Professional Documents
Culture Documents
John C. Rosenbek, Margaret !.. Lemme, Margery B. Ahern, Elizabeth H. Harris, and Robert T. Wertz
Uploaded by
Gabriel MoralesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
John C. Rosenbek, Margaret !.. Lemme, Margery B. Ahern, Elizabeth H. Harris, and Robert T. Wertz
Uploaded by
Gabriel MoralesCopyright:
Available Formats
A TREATMENT FOR APRAXIA OF SPEECH IN ADULTS
John C. Rosenbek, Margaret !.. Lemme, Margery B. Ahern,
Elizabeth H. Harris, and Robert T. Wertz
University o[ Colorado, Boulder, Colorado
Principles of therapy for the apraxic adult are discussed. An eight-step task con-
tinuum, consistent with these principles, to restore volitional-purposive communi-
cation is presented. Three case histories of patients with severe apraxia of speech
and mild-to-moderate aphasia demonstrate the application of the principle and the
procedure.
This article discusses therapeutic principles and procedures for treating
apraxia of speech in adults and demonstrates in three case histories how these
may be applied. T h e sources of these principles and procedures are many and
varied and include previous clinical reports (Nathan, 1947; Goldstein, 1948;
Johns, 1970), experimental research (Shankweiler and Harris, 1966; LaPointe,
1969; Johns and Darley, 1970; Larimore, I970; Trost, 1970; Deal and Darley,
1972), and our clinical work with a variety of apraxic patients.
T h e very fact that an apraxic adult is brain-injured generates certain princi-
ples for therapy. Some of these are similar, if not identical, to those which
have been emphasized for the aphasic adult. This is a fortunate economy so
long as we continually remember that the specific methodology is quite differ-
ent. T h e essential principles are these: (1) All therapy activities should be
organized according to task continua so that the patient does not struggle and
so that he works at a high level of success during each session. (2) T h e brain
injury in most instances will require that the patient take longer and work
harder at regaining or learning lost articulatory skills, so the clinician should
plan for intensive and extensive drill. (3) Because the patient is an adult with
a history of normal speech and language comprehension/use, mastery of mean-
ingful and useful verbal communication should be emphasized as early as
possible. (4) Efficient self-correction must be encouraged, although gentle re-
minders will be sufficient for those patients who appear to begin self-correction
without therapy. (5) T h e brain injury may have imposed physiological limits
on the patient's speech production mechanism. If so, the clinician should teach
compensatory movements such as the intrusive schwa, equal and even stress,
judicious use of the pause, and continuant and vowel prolongation.
462
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
ROSENBEK ET AL.. TREATMENT FOR APRAXIA OF SPEECH 463
Apraxia of speech is a nonlinguistic sensorimotor disorder of articulation
characterized by impaired "capacity to program the positioning of speech
musculature and the sequencing of muscle movements for the volitional pro-
duction of phonemes" (Darley, 1969). Therefore, therapy should (1) concen-
trate on the disordered articulation and, hence, be different from the language
stimulation and auditory and visual processing therapies appropriate to the
aphasias; (2) emphasize the regaining of ttdequate points of articdlatibn and
the sequencing of articulatory gestures; and (3) provide conditions such that
the patient can advance from limited, automatic-reactive speech to appropri-
ate, volitional-purposive communication.
In general, a variety of phonetic conditions affect the apraxic adult's articu-
latory accuracy in predictable ways:
manner of articulation-fricatives, atfricatives,.ond cqnsotlant clusters are more likely
to be in error than vowels, nasals, and plos|ves;
speech-sound position-errors are more likely on initial than final speech sounds;
difficulty of initial speech sound-a word is most likely td be in error if it begins with
a fricative, affricative, or consonant cluster; ~
distance between successive speech sounds.the likelihood of error increases as the
distance between successive points of articulation hrithill an utter~hde in.eases;
word length--errors increase as words increase in length;
word frequency-errors more likely on rare than on common words.
Therapeutic principles derived from these phonetic conditions are several:
(1) A hierarchial arrangement of speech sounds and clusters as a basis for
therapy is advisable. Therapy can begin with the easiest speech sounds and
advance systematically through more difficult ones. (2) As sound sequencing
becomes possible, stimuli should be selected so that the distance between
points of articulation of successive sounds increases systematically. (3) Careful
selection of stimuli with regard to initial sound will increase response ade-
quacy and, therefore, should be considered in preparing therapeutic materials.
(4) T h e length of stimulus items should also increase systematically. Begin
with short reduplicating utterances, depending on the severity of the patient's
apraxia, and increase stimulus length. Of course, work on several response
lengths may go on simultaneously. (5) When real words are used, these should
be selected from a list of words with a high frequency of occurrence. Response
length, speech-sound difficulty, and distance between successive sounds, how-
ever, are more potent influences on articulatory accuracy and should be more
carefully controlled. Finally, articulatory accuracy in apraxia of speech is
influenced by the mode of stimulus. Auditory-visual stimulation is better than
auditory or visual alone. (Visual in this instance refers to watching the clini-
cian as he speaks.) Useful as well are written stimuli for many apraxic patients,
especially those who are relatively free of a coexisting aphasia. In general,
apraxic patients achieve greater articulatory accuracy, at least at the single-
sound level, if they are encouraged to monitor their own speech in a mirror.
