Professional Documents
Culture Documents
Cell Injury, Cell Death and Adaptations
Uploaded by
Sara SultanaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cell Injury, Cell Death and Adaptations
Uploaded by
Sara SultanaCopyright:
Available Formats
reversible injury — necrosis + Mitochondrial damage: ATP depletion —> failure of energy- dependent cellular functions — ultimately, necrosis; under some conditions, leakage of mitochondrial proteins that cause apoptosis + Influx of calcium: activation of enzymes that damage cel- lular components and may also trigger apoptosis * Accumulation of reactive oxygen species: covalent modifica- tion of cellular proteins, lipids, nucleic acids + Increased permeability of cellular membranes: may affect plasma membrane, lysosomal membranes, mitochondrial membranes; typically culminates in necrosis + Accumulation of damaged DNA and misfolded proteins: trig- gers apoptosi CLINICOPATHOLOGIC CORRELATIONS: EXAMPLES OF CELL INJURY ‘AND NECROSI; ISCHEMIC AND HYPOXIC INJURY: + Ischemia—common cause of acute cell injury underlying human disease + Hypoxia—energy generation by anaerobic glycolysis can continue (albeit less efficiently than by oxidative pathways). ischemia. because of reduced blood supply—compromises the delivery of substrates for glycolysis + Anaerobic energy generation also ceases in ischemic tissues after potential substrates are exhausted or when glycolysis is inhibited by the accumulation of metabolites that would normally be removed by blood flow + Thus. ischemia injures tissues faster and more severely than hypoxia, + Major cellular abnormalities in oxygen deprived cells—decreased ATP generation. mitochondrial damage. and accumulation of ROS + Most important biochemical abnormality in hypoxic cells that leads to cell injury—reduced intracellular generation of ATP. as consequence of reduced supply of oxygen + Loss of ATP—failure of many energy dependent cellular systems'nden (2) ion pumps (leading to cell swelling. and influx of a2 . with its deleterious consequences) (2) depletion of glycogen stores and accumulation of lactic acid, thus lowering the intracellular pH’ and (3) reduction in protein synthesis. + Heart muscle ceases to contract within 60 seconds of coronary occlusion + If hypoxia continues, worsening ATP depletion causes further deterioration, with loss of microvilli and the formation of "blebs" + Ifoxygen is restored, all of these disturbances are reversible’ in myocardium— contractility returns + If ischemia persists—irreversible injury and necrosis. + Irreversible injury—severe swelling of mitochondria. extensive damage to plasma membranes and swelling of lysosomes + ROS accumulate in cells, massive influx of calcium. + Death—necrosis, apoptosis + Apoptotic pathway—activated by release of proapoptotic molecules from mitochondria. + Cell’s components—degraded. widespread leakage of cellular enzymes into the extracellular space + Dead cells may become replaced by large masses composed of phospholipids in the form of myelin figures—then either phagocytosed by leukocytes or degraded further into FA's that may become calcified ISCHEMIA-REPERFUSION INJURY: Cells reversibly injured—restoration of blood flow—cell recovery. + Restoration of blood flow to ischemic but viable tissues result in death of cells that are not otherwise irreversibly injured—ischemia reperfusion injury. MECHANISMS ACCOUNTING FOR EXACERBATION OF CELL INJURY RESULTING FROM REPERFUSION INTO ISCHEMIC TISSUES New damage may be initiated during reoxygenation by increased generation of, ROS from parenchymal and endothelial cells and from infiltrating leukocytes + Oxygen increased—increase in production of ROS—because mitochondrial damage leads to incomplete reduction of oxygen and because of the action of oxidases in leukocytes. endothelial cells. or parenchymal cells, + Cellular antioxidant defence mechanisms—compromised by ischemia— accumulation of free radicals + Inflammation induced by ischemic injury—increases with reperfusion because of increased influx of leukocytes—additional tissue injury. + Activation of complement system may also contribute + Complement proteins may bind in the injured tissues. or to antibodies that are deposited in the tissues. and subsequent complement activation generates by products that exacerbate the cell injury and inflammation CHEMICAL (TOXIC) INJURY: ‘Two general mechanisms 1. Some chemicals act directly by combining with a critical molecular component or cellular organelle. + Mercuric chloride poisoning ( from ingestion of contaminated seafood), mercury binds to the sulfhydryl groups of various cell membrane proteins. causing inhibition of ATP-dependent transport and increased membrane permeability. + Many antineoplastic chemotherapeutic agents also induce cell damage by direct cytotoxic effects + Greatest damage is sustained by the cells that use, absorb, excrete. or concentrate the compounds. 