Professional Documents
Culture Documents
Non-Small-Cell Lung Cancers - A Heterogeneous Set of Diseases
Uploaded by
XyzOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Non-Small-Cell Lung Cancers - A Heterogeneous Set of Diseases
Uploaded by
XyzCopyright:
Available Formats
REVIEWS
Non-small-cell lung cancers:
a heterogeneous set of diseases
Zhao Chen1*, Christine M. Fillmore2,3,4*, Peter S. Hammerman1, Carla F. Kim2,3,4 and
Kwok-Kin Wong1,5,6
Abstract | Non-small-cell lung cancers (NSCLCs), the most common lung cancers, are known
to have diverse pathological features. During the past decade, in-depth analyses of lung
cancer genomes and signalling pathways have further defined NSCLCs as a group of distinct
diseases with genetic and cellular heterogeneity. Consequently, an impressive list of
potential therapeutic targets was unveiled, drastically altering the clinical evaluation and
treatment of patients. Many targeted therapies have been developed with compelling
clinical proofs of concept; however, treatment responses are typically short-lived. Further
studies of the tumour microenvironment have uncovered new possible avenues to control
this deadly disease, including immunotherapy.
Lung cancer results in the largest number of cancer- and tumour microenvironment studies might be used
related deaths worldwide1,2. More than 85% of those to improve the survival of patients with NSCLC through
cases are currently classified as non-small-cell lung the development of novel therapeutic strategies.
cancer (NSCLC), for which the predicted 5‑year sur-
vival rate is 15.9% — a figure that has only marginally Defining NSCLC subsets
improved during the past few decades3. Technological NSCLC is currently defined by pathological character
1
Department of Medical
Oncology, Dana-Farber advances during the past decade, including the intro- istics. The two predominant NSCLC histological pheno-
Cancer Institute, Boston, duction of next-generation sequencing (NGS), the types are adenocarcinoma (ADC; ~50%) and squamous
Massachusetts 02115, USA. generation of multiple genetically engineered mouse cell carcinoma (SCC; ~40%)4,5. In general, ADCs arise in
2
Stem Cell Program, Boston models (GEMMs) of lung cancer and the construction more distal airways, whereas SCCs arise in more proxi-
Children’s Hospital, Boston,
Massachusetts 02115, USA.
of large databases characterizing the molecular fea- mal airways and are more strongly associated with smok-
3
Harvard Stem Cell Institute, tures of human tumours, have transformed our view of ing and chronic inflammation than ADCs4,5. ADCs often
Cambridge, Massachusetts NSCLC from histopathological descriptions to precise have glandular histology and express biomarkers that
02138, USA. molecular and genetic identities that can be resolved to are consistent with an origin in the distal lung, includ-
4
Department of Genetics,
the single-cell level. In parallel, approaches and concepts ing thyroid transcription factor 1 (TTF1; also known
Harvard Medical School,
Boston, Massachusetts from fields such as developmental biology, stem cell biol- as NKX2‑1) and keratin 7 (KRT7)4,5. By contrast, SCCs
02115, USA. ogy and immunology have deepened our knowledge of are characterized by squamous differentiation, which is
5
Department of Medicine, tumour development, cellular heterogeneity and inter- more reminiscent of the pseudostratified columnar epi-
Harvard Medical School, actions between the lung tumour and its surrounding thelium that lines the trachea and upper airways4,6. SCCs
Boston, Massachusetts
02115, USA.
microenvironment. These multidisciplinary efforts are distinguished from ADCs in the clinic by immuno
6
Belfer Institute for Applied have enhanced our understanding of molecular disease staining for cytokeratin 5 and cytokeratin 6 and/or
Cancer Science, Dana-Farber mechanisms, thereby forming the rationales for target- the transcription factors SRY-box 2 (SOX2) and p63
Cancer Institute, Boston, ing different cellular compartments simultaneously. (REFS 4,5,7). Other subtypes of NSCLC include large cell
Massachusetts 02115, USA.
Scientists and physicians have better tools than ever to carcinoma, which is diagnosed by exclusion if tumour
*These authors contributed
equally to this work. pursue answers to two provocative questions: first, how cells do not appear glandular or squamous in shape or
Correspondence to P.S.H., can we define the specific subsets of NSCLC that differ express ADC or SCC biomarkers, although it is unclear
C.F.K. and K.-K.W. by cellular and molecular composition? Second, how whether large cell carcinomas are genetically distinct
e‑mails: phammerman@ can we effectively control lung cancer growth for each from ADC or SCC4. Some neuroendocrine tumours
partners.org; carla.kim@
childrens.harvard.edu;
specific subset of NSCLC? In this Review, we discuss are also classified as NSCLC, although the most aggres-
kwong1@partners.org how data that are derived from technological advances sive form of neuroendocrine tumour is classified as
doi:10.1038/nrc3775 in lung cancer genomics, mouse modelling of cancers small-cell lung cancer (SCLC)4.
NATURE REVIEWS | CANCER VOLUME 14 | AUGUST 2014 | 535
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Genetic mutations and genomic heterogeneity. the net effects of genotype and therapy response may be
Although histological features and marker expression achieved and will ultimately inform the most suitable
remain the basis of clinical tumour diagnosis, recent treatment strategies.
advances in NGS and other high-throughput genomic Other novel technologies have also facilitated the
profiling platforms have allowed researchers to exam- discovery and validation of somatic mutations in lung
ine the breadth of genetic mutations within lung cancer. For example, high-throughput screens using
tumours. Following the identification of KRAS and established short hairpin RNA (shRNA) libraries have
BRAF mutations8,9, epidermal growth factor receptor identified genes that cause synthetic lethality with
(EGFR) mutations were discovered in patients with common oncogenic events, such as KRAS-activating
lung ADC and were associated with response to EGFR mutations or p53 inactivation, leading to potential
inhibitors10–13. Further recurrent mutations and ampli- new treatment targets, such as TANK-binding kinase 1
fications in many potentially targetable oncogenes have (TBK1)32. Similarly, the application of mass spectro
since been identified in lung ADC, including HER2 metry to metabolomic, proteomic and phosphoki-
(also known as ERBB2), MET, fibroblast growth fac- nase profiling, as well as single cell time-of-flight mass
tor receptor 1 (FGFR1) and FGFR2, as well as fusion cytometry (cyTOF), have led to numerous new findings,
oncogenes involving anaplastic lymphoma kinase including the discovery of recurrent aberrations such as
(ALK), the ROS1 receptor tyrosine kinase, neuregu- the ROS1 fusions and the potential diagnostic or prog-
lin 1 (NRG1), neurotrophic tyrosine kinase recep- nostic marker isocitrate dehydrogenase 1 (IDH1)17,33,34.
tor type 1 (NTRK1) and RET 14–22. These oncogenic Such advances in high-throughput technology are pro-
changes, many of which predict sensitivity to clini- moting rapid advances in our understanding of NSCLC
cal inhibitors, jointly account for most cases of lung biology and, ultimately, will help to determine how
ADC23–25. For lung SCC, the number of tumours for NSCLC develops, spreads and can be better treated.
which whole-exome sequencing is available is lower
than for ADC but, so far, potentially targetable muta- Heterogeneity in lung tumour microenvironments.
tions in ADC do not seem to be prevalent in this The concept of tumour heterogeneity applies not only
histological subtype20. Instead, genes such as discoi- to tumour epithelial cells but also to the diverse micro-
din domain-containing receptor 2 (DDR2), FGFR1, environments with which the tumour cells interact 35.
FGFR2, FGFR3 and genes in the PI3K pathway seem Carcinoma cells, in the lung and other organs, are closely
to be more commonly mutated in lung SCC20. Many associated with the extracellular matrix (ECM), mesen-
of these mutations (with the exception of those in chymal cells such as fibroblasts, infiltrating immune cells
the PI3K pathway) have been validated by preclinical and vasculature (FIG. 1). In some cases, this environment
studies as driver mutations22,26,27. is essential to tumour initiation or tumour growth,
NGS studies have also revealed the molecular tax- whereas in other cases it can prevent tumorigenesis or
onomy of lung cancer and have shown a dazzling com- even promote tumour clearance35,36.
plexity of somatic alterations in NSCLCs that extends In lung tumorigenesis, genesis of new blood and lym-
far beyond protein kinases to include epigenome phatic vessels supplies necessary nutrients for tumour
modifiers, transcription factors, splicing factors and growth and allows for an influx of immune cells of the
genes involved in cellular immunity 20,28,29. Potentially myeloid and lymphoid lineages. The myeloid cells that
important mutations and copy number gains identified are implicated in this process include tumour-associated
from patient tumours are summarized in TABLE 1, with macrophages (TAMs) and tumour-associated neutro-
relevant preclinical and clinical evidence. Among the phils37. Mice that harboured germline knock‑in of kinase-
21 different tumour types for which exome sequences dead inhibitor of nuclear factor-κB (NF‑κB) kinase
were directly compared, lung SCC and ADC ranked subunit-α (IKKα) developed spontaneous lung SCC
second and third highest in median somatic muta- that is characterized by NF‑κB activation and marked
tion frequency, with an average of ten mutations per accumulation of TAMs that were essential for disease
megabase of coding DNA sequenced30. It is worth progression38. Secretion of pro-angiogenic factors such
noting that ADCs in non-smokers have 5–6‑times as platelet-derived growth factor (PDGF) and vascular
fewer mutations24,31. Given this relatively large num- endothelial growth factor (VEGF) by TAMs in lung can-
ber of mutations per tumour, there will probably be cer suggests why these cells are associated with increased
more important mutations identified for NSCLC as microvessel formation39,40. Likewise, increased neutro-
the number of tumours that are analysed increases. phil numbers have been associated with poor prognosis
An important challenge that remains is understanding in NSCLCs, perhaps owing to their ability to degrade
which of these many mutations are important in lung matrices with elastase41,42. Neutrophils that are found
Myeloid-derived
carcinogenesis and/or treatment response, in contrast in mouse tumours are phenotypically characterized as
suppressor cells
(MDSCs). MDSCs encompass a to those mutations that are merely a consequence of polymorphonuclear CD11B- and lymphocyte antigen
heterogeneous population of the tumorigenic process. Thus, the genomic profiles 6G‑expressing (CD11B+Ly6G+) cells, and are often con-
myeloid cells, which share the highlight the heterogeneity of the NSCLC genome and sidered to be a subtype of myeloid-derived suppressor cells
ability to suppress T cells provide a plausible explanation for the highly hetero- (MDSCs)43. In the tumour microenvironment, accu-
through the production of
arginase and the expression
geneous treatment responses that we have observed in mulated MDSCs are thought to promote tumour pro-
of inducible nitric oxide the clinic. By cataloguing a large collection of muta- gression by increasing matrix degradation, tumour cell
synthase (iNOS). tions for each patient, a more accurate evaluation of proliferation, metastasis and angiogenesis35,37.