Principles of therapy, then, are four: (1) T h e integral stimulation method
("Listen to me and watch me") is parsimonious, effective, and should be tried
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
464 JOURNAL OF SPEECH AND HEARING DISORDERS - - XXXVIII, 4
first. (2) As therapy progresses and the patient becomes more able to produce
volitional, nonimitative speech, first auditory, then visual cues should be faded
gradually. (3) Developing a strong visual memory of correct production should
be emphasized from "day one." T h e mirror and written word are useful to
this process. (4) Only after the integral stimulation method has failed with a
patient or with a particular speech sound should the clinician move to other
methods. Useful alternatives are phonetic placement, phonetic derivation, and
the "key word" method.
A TASK CONTINUUM
An eight-step task continuum generated by certain of the foregoing princi-
ples was constructed. T h e continuum was then employed to establish pre-
dictable, volitional control of selected utterances in three severely apraxic
adults with mild-to-moderate aphasia. T h e eight-step continuum, its applica-
tion to the three patients, and an evaluation of its efficacy are next presented.
Step 1. Integral stimulation--"Watch me" (visual [vl]); "Listen to me"
(auditory [a]) and simultaneous production (client and clinician produce the
utterance at the same time). T h e clinician urges the client to attend carefully
to the auditory and especially to the visual cues of correct production as they
say the utterance together.
Step 2. Integral stimulation (vl, a) and delayed production (client imitates
clinician after a delay) with visual (vl) cue. T h e clinician provides a model to
which the client attends; then, while the clinician mimes or repeats the utter-
ance without sound, the client attempts the utterance aloud. In other words,
the simultaneous auditory cues are faded while the visual remain.
Step 3. Integral stimulation (vl, a) and delayed production with no visual
(v~) cue. This is the traditional 'TII say it first, and you say it after me" ap-
proach. No simultaneous cues are provided by the clinician.
Step 4. Integral stimulation and successive productions without intervening
stimulation and without auditory (a) or visual (vl) cues. After the clinician
produces the utterance once, the client is required to produce it several times
consecutively without cues of any kind.
Step 5. Written stimuli (v2) and simultaneous production.
Step 6. Written stimuli (w) and delayed production.
In Step 5, the client reads the target utterance from cards or from the black-
board, and i n Step 6 these cues are provided him but he doesn't attempt the
utterance until the written stimuli have been removed.
Step 7. Appropriate utterance elicited by question. The imitative model is
abandoned. T h e clinician now provides the conditions so that the target ut-
terance is used volitionally as the appropriate response to a question.
Step 8. Appropriate response in a role-playing situation. T h e clinician, staff,
and friends assume roles appropriate to the target utterance and the client
responds appropriately.
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
ROSENBEK El" AL.: TREATMENT FOR APRAXIA OF SPEECH 465
CLINICAL EVALUATION OF PROCEDURES
T o evaluate the eight-step continuum's efficacy in apraxia therapeutics, we
selected three adults with severe apraxia of speech of longer than one year's
duration and used it to teach them volitional control of five utterances. T h e
utterances varied in length from one to seven words. Each was functional for
the individual patient and not in his volitional repertoire at the project's
initiation. No further attempt was made to equate utterances beyond the con-
dition that no utterance be more than seven words long and contain no word
of more than three syllables. Each subject's responses were scored using a
slightly modified version of the Porch Index of Communicative Ability (Porch,
1971) 16-point multidimensional scoring system. Criterion performance for
each step was 80% correct in 20 trials. Because our subjects had suffered brain
injury which had imposed limits on their speech production mechanisms, the
judgment of maximum correctness was relative for each subject. In all cases,
terminal utterances were intelligible. A variable-ratio reinforcement schedule
of verbal responses was maintained throughout the project.
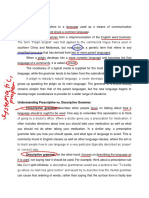
Figure 1 shows the percentage of total responses that each patient produced
at each of the eight steps as he moved from imitative (Step 1) productions to
volitional, purposive control (Step 8). T h e data are cumulative. For example,
of the total number of responses produced by Case 1, 32% were produced in
response to Step 1 procedures, 21% in response to Step 2 procedures, and so
on.
Case 1
JR, a 57-year-old male with eight years of education, suffered a left cerebral
infarct with probable occlusion of the left, middle cerebral artery in 1971. His
medical history revealed right hemiparesis, chronic undifferentiated schizo-
phrenia, and long periods of unemployment. He was seen in physical therapy
for three months and dismissed with good return of function in the right
extremities. Before the beginning of this project, he was seen by the speech
pathology staff for approximately 12 months.
At the initiation of this project, J g demonstrated moderate aphasia charac-
terized by word-finding, memory, and auditory-processing deficits; his writing
and reading were also impaired. He demonstrated no jargon, confusion, or
general intellectual deficit. He was seen for 11 45-minute sessions during a
period of six weeks. His target utterances were introduced in the following
order:
1. It is time to go (Session 1).
2. My name is J K.. (Session 1).
3. The weather is beautiful (Session 3).
4. I can not do it now (Session 8).
5. I saw something funny yesterday (Session 8).
Figure 1 presents the percentage of responses elicited at each of eight steps
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
466 JOURNAL OF SPEECH A N D HEARING DISORDERS -- XXXVlll, 4
32, I I i ] ! 1 I
30
, J CASE 1 (JR)
28 ........ CASE 2 (MF)
...... CASE 3 (RW)
26
24
"22
uJ
18
0 .... -,
i , Figure I. Percentage of total
16
responses required to reach
/I \, ,\/~ criterion at each of eight
14 / steps in the task continuum.