2. Many other chemicals are not intrinsically biologically active but must be first converted to reactive toxic metabolites. which then act on target cells + Usually accomplished by cyt P-450 in smooth ER of liver and other organs. + Metabolites might cause membrane damage and cell injury by direct covalent binding to protein and lipids ‘Most important mechanism of cell injury involves the formation of free radicals CCl4- now banned Analgesic acetaminophen belong in this category. Effect of CCl4—example of chemical injury. CCl is converted to the toxic free radical CCIS * . principally in the liver, and this free radical is the cause of cell injury. mainly by membrane phospholipid peroxidation. + Less than 30 mins after exposure to CCl4—breakdown of ER membranes with a decline in hepatic protein synthesis of enzymes and plasma proteins: within 2 hours. swelling of the smooth ER and dissociation of ribosomes from the smooth ER. + Reduced lipid export from the hepatocytes—result of their inability to synthesise apoprotein—form complexes with triglycerides and thereby facilitate lipoprotein secretion—fatty liver of CCl4 poisoning + Mitochondrial injury follows—diminished ATP stores—defective ion transport and progressive cell swelling’ plasma membranes further damaged by fatty aldehydes produced by lipid peroxidation in the ER—calcium influx—cell death, APOPTOSIS: + Pathway of cell death in which cells activate enzymes that degrade the cells’ own nuclear DNA and nuclear and cytoplasmic proteins + Falling off Plasma membrane remains intact ‘Membrane altered—cell altered—cell and its fragment become avid targets for phagocytes Dead cell and its fragments—rapidly cleared before cellular contents have leaked out—apoptotic cell death does not elicit an inflammatory reaction in the host. Necrosis—loss of membrane integrity. enzymatic digestion of cells, leakage of cellular contents. and frequently a host reaction. + Apoptosis and necrosis sometimes coexist—apoptosis may progress to necrosis. CAUSES OF APOPTOSIS: poptosis in physiologic situations: + Programmed destruction of cells during embryogenesis. Normal development—death of some cells and appearance of new cells and tissues— programmed cell death. Involution of hormone dependent tissues upon hormone deprivation— endometrial cell breakdown during the menstrual cycle, and regression of the lactating breast after weaning. + Cell loss in proliferating cell populations—intestinal crypt epithelia + Elimination of cells that have served their useful purpose—neutrophils in an. acute inflammatory response and lymphocytes at the end of an immune response + In these situations—apoptosis because deprived of necessary survival signals, such as growth factors + Elimination of potentially harmful self-reactive lymphocytes. before or after their maturation completes—to prevent reactions against the body's own tissues. + Cell death induced by cytotoxic T lymphocytes. a defence mechanism against viruses and tumors Apoptosis in pathologie condition: DNA damage by Radiation. cytotoxic anticancer drugs. extremes of temperature, and even hypoxia—directly or through production of free radicals + Ifrepair can't cope with injury. cell triggers intrinsic mechanisms that induce apoptosis—elimination of cell” better alternative than risking mutations in damaged DNA.~ progress to malignant transformation—apoptosis if mild insult. but larger doses of same stimuli—necrosis. + Inducing apoptosis of cancer cells—desired effect of chemotherapeutic agents— work by damaging DNA. + Accumulation of misfolded proteins’ because of mutations in the genes encoding these proteins or hecause of extrinsic factors—damage caused by free radicals + Excessive accumulation of these proteins in ER—ER stress—apoptosis. + Cell injury im certain infections less of infected cells—largely due to apoptotic death—induced by the virus (adenovirus and HIV) or by the host immune response (viral hepatitis) + Pathologic atrophy in parenchymal organs after duct obstruction’ in the pancreas, parotid gland. and kidney MORPHOLOGY: * Nuclei of apoptotic cells show various stages of chromatin