536 | AUGUST 2014 | VOLUME 14 www.nature.com/reviews/cancer
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Table 1 | Potential important alterations in ADC and SCC
Gene Status Frequency (%) Available GEMMs Currently Selected potential Refs
(M, C available targeted targeted therapies
or F)* ADC SCC therapies Preclinical Clinical
evidence evidence
Receptor tyrosine kinases
EGFR M or C 10 (M) 2–3 L858R, Del19, T790M and Erlotinib, gefitinib AZD9291, CO‑1686 and 126 11
Ins20 and afatinib HM61713
FGFR1 C N/A 20 N/A N/A Dovitinib, ponatinib, AZD4547 150 22
and BGJ398
FGFR2 M or C 3 (M) 3 N/A N/A Dovitinib, ponatinib, AZD4547 151 20
and BGJ398
ALK F 3–5 <1 ALK fusion, L1196M and Crizotinib and AP26113, alectinib, 125 18
F1174L ceritinib ganetespib and PF‑06463922
MET C 2–4 N/A Overexpression Crizotinib Tivantinib, cabozantinib, 152 14
INC280 and onartuzumab
ROS1 F 1–2 N/A N/A Crizotinib PF‑06463922 153 17
NTRK1 F 1–2 N/A N/A N/A Crizotinib and lestaurtinib 21 21
RET F 1 N/A N/A N/A Carbozantinib and vandetanib 154 16
HER2 M or C 2–4 N/A HER2-YVMA insertion N/A Neratinib, afatinib, lapatinib 155 19
(M) and trastuzumab
DDR2 M N/A 2–3 N/A N/A Dasatinib 27 27
PDGFRA M 6–7 4 N/A N/A Sunitinib 156 28
Signalling
KRAS M 15–25 1–2 G12D, G12C and G12V N/A Selumetinib plus docetaxel 157 158
combination
NF1 M 12 10 Null N/A 159 28
BRAF M 1–6 4–5 V600E N/A Vemurafenib, dabrafenib and N/A 160
trametinib
PIK3CA M 5 15 p110α N/A BEZ235, BKM120 and 99 161
GDC0941
MEK1 M 1 N/A N/A N/A Selumetinib and trametinib N/A 162
NOTCH1 M 8 1 Conditional null N/A N/A 163 164
Epigenetic factors
MLL2 M 9 20 N/A N/A N/A 165 28
EZH2 M 2 2 N/A N/A N/A 166 28
TET2 M 3 2 N/A N/A N/A 167 28
DNMT3A M 4 1 N/A N/A N/A 168 28
Transcription factors
SOX2 C 6 65 Overexpression N/A N/A 7 103
MYC C 25 N/A Overexpression N/A N/A 133 104
Proteolysis
KEAP1 M 17 12 N/A N/A N/A 169 170
Cell cycle
CDKN2A M 7 15 Null N/A N/A 171 172
Ligand
NRG1 F <1 N/A N/A N/A N/A 15 15
Tumour suppressor
TP53 M 52 79 Conditional null and R172H N/A N/A 98 173
LKB1 M 9 2 Conditional null N/A N/A 65 174
PTEN M 2 8 Conditional null N/A BEZ235, BKM120 and 175 176
GDC0941
ADC, adenocarcinoma; ALK, anaplastic lymphoma kinase; CDKN2A, cyclin-dependent kinase inhibitor 2A (which encodes INK4A and ARF); DDR2, discoidin
domain-containing receptor 2; Del19, EGFR exon 19 deletion; DNMT3A, DNA (cytosine‑5-)-methyltransferase 3α; EGFR, epidermal growth factor receptor;
EZH2, enhancer of zeste homologue 2; FGFR1, fibroblast growth factor receptor 1; GEMM, genetically engineered mouse model; Ins20, EGFR exon 20 insertion;
KEAP1, kelch-like ECH-associated protein 1; LKB1, liver kinase B1; MLL2, mixed-lineage leukaemia 2; N/A, not available; NF1, neurofibromin 1; NRG1, neuregulin 1;
NTRK1, neurotrophic tyrosine kinase, receptor, type 1; PDGFRA, platelet-derived growth factor receptor-α; PIK3CA, PI3K catalytic subunit-α; SCC, squamous cell
carcinoma; SOX2, SRY-box 2; TET2, TET methylcytosine dioxygenase 2. *Status refers to mechanisms by which each gene is altered in tumours — mutation (M),
copy number gain (C) or fusion (F).
NATURE REVIEWS | CANCER VOLUME 14 | AUGUST 2014 | 537
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Endothelial PDGF Macrophage Differences in the ability to secrete inflammatory
cell cytokines such as interleukin‑6 (IL‑6) may be one way
VEGF ECM: keratin,
Fibroblast fibronectin in which tumour cells influence their surroundings50,51.
and collagen Tumours that are driven by different oncogenic muta-
Erythrocyte tions in mice, such as EGFR and Kras, have distinguish-
Tumour cell
able immune infiltrates with respect to cell types and
their phenotypes in the tumour immune microenviron-
PDL1 ment 48,49. These mechanisms have not been defined in
detail, and there are other important questions to con-
Neutrophil PD1 sider: does each genetic subset of NSCLC have its own
CD8+
unique microenvironmental influences, or can common
T cell characteristics of how the surroundings drive tumour
CXCR2 CXCL
subsets be uncovered? How does targeted therapy alter
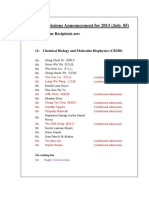
Figure 1 | The lung cancer microenvironment. The tumour microenvironment,
Nature Reviews | Cancer the tumour microenvironment? Do drug-resistant or
including endothelial cells, fibroblasts and myeloid cells, among others, has important recurrent tumours have an environmental milieu that is
roles in determining the characteristics of lung tumours. It is likely that a combination distinct from the initial untreated tumour? A more thor-
of the cell of origin, genetic alterations and microenvironmental factors all contribute to ough understanding of these dynamic interactions will
the lineage identity of lung tumours. Extracellular matrix (ECM), which often consists of help to show new targets that can be manipulated to pro-
keratins in lung squamous cell carcinoma and fibronectin in desmoplastic lung
mote antitumor effects. Importantly, many of these ques-
adenocarcinomas, gives structural support to tumour cells and is associated with
tumour-associated fibroblasts. Blood vessels are newly formed at the tumour site by
tions are challenging to understand, given the need to
recruitment of endothelial cells via platelet-derived growth factor (PDGF) and vascular study the immune system in vivo, and the use of mouse
endothelial growth factor (VEGF), among others. As the blood and lymphatic vessels models with intact immune systems in combination with
form, numerous blood cells, including macrophages, neutrophils, T cells and B cells, patient samples may be instructive.
home to the tumours. In particular, tumours can recruit neutrophils through secretion of
CXC-chemokine ligand (CXCL) family members, which bind to the neutrophil receptor Cell(s) of origin for NSCLC heterogeneity at tumour ini-
CXCR2. In addition, tumour cells often express immune checkpoint molecules, such as tiation. Another contributing factor to the diversity of
programmed cell death 1 ligand 1 (PDL1), to attenuate a cytotoxic response from T cells. NSCLCs may be the potential distinct cells of origin in
PD1, programmed cell death 1. which subsets of NSCLC first arise. The cell of origin for
each subset of NSCLC is essentially unknown beyond
Tumours can evade immune surveillance by initial work in this area in mouse models. For example,
expressing molecules that maintain tolerance to nor- it remains to be understood whether multiple cell types
mal peripheral tissues, including the interaction of the are equally likely to produce KRAS-mutant ADC or if
tumour-associated programmed cell death 1 ligand 1 only one cell type exists in the right microenvironment
(PDL1) with the immune receptor programmed cell and must gain oncogenic KRAS expression to produce
death 1 (PD1; also known as PDCD1). Recently, the this type of ADC. It is possible that the biology of differ-
use of antibodies targeting the PD1–PDL1 checkpoint ent cells of origin is what drives the different phenotypes
has resulted in some marked responses in early-stage of NSCLCs with distinct genotypes. This could be the
clinical trials for a large panel of therapy-refractory can- result of unique gene expression patterns of the originat-
cer subtypes, including advanced melanoma, NSCLC ing cells, differences in the type of cells that the originating
and renal cell cancer, with a proportion of responding cells can produce, or unique microenvironments of the
patients showing persistent long-term benefits44,45. The originating cell type. Ultimately, the clinical importance
PD1–PDL1 interaction inhibits CD8+ cytotoxic T lym- behind these seemingly basic biological questions is
phocyte proliferation, survival and effector function, whether a different cell of origin partly dictates treat-
and can induce apoptosis of tumour-infiltrating T cells; ment responses. Can knowledge of the cell of origin pre-
PD1–PDL1 interactions can also promote the differen- dict environmental influences that can be targeted for
tiation of CD4+ T cells into forkhead box P3‑expressing antitumour therapy? Furthermore, can knowledge of the
(FOXP3+) regulatory T (TReg) cells, which are known to cell of origin be used for the earlier detection of tumours?
further suppress the immune system and cause periph- The answers to these questions have the capacity to
eral immune tolerance in patients with lung cancer 46. revolutionize our current concept of the stratification,
Despite the promising clinical benefits, there is currently diagnosis and treatment of NSCLC.
no defined subset of patients with lung cancer who are A long-standing hypothesis proposes that stem and
particularly sensitive to PD1–PDL1 blockade. This is progenitor cells in adult tissues function as carcinoma
partly due to a lack in the understanding of how tumour cells of origin because they are the only cells that have a
cells affect their microenvironment, including the sur- sufficient lifespan to accumulate the many genetic altera-
rounding immune cells44,45,47. Evaluating the expres- tions required for tumour progression52. Furthermore,
sion of PDL1 on tumour cells is only the starting point stem cells have inherent self-renewal capacity and may
in the analysis of the interactions between tumour cells not need extensive epigenetic reprogramming. However,
and the surrounding microenvironment 48,49. Many even genetically normal cells with limited self-renewal
important questions remain, including whether lung capacity can be induced to acquire more stem cell-like
tumours with distinct genetic backgrounds differ in how properties in response to genetic alterations or micro
they shape their immune microenvironment. environmental changes53,54, and this supports the idea that
538 | AUGUST 2014 | VOLUME 14 www.nature.com/reviews/cancer
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Box 1 | Mouse models
such as AT2 cells and BASCs, AT2 cells seemed to be the
only cells that were capable of giving rise to advanced
Genetically engineered mouse models (GEMMs) have enabled numerous studies of ADC in the alveolar space, whereas club cells and BASCs
non-small-cell lung cancer (NSCLC) that would not be possible using patient samples or seemed to be limited to driving bronchiolar hyperplasia
cancer cell lines: for example, preclinical or co‑clinical trials of targeted therapies, the
within the same time frame59. Using these approaches, it
study of metastatic and transplanted disease and examination of tumour cells of
origin25,49,74,98,125,126. Today, GEMMs for most of the common NSCLC driver mutations
is notable that changes in the cells of origin were evident
have been generated, including for KRAS, epidermal growth factor receptor (EGFR), when the genotype for tumour initiation was altered (for
and echinoderm microtubule-associated protein-like 4 (EML4)–anaplastic lymphoma example, to include p53 loss) or if injury or inflamma-
kinase (ALK); and despite their lack of genetic complexity compared to human cancers, tion were present during tumour initiation (for example,
they have shown some remarkable similarities in pathological features and treatment after adenovirus infection or after naphthalene-induced
responses to the human disease98,125–127. injury)56,59–63. Injury or inflammation probably more
GEMMs are particularly informative when the net effects of several mutations need to closely mimics the scenario of tumour initiation in
be determined in vivo. For example, the conditional oncogenic KrasG12D mouse model humans, in which environmental influences and ongo-
has been used to elucidate the steps from early to late tumorigenesis, owing to the ing injury occur in contrast to the relatively sterile mouse
temporal control it affords128, and it is easy to combine with mice bearing conditional
colony. These questions are unexplored in other models
null alleles for other genes of interest. For example, KrasG12D tumours only reach a full
adenocarcinoma stage with a very long latency, but KrasG12D-expressing and Trp53‑null
of ADC that use distinct oncogenes or in SCC. Thus, it
tumours are more advanced and show a decreased response to certain treatment remains entirely possible that club cells, AT2 cells and
strategies when compared to KrasG12D tumours128,129. Simultaneous inactivation of BASCs are all possible initiators of lung ADC. Future
Pten and liver kinase B1 (Lkb1) in the lung produced only squamous cell carcinoma development of more precise lineage-specific Cre driv-
(SCC)49, and this fits with the preclinical observations that PI3K and mTOR pathways are ers combined with approaches to study tumorigenesis
activated in most human lung SCC tumours20,49,65. Similar genetic breeding schemes can in the context of injury and inflammation (situations
be used to identify and validate potential treatment targets through in vivo synthetic that are more likely to mimic carcinogenesis in humans)
lethal experiments. Elegant studies have recently shown that MYC, cyclin-dependent will be needed to better determine the comparable
kinase 4 (CDK4) and CRAF are crucial KRAS effectors that can lead to synthetic lethality ADC-initiating activity of these populations.
when genetically inactivated in tumours with activated KRAS130–134.