, \
%
', / ',,
12
iI ' "1 I,
10
II
o , .J , I I I I ~, I. I J
1 2 3 4 5 6 7 8
STEP
for the four utterances reaching the criterion of predictable, volitional con-
trol. JR's "correct" responses were intelligible but delayed and distorted. In
the PICA (Porch, 1971) system his responses were scored as 13s and 14s.
Therapy for the fifth utterance was interrupted at Step 5 when the clinician
was assigned to another hospital. Progress on this last utterance through five
steps was similar to that for the other four. The greatest number of responses
(32%) was elicited by Step 1, the least, 1%, by Step 8 (Figure 1). The percen-
tage of responses elicited imitatively at Steps 1 through 4 (78%) is substan-
tially greater than the percentage elicited by reading, questioning, and role-
playing (22%). Utterances tend to reach criterion somewhat more quickly as
one advances through the steps.
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
ROSENBEK ET AL.: TREATMENT FOR APRAXIA OF 5PEECH 467
An essentially equal number of responses was elicited at Steps 2 and 3, and
a limited number of responses was elicited at Step 4 (Figure 1). T h e number
of responses at Step 3 is increased for two reasons. T h e patient had not pre-
viously experienced this therapeutic approach and was reluctant to attend to
Step 2 visual cues. When he failed to attend to the visual even though the
clinician provided it, his utterances were considered to be in response to Step
3 rather than Step 2 stimulation. In addition, Step 4, requiring him to respond
several times without intervening cues from his clinician, precipitated con-
siderable inconsistency of response and obvious frustration. Because we wanted
the patient to experience high levels of success, in early sessions JR's clinician
dropped back to Step 3, hence increasing the number of responses at that
step. In later sessions, Step 4 was essentially ignored, reducing the absolute
number of responses, and therapy advanced to Step 5.
Once the therapy paradigm was established with one utterance, subsequent
utterances appeared to move through the steps more rapidly. For example,
utterance one and utterance four are similar in that the words are short and
of high frequency, most of the sounds are visible, and most of the combina-
tions require minimal excursions for proper points of articulation. Utterance
four, which was introduced after the paradigm was well established, required
one-fourth the number of trials to stabilize at criteriola that utterance One had
taken. Utterances which involved less visible, more complex sounds, greater
length, or greater excursions between points of articulation (utterances three
and five) required more time at each step than utterance four, but less than
utterances one and two. It was not necessary to pass systematically through
all steps for utterance three. J R was able to move directly from Step 3 to
Step 7.
T h e word is appeared in three of the target utterances. By the fourth ses-
sion, is was at criterion in utterances one and two, but not in utterance three,
although all three had been drilled equally often. This lack of generalization
may be explicable on the basis of phonetic environment or as an example of
what Winitz (1969) has called phonological conditioning.
Case 2
MF is a 59-year-old female with 12 years of education. She exhibited pro-
found verbal and nonverbal apraxia and moderate aphasia across all modali-
ties secondary to a cerebrovascular accident at age 51. Her writing was least
impaired and her auditory processing was Sufficient for most complex tasks of
daily living. She had first received speech therapy one year after the onset of
the apraxia, for seven months. After almost five years, she resumed therapy.
At that time, her automatic speech consisted of 10 words. She communicated
primarily by gesturing or writing. Her imitative speech consisted of [a].
Therapy has continued, three to five days ~i week, to the time of this writing.
Twenty-six consecutive therapy sessions were included in this project. T h e
45-minute sessions t o o k place approximately every two days for two months.
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
468 JOURNAL OF SPEECH AND HEARING DISORDERS -- XXXVIII, 4
Because of the severity of her apraxia, this subject was taught five single-word
utterances, each consisting of sounds she could imitate. T h e target utterances
and the sessions in which they were introduced follow:
1. out (Session 1)
2. more (Session S)
3. art (Session 14)
4. home (Session 10)
5. this (Session 19)
"Correct" for MF meant delayed or distorted responses that were nonetheless
intelligible. Reinforcement was gestural (nodding and patting her hand) as
well as verbal for Steps 1 through 4, after which almost no reinforcement was
necessary.
Figure 1 shows the percentage of responses necessary to reach criterion for
the five single-word utterances at each of the eight steps. T h e greatest percen-
tage of responses was elicited at Step 1 (29%). MF's clinician elicited 76% of
the total responses with Steps 1 through 4 and 24% with Steps 6 through 8.
T h e clear implication for Case 2, as for Case 1, is that criterion performance
was more rapidly achieved as therapy progressed through the continuum.
MF was generally unable to begin a session at the level attained in the
previous session. For four of five utterances, the subject generally began each
session two steps below the level achieved in the previous session. For three of
those utterances, it was necessary to begin each session at Step 1 until criterion
for Step 3 was reached during two consecutive sessions. T h e implication is that
Steps 1 through 3 must be "overworked" for success on subsequent steps to
be attained.
