulose AcetaeDhole ArchuNo ratings yet
- Sajp2 (4) 315 318Document4 pagesSajp2 (4) 315 318Habibur RahmanNo ratings yet
- Venlafaxine-Loaded Sustained-Release Poly (Hydroxyethyl Methacrylate-Co-Itaconic Acid) Hydrogel Composites: Their Synthesis and in Vitro/in Vivo AttributesDocument8 pagesVenlafaxine-Loaded Sustained-Release Poly (Hydroxyethyl Methacrylate-Co-Itaconic Acid) Hydrogel Composites: Their Synthesis and in Vitro/in Vivo AttributesshamsNo ratings yet
- Optimization of Finasteride Nano-Emulsion Preparation Using Chemometric ApproachDocument5 pagesOptimization of Finasteride Nano-Emulsion Preparation Using Chemometric ApproachNurul Hikmah12No ratings yet
- 4.kalpana ArticleDocument5 pages4.kalpana ArticleBaru Chandrasekhar RaoNo ratings yet
- Development of Curcumin Based Ophthalmic FormulationDocument9 pagesDevelopment of Curcumin Based Ophthalmic FormulationBagus Prasetya WirawanNo ratings yet
- Formulation and Evaluation of Transdermal Patch of Repaglinide PDFDocument9 pagesFormulation and Evaluation of Transdermal Patch of Repaglinide PDFapa menNo ratings yet
- Etoposide JurnalDocument6 pagesEtoposide JurnalShalie VhiantyNo ratings yet
- Nano Particulas en Diseño de Formas FarmaceuticasDocument8 pagesNano Particulas en Diseño de Formas FarmaceuticasMonica Andrea Marulanda GuzmanNo ratings yet
- Design and Statistical Optimization of Glipizide Loaded Lipospheres Using Response Surface MethodologyDocument17 pagesDesign and Statistical Optimization of Glipizide Loaded Lipospheres Using Response Surface MethodologyRoxana PoturNo ratings yet
- Preparation and Evaluation of Wound Healing Activity of Ursolic Acid Nanoemulgel Formulations in RatsDocument11 pagesPreparation and Evaluation of Wound Healing Activity of Ursolic Acid Nanoemulgel Formulations in RatsRAPPORTS DE PHARMACIENo ratings yet
- Synthesis and Biological Evaluation of 2,4,5-Triphenyl-1h-Imidazole-1-Yl DerivativesDocument7 pagesSynthesis and Biological Evaluation of 2,4,5-Triphenyl-1h-Imidazole-1-Yl DerivativesDannyNo ratings yet
- Data 1Document7 pagesData 1Citra MalasariNo ratings yet
- Research Article: Formula Optimization of Orally Disintegrating Tablet Containing Meloxicam NanoparticlesDocument12 pagesResearch Article: Formula Optimization of Orally Disintegrating Tablet Containing Meloxicam NanoparticlesLilia AndromedaNo ratings yet
- MMR 15 03 1109Document8 pagesMMR 15 03 1109SoniaNo ratings yet
- Hospital Pharmacy Volume 50 Issue 4 2015 (Doi 10.1310/hpj5004-296) Tomasello, Cristina Leggieri, Anna Cavalli, RobeDocument9 pagesHospital Pharmacy Volume 50 Issue 4 2015 (Doi 10.1310/hpj5004-296) Tomasello, Cristina Leggieri, Anna Cavalli, RobeArya FajarNo ratings yet
- Optimization and Formulation of Orodispersible Tablets ofDocument7 pagesOptimization and Formulation of Orodispersible Tablets ofUmar AliNo ratings yet
- Metoclopramida DegradacionDocument9 pagesMetoclopramida DegradacionYazminNo ratings yet
- Preformulation Studies Intended For Targeted Lamotrigine Polymeric NanosuspensionDocument8 pagesPreformulation Studies Intended For Targeted Lamotrigine Polymeric NanosuspensionVio MNo ratings yet