Although increasing amounts of genomic data show
The assessment of immunotherapeutics and the dynamic interactions between
tumour cells and their microenvironment using GEMMs (which are immunocompetent)
that distinct gene expression programmes and driver
is another emerging research direction. Experiments of particular interest include gene mutations distinguish ADC from SCC, it remains unclear
expression and pathway activation profiles for each cell type within the tumour; whether these two tumour types arise from a common
genotype- or treatment-dependent influences on the tumour microenvironment; and cell of origin or diverse cell types, including different lung
effects of individual or combination therapies on tumour cells, immune cells and other stem or progenitor cells (BOX 2). Until recently, a paucity of
cell types within the tumour microenvironment. GEMMs for SCC has precluded analysis of the cells
Patient-derived xenograft (PDX) models provide an alternative and complementary of origin of this important NSCLC subtype. It has long
method to GEMMs to address human–murine differences and allow for expansion of been hypothesized that SCC arises from basal cells, as
patient material to perform assays such as metabolomic and serial transplantation135. lung SCCs most frequently arise in the proximal lung 4,
A ‘humanized’ lung and even a ‘humanized’ immune system in the mouse might offer a
but also because they often express KRT5, SOX2 and
more accurate means to model NSCLC.
p63, which are markers of the normal basal cell popula-
tion5–7,62,64. GEMMs of ADC have been more widespread,
more mature, differentiated cells may be just as likely to mostly owing to the usefulness and availability of the con-
give rise to malignancy. Historically, ADCs have been pro- ditional oncogenic Kras allele (which drives lung ADCs
posed to arise from club cells (previously known as Clara both independently and more rapidly in combination
cells) or alveolar epithelial type 2 (AT2) cells, owing to with Trp53 loss) as well as early models using chemicals
the staining of patient ADCs by immunohistochemistry that induce RAS mutations to drive tumours. Although
with markers of these cell types4,5. However, it is impor- KRAS or NRAS mutations are present in up to 25% of
tant to note that the staining pattern of a tumour is merely ADCs, they are rarely detected in SCCs, and mouse
a snapshot of the gene expression of the tumour cells modelling with these oncogenes seems to result predomi-
at that time point and might not match the initiating nantly in the development of ADC. Mutations that are
cell type. Our current understanding of cells of origin common in samples from patients with SCC have only
for lung cancer is mostly derived from experimental recently been catalogued, and this opens up new ideas
data using GEMMs55 (BOX 1; FIG. 2). Many conditional about how to model SCC20. Kinase-dead IKKα knock‑in
GEMMs target activation and/or loss of genes specifically mice develop spontaneous lung SCC, but because this
to lung cells by intranasal or intratracheal instillation of mouse has a germline Ikka mutation, it is not clear which
adenovirus-Cre, which infects lung epithelial cells along cells in the lung expanded into the squamous tumours38.
the proximal to distal tract. After using intranasal adeno Loss of the tumour suppressor liver kinase B1 (Lkb1; also
virus-Cre to induce oncogenic Kras, loss of Pten or loss known as Stk11) in the oncogenic KrasG12D model pro-
of p38, the first hyperproliferative cells to be observed duces a mixture of tumours, including ADC, SCC and
were bronchioalveolar stem cells (BASCs) — implicat- large cell carcinoma65. Similarly, a mixture of ADC
ing them as possible ADC cells of origin56–58. However, and SCC is found in mice after targeted deletion of Pten
in more recent studies that targeted the expression of or transforming growth factor-β receptor 2 (Tgfbr2)
oncogenic KrasG12D only in cells expressing club cell in proximal cells with keratin-driven Cre alleles in the
secretory protein (CCSP), such as club cells and BASCs, KrasG12D background66. Expression of the transcription
or only in cells expressing surfactant protein C (SPC), factor Sox2 (overexpressed in 20–60% of human SCCs) in
NATURE REVIEWS | CANCER VOLUME 14 | AUGUST 2014 | 539
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Proximal Basement Pseudostratified
membrane columnar epithelium
Cartilage Club cell (CCSP+)
Ciliated cell (AcTUB+)
Goblet cell
Basal cell (KRT5+ and p63+)
Typical SCC Modelled by:
• SOX2+ • KrasG12D expression
• p63+ and Lkb1-null
• KRT5+ • Lkb1-null and Pten-null
• IKKα: kinase dead
Alveolar space AT2 (SPC+)
BASC
(CCSP+ and SPC+)
AT1
Distal
Simple columnar epithelium
Typical ADC Modelled by:
• KrasG12D
Neuroendocrine • TTF1+ • KrasG12D expression
cell (CGRP+) • KRT7+ and Trp53-null
• SPC+ • EGFRT790M/L858R
• Many others
Figure 2 | A diagram of proximal and distal lung cells, indicating markers that are retained in carcinomas and
putative squamous cell carcinoma (SCC) and adenocarcinoma (ADC) cells of origin. DiverseNature Reviews | Cancer
lung stem or progenitor
cell populations are thought to have the ability to drive lung oncogenesis in different contexts. In the proximal lung, the
tracheal basal cell has been proposed to be the cell of origin for lung SCC. The evidence for this relationship includes
the expression of p63, SRY-box 2 (SOX2) and keratin 5 (KRT5) within the basal cells, squamous metaplasia of the basal cells
(common in smokers), and squamous cell carcinomas. Squamous tumours are modelled in mice by KrasG12D expression and
liver kinase B1 (Lkb1) knockout (20% of lesions are squamous), knocking in a germline dominant-negative kinase-dead
inhibitor of nuclear factor-κB kinase subunit-α (IKKα) and knocking out both Lkb1 and Pten (100% of lesions are squamous
for the second two models). Two bronchiolar cell populations, the bronchiolar progenitor cells and the bronchioalveolar
stem cells (BASCs) may also be able to give rise to tumours with squamous characteristics, although experimental lineage
tracing is needed to confirm this theory. ADCs can be modelled by KrasG12D expression (long latency), KrasG12D expression
and Trp53‑null, and epidermal growth factor receptor (EGFR)T790M/L858R, among other genetic models, and they are thought
to arise from more proximal airway cells. These tumours often retain characteristics of proximal airways, such as the
expression of surfactant protein C (SPC), KRT7 and thyroid transcription factor 1 (TTF1). Again, BASCs or bronchiolar
progenitor cells, which are able to give rise to alveolar lineages after lung injury, may likewise be able to give rise to
tumours with alveolar characteristics. AcTUB, acetylated tubulin; AT, alveolar epithelial type; CCSP, club cell secretory
protein; CGRP, calcitonin gene-related peptide.
club cells and BASCs produces lung tumours that express transplantation assays. Establishment of tumours at
the marker p63 but histologically resemble ADCs7. This metastatic sites and tumour recurrence following treat-
intriguing finding suggests that distal lung epithelia are ment have been attributed to growth and survival of
unable to produce a fully squamous phenotype, despite the TPCs67,68. Recent studies have identified potential cell
expression of an SCC transcription factor. In addition, surface markers or genetic traits that may mark the TPC
the deletion of Lkb1 and Pten in the lung via intranasal population in NSCLC, such as aldehyde dehydroge-
adenovirus-Cre was recently shown to give rise to fully nase (ALDH) activity or expression of NOTCH, CD24,
penetrant lung SCCs49. The next important step will be to CD166 or CD44 (REFS 38,69–73). However, these stud-
use lineage-restricted Cre alleles, such as the oestrogen- ies have not used serial transplant assays in the context
responsive Cre under control of the Krt5 promoter of the lung environment, and a bona fide human lung
(Krt5–Cre-ER), to determine which lung cells that are TPC remains to be defined. GEMMs have allowed for
null for Lkb1 and Pten are able to drive squamous disease. more systematic study of lung TPC phenotypes, includ-
ing serially transplanted tumours and metastases. Studies
Tumour-propagating cells (TPCs) and cellular plastic- in the KrasG12D-expressing and Trp53‑null model of ADC
ity: heterogeneity between tumour cells. ‘Cancer stem suggest that stem cell antigen 1 (SCA1, also known as
cells’ or TPCs, which are defined as the tumour cells Ly6A)+, CD24+, β4 integrin+, and NOTCH3hi mark
with the stem cell-properties of self-renewal and dif- the TPC population70,73. The identity of TPCs from
ferentiation, have the capacity to produce tumours in other ADC GEMMs is unknown; SCA1 did not enrich
540 | AUGUST 2014 | VOLUME 14 www.nature.com/reviews/cancer
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Box 2 | Lung stem and progenitor cell populations
after therapy 75. Further careful evaluation of TPC activ-
ity and cellular plasticity of tumour cells with patient
Genetic lineage tracing and cell biology approaches have shown that the murine lung tissues, probably using patient-derived xenograft (PDX)
contains region-specific stem and progenitor cell populations that respond to local
models and GEMMs of lung cancer, will help us to better
injury. Basal cells function as stem cells for the trachea, main bronchi and upper airways,
where they can replace the pseudostratified epithelium, including secretory club cells
understand tumour lineage conversion as a path towards
(previously known as Clara cells), mucus-producing goblet cells and ciliated cells136–138. developing chronic treatment resistance. These findings
In more distal airways, club cells are a self-renewing population that maintains the also highlight the importance of considering how cells of
ciliated cells139, and subsets of club cells, such as bronchiolar progenitors, can give rise origin may differ, depending on the therapeutic status
to ciliated and club cell lineages after injury140,141. In the alveolar space, where gas of the tumour environment.
exchange is carried out by alveolar epithelial type 1 (AT1) cells, the surfactant-
expressing AT2 cells can function as stem cells60,142. Another alveolar cell Integrated therapies for NSCLC
population, expressing α6β4 integrin, can also produce alveolar epithelia142,143. Target validation and patient stratification. Although
Bronchioalveolar stem cells (BASCs), which reside between the airway and alveolar studies of lung cancer genomes have implicated several
space, can give rise to both epithelial lineages56,114,144–146. Murine proximal and distal
genes as likely crucial mediators of tumour initiation and
lung stem cells can be isolated by fluorescence-activated cell sorting that uses different
cell surface markers and can be grown in three-dimensional culture systems to study
progression, experimental validation of the most impor-
their differentiation potential114,136,141,147. Basal cells can be isolated from mouse or tant, functional genomic changes in lung cancer cells
human lung on the basis of their expression of nerve growth factor receptor remains a challenge. Despite computational approaches
(NGFR)136,148, and AT2 cells can be purified from distal lung — most recently with the to separate ‘driver’ alterations from passenger altera-
marker HTII‑280 (REF. 142). Several other human lung stem cell populations have been tions, this distinction is probably more nuanced, and
reported in the human lung, but their roles have been controversial149, and this points to substantial work will need to be completed to model the
the characterization of human lung stem and progenitor cells as an important area for consequences of specific genome alterations in NSCLC.
future research. Furthermore, precisely how these cell types change their lineage Existing repositories of lung cancer cell lines, as well as
potential in the face of oncogenic insult coupled with injury is unknown and is likely to efforts to generate new cell lines from patient tumours
influence tumorigenesis; injury and transformation might substantially alter plasticity53.
have led to a number of important discoveries, although
A better understanding of lung stem and progenitor cells and methods for their analysis
would open up new ways to explore the cellular origins of lung tumorigenesis.
these cell lines still fail to represent the full diversity of
human NSCLCs79. Three-dimensional culture techniques
might also offer a new way to propagate normal and
for TPCs from the Kras- or EGFR-driven GEMMs74. tumorigenic lung cells to better probe vulnerabilities of
In the first lung-specific genetic model of SCC (the Lkb1- tumour cells49,73. Multiple in vivo models using mice to
and Pten-null model) the TPCs had a high expression recapitulate lung cancer disease processes and treatment
of SCA1 and the basal cell marker nerve growth factor responses have been generated, including GEMMs har-
receptor (NGFR). Intriguingly, these TPCs also expressed bouring specific genetic aberrations that have been iden-
high levels of the immune-checkpoint molecule PDL1, tified in human tumours55,80 (BOX 1). Translation of the
which may be targetable as described above49. Overall, experimental results obtained through in vitro and in vivo
these findings indicate the importance of taking the modelling systems has formed the basis for current and
genotype of the tumour into account when seeking to future patient stratification paradigms (BOX 3). The limi-
define a TPC population; each subset of NSCLC might tations of these approaches should also be considered in
harbour TPCs with unique surface markers and molec- future work to develop a more precise understanding of
ular drivers, which could each be uniquely targeted. how to predict therapy response.