Two supplemental steps not shown in Figure 1 were included for this sub-
ject. They functioned as a transition between Step 4 and Step 5 (v2 stimulus
only). T h e first (T~) required simultaneous production with the clinician (a),
while looking at the written word (v2) printed on a card and held for her by
the clinician. T h e second (T~) required delayed production following auditory
stimulation from the clinician (a), but simultaneous with looking at the writ-
ten word (v~).
Step 4 was very difficult for MF as it was for Case 1 and was bypassed for
some utterances if success was not immediately forthcoming. It appears that
Step 4 is actually a harder task than some of the higher-numbered steps. Ap-
parently the auditory, tactile-kinesthetic stimulation of the subject's own pro-
duction (as obtained in Step 4) is insufficient to facilitate another production.
T h e number of responses at each step was essentially the same for four of
five utterances. Utterance 5 (this) was the most difficult for MF and required
more responses at each step. Overlapping movements of a single articulator
may have accounted for this difficulty.
Case 3
RW, a 59-year-old male with 12 years of education, suffered a stroke in
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
ROSENBEK ET AL.. TREATMENT FOR APRAXIA OF SPEECH 469
1966 which left him with a dense right hemiparesis. Two months of twice
daily speech therapy began soon after his stroke. After three more months of
twice weekly sessions, the therapy was discontinued as no progress was being
made. Periodic therapy interrupted by illness, personal affairs, and travel be-
gan at the University of Colorado Speech and Hearing Clinic in 1970.
RW's speech diagnosis at the beginning of this project was moderate aphasia
across all modalities, with a severe deficit in writing; mild dysarthria; and
severe oral, nonverbal apraxia and apraxia of speech. He did not exhibit
jargon, confusion, or general intellectual deficit. His target utterances and
the sessions in which they were introduced were as follows:
1. I'm going to a Bronco football game (Session 1).
2. I want a touchdown (Session 1).
3. It's time to go (Session 1).
4. They might have five wins (Session 1).
5. I wish I had therapy every day (Session 1).
T h e utterances were introduced simultaneously and an 80% "correct" cri-
terion was maintained through all 21 sessions. "Correct" for R W meant that
an utterance was intelligible. In PICA (Porch 1971) scoring we accepted a 7,
13, 14 profile as correct-in other words, utteranceg which were intelligible but
contained articulation errors, delayed utterances, and distorted utterances.
Physiological limitations made greater expectations unrealistic.
Figure 1 presents the percentage of total trials spent at each of eight steps
for the five target utterances. Steps 1 through 4 were used to elicit only 47%
of the total responses. Step 4 (several consecutive repetitions of the target ut-
terance without intervening cues from the clinician) and Step 5 (reading) were
employed to elicit 34% of the total number of responses. RW's clinician
tended to use all steps more equally than did the other two clinicians. It is as
if Steps 4 through 8 especially were independent exercises.
R W had problems with carry-over from session to session. An utterance
advanced to Step 8 at the end of one session would inevitably have to be
elicited with the Step 4 procedure at the beginning of the next session. This
particular situation is in part responsible for the high percentage of total trials
spent at Step 4, and may result from unavoidably long periods between thera-
py sessions.
His performance demonstrates the power of motivation. T h e utterance he
most wanted to acquire was "I want a touchdown." This utterance went
rapidly to Steps 7 and 8 adequacy. T h e high-percentages of trials at these two
steps, 15% for Step 7 and 10% for Step 8, are inflated by his expressed desire
to work on this utterance and because the clinician used his good performance
to motivate him to attempt the others. Performance at Steps 7 and 8 for the
other utterances could only be maintained with minimal vl cues, a condition
he could never quite overcome.
Carry-over was evident for three of the five utterances for Case 1 three
months after the termination of therapy. Carry-over for Case 2 in role-playing
situations was successful for four utterances three months after the termination
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
470 JOURNAL OF SPEECH AND HEARING DISORDERS -- XXXVIII, 4
of the project. T h e fifth utterance (this) was the most difficult for MF through-
out therapy. Volitional production of this was correct 75% of the time in
role-playing situations. Case 3 continues in therapy and formal carry-over
testing was never completed.
DISCUSSION
The eight steps, with the exception of Step 4, appear to represent a legiti-
mate task continuum, as evidenced by the performance of Cases 1 and 2.
They achieved volitional control of target utterances with a minimum of
struggle and frustration. In general, fewer responses were required to reach
criterion at each step.
Step 4 was difficult for both these patients, and facilitation in the form of a
return to previous steps (Case 1) and creation of additional steps (Case 2) were
necessary to complete the continuum. It may well be that increasing the
amount of drill at Steps 1 through 3 or stricter criteria at these steps would
reduce patients' difficulty at Step 4. Or Step 4 might be omitted or replaced.
Logical candidates for substitutes are the two steps created for Case 2, simul-
taneous auditory and reading (v2) cues, and simultaneous and delayed pro-
duction from a (w) cue. T h e Language Master could easily be employed at
these steps, making this program more usable for home practice. These inter-
pretations and alternations are being evaluated.
T h e graph for Case 3, while it appears radically different from those of
Cases 1 and 2, does share some common features with them. T h e patient
reached criterion performance with progressively fewer trials across Steps 1,
2, and 3. Step 4 was difficult and required considerable repetition. It could be
that had a higher percentage of total trials been used at Steps 1, 2, and 3, this
patient's difficulty with Step 4 would also have been lessened.
