Professional Documents
Culture Documents
1.13 Hyper-CVAD-MA Version 2.1
Uploaded by
Alina CrissCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1.13 Hyper-CVAD-MA Version 2.1
Uploaded by
Alina CrissCopyright:
Available Formats
1.
Acute Myeloid Leukaemia
1.13 Hyper-CVAD/MA
Indication
• Mantle-cell lymphoma (diffuse, nodular or blastic variants).
• Hyper-CVAD/MA has also been used in adult B-cell Acute
Lymphoblastic Leukaemia.
• Relapsed lymphomas
• Burkitt’s Lymphoma
Pre-treatment Evaluation
• Document histological sub-type of lymphoproliferative
disorder according to WHO Classification.
• Document disease stage clinically, including presence or
absence of B symptoms. Investigations should include CT
scan of chest, abdomen and pelvis, bone marrow aspirate
& trephine biopsy.
• Document FBC (with film), U&E, creatinine, LFTs, calcium,
glucose, LDH, immunoglobulin levels, β2-microglobulin and
a direct antiglobulin test.
• CSF cytology must be obtained for patients with aggressive
NHL involving peripheral blood, testis, orbit, paranasal
sinus or paraspinal area. If indicated, give CNS-prophylaxis
according to local protocols.
• Document WHO performance status of patient.
• Document height, weight and body surface area.
• Consider ECG ± echocardiogram if clinical suspicion of
cardiac dysfunction.
• Give adequate verbal and written information for patients
and relatives concerning patient’s disease, treatment
strategy and side effects.
• Obtain written consent from patient or guardian.
• If appropriate, discuss the possibility of pregnancy with
female patients of child-bearing age and the need for
contraception with both male and female patients.
• If appropriate, discuss potential risk of infertility with patient
and relatives.
• Consider intravenous hydration in patients with bulk
disease and tumour lysis precautions according to local
practice.
• Insert a tunnelled central venous access line.
1.13 Hyper-CVAD-MA Version 2.1.docPage 1 of 5
Drug Regimen
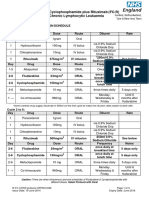
Course 1: Hyper-CVAD (Cycles 1, 3, 5, & 7)
Days Drug Dose Route Comments
1-3 *Cyclophosphamide 300mg/m² IV over 2hrs, 12hrly *Mesna see
total of 6 doses. below
4 Doxorubicin 50mg/m² IV continuously over
48hrs
4 & 11 Vincristine 1.4mg/m² IV bolus Maximum 2mg
1-4 Dexamethasone 40mg Oral, daily
11-14
Course 2: MTX/ARA-C (Cycles 2, 4, 6, & 8)
Days Drug Dose Route Comments
1 Methotrexate 1g/m² IV for 24hrs 200mg/m² for 2hrs then
continuously 800mg/m² for 22hrs
See hydration and folinic
acid rescue below
2-3 Cytarabine 3g/m² IV over 2hrs, 12hrly Total of 4 doses
1-7 Prednisolone 1 drop Eyedrops Both eyes, 4-6 hourly
0.5%
Cycle Frequency and Treatment Duration
Every 21 days for up to up to 8 cycles (4 cycles if stem cell transplant is considered)
HVAD: cycles 1, 3, 5, 7
MTX-ARAC: Cycles 2, 4, 6, 8
Dose Modifications
• Age ≥ 60 years: reduce Cytarabine to 1g/m2
• Pleural effusion/ascites reduce Methotrexate by 50%
• Mucositis (grade 3/4): reduce Methotrexate by 25%
• Hepatic dysfunction:
Serum Bilirubin (µmol/l) Modification
34-50 Reduce Vincristine to 1mg
Reduce Doxorubicin by 25%
51-68 Reduce Doxorubicin by 50%
>68 µmol/l Reduce Doxorubicin by 75%
1.13 Hyper-CVAD-MA Version 2.1.docPage 2 of 5
• Renal dysfunction:
Serum Creatinine (µ
µmol/l) Modification
177 - 265 Reduce Cytarabine by 1g/m²
Reduce Methotrexate by 50%
> 265 µmol/l Reduce Methotrexate by 75%
• Delay of marrow recovery:
Platelets x Or Neutrophils x Dose Given
109/l 109/l
<100 <1.0 After 21 days Postpone next cycle by 7 days
<100 <1.0 After 28 days Reduce Cyclophosphamide by
20%
Reduce Doxorubicin by 20%
Reduce Methotrexate by 25%
Reduce ARA-C by 33%
Investigations prior to subsequent cycles
• FBC, U&E, Creatinine, Liver function tests, LDH and glucose (if
indicated).