Alternatively, many subsets of NSCLC might not have
one TPC population that can be defined. Future research Current treatments for NSCLC. The past decade has
focusing on resolving the metastatic activity and therapy seen some truly impressive new treatments for subsets of
response of murine TPCs and the molecules that control patients with lung cancer, most of whom harbour muta-
them may help to translate these findings to improve the tions in one of the key oncogenic driver mutants upon
treatment of patients with lung cancer. which tumour survival and progression are depend-
The genetic complexity and rapid clonal evolution ent. These include mutations in EGFR, the echinoderm
of lung tumours could mean that if TPCs do occur in microtubule-associated protein-like 4 (EML4)–ALK fusion
most lung cancers, they will have a high degree of plas- and ROS1 fusions81,82. Extensive preclinical and clinical
ticity. Fascinating clinical observations have shown some studies have proven the marked treatment responses and
patients who are initially diagnosed with EGFR-driven survival advantages over conventional chemotherapies
Pseudostratified epithelium ADCs develop SCLC after long-term treatment with the that are provided by target-specific inhibitors to EGFR-
This describes the epithelium EGFR tyrosine kinase inhibitors gefitinib or erlotinib75,76. activating mutations or to ALK fusions 83–85. Recent
of the trachea, which is truly a In contrast to ADC models, lineage tracing and viruses genomic analyses of lung SCC have also given the first
monolayer but appears to have
that are engineered to express Cre under the control of set of potentially targetable driver mutations, including
some stratification due to the
variable distances of the nuclei various cell-type-specific promoters have been used to FGFR1, FGFR2, FGFR3, DDR2 and PI3K20. Clinical trials
from the basal lamina. show that SCLCs probably arise from neuroendocrine that aim to target these subsets of patients who have Stage
cells76–78. However, examination of these tumours before I–IIIA lung cancers are currently underway; preliminary
Patient-derived xenograft and after SCLC conversion shows the persistence of the results were presented at the 2014 American Association
(PDX). Primary tumour cells
from fresh patient tumours that
same EGFR mutations, suggesting a shared clonal ori- for Cancer Research Annual Meeting86, and these showed
are propagated subcutaneously gin of both types of tumours. This highlights the poten- responses to an FGFR inhibitor (BGJ398) in a subset of
in immunocompromised mice. tial epigenetic plasticity of lung cells and lung tumours patients with SCC who have FGFR1 amplification.
NATURE REVIEWS | CANCER VOLUME 14 | AUGUST 2014 | 541
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Box 3 | Patient stratification
resistance mechanism that is evident by an improved
response and survival in patients with EGFR mutations
Stratification and treatment selection for patients with non-small-cell lung cancer who have an increased expression of the NF‑κB inhibi-
(NSCLC) heavily relies on radiographical and pathological evaluation in standard tor IκBα (also known as NFKBIA)96. In addition, a com-
clinical practice. In recent years, molecular diagnostic platforms have been gradually mon BIM (also known as BCL2L11) polymorphism that
introduced into this process. Today, many cancer centres and hospitals have adopted
results in changes in splicing and the deletion of the pro-
some degree of genetic diagnosis. Commonly accepted oncogenic driver mutations,
including KRAS, epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase
apoptotic BCL‑2‑homology domain (BH3) was shown to
(ALK), ROS and BRAF, are being sequenced and detected as a standard diagnosis potentially mediate intrinsic resistance to EGFR inhibi-
procedure. Increasingly, mutation-based decision-making procedures are being tors97, highlighting the complexity of possible resistance
integrated in the clinic, and we expect that additional novel technology platforms that mechanisms. It is conceivable that the comprehen-
stratify tumours according to the specific metabolome, epigenome and immune profile sive acquisition of information on different aspects of
of each patient will be applied in the clinic in the near future. The anticipated challenge tumour biology, such as genomic and kinase profiling in
is how best to verify and use the vast amounts of sequencing information for translation patients, will be crucial in the future to determine the best
to the clinic. Ongoing efforts seek to optimize data mining that will link existing course of treatment following any new diagnosis or the
genomic and biological data with clinical databases. In 2013, the Broad Institute, development of acquired resistance.
Cambridge, Massachusetts, USA, launched a global alliance that intends to share
Most patients with advanced stage NSCLC without
genomic and clinical data. A similar effort at Vanderbilt University, Nashville, Tennessee,
USA, which is mediated by a publicly accessible website (My Cancer Genome),
targetable genomic alterations are still treated by conven-
emphasizes the clinical application of cancer research. Worldwide efforts, such as the tional chemotherapies. Activating KRAS mutations were
International Cancer Genome Consortium (ICGC) and the Catalogue of Somatic identified and verified long before the discovery of mutant
Mutations in Cancer (COSMIC) from the Sanger Institute, Hinxton, UK, and joint efforts EGFR. However, treatment choices for patients with
in European countries to establish organoid cultures from primary tumours or biopsies KRAS-mutant lung cancer are still very limited. Current
from patients are also under way. Despite these independent efforts to integrate data efforts to treat this subset of patients have been mostly
sets, a more organized programme is needed on the national and international levels. focused on inhibiting common KRAS downstream sig-
The US National Center for Biotechnology Information recently initiated nalling cascades. The RAF–MEK–ERK pathway, which
whole-genome sequencing to identify rare, druggable oncogenic events in patients is activated directly downstream of KRAS, has proven to
who showed isolated but marked responses to certain drugs; this may represent the
be a valid target in both preclinical models and clinical tri-
first exploratory step towards an integrated programme.
als98–100. However, the clinical benefits of MEK inhibitors,
even in combination with other agents, are still somewhat
Unfortunately, acquired resistance to chronic treat- moderate compared to those of target-specific inhibi-
ment often develops within 9–12 months in most patients tors such as erlotinib for patients with activating EGFR
who are treated with kinase inhibitors84,87,88. Therefore, mutations, and the use of MEK inhibitors is associated
patients who have Stage I–IIIA tumours are still treated with additional complications and enhanced toxicity 100.
by surgical resection as a first-line treatment and receive The available preclinical and clinical results present clear
combination chemotherapy as a standard of care, with challenges to the common belief that therapies target-
the use of targeted agents still considered to be experi- ing one or a few specific alterations should have fewer
mental. For patients with advanced disease who have side effects and lower toxicity compared to standard
progressed on an inhibitor of EGFR or ALK, several chemotherapies. Indeed, this is not entirely a surprise,
recurrent secondary mutations have been identified, such as many of the targeted pathways for lung cancer treat-
as EGFR‑T790M and additional kinase domain mutations ment are also essential for normal tissue functions. The
in ALK87,88. Hence, finding treatments for tumours that simultaneous inhibition of multiple signalling pathways
are resistant to first-generation EGFR or ALK inhibi- can be deleterious to necessary normal cells. One pos-
tors has been a recent focus. Several newly developed sible remedy being explored is to optimize treatment
inhibitors that either have more potency or are ration- schedules and improve targeting efficiencies for single-
ally designed to favourably target the mutated kinases, pathway inhibition by improving inhibitor potency or
such as AZD9291 and CO‑1686 for EGFR and LDK378 linear inhibition of multiple targets within the pathway.
for EML4–ALK, have generated promising initial clini- Nonetheless, alternative treatment approaches with less
cal results89–91. Discovery of the mechanisms that under- toxicity and better responses are of immediate need. A few
lie acquired resistance in patients without additional studies have more recently reported the rational design
mutations in the primary driver gene is also greatly of KRAS inhibitors that target the cysteine residue of the
facilitated by high-throughput analytical approaches. common KRAS mutation G12C in lung cancer 101,102, and
Amplifications of ALK and alternative pro-cancerous these are therefore similar to the second-generation EGFR
pathway activations were identified in ALK fusion- inhibitors (such as WZ4002, AZD9291 and CO‑1686)
positive patients who have become resistant to the first- that target EGFR‑T790M. In vitro studies of these KRAS
generation ALK inhibitor crizotinib87. In patients who inhibitors demonstrate a proof of concept 101,102; however,
are resistant to chronic EGFR inhibitor treatment, a wide the in vivo efficacy of these molecules still requires much
EGFR‑T790M range of resistance mechanisms has been reported. These more investigation.
The most common mutation include increased activities of additional kinases owing
(~50%) in the epidermal to MET, HER2 or ERK amplification, additional muta- Targeting multiple cellular compartments in lung can-
growth factor receptor (EGFR)
gene that confers resistance to
tion of PIK3CA (which encodes the PI3K p110α sub cer. Similar to KRAS mutations, many newly identified
EGFR tyrosine kinase inhibitors unit) or overexpression of AXL kinase14,92–95. Enhanced potential pro-cancerous changes, such as overexpression
such as erlotinib and gefitinib. NF‑κB signalling activity was also implied as one possible of the transcription factors SOX2 and MYC103–105, present
542 | AUGUST 2014 | VOLUME 14 www.nature.com/reviews/cancer
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
Cytotoxic T lymphocyte clear challenges to our current ideas about treatment enable marked perturbation of gene expression within
protein 4 approaches — in cases in which there is no clear drugga- tumour cells to stop tumour growth. The recently devel-
(CTLA4; also known as ble target, what can be done? Furthermore, the short-lived oped bromodomain protein inhibitors have shown effi-
CD152). A surface receptor in vivo efficacy for most if not all existing small molecule cacy in numerous preclinical studies116, including in lung
that transmits inhibitory
signals to T cells.
inhibitors87,106 also advocates more durable treatment cancer 117, and they are currently under evaluation in the
approaches. On the basis of our current understanding, clinic, including in the ongoing Phase I clinical trials
CD73 the more effective approach probably requires therapies NCT01987362 and NCT01587703. Variations in expres-
A cell surface enzyme that that not only target tumour cells but also target other sion as well as recurrent mutations were also reported
generates extracellular
components of the tumour, such as tumour vasculature, for several histone- and DNA-modifying enzymes,
adenosine, which inhibits
T cell function.
tumour-associated fibroblasts and tumour-specific and/or including enhancer of zeste homologue 2 (EZH2), TET
non-specific immune cells. Besides the more recently methylcytosine dioxygenase 2 (TET2) and DNA methyl
CD47 studied PD1–PDL1 inhibitory pathway, other approaches transferase 3A (DNMT3A) in all subtypes of NSCLC28.