- Formulation And Evaluation Of Sustained Release Sodium Alginate Microbeads Of CarvedilolDocument8 pagesFormulation And Evaluation Of Sustained Release Sodium Alginate Microbeads Of CarvedilolDelfina HuangNo ratings yet
- Gel FormulationDocument11 pagesGel FormulationKhuncoro AdiNo ratings yet
- Alogliptin PDFDocument8 pagesAlogliptin PDFAn-nisaNo ratings yet
- Acetazolamide PPT@Document39 pagesAcetazolamide PPT@SREEDHAR ATTLANo ratings yet
- Paper 2Document8 pagesPaper 2jodiNo ratings yet
- Rabinovich Guilatt2004Document13 pagesRabinovich Guilatt2004Megaa ShasiaNo ratings yet
- 5.development of Meloxicam Sodium Transdermal GelDocument7 pages5.development of Meloxicam Sodium Transdermal GelDenny Hendra SNo ratings yet
- Formulation and Evaluation of Nanoemulsion For Solubility Enhancement of KetoconazoleDocument14 pagesFormulation and Evaluation of Nanoemulsion For Solubility Enhancement of KetoconazoledgdNo ratings yet
- Pharmaceutics: Basic Principles and FormulationsFrom EverandPharmaceutics: Basic Principles and FormulationsRating: 3.5 out of 5 stars3.5/5 (6)
- Job Satisfaction, Organizational Commitment and Job Involvement: The Mediating Role of Job InvolvementDocument12 pagesJob Satisfaction, Organizational Commitment and Job Involvement: The Mediating Role of Job InvolvementmehakNo ratings yet
- BoswellOlson BuchananLePine2004JVBStressDocument18 pagesBoswellOlson BuchananLePine2004JVBStressmehakNo ratings yet
- The Corporate Governance of Environmental Sustainability: A Review and Proposal For More Integrated ResearchDocument30 pagesThe Corporate Governance of Environmental Sustainability: A Review and Proposal For More Integrated ResearchmehakNo ratings yet
- The Relationship Between Challenge and Hindrance Stressors and Emotional Exhaustion: The Moderating Role of Perceived Servant LeadershipDocument15 pagesThe Relationship Between Challenge and Hindrance Stressors and Emotional Exhaustion: The Moderating Role of Perceived Servant LeadershipmehakNo ratings yet
- Hobfoll Et Al., 2018 PDFDocument28 pagesHobfoll Et Al., 2018 PDFQundeel HaiderNo ratings yet
- Corporate Governance Integration With Sustainability: A Systematic Literature ReviewDocument15 pagesCorporate Governance Integration With Sustainability: A Systematic Literature ReviewmehakNo ratings yet
- A Review of The Challenge-Hindrance Stress Model: Recent Advances, Expanded Paradigms, and Recommendations For Future ResearchDocument12 pagesA Review of The Challenge-Hindrance Stress Model: Recent Advances, Expanded Paradigms, and Recommendations For Future ResearchmehakNo ratings yet
- Ijbel22 204Document9 pagesIjbel22 204mehakNo ratings yet
- A Review Corporate Governance and SustainabilityDocument11 pagesA Review Corporate Governance and SustainabilitymehakNo ratings yet
- Corporate Governance Integration With Sustainability: A Systematic Literature ReviewDocument15 pagesCorporate Governance Integration With Sustainability: A Systematic Literature ReviewmehakNo ratings yet
- The Corporate Governance of Environmental Sustainability: A Review and Proposal For More Integrated ResearchDocument30 pagesThe Corporate Governance of Environmental Sustainability: A Review and Proposal For More Integrated ResearchmehakNo ratings yet