We employed a variety of response facilitators in this project. Their inclu-
sion as steps along the continuum does not appear justified because of the
unduly burdensome and restrictive therapy outline which would have resulted.
Apraxic patients differ-in speech characteristics, in the severity of their
apraxia, and in the presence and severity of associated peripheral and central
deficits-to a degree that makes restrictive therapy outlines untenable. T h e
facilitators need to be mentioned, however, because our clinical experience
suggests they are additional flesh and blood for our therapy.
One set of response facilitators grows out of variations in the clinician's
presentation of stimuli. In general, stimuli were presented slowly, with pauses
between words or word groups, with prolongation of some consonants and
vowels, and with use of an intrusive schwa within consonant clusters. Parts of
utterances with which our patients were having particular difficulty were
produced with increased stress or with exaggerated articulatory gestures. Some
utterances were presented with a stereotyped, practically unchanging prosodic
pattern. These facilitators were useful when new utterances were first being
introduced.
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
ROSENBEK ET AL.: TREATMENT FOR APRAXlA OF SPEECH 471
With Case 1 we used phonetic placement techniques to teach adequate pro-
duction of [s] and [d3]. Ordinarily we would not introduce these two sounds
in early therapy sessions because of their difficulty for many apraxic adults,
JR included, but did so this time because the [s] appeared as part of an
utterance he wanted to learn and [d3] was the first sound in his name. A mirror
was necessary for Case 2's last utterance (this), possibly because of the diffi-
culty with overlapping movements of one articulator. T h e mirror is a useful
adjunct to apraxia therapy. We suspect its best use will be as a prerequisite or
companion to the technique of Steps 1 and 2.
Individual words in the target utterances for Cases 1 and 3 were not under
the same stimulus control. Rather than staying at an early step until all
components of an utterance were equally controlled, the clinicians made sev-
eral adjustments. These included cuing some sounds and not others and
accepting omissions, substitutions, or distortions if these did not adversely
affect the overall communication. Also, words were worked on independently,
employing the eight-step continuum, and then returned to the utterance. As a
general rule, it appears preferable to accept a variety of articulation errors
and even telegraphic utterances if failure to do so inordinately delays the
patient's use of meaningful, useful utterances.
Fortunately, for a variety of reasons, the clinician need not pass systematical-
ly through all steps nor employ all the facilitators with each patient. At the
single-sound level and, to a lesser extent, at the single-word level, Steps 7 and
8 are artificial or impossible. In other instances the patient may be able to
jump from Step 4 and Step 8; less likely are even larger jumps. This is often
the case when the patient is only mildly or moderately involved or when the
utterance is a simple one phonetically. It is also the case when response gen-
eralization occurs, as it does occasionally even with a severe patient, and he
begins to engage in effective, efficient, searching, and self-corrective behavior.
All these conditions which permit skipping of some steps should prompt the
clinician to probe systematically for the target response while progressing
through the steps.
It would be folly to expect that this approach can improve the speech of all
severely apraxic adults. Certainly the literature (for example, Sarno, Silver-
man, and Sands, 1970) urges us to be cautious in promising results, especially
to the severely affected patient. This continuum can, if intelligently employed,
help to restore some communicative ability to some severely apraxic patients.
This is a painfully long, grueling process and, if a patient has to pay, pro-
hibitively expensive. Continued refinement may yield a systematic home
program as a less expensive alternative. Refinement resulting from experi-
mentation and systematic clinical use may also provide a therapy approach
sufficiently well-defined that we can, as Darley (1972) urges, specify the therapy
and improve our ability to play the real game, which is to "restore the patient
to communicative efficiency" (p. 4).
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
472 JOURNAL OF SPEECH AND HEARING DISORDERS - - XXXVIII, 4
ACKNOWLEDGMENT
At the time of the research reported here, all the authors were affiliated with the University
of Colorado, Boulder. Margaret L. Lemme is now affiliated with the Department of Physical
Medicine and Rehabilitation at the University of Colorado Medical Center, in Denver; and
Robert T. Wertz is with the Veterans Administration Hospital in Albuquerque. Requests for
reprints should be addressed to John C. Rosenbek, Speech and Hearing Clinic, University of
Colorado, Boulder, Colorado, 80302, or to Robert T. Wertz, Speech Pathology and Audiology
Service, Veterans Administration Hospital, 2100 Ridgecrest Drive, Albuquerque, New Mexico
87108.
REFERENCES
BARLEY, F. L., The classification of output disturbances in neurologic communication dis-
orders. Paper presented in dual session on Aphasia: Input and output disturbances in
speech and language processing, at the Annual Convention of the American Speech and
Hearing Association, Chicago (1969).
DARLEY, F. L., The efficacy of language rehabilitation in aphasia. J. Speech Hearing Dis., 37,
3-21 (1972).
DEAL, J. L., and DARLEY, F. L., The influence of linguistic and situational variables on
phonemic accuracy in apraxia of speech. J. Speech Hearing Res., 15, 639-653 (1972).
GOLDSTEIN, K., Language and Language Disturbances. New York: Grune and Stratton (1948).