The receptor for that intervene with the immune system, such as antibod- In a similar concept, altered metabolism is one of the key
thrombospondin 1 (TSP1).
CD47 is highly expressed in
ies against cytotoxic T lymphocyte protein 4 (CTLA4; also features of cancer cells. Anti-diabetic drugs, insulin-like
many tumour cells. known as CD152), CD73 or CD47, and more sophisticated growth factor 1 receptor (IGF1R) inhibitors and drugs
cellular immune therapies, such as engineered T cell that target glycolysis or lipid, nucleic acid and amino acid
Chimeric antigen receptors therapy using chimeric antigen receptors (CARs), are also synthesis are currently being explored for antitumour
(CARs). Genetically engineered
under extensive scrutiny 107–110. More importantly, ongo- activities in NSCLC118–121. Targeting metabolism is cer-
receptors that result in desired
specificity (to tumour cells) in
ing efforts are seeking to discover the best combination tainly promising for cancer control, particularly when
effector T cells. approach that integrates immune therapy with other combined with other approaches. Recent studies have also
therapies. Angiogenesis has long been seen as a possible highlighted connections between TET and IDH, which
CpG island methylator therapeutic window, with many novel therapeutic agents could have resulted in a CpG island methylator phenotype
phenotype
(CIMP). Reflects the genomic
that have been developed or are being developed to clini- (CIMP) in a subset of lung cancer, and this ‘connects the
status that multiple CpG cally target this process, although the overall efficacy of dots’ between epigenetics and metabolism122–124.
islands are methylated anti-angiogenic agents has been modest in unselected
simultaneously, leading to patient cohorts111. Emerging evidence has suggested that Conclusion
epigenetic inactivation of
the combination of immunotherapy and anti-angiogenic The quickened pace of discovery of mechanisms that
different genes, including
tumour suppressors.
agents has potential synergistic effects112,113, pointing to underlie lung cancer development and possible treatments
a new possible avenue to mutually enhance both treat- in the past decade present the opportunity to integrate
ments. In addition to providing key nutrients and oxy- information from multiple approaches for future lung
genated blood, tumour vasculature might have a role cancer treatment. Large amounts of information about the
in supporting TPCs35,114. Similarly, stromal cells such as identity of individual lung tumours are being collected.
fibroblasts have been shown to provide additional signals New and improved functional studies are needed to meet
that support tumour growth and survival, and they may the pace of data set generation, and all of the aspects of
therefore have major roles in primary and acquired treat- tumour heterogeneity — genetic, cellular and epigenetic
ment resistance35,115. Understanding how best to target — need to be integrated to determine better approaches to
these various aspects of the tumour microenvironment make an impact in this devastating disease. We anticipate
would require a high-throughput comparison of changes the future treatment scheme to be a genotype-depend-
in the tumour microenvironment that occur upon single ent, carefully selected combination that would ensure an
and combination treatments. enhanced tumour immune reaction, inhibition of angio-
Targeted therapies might also be able to indirectly genesis and blockade of interactions between tumour cells
regulate tumour growth. Two prominent examples are and stromal cells. Thus, we advocate ‘integrated therapy’,
drugs that target epigenetic enzymes and metabolic in contrast to the current concept of targeted therapy, as
enzymes. Targeting epigenetic enzymes is expected to the future of effective NSCLC treatment.
1. Jemal, A. et al. Global cancer statistics. CA Cancer 8. Davies, H. et al. Mutations of the BRAF gene in human 12. Pao, W. et al. EGF receptor gene mutations are
J. Clin. 61, 69–90 (2011). cancer. Nature 417, 949–954 (2002). common in lung cancers from “never smokers” and are
2. Siegel, R., Naishadham, D. & Jemal, A. Cancer 9. Santos, E. et al. Malignant activation of a K‑ras associated with sensitivity of tumors to gefitinib and
statistics, 2013. CA Cancer J. Clin. 63, 11–30 (2013). oncogene in lung carcinoma but not in normal erlotinib. Proc. Natl Acad. Sci. USA 101,
3. Ettinger, D. S. et al. Non-Small Cell Lung Cancer, tissue of the same patient. Science 223, 661–664 13306–13311 (2004).
Version 2.2013. J. Natl Compr. Canc. Netw. 11, (1984). 13. Shepherd, F. A. et al. Erlotinib in previously treated
645–653 (2013). 10. Lynch, T. J. et al. Activating mutations in the epidermal non-small-cell lung cancer. N. Engl. J. Med. 353,
4. Davidson, M. R., Gazdar, A. F. & Clarke, B. E. The growth factor receptor underlying responsiveness of 123–132 (2005).
pivotal role of pathology in the management of lung non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 14. Engelman, J. A. et al. MET amplification leads to
cancer. J. Thorac. Dis. 5, S463–S478 (2013). 350, 2129–2139 (2004). gefitinib resistance in lung cancer by activating ERBB3
5. Langer, C. J., Besse, B., Gualberto, A., Brambilla, E. & 11. Paez, J. G. et al. EGFR mutations in lung cancer: signaling. Science 316, 1039–1043 (2007).
Soria, J.‑C. The evolving role of histology in the correlation with clinical response to gefitinib therapy. 15. Fernandez-Cuesta, L. et al. CD74‑NRG1 fusions in lung
management of advanced non–small-cell lung cancer. Science 304, 1497–1500 (2004). adenocarcinoma. Cancer Discov. 4, 415–422 (2014).
J. Clin. Oncol. 28, 5311–5320 (2010). In this study, the clinical observation that only 16. Kohno, T. et al. KIF5B‑RET fusions in lung
6. Rock, J. R., Randell, S. H. & Hogan, B. L. M. Airway some lung cancers responded well to the EGFR adenocarcinoma. Nature Med. 18, 375–377 (2012).
basal stem cells: a perspective on their roles in inhibitor gefitinib was linked to the presence of 17. Rikova, K. et al. Global survey of phosphotyrosine
epithelial homeostasis and remodeling. Dis. Model. EGFR-activating mutations in the responding signaling identifies oncogenic kinases in lung cancer.
Mech. 3, 545–556 (2010). tumours. This finding revolutionized the Cell 131, 1190–1203 (2007).
7. Lu, Y. et al. Evidence that Sox2 overexpression is stratification of patients that receive EGFR 18. Soda, M. et al. Identification of the transforming
oncogenic in the lung. PLoS ONE 5, http://dx.doi. inhibitor treatment and furthered our EML4‑ALK fusion gene in non-small-cell lung cancer.
org/10.1371/journal.pone.0011022 (2010). understanding of oncogene addiction in NSCLC. Nature 448, 561–566 (2007).
NATURE REVIEWS | CANCER VOLUME 14 | AUGUST 2014 | 543
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
19. Stephens, P. et al. Lung cancer: intragenic ERBB2 40. Zaynagetdinov, R. et al. A critical role for macrophages 62. Rowbotham, S. P. & Kim, C. F. Diverse cells at the
kinase mutations in tumours. Nature 431, 525–526 in promotion of urethane-induced lung carcinogenesis. origin of lung adenocarcinoma. Proc. Natl Acad. Sci.
(2004). J. Immunol. 187, 5703–5711 (2011). USA 111, 4745–4746 (2014).
20. The Cancer Genome Atlas Research Network (TCGA). 41. Bellocq, A. et al. Neutrophil alveolitis in 63. Sutherland, K. D. et al. Multiple cells‑of‑origin of
Comprehensive genomic characterization of squamous bronchioloalveolar carcinoma: induction by tumor- mutant K‑Ras–induced mouse lung adenocarcinoma.
cell lung cancers. Nature 489, 519–525 (2012). derived interleukin‑8 and relation to clinical outcome. Proc. Natl Acad. Sci. USA 111, 4952–4957 (2014).
As part of The Cancer Genome Atlas, this study Am. J. Pathol. 152, 83–92 (1998). 64. Giangreco, A. et al. β‑Catenin determines upper
was the first to provide a comprehensive landscape 42. Houghton, A. M. et al. Neutrophil elastase-mediated airway progenitor cell fate and preinvasive squamous
of genomic and epigenomic alterations in lung degradation of IRS‑1 accelerates lung tumor growth. lung cancer progression by modulating epithelial–
SCCs. This study identified potential druggable Nature Med. 16, 219–223 (2010). mesenchymal transition. J. Pathol. 226, 575–587
targets in most tumours, and many of these targets 43. Mantovani, A., Cassatella, M. A., Costantini, C. & (2012).
are now being validated as therapeutic options. Jaillon, S. Neutrophils in the activation and regulation 65. Ji, H. et al. LKB1 modulates lung cancer
21. Vaishnavi, A. et al. Oncogenic and drug-sensitive of innate and adaptive immunity. Nature Rev. differentiation and metastasis. Nature 448, 807–810
NTRK1 rearrangements in lung cancer. Nature Med. Immunol. 11, 519–531 (2011). (2007).
19, 1469–1472 (2013). 44. Brahmer, J. R. et al. Safety and activity of anti‑PD‑L1 This study validated Lkb1 as a bona fide tumour
22. Weiss, J. et al. Frequent and focal FGFR1 amplification antibody in patients with advanced cancer. N. Engl. suppressor in NSCLC by deleting Lkb1 in the
associates with therapeutically tractable FGFR1 J. Med. 366, 2455–2465 (2012). KRAS-driven GEMM of lung cancer. Lkb1 loss not
dependency in squamous cell lung cancer. Sci Transl. 45. Topalian, S. L. et al. Safety, activity, and immune only potentiated tumour development but also
Med. 2, 62ra93 (2010). correlates of anti‑PD‑1 antibody in cancer. N. Engl. promoted metastasis and drove tumours with
23. Ding, L. et al. Somatic mutations affect key pathways J. Med. 366, 2443–2454 (2012). mixed ADC and SCC characteristics.
in lung adenocarcinoma. Nature 455, 1069–1075 References 44 and 45 were the first studies to 66. Malkoski, S. P. et al. Role of PTEN in basal cell derived
(2008). show the efficacy and durable response of lung carcinogenesis. Mol. Carcinog. http://dx.doi.
24. Imielinski, M. et al. Mapping the hallmarks of lung immunotherapy for the treatment of late-stage org/10.1002/mc.22030 (2013).
adenocarcinoma with massively parallel sequencing. NSCLCs. The data suggest a relationship between 67. Beck, B. & Blanpain, C. Unravelling cancer stem cell
Cell 150, 1107–1120 (2012). PDL1 expression on tumour cells and objective potential. Nature Rev. Cancer 13, 727–738 (2013).
25. Heist, R. S. & Engelman, J. A. Snapshot: non-small response, leading to many new studies examining 68. Li, F., Tiede, B., Massague, J. & Kang, Y. Beyond
cell lung cancer. Cancer Cell 21, 448–448.e2 (2012). the expression of this immune-evasion molecule tumorigenesis: cancer stem cells in metastasis. Cell
26. Guagnano, V. et al. FGFR genetic alterations predict on different NSCLCs. Res. 17, 3–14 (2007).
for sensitivity to NVP‑BGJ398, a selective pan-FGFR 46. Keir, M. E., Butte, M. J., Freeman, G. J. & 69. Jiang, F. et al. Aldehyde dehydrogenase 1 is a tumor
inhibitor. Cancer Discov. 2, 1118–1133 (2012). Sharpe, A. H. PD‑1 and its ligands in tolerance and stem cell-associated marker in lung cancer. Mol.
27. Hammerman, P. S. et al. Mutations in the DDR2 immunity. Annu. Rev. Immunol. 26, 677–704 (2008). Cancer Res. 7, 330–338 (2009).
kinase gene identify a novel therapeutic target in 47. Forde, P. M., Kelly, R. J. & Brahmer, J. R. New 70. Lau, A. N. et al. Tumor-propagating cells and Yap/Taz
squamous cell lung cancer. Cancer Discov. 1, 78–89 strategies in lung cancer: translating immunotherapy activity contribute to lung tumor progression and
(2011). into clinical practice. Clin. Cancer Res. 20, metastasis. EMBO J. 33, 468–481 (2014).