• CT after 2 cycles of chemotherapy and at end of therapy
Bone marrow examination at the end of therapy if involved at
diagnosis; during treatment if clinically indicated.
Concurrent Medication
Both cycles:
• Allopurinol 300mg od PO (100mg if creatinine clearance <20mls/min)
for first 2 cycles.
• G-CSF 5 ug/kg daily s/c from day 4 (cycle 1) or day 5 (cycle 2) until
neutrophils reach >1.0 x 109/l.
• PCP prophylaxis is recommended until one month after completion of
the regime (stop one day prior to Methotrexate until neutrophil recovery
to >1.0 x 109/l) - refer to local protocol.
• Systemic oral antifungal prophylaxis is recommended - refer to local
protocol.
• Consider Acyclovir antiviral prophylaxis if previous history of VZV or
HSV reactivation.
1.13 Hyper-CVAD-MA Version 2.1.docPage 3 of 5
Hyper-CVAD Cycles 1, 3, 5, & 7:
Mesna 600mg/m2/day via continuous infusion beginning one hour before first
dose of Cyclophosphamide until 12 hours after the final dose.
MTX/ARA-C Cycles 2, 4, 6, & 8 :
• Dextrose 5%/Sodium Chloride 0.45% + 50mmols Sodium Bicarbonate and
20mmols KCl (per 1 litre of fluid). Start 6 hours before Methotrexate and until
Methotrexate excretion to <0.1µmol/l.
Infuse at 100mls/h and maintain fluid balance with diuretics. Give additional
doses of Sodium Bicarbonate orally to maintain urinary pH at >7.0. Use oral
Acetazolamide (250mg qds PO) to promote excretion if urinary pH drops
<7.0.
• Folinic Acid 50mg IV 12 hours after completion of Methotrexate, then 15mg 6
hourly for 8 doses or until Methotrexate level is <0.1µmol/l.
• Stop Co-Trimoxazole PCP prophylaxis at least one day prior to Methotrexate
and re-start once neutrophils have recovered to >1.0 x 109/l.
Investigations during therapy
• FBC, LDH, U&Es, Creatinine, Liver function tests
• Methotrexate levels at 24h after the completion of Methotrexate infusion and
daily until level <0.1µmol/l.
Anti-emetics
This regimen is highly emetogenic – follow local protocol
References
• Khouri IF et al. Hyper-CVAD and high-dose Methotrexate/Cytarabine followed
by stem cell transplantation: an active regimen for aggressive Mantle-Cell
Lymphoma. J Clin Oncol,1998,16:3803-3809.
• Romaguera JE et al. Untreated aggressive Mantle Cell Lymphoma: results
with intensive chemotherapy without stem cell transplantation in elderly
patients. Leukaemia and Lymphoma,2000,39(1-2):77-85.
• Kantarjian HM et al. Results of treatment with Hyper-CVAD, a dose intensive
regimen, in adult Acute Lymphocytic Leukemia. J Clin Oncol,2000,18:547-
561.
• Thomas DA et al. Hyper-CVAD program in Burkitt’s-type adult Acute
Lymphoblastic Leukemia. J Clin Oncol,1999,17:2461-2470.
1.13 Hyper-CVAD-MA Version 2.1.docPage 4 of 5
Patient Information
http://www.cancerbackup.org.uk/Treatments/Chemotherapy/Combinationregi
men/Hyper-CVAD
Written by: Dr G Hughes, Dr E Kanfer, Dr D Macdonald, Dr M Sekhar and M Schenck.