JOHNS, D. F., Treatment of apraxia of speech. Paper presented at the Annual Convention of
the American Speech and Hearing Association, New York (1970).
JOHNS, D. F., and DA~J~Y, F. L., Phonemic variability in apraxia of speech. ]. Speech Hearing
Res., 13, 556-583 (1970).
LAPmNTE, L. L., An investigation of isolated oral movements, oral motor sequencing abilities,
and articulation of brain-injured adults. Doctoral dissertation, Univ. of Colorado (1969).
LAtUMOtU~, H. W., Some verbal and non-verbal factors associated with apraxia of speech.
Doctoral dissertation, Univ. of Denver (1970).
NATHAN, P. W., Facial apraxia and apraxic dysarthria. Brain, 70, 449-478 (1947).
PORCH, B. E., Porch Index o/ Communicative Ability. Palo Alto, Calif.: Consulting Psycholo-
gists (1971).
SAtNO, M. T., SILVE~VIAN,M., and SANDS,E., Speech therapy and language recovery in severe
aphasia. J. Speech Hearing Res., 13, 607-623 (1970).
SHANKWEXLER,D., and HARRIS,K. S., An experimental approach to the problem of articulation
in aphasia. Cortex, 2, 272-292 (1966).
TROST, J. E., Patterns of articulatory deficits in patients with Broca's aphasia. Doctoral disser-
tation, Northwestern Univ. (1970).
WINITZ, H., Articulatory Acquisition and Behavior. New York: Appleton (1969).
Received April 9, 1973.
Accepted July 20, 1973.
Downloaded From: http://jshd.pubs.asha.org/ by a Western Michigan University User on 02/18/2016
Terms of Use: http://pubs.asha.org/ss/rights_and_permissions.aspx
You might also like
- Unit 15: Evaluation and TestingDocument12 pagesUnit 15: Evaluation and TestingDongjin LeeNo ratings yet
- Treatment of Wernicke'S Aphasia With Jargon: A Case StudyDocument11 pagesTreatment of Wernicke'S Aphasia With Jargon: A Case StudyIvanaNo ratings yet
- Phonology Exercises: Minimal Pairs Reveal ContrastsDocument7 pagesPhonology Exercises: Minimal Pairs Reveal Contrastsomar chNo ratings yet
- Voice TherapyDocument8 pagesVoice TherapyJoseph100% (1)
- Aphasia Therapy Guide: Impairment-Based TherapiesDocument33 pagesAphasia Therapy Guide: Impairment-Based TherapiesCarolina GudiñoNo ratings yet
- Voice Therapy Does Science Support The ArtDocument1 pageVoice Therapy Does Science Support The ArtEvelyn Bernardita Avello CuevasNo ratings yet
- Efficacy of Doctorvox On Mutational FalsettoDocument8 pagesEfficacy of Doctorvox On Mutational FalsettoANA CRISTINA MENDEZ DIAZNo ratings yet
- Voice TherapybookwebDocument23 pagesVoice TherapybookwebPola Constanza100% (1)
- " The Effectiveness of Verbal-Gestural Treatment On Verb Naming in Acute Inpatient Rehabilitation" Journal Article ReviewDocument6 pages" The Effectiveness of Verbal-Gestural Treatment On Verb Naming in Acute Inpatient Rehabilitation" Journal Article Reviewapi-709202309No ratings yet
- Aphasia Therapy GuideDocument4 pagesAphasia Therapy GuideDavid SugiartoNo ratings yet
- 2 VIM - in - Voice - TherapyDocument7 pages2 VIM - in - Voice - TherapyLaura MontenegroNo ratings yet
- Recent Advances in Stuttering TherapyDocument7 pagesRecent Advances in Stuttering TherapyKUNNAMPALLIL GEJO JOHNNo ratings yet
- Voice Disorders - TreatmentDocument10 pagesVoice Disorders - TreatmentPritNo ratings yet
- E. Management of AnsdDocument3 pagesE. Management of AnsdsherinNo ratings yet
- MedSLPCollective Handout Vocal Function ExercisesDocument8 pagesMedSLPCollective Handout Vocal Function ExercisesFenti FentikaNo ratings yet
- Voice Therapy OutcomeDocument10 pagesVoice Therapy Outcomemajid mirzaeeNo ratings yet
- Factors Affecting Stimulability of Erred Sounds inDocument7 pagesFactors Affecting Stimulability of Erred Sounds inLaurentiu Marian MihailaNo ratings yet
- Voice Therapy For The Professional VoiceDocument17 pagesVoice Therapy For The Professional Voiceapi-19500641100% (5)
- Conocimientos Cuidados en La VozDocument12 pagesConocimientos Cuidados en La VozJo QuezadaNo ratings yet
- SHS 451 Guided Worksheet 1 Chapters 1-2Document7 pagesSHS 451 Guided Worksheet 1 Chapters 1-2EveNo ratings yet
- Chewing Technique in Phonation of SLP StudentsDocument5 pagesChewing Technique in Phonation of SLP Studentsmajid mirzaeeNo ratings yet