28. Kandoth, C. et al. Mutational landscape and 1067–1073 (2014). 71. Liu, J. et al. Lung cancer tumorigenicity and drug
significance across 12 major cancer types. Nature 48. Akbay, E. A. et al. Activation of the PD‑1 pathway resistance are maintained through ALDHhiCD44hi
502, 333–339 (2013). contributes to immune escape in EGFR-driven lung tumor initiating cells. Oncotarget 4, 1698–1711
29. The Cancer Genome Atlas Research Network (TCGA). tumors. Cancer Discov. 3, 1355–1363 (2013). (2013).
Comprehensive molecular profiling of lung 49. Xu, C. et al. Loss of Lkb1 and Pten leads to lung 72. Sullivan, J. P. et al. Aldehyde dehydrogenase activity
adenocarcinoma. Nature http://dx.doi.org/10.1038/ squamous cell carcinoma with elevated PD‑L1 selects for lung adenocarcinoma stem cells dependent
nature13385 (2014). expression. Cancer Cell 25, 590–604 (2014). on Notch signaling. Cancer Res. 70, 9937–9948
30. Lawrence, M. S. et al. Discovery and saturation 50. Ancrile, B., Lim, K. H. & Counter, C. M. Oncogenic Ras- (2010).
analysis of cancer genes across 21 tumour types. induced secretion of IL6 is required for tumorigenesis. 73. Zheng, Y. et al. A rare population of
Nature 505, 495–501 (2014). Genes Dev. 21, 1714–1719 (2007). CD24+ITGB4+Notchhi cells drives tumor propagation
In this study, the genetic complexity of 21 tumour 51. Gao, S. P. et al. Mutations in the EGFR kinase domain in NSCLC and requires Notch3 for self-renewal. Cancer
types was directly compared, demonstrating that mediate STAT3 activation via IL‑6 production in Cell 24, 59–74 (2013).
both lung ADCs and lung SCCs have extremely high human lung adenocarcinomas. J. Clin. Invest. 117, 74. Curtis, S. J. et al. Primary tumor genotype is an
somatic mutation rates compared with other 3846–3856 (2007). important determinant in identification of lung cancer
tumour types. These authors also present a 52. Visvader, J. E. Cells of origin in cancer. Nature 469, propagating cells. Cell Stem Cell 7, 127–133 (2010).
comprehensive catalogue of cancer genes for each 314–322 (2011). In this study, an orthotopic serial transplantation
tumour subtype, furthering our global 53. Tata, P. R. et al. Dedifferentiation of committed model of primary murine lung tumour cells was
understanding of cancer. epithelial cells into stem cells in vivo. Nature 503, used to identify the first bona fide TPC population
31. Govindan, R. et al. Genomic landscape of non-small 218–223 (2013). in lung cancer. Importantly, TPC phenotype was
cell lung cancer in smokers and never-smokers. Cell 54. Chaffer, C. L. et al. Normal and neoplastic nonstem shown to be dependent on primary tumour
150, 1121–1134 (2012). cells can spontaneously convert to a stem-like state. genotype, suggesting that TPC characteristics will
32. Barbie, D. A. et al. Systematic RNA interference Proc. Natl Acad. Sci. 108, 7950–7955 (2011). differ for different driver mutations.
reveals that oncogenic KRAS-driven cancers require 55. Kwon, M. & Berns, A. Mouse models for lung cancer. 75. Sequist, L. V. et al. Genotypic and histological
TBK1. Nature 462, 108–112 (2009). Mol. Oncol. 7, 165–177 (2013). evolution of lung cancers acquiring resistance to EGFR
33. Sun, N. et al. Isocitrate dehydrogenase 1 is a novel 56. Kim, C. et al. Identification of bronchioalveolar stem inhibitors. Sci. Transl. Med. 3, 75ra26 (2011).
plasma biomarker for the diagnosis of non-small cell cells in normal lung and lung cancer. Cell 121, 76. Song, H. et al. Functional characterization of
lung cancer. Clin. Cancer Res. 19, 5136–5145 823–835 (2005). pulmonary neuroendocrine cells in lung development,
(2013). This study was the first to characterize a bipotent injury, and tumorigenesis. Proc. Natl Acad. Sci. USA
34. Tan, F. et al. Identification of isocitrate cell type in the distal lung, termed the BASC. 109, 17531–17536 (2012).
dehydrogenase 1 as a potential diagnostic and Importantly, the BASCs were shown to expand in 77. Park, K.‑S. et al. Characterization of the cell of origin
prognostic biomarker for non-small cell lung cancer response to oncogenic KRAS activation, suggesting for small cell lung cancer. Cell Cycle 10, 2806–2815
by proteomic analysis. Mol. Cell Proteomics 11, that they could function as a cell of origin for lung (2011).
M111.008821 (2012). ADC. 78. Sutherland, K. D. et al. Cell of origin of small cell lung
35. Quail, D. F. & Joyce, J. A. Microenvironmental 57. Tiozzo, C. et al. Deletion of Pten expands lung cancer: inactivation of Trp53 and Rb1 in distinct cell
regulation of tumor progression and metastasis. epithelial progenitor pools and confers resistance to types of adult mouse lung. Cancer Cell 19, 754–764
Nature Med. 19, 1423–1437 (2013). airway injury. Am. J. Respir. Crit. Care Med. 180, (2011).
36. DuPage, M. et al. Endogenous T cell responses to 701–712 (2009). 79. Gazdar, A. F., Girard, L., Lockwood, W. W., Lam, W. L.
antigens expressed in lung adenocarcinomas delay 58. Ventura, J. J. et al. p38α MAP kinase is essential in & Minna, J. D. Lung cancer cell lines as tools for
malignant tumor progression. Cancer Cell 19, 72–85 lung stem and progenitor cell proliferation and biomedical discovery and research. J. Natl Cancer
(2011). differentiation. Nature Genet. 39, 750–758 (2007). Inst. 102, 1310–1321 (2010).
By engineering KRAS-driven GEMM tumours to 59. Xu, X. et al. Evidence for type II cells as cells of origin 80. Dow, L. E. & Lowe, S. W. Life in the fast lane:
express neoantigens, the authors of this study of K‑Ras-induced distal lung adenocarcinoma. Proc. mammalian disease models in the genomics era. Cell
explored the dynamic responses of endogenous Natl Acad. Sci. USA109, 4910–4915 (2012). 148, 1099–1109 (2012).
T cells to naturally arising tumours and informed This study expanded our understanding of cells of 81. Levy, M. A., Lovly, C. M. & Pao, W. Translating
our ideas about how lung tumours interact with origin in GEMMs of lung ADC by using cell-type genomic information into clinical medicine: lung cancer
immune cells. specific promoters to drive Cre-Lox Kras activation. as a paradigm. Genome Res. 22, 2101–2108 (2012).
37. Murdoch, C., Muthana, M., Coffelt, S. B. & Lewis, C. E. In contrast to previous theories, the authors find 82. Shaw, A. T., Hsu, P. P., Awad, M. M. & Engelman, J. A.
The role of myeloid cells in the promotion of tumour that AT2 cells, rather than BASCs or club cells, are Tyrosine kinase gene rearrangements in epithelial
angiogenesis. Nature Rev. Cancer 8, 618–631 the most likely cells of origin for KRAS-driven malignancies. Nature Rev. Cancer 13, 772–787
(2008). tumours. (2013).
38. Xiao, Z. et al. The pivotal role of IKKα in the 60. Desai, T. J., Brownfield, D. G. & Krasnow, M. A. 83. Camidge, D. R. et al. Activity and safety of crizotinib in
development of spontaneous lung squamous cell Alveolar progenitor and stem cells in lung patients with ALK-positive non-small-cell lung cancer:
carcinomas. Cancer Cell 23, 527–540 (2013). development, renewal and cancer. Nature 507, updated results from a phase 1 study. Lancet Oncol.
39. Vignaud, J.‑M. et al. The role of platelet-derived 190–194 (2014). 13, 1011–1019 (2012).
growth factor production by tumor-associated 61. Mainardi, S. et al. Identification of cancer initiating 84. Mok, T. S. et al. Gefitinib or carboplatin-paclitaxel in
macrophages in tumor stroma formation in lung cells in K‑Ras driven lung adenocarcinoma. Proc. Natl pulmonary adenocarcinoma. N. Engl. J. Med. 361,
cancer. Cancer Res. 54, 5455–5463 (1994). Acad. Sci. USA 111, 255–260 (2014). 947–957 (2009).
544 | AUGUST 2014 | VOLUME 14 www.nature.com/reviews/cancer
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
85. Shaw, A. T. et al. Effect of crizotinib on overall survival 109. Tseng, D. et al. Anti‑CD47 antibody-mediated 135. Zhang, W. C. et al. Glycine decarboxylase activity
in patients with advanced non-small-cell lung cancer phagocytosis of cancer by macrophages primes an drives non-small cell lung cancer tumor-initiating cells
harbouring ALK gene rearrangement: a retrospective effective antitumor T‑cell response. Proc. Natl Acad. and tumorigenesis. Cell 148, 259–272 (2012).
analysis. Lancet Oncol. 12, 1004–1012 (2011). Sci. USA 110, 11103–11108 (2013). 136. Rock, J. R. et al. Basal cells as stem cells of the mouse
86. Sequist, L. V. et al. Phase I study of BGJ398, a 110. Zhang, B. CD73: a novel target for cancer trachea and human airway epithelium. Proc. Natl
selective pan-FGFR inhibitor in genetically immunotherapy. Cancer Res. 70, 6407–6411 Acad. Sci. USA 106, 12771–12775 (2009).
preselected advanced solid tumors. AACR Meet. (2010). In this study, the KRT5+ and p63+ basal cells of the
[Abstr] CT326 (2014). 111. Sandler, A. et al. Paclitaxel-carboplatin alone or with trachea were shown to be true stem or progenitor
87. Katayama, R. et al. Mechanisms of acquired crizotinib bevacizumab for non-small-cell lung cancer. N. Engl. cells through lineage tracing experiments during
resistance in ALK-rearranged lung cancers. Sci. Transl. J. Med. 355, 2542–2550 (2006). development and tracheal epithelial repair. The
Med. 4, 120ra17 (2012). 112. Schoenfeld, J. et al. Active immunotherapy induces authors isolated similar cells from human tracheas
88. Kobayashi, S. et al. EGFR mutation and resistance of antibody responses that target tumor angiogenesis. and showed that both murine and human cells can
non-small-cell lung cancer to gefitinib. N. Engl. J. Med. Cancer Res. 70, 10150–10160 (2010). be cultured as tracheospheres in three-dimensional
352, 786–792 (2005). 113. Yuan, J. et al. Pretreatment serum VEGF is associated Matrigel-containing transwells.
89. Shaw, A. T. et al. Ceritinib in ALK-rearranged non- with clinical response and overall survival in advanced 137. Hegab, A. E. et al. Novel stem/progenitor cell
small-cell lung cancer. N. Engl. J. Med. 370, melanoma patients treated with ipilimumab. Cancer population from murine tracheal submucosal gland
1189–1197 (2014). Immunol. Res. 2, 127–132 (2014). ducts with multipotent regenerative potential.
90. Walter, A. O. et al. Discovery of a mutant-selective 114. Lee, J.‑H. et al. Lung stem cell differentiation in mice Stem Cells 29, 1283–1293 (2011).
covalent inhibitor of EGFR that overcomes directed by endothelial cells via a 138. Rock, J. R. & Hogan, B. L. M. Epithelial progenitor cells
T790M‑mediated resistance in NSCLC. Cancer Discov. BMP4‑NFATc1‑thrombospondin‑1 axis. Cell 156, in lung development, maintenance, repair, and disease.