Revised by: Dr Ed Kanfer, Dr G Hughes, Pauline McCalla
Authorised by: WLCN Haematology TWG
Date for review by Haematology TWG:
1.13 Hyper-CVAD-MA Version 2.1.docPage 5 of 5
You might also like
- L 51 R Hypercvad R MaDocument7 pagesL 51 R Hypercvad R MaMohamed MahmoudNo ratings yet
- Hyper Cvad NHLhiDocument6 pagesHyper Cvad NHLhisevag002816No ratings yet
- BCCA CHOP Protocol for Lymphoma TreatmentDocument3 pagesBCCA CHOP Protocol for Lymphoma TreatmentNararto PrijogoNo ratings yet
- Chemotherapy protocols for trophoblastic neoplasiaDocument3 pagesChemotherapy protocols for trophoblastic neoplasiaImam Hakim SuryonoNo ratings yet
- Ema-Co Gy GTDDocument4 pagesEma-Co Gy GTDTowhidulIslamNo ratings yet
- Anti Cancer DrugsDocument29 pagesAnti Cancer DrugsFrances RamosNo ratings yet
- R ChopDocument6 pagesR Chopจีทีเอส สุรเชษฐNo ratings yet
- Chemotherapy Protocol: RegimenDocument6 pagesChemotherapy Protocol: RegimenAlexandra AndronescuNo ratings yet
- Drug Dosing in CRRT FinalDocument42 pagesDrug Dosing in CRRT FinalVrushali MahajanNo ratings yet
- Apixaban Eliquis MonographDocument14 pagesApixaban Eliquis MonographTran Minh NgocNo ratings yet
- LYCHOP_Protocol (2)Document4 pagesLYCHOP_Protocol (2)Lola WooNo ratings yet
- 311 Topotecan Monotherapy 5 DayDocument4 pages311 Topotecan Monotherapy 5 DayRuxandra BănicăNo ratings yet
- Hyper CvadDocument5 pagesHyper CvadAmr MuhammedNo ratings yet
- Beacopp Hem HL ADocument8 pagesBeacopp Hem HL AAnonymous 9dVZCnTXSNo ratings yet
- ChemotherapyDocument39 pagesChemotherapyAnju Radhika100% (3)
- CetuximabDocument8 pagesCetuximabcrespo2816100% (1)
- VIDE v3Document3 pagesVIDE v3gonococo29No ratings yet
- (R) Choep: IndicationDocument5 pages(R) Choep: IndicationAlina CrissNo ratings yet
- Class Indications: GentamicinDocument3 pagesClass Indications: GentamicinBer Anne Jaropojop TahilNo ratings yet
- Breast Cancer FinaleDocument30 pagesBreast Cancer Finaleخايزورا راهيمNo ratings yet
- Nursing ResponsibilitiesDocument4 pagesNursing ResponsibilitiesMaureen Joy Cascayan EspirituNo ratings yet
- Aminogycoside AntibioticsDocument31 pagesAminogycoside AntibioticsNurul Febrina100% (2)
- ABVDDocument3 pagesABVDEsther WanguiNo ratings yet
- Guideline: Antibiotic Drug Monitoring: Aminoglycosides and GlycopeptidesDocument8 pagesGuideline: Antibiotic Drug Monitoring: Aminoglycosides and GlycopeptidesKenRodulfReyesVillaruelNo ratings yet
- SMILE (Etoposide, Ifosfamide, Methotrexate and Dexamethasone)Document7 pagesSMILE (Etoposide, Ifosfamide, Methotrexate and Dexamethasone)SolikinNo ratings yet
- Vancomycin Protocol RQHRDocument15 pagesVancomycin Protocol RQHRl1o2stNo ratings yet
- King Saud University College of Pharmacy Department of Clinical Pharmacy Clinical Pharmacokinetics - PHCL 462Document26 pagesKing Saud University College of Pharmacy Department of Clinical Pharmacy Clinical Pharmacokinetics - PHCL 462Altaf AhmedNo ratings yet
- Aida Protocol For Apl: InductionDocument4 pagesAida Protocol For Apl: InductionGabrielNo ratings yet
- Acute Lymphoblastic Leukemia Prof.S.Tito'S Unit M5 Dr.M.ArivumaniDocument47 pagesAcute Lymphoblastic Leukemia Prof.S.Tito'S Unit M5 Dr.M.ArivumaniaymenNo ratings yet
- Inflammatory Colitis - A RecapDocument34 pagesInflammatory Colitis - A RecapanahitaasharmaNo ratings yet