- What Speech and Language Therapy Do Community Dwelling Stroke Survivors With Aphasia Receive in The UK?Document20 pagesWhat Speech and Language Therapy Do Community Dwelling Stroke Survivors With Aphasia Receive in The UK?Ranti AgustiniNo ratings yet
- CP UploadDocument4 pagesCP UploadmarufNo ratings yet
- Effects of Voice Therapy Using The Lip Trill Technique in P - 2019 - Journal ofDocument9 pagesEffects of Voice Therapy Using The Lip Trill Technique in P - 2019 - Journal ofJulia GavrashenkoNo ratings yet
- Awareness Training and Regulated-Breathing MethodDocument8 pagesAwareness Training and Regulated-Breathing Methodmajid mirzaeeNo ratings yet
- Does Voice Therapy Cure All Vocal Fold Nodules?: Ijopl IjoplDocument5 pagesDoes Voice Therapy Cure All Vocal Fold Nodules?: Ijopl IjoplDesi Ratnasari EndangNo ratings yet
- Integrating singing into voice therapyDocument7 pagesIntegrating singing into voice therapyMartin SpencerNo ratings yet
- Be Clear ProgramDocument25 pagesBe Clear ProgramAleix Criado i MarquezNo ratings yet
- Apraxia Del Habla PDFDocument60 pagesApraxia Del Habla PDFEsther CillaNo ratings yet
- Melodic Intonation Therapy and Aphasia Another Variation On A Theme PDFDocument13 pagesMelodic Intonation Therapy and Aphasia Another Variation On A Theme PDFCat TwentyTwoNo ratings yet
- Application of Singing Techniques For The Treatment of DysphoniaDocument13 pagesApplication of Singing Techniques For The Treatment of DysphoniaConcepcion NeulingNo ratings yet
- Carroll 2Document19 pagesCarroll 2Anonymous JonAFVUi4No ratings yet
- Habla ClaraDocument14 pagesHabla ClaraCristóbal Landeros TorresNo ratings yet
- Efficacy of Stuttering Therapies - PDF /KUNNAMPALLIL GEJODocument24 pagesEfficacy of Stuttering Therapies - PDF /KUNNAMPALLIL GEJOKUNNAMPALLIL GEJO JOHNNo ratings yet
- Intensive Versus Traditional Voice Therapy For VocalDocument14 pagesIntensive Versus Traditional Voice Therapy For VocalAnonymous xvlg4m5xLXNo ratings yet
- FulltextDocument7 pagesFulltextNicolas CruzNo ratings yet
- MANAGEMENT FOR ADULTS WITH STUTTERING - PDF / KUNNAMPALLIL GEJODocument28 pagesMANAGEMENT FOR ADULTS WITH STUTTERING - PDF / KUNNAMPALLIL GEJOKUNNAMPALLIL GEJO JOHN100% (1)
- ARTIGO - Efeitos Do Gargarejo - Effects of Voiced Gargling On The Electrical Activity of Extrinsic Laryngeal Muscles and Vocal Self-AssessmentDocument8 pagesARTIGO - Efeitos Do Gargarejo - Effects of Voiced Gargling On The Electrical Activity of Extrinsic Laryngeal Muscles and Vocal Self-AssessmentCarol BarbozaNo ratings yet
- Da Cunha Pereira 2017Document7 pagesDa Cunha Pereira 2017Pablo Andrés Sánchez MonsalveNo ratings yet
- Efectos de La Terapia en Disfonia Musculotensional.2017Document7 pagesEfectos de La Terapia en Disfonia Musculotensional.2017Jenith Karem Paredes GonzalezNo ratings yet
- Evidence Based Approaches To InterventionDocument28 pagesEvidence Based Approaches To InterventionSriram ManikantanNo ratings yet
- ORLADocument10 pagesORLACarol CoelhoNo ratings yet
- 10 1016@j Jvoice 2017 05 018Document7 pages10 1016@j Jvoice 2017 05 018Felipe MuñozNo ratings yet
- First Draft - LandonDocument18 pagesFirst Draft - Landonapi-347359609No ratings yet
- Glossectomy: Mr. Vijay Lazarus, M.sc. SLPDocument4 pagesGlossectomy: Mr. Vijay Lazarus, M.sc. SLPLara FraserNo ratings yet
- AdvBiomedRes418-2302049 003822Document9 pagesAdvBiomedRes418-2302049 003822JouleAlSBNo ratings yet
- Physiologic Voice Rehabilitation BasedDocument10 pagesPhysiologic Voice Rehabilitation BasedESTEFANIA GEOVANNA MEJIA MACASNo ratings yet
- 10 1016@j Otc 2019 03 002Document7 pages10 1016@j Otc 2019 03 002Mariana Fikir OrdóñezNo ratings yet
- HAT S The Vidence For: Elise BakerDocument4 pagesHAT S The Vidence For: Elise BakerRashid HussainNo ratings yet
- Communication Disorders Quarterly 2010 Bahr 131 8Document9 pagesCommunication Disorders Quarterly 2010 Bahr 131 8LauraLunguNo ratings yet
- FPL369167 InddDocument7 pagesFPL369167 Indddaniel morenoNo ratings yet
- Strech and Flow TherapyDocument9 pagesStrech and Flow TherapysopranopatriciaNo ratings yet
- A Holistic Approach To Voice TherapyDocument8 pagesA Holistic Approach To Voice Therapybz4dzwpzw8No ratings yet