- Ijbel22 204Document9 pagesIjbel22 204mehakNo ratings yet
- Impact of Corporate Governance On Corporate Sustainable GrowthDocument18 pagesImpact of Corporate Governance On Corporate Sustainable GrowthmehakNo ratings yet
- Journal of Cleaner Production: Marco Formentini, Paolo TaticchiDocument14 pagesJournal of Cleaner Production: Marco Formentini, Paolo TaticchiJuan AlmeydaNo ratings yet
- Corporate Governance Integration With Sustainability: A Systematic Literature ReviewDocument15 pagesCorporate Governance Integration With Sustainability: A Systematic Literature ReviewmehakNo ratings yet
- Journal of Cleaner Production: Marco Formentini, Paolo TaticchiDocument14 pagesJournal of Cleaner Production: Marco Formentini, Paolo TaticchiJuan AlmeydaNo ratings yet
- A Review Corporate Governance and SustainabilityDocument11 pagesA Review Corporate Governance and SustainabilitymehakNo ratings yet
- Ijbel22 204Document9 pagesIjbel22 204mehakNo ratings yet
- The Corporate Governance of Environmental Sustainability: A Review and Proposal For More Integrated ResearchDocument30 pagesThe Corporate Governance of Environmental Sustainability: A Review and Proposal For More Integrated ResearchmehakNo ratings yet
- Impact of Corporate Governance On Corporate Sustainable GrowthDocument18 pagesImpact of Corporate Governance On Corporate Sustainable GrowthmehakNo ratings yet
- Journal of Cleaner Production: Marco Formentini, Paolo TaticchiDocument14 pagesJournal of Cleaner Production: Marco Formentini, Paolo TaticchiJuan AlmeydaNo ratings yet
- Impact of Corporate Governance On Corporate Sustainable GrowthDocument18 pagesImpact of Corporate Governance On Corporate Sustainable GrowthmehakNo ratings yet
- Relationship Between Corporate Governance, Corporate Sustainability and Financial PerformanceDocument21 pagesRelationship Between Corporate Governance, Corporate Sustainability and Financial PerformancemehakNo ratings yet
- Michel On 2010Document33 pagesMichel On 2010Tawsif HasanNo ratings yet
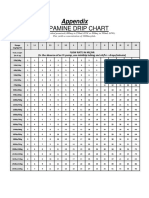
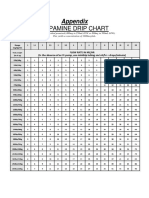
- Dopamine Drip Chart AppendixDocument1 pageDopamine Drip Chart AppendixmehakNo ratings yet
- Governance and SustainabilityDocument17 pagesGovernance and SustainabilitymehakNo ratings yet
- A Review Corporate Governance and SustainabilityDocument11 pagesA Review Corporate Governance and SustainabilitymehakNo ratings yet
- Dopamine Drip ChartDocument1 pageDopamine Drip ChartmehakNo ratings yet
- Guias Del Uso de Albumina e IgGDocument19 pagesGuias Del Uso de Albumina e IgGRonny Muñoz AcuñaNo ratings yet
- Current Management of Hepatocellular Carcinoma: Ana Maria Crissien, MD, and Catherine Frenette, MDDocument9 pagesCurrent Management of Hepatocellular Carcinoma: Ana Maria Crissien, MD, and Catherine Frenette, MDmehakNo ratings yet
- Analisa Pengaruh Diameter Impeller Terhadap Kapasitas Dan Penurunan Tekanan Blower SentrifugalDocument10 pagesAnalisa Pengaruh Diameter Impeller Terhadap Kapasitas Dan Penurunan Tekanan Blower SentrifugalMuwafiqah MarwaNo ratings yet