- DUBDocument44 pagesDUBStangPongritNo ratings yet
- R-CHOP regimen for diffuse large B cell lymphomaDocument3 pagesR-CHOP regimen for diffuse large B cell lymphomasatishNo ratings yet
- BCCA Protocol for DOXOrubicin - Ifosfamide - Mesna ChemoDocument4 pagesBCCA Protocol for DOXOrubicin - Ifosfamide - Mesna ChemoHep PutNo ratings yet
- BevacizumabDocument4 pagesBevacizumabMartínez Roldán Johana Yadira 3EZNo ratings yet
- Final Anti TB in SP - SituationDocument50 pagesFinal Anti TB in SP - SituationAbdul JalilNo ratings yet
- Antibiotik For Renal FailureDocument6 pagesAntibiotik For Renal FailureWidhy Joss BangetzNo ratings yet
- Doxorubicin: Mechanism of ActionDocument3 pagesDoxorubicin: Mechanism of ActionGeorge FogNo ratings yet
- Capecitabine 14 DayDocument6 pagesCapecitabine 14 DaybrystyyNo ratings yet
- Princy N. Kumar, MDDocument8 pagesPrincy N. Kumar, MDfeedodeedoNo ratings yet
- Pharmacokinetic Training Packet For PharmacistsDocument24 pagesPharmacokinetic Training Packet For PharmacistsGlory Claudia KarundengNo ratings yet
- Management of Tuberculosis in Special Situations: Prof. Dr. Zafar Hussain IqbalDocument27 pagesManagement of Tuberculosis in Special Situations: Prof. Dr. Zafar Hussain IqbalFahadKamalNo ratings yet
- Oncology Study GuideDocument26 pagesOncology Study Guidey7k2b5s7fyNo ratings yet
- ASWCS10 HN001 Weekly Cisp and Radtx Final 110325 - AmendedJuly2012Document3 pagesASWCS10 HN001 Weekly Cisp and Radtx Final 110325 - AmendedJuly2012Kurnia AnharNo ratings yet
- Revision 1Document21 pagesRevision 1NaifmxNo ratings yet
- Pediatric Hematology Oncology Ward Officer HandbookDocument40 pagesPediatric Hematology Oncology Ward Officer HandbookAnonymous FSUnLYr4yNo ratings yet
- Diagnosis & Disease Information Center - Cancer Therapy AdvisorDocument16 pagesDiagnosis & Disease Information Center - Cancer Therapy AdvisorIrfan FathurrahmanNo ratings yet
- Paper Taceedo Vs TaxotereDocument17 pagesPaper Taceedo Vs TaxotereAnonymous R8fT2CNo ratings yet
- De GramontDocument6 pagesDe Gramontsmansa123No ratings yet
- Ovarian Cancer Treatment Regimens - Print Article - Cancer Therapy AdvisorDocument5 pagesOvarian Cancer Treatment Regimens - Print Article - Cancer Therapy AdvisorAnonymous g1hIPZNo ratings yet
- Daepoch Protocolo BccancerDocument9 pagesDaepoch Protocolo BccancerLuiz MeloNo ratings yet
- L 44 Bendamustine 70 R CLLDocument7 pagesL 44 Bendamustine 70 R CLLsatishNo ratings yet
- General Principles of Antibiotic TherapyDocument44 pagesGeneral Principles of Antibiotic TherapyFadhly SharimanNo ratings yet
- R-Bendamustine Regimen for Low Grade LymphomasDocument2 pagesR-Bendamustine Regimen for Low Grade LymphomasagusjatNo ratings yet
- Role of Growth Factors in HematopoiesisDocument54 pagesRole of Growth Factors in Hematopoiesismuhammad hayunNo ratings yet
- Lenvatinib/Pembrolizumab vs Lenvatinib/Placebo in First Line HCC: Adverse Events ManagementDocument39 pagesLenvatinib/Pembrolizumab vs Lenvatinib/Placebo in First Line HCC: Adverse Events ManagementFERNANDO BUSTAMANTE MORALESNo ratings yet
- Ulkamlaven ProtocolDocument10 pagesUlkamlaven ProtocolLeutrim S. SalltekuNo ratings yet
- Pediatric Hematology Oncology Ward Officer HandbookDocument40 pagesPediatric Hematology Oncology Ward Officer HandbookLetchumana KrishnanNo ratings yet