3, 1404–1415 (2013). 440–455 (2014). Annu. Rev. Cell Dev. Biol. 27, 493–512 (2011).
91. Cross, D. A. et al. AZD9291, an irreversible EGFR TKI, 115. Straussman, R. et al. Tumour micro-environment 139. Rawlins, E. L. et al. The role of Scgb1a1+ Clara cells in
overcomes T790M‑mediated resistance to EGFR elicits innate resistance to RAF inhibitors through HGF the long-term maintenance and repair of lung airway,
inhibitors in lung cancer. Cancer Discov. http://dx.doi. secretion. Nature 487, 500–504 (2012). but not alveolar, epithelium. Cell Stem Cell 4,
org/10.1158/2159-8290.CD-14-0337 (2014). 116. Filippakopoulos, P. et al. Selective inhibition of BET 525–534 (2009).
92. Yonesaka, K. et al. Activation of ERBB2 signaling bromodomains. Nature 468, 1067–1073 (2010). 140. Teixeira, V. H. et al. Stochastic homeostasis in human
causes resistance to the EGFR-directed therapeutic 117. Shimamura, T. et al. Efficacy of BET bromodomain airway epithelium is achieved by neutral competition of
antibody cetuximab. Sci. Transl. Med. 3, 99ra86 inhibition in Kras-mutant non-small cell lung cancer. basal cell progenitors. eLife 2, http://dx.doi.org/
(2011). Clin. Cancer Res. 19, 6183–6192 (2013). 10.7554/eLife.00966#sthash.XxrCqaIk.dpuf (2013).
93. Zhang, Z. et al. Activation of the AXL kinase causes 118. Liu, Y. et al. Metabolic and functional genomic studies 141. Teisanu, R. M., Lagasse, E., Whitesides, J. F. &
resistance to EGFR-targeted therapy in lung cancer. identify deoxythymidylate kinase as a target in Stripp, B. R. Prospective Isolation of Bronchiolar Stem
Nature Genet. 44, 852–860 (2012). LKB1‑mutant lung cancer. Cancer Discov. 3, 870–879 Cells Based Upon Immunophenotypic and
94. Ercan, D. et al. Reactivation of ERK signaling causes (2013). Autofluorescence Characteristics. Stem Cells 27,
resistance to EGFR kinase inhibitors. Cancer Discov. 2, 119. Molina-Arcas, M., Hancock, D. C., Sheridan, C., 612–622 (2009).
934–947 (2012). Kumar, M. S. & Downward, J. Coordinate direct input 142. Barkauskas, C. E. et al. Type 2 alveolar cells are stem
95. Lin, L. & Bivona, T. G. Mechanisms of resistance to of both KRAS and IGF1 receptor to activation of PI3 cells in adult lung. J. Clin. Invest. 123, 3025–3036
epidermal growth factor receptor inhibitors and novel kinase in KRAS-mutant lung cancer. Cancer Discov. 3, (2013).
therapeutic strategies to overcome resistance in 548–563 (2013). This study was the first to show that AT2 cells can
NSCLC patients. Chemother. Res. Pract. 2012, 120. Orita, H. et al. Selective inhibition of fatty acid function as facultative stem or progenitor cells in
817297 (2012). synthase for lung cancer treatment. Clin. Cancer Res. the adult lung to differentiate into both AT2 and
96. Bivona, T. G. et al. FAS and NF‑κB signalling modulate 13, 7139–7145 (2007). AT1 lineages after injury.
dependence of lung cancers on mutant EGFR. Nature 121. Shackelford, D. B. et al. LKB1 inactivation dictates 143. Chapman, H. A. et al. Integrin α6β4 identifies an adult
471, 523–526 (2011). therapeutic response of non-small cell lung cancer to distal lung epithelial population with regenerative
97. Xu, K. et al. EZH2 Oncogenic Activity in Castration- the metabolism drug phenformin. Cancer Cell 23, potential in mice. J. Clin. Invest. 121, 2855–2862
Resistant Prostate Cancer Cells Is Polycomb- 143–158 (2013). (2011).
Independent. Science 338, 1465–1469 (2012). 122. Hughes, L. A. et al. The CpG island methylator 144. Tropea, K. A. et al. Bronchioalveolar stem cells increase
98. Chen, Z. et al. A murine lung cancer co‑clinical trial phenotype: what’s in a name? Cancer Res. 73, after mesenchymal stromal cell treatment in a mouse
identifies genetic modifiers of therapeutic response. 5858–5868 (2013). model of bronchopulmonary dysplasia. Am. J. Physiol.
Nature 483, 613–617 (2012). 123. Losman, J. A. & Kaelin, W. G. Jr. What a difference a Lung Cell. Mol. Physiol. 302, L829–L837 (2012).
This study was the first of its kind to use GEMMs to hydroxyl makes: mutant IDH, (R)-2‑hydroxyglutarate, 145. Zacharek, S. J. et al. Lung stem cell self-renewal relies
conduct a co-clinical trial that mirrored an ongoing and cancer. Genes Dev. 27, 836–852 (2013). on BMI1‑dependent control of expression at imprinted
human clinical trial in patients with KRAS-mutant 124. Shinjo, K. et al. Integrated analysis of genetic and loci. Cell Stem Cell 9, 272–281 (2010).
lung cancer. The study found genetic predictors of epigenetic alterations reveals CpG island methylator 146. Rock, J. R. et al. Multiple stromal populations
therapy response and provided a model for future phenotype associated with distinct clinical characters contribute to pulmonary fibrosis without evidence for
co-clinical trials aimed at accelerating the pace of of lung adenocarcinoma. Carcinogenesis 33, epithelial to mesenchymal transition. Proc. Natl Acad.
novel therapeutic development. 1277–1285 (2012). Sci. USA 108, E1475–E1483 (2011).
99. Engelman, J. A. et al. Effective use of PI3K and MEK 125. Chen, Z. et al. Inhibition of ALK, PI3K/MEK, and 147. McQualter, J. L., Yuen, K., Williams, B. &
inhibitors to treat mutant Kras G12D and PIK3CA HSP90 in murine lung adenocarcinoma induced by Bertoncello, I. Evidence of an epithelial stem/
H1047R murine lung cancers. Nature Med. 14, EML4‑ALK fusion oncogene. Cancer Res. 70, progenitor cell hierarchy in the adult mouse lung.
1351–1356 (2008). 9827–9836 (2010). Proc. Natl Acad. Sci. USA 107, 1414–1419 (2010).
100. Janne, P. A. et al. Selumetinib plus docetaxel for 126. Ji, H. et al. The impact of human EGFR kinase domain 148. Hegab, A. E. et al. Isolation and in vitro
KRAS-mutant advanced non-small-cell lung cancer: a mutations on lung tumorigenesis and in vivo characterization of basal and submucosal gland duct
randomised, multicentre, placebo-controlled, phase 2 sensitivity to EGFR-targeted therapies. Cancer Cell 9, stem/progenitor cells from human proximal airways.
study. Lancet Oncol. 14, 38–47 (2013). 485–495 (2006). Stem Cells Translat. Med. 1, 719–724 (2012).
101. Lim, S. M. et al. Therapeutic targeting of oncogenic 127. Chen, Z. et al. Co‑clinical trials demonstrate superiority 149. Kajstura, J. et al. Evidence for human lung stem cells.
K‑Ras by a covalent catalytic site inhibitor. Angew. of crizotinib to chemotherapy in ALK-rearranged non- New Engl. J. Med. 364, 1795–1806 (2011).
Chem. Int. Ed Engl. 53, 199–204 (2014). small cell lung cancer and predict strategies to overcome 150. Marek, L. et al. Fibroblast growth factor (FGF) and
102. Ostrem, J. M., Peters, U., Sos, M. L., Wells, J. A. & resistance. Clin. Cancer Res. 20, 1204–1211 (2014). FGF receptor-mediated autocrine signaling in non-
Shokat, K. M. K‑RasG12C inhibitors allosterically control 128. Jackson, E. L. et al. The Differential effects of mutant small-cell lung cancer cells. Mol. Pharmacol. 75,
GTP affinity and effector interactions. Nature 503, p53 alleles on advanced murine lung cancer. Cancer 196–207 (2009).
548–551 (2013). Res. 65, 10280–10288 (2005). 151. Liao, R. G. et al. Inhibitor-sensitive FGFR2 and FGFR3
103. Bass, A. J. et al. SOX2 is an amplified lineage-survival 129. Oliver, T. G. et al. Chronic cisplatin treatment mutations in lung squamous cell carcinoma. Cancer
oncogene in lung and esophageal squamous cell promotes enhanced damage repair and tumor Res. 73, 5195–5205 (2013).
carcinomas. Nature Genet. 41, 1238–1242 (2009). progression in a mouse model of lung cancer. Genes 152. Xu, L. et al. Combined EGFR/MET or EGFR/HSP90
104. Iwakawa, R. et al. MYC amplification as a prognostic Dev. 24, 837–852 (2010). inhibition is effective in the treatment of lung cancers
marker of early-stage lung adenocarcinoma identified 130. Blasco, R. B. et al. c‑Raf, but not B‑Raf, is essential for codriven by mutant EGFR containing T790M and MET.
by whole genome copy number analysis. Clin. Cancer development of K‑Ras oncogene-driven non-small cell Cancer Res. 72, 3302–3311 (2012).
Res. 17, 1481–1489 (2011). lung carcinoma. Cancer Cell 19, 652–663 (2011). 153. Davies, K. D. et al. Identifying and targeting ROS1
105. Lin, C. Y. et al. Transcriptional amplification in tumor 131. Puyol, M. et al. A synthetic lethal interaction between gene fusions in non-small cell lung cancer. Clin. Cancer
cells with elevated c‑Myc. Cell 151, 56–67 (2012). K‑Ras oncogenes and Cdk4 unveils a therapeutic Res. 18, 4570–4579 (2012).
106. Engelman, J. A. & Janne, P. A. Mechanisms of acquired strategy for non-small cell lung carcinoma. Cancer Cell 154. Takeuchi, K. et al. RET, ROS1 and ALK fusions in lung
resistance to epidermal growth factor receptor 18, 63–73 (2010). cancer. Nature Med. 18, 378–381 (2012).
tyrosine kinase inhibitors in non-small cell lung cancer. 132. Savino, M. et al. The action mechanism of the Myc 155. Wang, S. E. et al. HER2 kinase domain mutation
Clin. Cancer Res. 14, 2895–2899 (2008). inhibitor termed Omomyc may give clues on how to results in constitutive phosphorylation and activation
107. Grosso, J. F. & Jure-Kunkel, M. N. CTLA‑4 blockade in target Myc for cancer therapy. PLoS ONE 6, e22284 of HER2 and EGFR and resistance to EGFR tyrosine
tumor models: an overview of preclinical and (2011). kinase inhibitors. Cancer Cell 10, 25–38 (2006).
translational research. Cancer Immun. 13, 5 (2013). 133. Soucek, L. et al. Modelling Myc inhibition as a cancer 156. McDermott, U. et al. Ligand-dependent platelet-
108. Lee, D. W., Barrett, D. M., Mackall, C., Orentas, R. & therapy. Nature 455, 679–683 (2008). derived growth factor receptor (PDGFR)-α activation
Grupp, S. A. The future is now: chimeric antigen 134. Soucek, L. et al. Inhibition of Myc family proteins sensitizes rare lung cancer and sarcoma cells to
receptors as new targeted therapies for childhood eradicates KRas-driven lung cancer in mice. Genes PDGFR kinase inhibitors. Cancer Res. 69,
cancer. Clin. Cancer Res. 18, 2780–2790 (2012). Dev. 27, 504–513 (2013). 3937–3946 (2009).