- 29006.eng - Cpi.std - Painting Systems SheetsDocument37 pages29006.eng - Cpi.std - Painting Systems SheetsMatteoNo ratings yet
- Series and Patterns Test QuestionsDocument96 pagesSeries and Patterns Test Questionssaroj2058No ratings yet
- Chapt 4Document33 pagesChapt 4Ahmed AL-HarthiNo ratings yet
- 02 May 2019 160030223F9D5GNRMPFRDocument46 pages02 May 2019 160030223F9D5GNRMPFRSwami PrabhuNo ratings yet
- Tugas Mandiri 2 FlotasiDocument7 pagesTugas Mandiri 2 FlotasiM Rallupy MeyraldoNo ratings yet
- Completions InfoDocument3 pagesCompletions InfoHamza MalikNo ratings yet
- Additivity of Heats of Reaction: Hess's LawDocument5 pagesAdditivity of Heats of Reaction: Hess's Lawnipuna920% (1)
- Heidolph Rotary Evaporators CatalogDocument15 pagesHeidolph Rotary Evaporators CatalogMuhammad AminNo ratings yet
- Study On The Semiconducting PropertiesDocument155 pagesStudy On The Semiconducting Propertiespadidela swarochishraoNo ratings yet
- NRT-05A TYM (P1&2) 18-02-2024 SolDocument17 pagesNRT-05A TYM (P1&2) 18-02-2024 Solvavc720No ratings yet
- Technical Data Sheet: Desothane HS CA8200 Military and Defense TopcoatsDocument8 pagesTechnical Data Sheet: Desothane HS CA8200 Military and Defense TopcoatsBianca MoraisNo ratings yet
- Ethylene Glycol PLantDocument15 pagesEthylene Glycol PLantBangeen JalalNo ratings yet
- National Standard of The People's Republic of China PDFDocument16 pagesNational Standard of The People's Republic of China PDFJCuchapin100% (1)
- Userdata Paziras Chem101 Review 09ANSDocument4 pagesUserdata Paziras Chem101 Review 09ANSMark CarpesoNo ratings yet
- Assignment-1: Physical Chemistry: Na (Sodium Sir)Document2 pagesAssignment-1: Physical Chemistry: Na (Sodium Sir)Aaryan KeshanNo ratings yet
- UACE Chemistry 2019 Paper 1Document16 pagesUACE Chemistry 2019 Paper 1UV Vïpêr UnïcôrnNo ratings yet
- PTFE Cartridges LPF SereisDocument1 pagePTFE Cartridges LPF SereisPavan AvulaNo ratings yet
- AntibiotikDocument10 pagesAntibiotikmayaNo ratings yet
- Atom Pusat - Merged PDFDocument95 pagesAtom Pusat - Merged PDFCHERLLIN EVANIANo ratings yet
- Question Bank Nitric Acid and NitratesDocument19 pagesQuestion Bank Nitric Acid and NitratesGanesh sargarNo ratings yet
- Periodic Trends GizmoDocument9 pagesPeriodic Trends GizmoGabe Itch67% (61)
- Module 8 RationaleDocument3 pagesModule 8 RationaleG INo ratings yet
- 5 Activity Sheet in GC1 Week2 Melc 19Document11 pages5 Activity Sheet in GC1 Week2 Melc 19Jhun Lerry TayanNo ratings yet
- Providing and Laying High Strength Flexible Bonded Geogrids As Basal ReinforcementDocument4 pagesProviding and Laying High Strength Flexible Bonded Geogrids As Basal Reinforcementabhi0912No ratings yet
- DIY Camping Fuel and Fire StartersDocument2 pagesDIY Camping Fuel and Fire StartersjustaloserNo ratings yet
- Sept 2023 Product List TMPDocument27 pagesSept 2023 Product List TMPedward yohanesNo ratings yet
- 2020 05 10 Foreva Composite TFC350 ACI EN V1Document2 pages2020 05 10 Foreva Composite TFC350 ACI EN V1pabloNo ratings yet
- SP Sendo KF 122Document5 pagesSP Sendo KF 122nurhadri azmiNo ratings yet
- Eliza Budarz - B6.1 Why Are Metals Useful.Document11 pagesEliza Budarz - B6.1 Why Are Metals Useful.Eliza BudarzNo ratings yet