- Brajac - ProtocolDocument13 pagesBrajac - Protocolthanh ngôNo ratings yet
- Urolithiasis PDFDocument464 pagesUrolithiasis PDFAlina Criss100% (2)
- Antibiotic Guidelines (2020) - 0Document55 pagesAntibiotic Guidelines (2020) - 0yudhit bessieNo ratings yet
- AFib Guidelines 2014 2019 Comparison ToolDocument2 pagesAFib Guidelines 2014 2019 Comparison ToolAlina CrissNo ratings yet
- 06-Actualizarea Ghidului National de Boala Venoasa Cronica Ro 258Document9 pages06-Actualizarea Ghidului National de Boala Venoasa Cronica Ro 258Georgiana CiobanuNo ratings yet
- Multiple Files Are Bound Together in This PDF Package.: Click Here To Download The Latest Version of Adobe ReaderDocument1 pageMultiple Files Are Bound Together in This PDF Package.: Click Here To Download The Latest Version of Adobe ReaderAlina CrissNo ratings yet
- Vademecum 2015 PDFDocument24 pagesVademecum 2015 PDFAlina CrissNo ratings yet
- R FC NECN Protocol CRP09 H039Document5 pagesR FC NECN Protocol CRP09 H039Alina CrissNo ratings yet
- R FC NECN Protocol CRP09 H039Document5 pagesR FC NECN Protocol CRP09 H039Alina CrissNo ratings yet
- Amyloid and Related Disorders PDFDocument419 pagesAmyloid and Related Disorders PDFAlina CrissNo ratings yet
- WaldenstromDocument2 pagesWaldenstromAlina CrissNo ratings yet
- He Choep RDocument2 pagesHe Choep RAlina CrissNo ratings yet
- Choep Hem Nhlinthi ADocument4 pagesChoep Hem Nhlinthi AAlina CrissNo ratings yet
- Neurobiology of DepressionDocument7 pagesNeurobiology of DepressionAlina CrissNo ratings yet
- CLL Fludara-Cyclo-Ritux Oral Protocol v4Document4 pagesCLL Fludara-Cyclo-Ritux Oral Protocol v4Alina CrissNo ratings yet
- The Agony and The Ecstasy (Agonie Si Extaz - Viata Lui Michelangelo Buonarroti) - Irving StoneDocument813 pagesThe Agony and The Ecstasy (Agonie Si Extaz - Viata Lui Michelangelo Buonarroti) - Irving Stonemonique801067% (6)
- (R) Choep: IndicationDocument5 pages(R) Choep: IndicationAlina CrissNo ratings yet
- Approach To The Diagnosis and Therapy of Lower Extremity Deep Vein ThrombosisDocument20 pagesApproach To The Diagnosis and Therapy of Lower Extremity Deep Vein ThrombosisAlina CrissNo ratings yet
- Venofer PI 82015Document2 pagesVenofer PI 82015Alina CrissNo ratings yet
- The Diagnosis of B-Cell Chronic Lymphocytic Leukemia (B-CLL) Relies On The ImmunophenotypeDocument5 pagesThe Diagnosis of B-Cell Chronic Lymphocytic Leukemia (B-CLL) Relies On The ImmunophenotypeAlina CrissNo ratings yet
- Primary Therapy For Transplant Candidates: Preferred RegimensDocument9 pagesPrimary Therapy For Transplant Candidates: Preferred RegimensAlina CrissNo ratings yet
- Atlas de Dermato-VenerologieDocument451 pagesAtlas de Dermato-VenerologieCorina Sima94% (31)
- Assignment 12Document7 pagesAssignment 12Anonymous mqIqN5zNo ratings yet
- Assignment in English Plus Core 11 Full CircleDocument76 pagesAssignment in English Plus Core 11 Full CircleRitu Maan68% (38)
- Blackmer Pump Parts ListDocument2 pagesBlackmer Pump Parts ListFelipe Ignacio PaillavilNo ratings yet
- Catalogo Tecnico Gb-S v07Document29 pagesCatalogo Tecnico Gb-S v07farou9 bmzNo ratings yet
- Lab ReportDocument9 pagesLab ReportQi Yi TanNo ratings yet