NATURE REVIEWS | CANCER VOLUME 14 | AUGUST 2014 | 545
© 2014 Macmillan Publishers Limited. All rights reserved
REVIEWS
157. Jackson, E. L. et al. Analysis of lung tumor initiation 165. Issaeva, I. et al. Knockdown of ALR (MLL2) reveals 173. Mitsudomi, T., Hamajima, N., Ogawa, M. &
and progression using conditional expression of ALR target genes and leads to alterations in cell Takahashi, T. Prognostic significance of p53
oncogenic K‑ras. Genes Dev. 15, 3243–3248 (2001). adhesion and growth. Mol. Cell. Biol. 27, alterations in patients with non-small cell lung cancer:
GEMMs of lung cancer have been developed largely 1889–1903 (2007). a meta-analysis. Clin. Cancer Res. 6, 4055–4063
based on this prototypical study, in which the 166. Takawa, M. et al. Validation of the histone (2000).
Cre-Lox system was used to induce oncogenic Kras methyltransferase EZH2 as a therapeutic target for 174. Sanchez-Cespedes, M. et al. Inactivation of LKB1/
expression specifically in the lung through various types of human cancer and as a prognostic STK11 is a common event in adenocarcinomas of the
Adeno-Cre intranasal instillation. marker. Cancer Sci. 102, 1298–1305 (2011). lung. Cancer Res. 62, 3659–3662 (2002).
158. Mascaux, C. et al. The role of RAS oncogene in 167. Yang, H. et al. Tumor development is associated with 175. Iwanaga, K. et al. Pten inactivation accelerates
survival of patients with lung cancer: a systematic decrease of TET gene expression and 5‑methylcytosine oncogenic K‑ras-initiated tumorigenesis in a mouse
review of the literature with meta-analysis. Br. hydroxylation. Oncogene 32, 663–669 (2013). model of lung cancer. Cancer Res. 68, 1119–1127
J. Cancer 92, 131–139 (2005). 168. Gao, Q. et al. Deletion of the de novo DNA (2008).
159. De Raedt, T. et al. Exploiting cancer cell vulnerabilities methyltransferase Dnmt3a promotes lung tumor 176. Soria, J. C. et al. Lack of PTEN expression in non-
to develop a combination therapy for ras-driven progression. Proc. Natl Acad. Sci. USA 108, small cell lung cancer could be related to promoter
tumors. Cancer Cell 20, 400–413 (2011). 18061–18066 (2011). methylation. Clin. Cancer Res. 8, 1178–1184
160. Paik, P. K. et al. Clinical characteristics of patients with 169. Ohta, T. et al. Loss of Keap1 function activates Nrf2 (2002).
lung adenocarcinomas harboring BRAF mutations. and provides advantages for lung cancer cell growth.
J. Clin. Oncol. 29, 2046–2051 (2011). Cancer Res. 68, 1303–1309 (2008). Acknowledgements
161. Kawano, O. et al. PIK3CA mutation status in Japanese 170. Singh, A. et al. Dysfunctional KEAP1‑NRF2 interaction The authors thank United Against Lung Cancer, Thoracic
lung cancer patients. Lung Cancer 54, 209–215 in non-small-cell lung cancer. PLoS Med. 3, e420 Foundation, Bonnie J Addario Lung Cancer Foundation,
(2006). (2006). Claudia Adams Barr Program For Basic Cancer Research,
162. Marks, J. L. et al. Novel MEK1 mutation identified by 171. Wang, Y., Zhang, Z., Kastens, E., Lubet, R. A. & grant numbers CA122794, CA166480, CA163896,
mutational analysis of epidermal growth factor receptor You, M. Mice with alterations in both p53 and Ink4a/ CA154303, CA120964 CA140594.
signaling pathway genes in lung adenocarcinoma. Arf display a striking increase in lung tumor multiplicity
Cancer Res. 68, 5524–5528 (2008). and progression: differential chemopreventive effect of Competing interests statement
163. Licciulli, S. et al. Notch1 is required for Kras-induced budesonide in wild-type and mutant A/J mice. Cancer The authors declare no competing interests.
lung adenocarcinoma and controls tumor cell survival Res. 63, 4389–4395 (2003).
via p53. Cancer Res. 73, 5974–5984 (2013). 172. Lou-Qian, Z. et al. The prognostic value of epigenetic DATABASES
164. Westhoff, B. et al. Alterations of the Notch pathway in silencing of p16 gene in NSCLC patients: a systematic My Cancer Genome: http://www.mycancergenome.org/
lung cancer. Proc. Natl Acad. Sci. USA 106, review and meta-analysis. PLoS ONE 8, e54970 ALL LINKS ARE ACTIVE IN THE ONLINE PDF
22293–22298 (2009). (2013).
546 | AUGUST 2014 | VOLUME 14 www.nature.com/reviews/cancer
© 2014 Macmillan Publishers Limited. All rights reserved
You might also like
- NAD (P) H Quinone Oxidoreductase 1 (NQO1) in The Sensitivity and Resistance To Antitumor QuinonesDocument8 pagesNAD (P) H Quinone Oxidoreductase 1 (NQO1) in The Sensitivity and Resistance To Antitumor QuinonesXyzNo ratings yet
- Nat Protoc 2012 ZhangDocument18 pagesNat Protoc 2012 ZhangXyzNo ratings yet
- Anthony Horowitz - Alex Rider Short Story - UndergroundDocument3 pagesAnthony Horowitz - Alex Rider Short Story - UndergroundXyzNo ratings yet
- Medical Hierarchy - NEJMDocument4 pagesMedical Hierarchy - NEJMXyzNo ratings yet
- Referral Cheat Sheet: Before You CallDocument2 pagesReferral Cheat Sheet: Before You CallXyz100% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5796)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Amy E. Zanne, Mark Westoby, Daniel S. Falster, David D. Ackerly, Scott R. Loarie, Sarah E. J. Arnold, and David A. CoomesDocument9 pagesAmy E. Zanne, Mark Westoby, Daniel S. Falster, David D. Ackerly, Scott R. Loarie, Sarah E. J. Arnold, and David A. CoomesRandu Pinandito NugrohoNo ratings yet
- Human Digestive System - QuizDocument11 pagesHuman Digestive System - QuizSher SherwinNo ratings yet
- Multiple Choice Questions On MycorrhizaDocument10 pagesMultiple Choice Questions On Mycorrhizaamandajwarner58No ratings yet
- Molecular Genetics: Test Yourself 20.1 (Page 389) 1Document2 pagesMolecular Genetics: Test Yourself 20.1 (Page 389) 1leeNo ratings yet
- A Guidebook To Plant ScreeningDocument19 pagesA Guidebook To Plant ScreeningRenzo Fernandez33% (6)
- Performance of Non-Invasive Prenatal Testing For Foetal Chromosomal Abnormalities in 1048 Twin PregnanciesDocument7 pagesPerformance of Non-Invasive Prenatal Testing For Foetal Chromosomal Abnormalities in 1048 Twin PregnanciesMariana HernandezNo ratings yet
- Biofilm-Inactivating Activity of Silver Nanoparticles - A Comparison With Silver IonsDocument6 pagesBiofilm-Inactivating Activity of Silver Nanoparticles - A Comparison With Silver IonsFabio SenaNo ratings yet
- Rajiv Gandhi University of Health Sciences, Karnataka, Bangalore Proforma For Registration of Subjects For DissertationDocument9 pagesRajiv Gandhi University of Health Sciences, Karnataka, Bangalore Proforma For Registration of Subjects For DissertationTiara Febriani NurantiNo ratings yet
- An IntroductionDocument21 pagesAn IntroductionOmar GardiNo ratings yet
- Importance of Dna IsolationDocument4 pagesImportance of Dna Isolationapi-291218692No ratings yet
- 4hb1 01 Rms 20240125Document11 pages4hb1 01 Rms 20240125Raiyad RezaNo ratings yet
- 3 Chapter - Test - B PDFDocument4 pages3 Chapter - Test - B PDF우상범No ratings yet
- Study of Cancer Investigatory ProjectDocument15 pagesStudy of Cancer Investigatory ProjectRavi KNo ratings yet
- Drosophila Melanogaster As A Potential Model OrganismDocument16 pagesDrosophila Melanogaster As A Potential Model OrganismGerardo SotoNo ratings yet
- Second Quarter Earth and Life SciencesDocument5 pagesSecond Quarter Earth and Life SciencesRey Mark QueanoNo ratings yet
- (I Gordon) Reproductive Technologies in Farm Anima (BookFi) PDFDocument347 pages(I Gordon) Reproductive Technologies in Farm Anima (BookFi) PDFskumarNo ratings yet
- D0679sci Part2 QR 2020 FinalDocument21 pagesD0679sci Part2 QR 2020 FinalEND GAMINGNo ratings yet
- Dafpus ProposalDocument3 pagesDafpus ProposalJantikaNo ratings yet
- Q3-W4B-Protein Synthesis (By Group)Document5 pagesQ3-W4B-Protein Synthesis (By Group)Catherine CantadaNo ratings yet
- National Symposium PosterDocument1 pageNational Symposium PosterkalyankpyNo ratings yet
- Gastrointestinal Hormones: A Mini-Review: European Journal Pharmaceutical and Medical Research April 2022Document6 pagesGastrointestinal Hormones: A Mini-Review: European Journal Pharmaceutical and Medical Research April 2022Yared gebremedhinNo ratings yet
- Carbon - The Element of Life Bio Draft FinalDocument51 pagesCarbon - The Element of Life Bio Draft Finalyalavarthi vishalNo ratings yet
- TIGP Admissions Announcement For 2013Document6 pagesTIGP Admissions Announcement For 2013WinataWahyuFajarNo ratings yet
- Ecology Vocabulary WordsDocument2 pagesEcology Vocabulary Wordspatru177No ratings yet
- SCIENCE-9-Q1-Week1-MELC05-ASP-Calabucal, Ma. Belinda - Docx (2) - Ma. BELINDA CALABUCALDocument9 pagesSCIENCE-9-Q1-Week1-MELC05-ASP-Calabucal, Ma. Belinda - Docx (2) - Ma. BELINDA CALABUCALNOVA LESLIE AGAPAYNo ratings yet
- Cambridge Assessment International Education: Agriculture 5038/12 October/November 2017Document24 pagesCambridge Assessment International Education: Agriculture 5038/12 October/November 2017Ahmed NaserNo ratings yet
- Z-Q. Zhang, 2011, Animal Biodiversity An Outline of Higher-Level Classification and Survey of Taxonomic RichnessDocument23 pagesZ-Q. Zhang, 2011, Animal Biodiversity An Outline of Higher-Level Classification and Survey of Taxonomic Richnessdavid vergara morenoNo ratings yet
- Analisis Metabolit Sekunder Kultur Pucuk, Kalus, Dan Tanaman LapangDocument10 pagesAnalisis Metabolit Sekunder Kultur Pucuk, Kalus, Dan Tanaman LapangNabilla PrastikadewiNo ratings yet
- Journal of Experimental and Integrative Medicine: Channa Striatus Capsules Induces Cytokine Conversion inDocument6 pagesJournal of Experimental and Integrative Medicine: Channa Striatus Capsules Induces Cytokine Conversion inPT. Royal Medicalink PharmalabNo ratings yet
- Cell Cycle Regulators: Namrata Sengupta Mds 1 Year Oral Pathology & MicrobiologyDocument33 pagesCell Cycle Regulators: Namrata Sengupta Mds 1 Year Oral Pathology & MicrobiologyMadhura ShekatkarNo ratings yet