condensation and aggregation—ultimately karyorrhexis. + Cells rapidly shrink. form cytoplasmic buds, and fragment into apoptotic bodies + Fragments—quickly extruded and phagocytosed without eliciting an inflammatory response, even substantial apoptosis—histologically undetectable MECHANISMS OF APOPTOSIS: * Apoptosis results from activation of enzymes called caspases (cysteine proteases that cleave proteins after aspartic residues) + e activation of caspases depends on a finely tuned balance between production of pro: and anti"apoptotic proteins + Two distinct pathways converge on caspase activation’ the mitochondrial pathway and the death receptor pathway—can intersect ‘The mitochondrial (intrinsic) pathway of apoptos Mitochondria—proteins capable of inducing apoptosis—cytochrome c and other proteins that neutralize endogenous inhibitors of apoptosis. + Choice béw cell survival and death—determined by permeability of mitochondria—controlled by a family of more than 20 proteins. prototype of which is Bel-2 + When cells deprived of GF's and other survival signals. or are exposed to agents that damage DNA. or accumulate unacceptable amounts of misfolded proteins, a number of sensors are activated—members of Bcl'2 family called "BHS proteins" (contain only the third of multiple conserved domains of the Bel'2 family) + In turn activate two pro” apoptotic members of the family—Bax and Bak— dimerize. insert into the mitochondrial proteins escape into the cytosol Cytochrome c. together with some cofactors. activates caspase'9 Net result—activation of the caspase cascade—nuclear fragmentation + Conversely. if cells are exposed to GF's and other survival signals. they synthesise antiapoptotic members of the Bcl-2 family, the two main ones of which are Bel’? itself and BclxL—further tilting the balance toward death Mitochondrial pathway—responsible for apoptosis in most situations, ‘The Death Receptor (Extrinsic) Pathway of Ay + Many cells—surface molecules—death receptors—trigger apoptosis, + Most—members of tumour necrosis factor (TNF) receptor family—contain in their cytoplasmic regions a conserved "death domain" mediates interaction with other proteins involved in cell death. + Prototypic death receptors—type I TNF receptor and Fas (CD95), Fas ligand (FasL) membrane protein expressed mainly on activated T lymphocytes. When these T cells recognize Fas‘expressing targets. Fas molecules are cross linked by FasL and bind adaptor proteins via the death domain—recruit and activate caspase’8.~~ may cleave and activate a pro‘apoptotic member of the Bcl-2 family—Bid—feeding into the mitochondrial pathway. + Combined activation of both pathways delivers a lethal blow to the cell. Death receptor pathway—involved in elimination of self reactive lymphocytes and in killing of target cells by some cytotoxic T lymphocytes Activation and Function of Caspase Mitochondrial and death receptor pathways—activation of the initiator caspases. caspase’9 and -8 Active forms of these enzymes are produced—cleave and thereby activate another series of caspases—executioner caspases. Caspases—degrade components of the nuclear matrix and cytoskeleton— fragmentation of cells. Clearance of apoptotic cell ‘Apoptotic cells entice phagocytes by producing “eatme’ signals + In normal cells phosphatidylserine is present on the inner leaflet of the plasma membrane. but in apoptotic cells this phospholipid ‘flips’ to the outer leaflet— recognized by tissue macrophages ~ phagocytosis of apoptotic cells.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CONSPOSTERDocument1 pageCONSPOSTERSara SultanaNo ratings yet
- Document From Sara SultanaDocument49 pagesDocument From Sara SultanaSara SultanaNo ratings yet
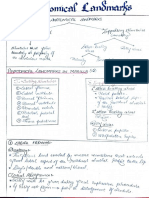
- Anatomical Landmarks - PCPDocument14 pagesAnatomical Landmarks - PCPSara Sultana0% (1)
- CADAVER As Our First TeacherDocument1 pageCADAVER As Our First TeacherSara Sultana80% (5)
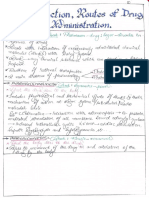
- Introduction, Routes of Drug Administration (Notes)Document24 pagesIntroduction, Routes of Drug Administration (Notes)Sara Sultana100% (1)
- William Shakespeare PoemsDocument471 pagesWilliam Shakespeare PoemsSara SultanaNo ratings yet
- General Anatomy Syllabus PDFDocument3 pagesGeneral Anatomy Syllabus PDFSara SultanaNo ratings yet
- Sl. No. Chapter Name Checked Questions 1 2 3 4Document4 pagesSl. No. Chapter Name Checked Questions 1 2 3 4Sara SultanaNo ratings yet
- Why Do We Fall IllDocument11 pagesWhy Do We Fall IllSara SultanaNo ratings yet