- Cefiget-Range-Leaflet-PakistanDocument2 pagesCefiget-Range-Leaflet-PakistanZafran KhanNo ratings yet
- Understanding Revit Architecture - BeginnersDocument56 pagesUnderstanding Revit Architecture - BeginnersBudega100% (95)
- Caelus TT - Caelus Product TrainingDocument93 pagesCaelus TT - Caelus Product TrainingYader Daniel Ortiz CerdaNo ratings yet
- 2011 02 Huijben Spie Why Every Urea Plant Needs A Continuous NC Meter PDFDocument9 pages2011 02 Huijben Spie Why Every Urea Plant Needs A Continuous NC Meter PDFfawadintNo ratings yet
- A Study On Renewable Energy Resources in IndiaDocument39 pagesA Study On Renewable Energy Resources in IndiaDevendra SharmaNo ratings yet
- Entry-Exit Arrangement With Service RoadDocument1 pageEntry-Exit Arrangement With Service RoadRamBhuvan SonkarNo ratings yet
- 9th Mole Concept and Problems Based On PDFDocument2 pages9th Mole Concept and Problems Based On PDFMintu KhanNo ratings yet
- ISO 14000 - WikipediaDocument5 pagesISO 14000 - WikipediaalexokorieNo ratings yet
- Friends of Hursley School: Late Summer NewsletterDocument6 pagesFriends of Hursley School: Late Summer Newsletterapi-25947758No ratings yet
- Flange Insulation Sets: Technical SpecificationDocument6 pagesFlange Insulation Sets: Technical SpecificationNor Azlan AwangNo ratings yet
- K2N Final Internship ReportDocument55 pagesK2N Final Internship ReportAceZeta0% (1)
- management of burns readingDocument28 pagesmanagement of burns readinghimanshugupta811997No ratings yet
- Tugas Bahasa Inggris-1Document8 pagesTugas Bahasa Inggris-1Nur KomariyahNo ratings yet
- Roland Berger Hot Trends InconstructionDocument24 pagesRoland Berger Hot Trends InconstructionJavier ContrerasNo ratings yet
- A Feminist Analysis of Habba Khatoon'S Poetry: Dr. Mir Rifat NabiDocument7 pagesA Feminist Analysis of Habba Khatoon'S Poetry: Dr. Mir Rifat NabiShabir AhmadNo ratings yet
- LEEA-036 (B) - Academy ITS Practical Training Courses Jan - June 2020 Version 1 October 2019Document18 pagesLEEA-036 (B) - Academy ITS Practical Training Courses Jan - June 2020 Version 1 October 2019kaito kurabaNo ratings yet
- Marketing 5 0Document23 pagesMarketing 5 0gmusicestudioNo ratings yet
- Effect of Water Immersion On Mechanical Properties of Polyurethane ...Document8 pagesEffect of Water Immersion On Mechanical Properties of Polyurethane ...konshoeNo ratings yet
- Practical 7 - Angiosperms Marking Guide Exercise 1: Class DicotyledonsDocument3 pagesPractical 7 - Angiosperms Marking Guide Exercise 1: Class DicotyledonsDitiro Maletsanake50% (2)
- TheologicalDiscipleship English 2011-1Document144 pagesTheologicalDiscipleship English 2011-1bilnyangnatNo ratings yet
- Aula 4 - Wooten - Organizational FieldsDocument28 pagesAula 4 - Wooten - Organizational FieldsferreiraccarolinaNo ratings yet
- MUSCULAR SYSTEM WORKSHEET Slides 1 To 4Document4 pagesMUSCULAR SYSTEM WORKSHEET Slides 1 To 4kwaiyuen ohnNo ratings yet
- 3 Soal Ganjil Inggris MaritimDocument8 pages3 Soal Ganjil Inggris MaritimFikri Mu'izNo ratings yet
- Oxygen Concentrator SpecificationsDocument3 pagesOxygen Concentrator Specificationsmino pharmNo ratings yet
- Path Loss Models and Wireless Propagation EffectsDocument17 pagesPath Loss Models and Wireless Propagation EffectsAhsan RafiqNo ratings yet