- Intervention, Management of HallucinationDocument52 pagesIntervention, Management of HallucinationAshish_Singh_5126No ratings yet
- Interventions of Auditory HallucinationsDocument2 pagesInterventions of Auditory HallucinationsRijal MaullaNo ratings yet
- Vocal Improvement After Voice Therapy in Unilateral Vocal Fold ParalysisDocument6 pagesVocal Improvement After Voice Therapy in Unilateral Vocal Fold ParalysisAngela Lleuful ToledoNo ratings yet
- Ayllon 1964Document11 pagesAyllon 1964Sofya AmarisNo ratings yet
- Physical LinguisticsDocument15 pagesPhysical LinguisticsNajlaNo ratings yet
- An Eclectic Voice Therapy Program For The Treatment of Hyperfunctional Voice Disorders (HFVD)Document21 pagesAn Eclectic Voice Therapy Program For The Treatment of Hyperfunctional Voice Disorders (HFVD)daniel morenoNo ratings yet
- Efficacy of Intensive Phonatory Treatment for PresbyphoniaDocument13 pagesEfficacy of Intensive Phonatory Treatment for PresbyphoniaLindsey Bond100% (1)
- Hypnosis for Acute and Procedural Pain Management: Favorite Methods of Master Clinicians: Voices of Experience, #3From EverandHypnosis for Acute and Procedural Pain Management: Favorite Methods of Master Clinicians: Voices of Experience, #3Rating: 5 out of 5 stars5/5 (1)
- Jordanian Wedding Invitation Genre AnalysisDocument9 pagesJordanian Wedding Invitation Genre AnalysisAla'a Bani KhalefNo ratings yet
- ESP Needs Analysis for LearnersDocument8 pagesESP Needs Analysis for LearnersStephanieNo ratings yet
- Bahan Ajar English Club SMAN 1 BatujayaDocument30 pagesBahan Ajar English Club SMAN 1 BatujayaPutri AmaliaNo ratings yet
- EL101 - Module 2Document9 pagesEL101 - Module 2jhna mggyNo ratings yet
- ENGLISHDocument11 pagesENGLISHAyush GoswamiNo ratings yet
- 105 Capol, NemwelDocument2 pages105 Capol, Nemwelnemwel capolNo ratings yet
- ELLIPSISDocument15 pagesELLIPSISPutu Wulan Sari AnggraeniNo ratings yet
- Can - Abilities WorkshopDocument5 pagesCan - Abilities WorkshopestebanNo ratings yet
- Unit 4 Pronoun & Answer KeyDocument22 pagesUnit 4 Pronoun & Answer KeyZulkifli HikmahNo ratings yet
- Syllabus-IX - Eng Comm (101) - PT IIDocument2 pagesSyllabus-IX - Eng Comm (101) - PT IIpriyanshu.satapathy3600No ratings yet
- Giáo Án Môn Tiếng Anh Lớp 8 Cả Năm (Global Success) Theo Công Văn 5512 (2 Cột) Năm Học 2023-2024 (Tuần 1-31) (Ma Trận + Đặc Tả + Đề Kiểm Tra Giữa Kỳ Có Đáp Án Và File Nghe)Document152 pagesGiáo Án Môn Tiếng Anh Lớp 8 Cả Năm (Global Success) Theo Công Văn 5512 (2 Cột) Năm Học 2023-2024 (Tuần 1-31) (Ma Trận + Đặc Tả + Đề Kiểm Tra Giữa Kỳ Có Đáp Án Và File Nghe)Dạy Kèm Quy Nhơn OfficialNo ratings yet
- CILR 622 Amy Sorensen Lesson PlansDocument86 pagesCILR 622 Amy Sorensen Lesson PlansAmy SorensenNo ratings yet
- 2Document173 pages2Ankita DasNo ratings yet
- Division Learning Resource Expo PresentationDocument18 pagesDivision Learning Resource Expo PresentationLey BitosNo ratings yet
- Clause As Message 3.1. Theme and Rheme FRANDocument8 pagesClause As Message 3.1. Theme and Rheme FRANbelen oroNo ratings yet
- Possessive pronouns and apostrophesDocument2 pagesPossessive pronouns and apostrophesМади ГомарNo ratings yet
- Tasks A. Choose The Right AnswerDocument5 pagesTasks A. Choose The Right AnswerDeeaMusatNo ratings yet
- W11-12 Module 013 Logic Statements and QuantifiersDocument2 pagesW11-12 Module 013 Logic Statements and QuantifiersJL Santiago BarengNo ratings yet
- Oral Evaluation Rubric - Going ShoppingDocument1 pageOral Evaluation Rubric - Going ShoppingAna María González RodríguezNo ratings yet
- Day4 TensesDocument32 pagesDay4 TensesM.Nawaz SharifNo ratings yet
- Actividad Cotidianas InglesDocument5 pagesActividad Cotidianas InglesWilliam Geovani Maravilla CisnerosNo ratings yet
- Keep It Going (B1)Document3 pagesKeep It Going (B1)Robert PritchardNo ratings yet
- Language For ... : Medical EmergenciesDocument3 pagesLanguage For ... : Medical EmergenciesAndrzej100% (1)
- Ilovepdf MergedDocument16 pagesIlovepdf Mergedbrendanyip1129No ratings yet
- Distributional Semantics in Linguistic and Cognitive Research Article in Italian Journal of LinguisticsDocument3 pagesDistributional Semantics in Linguistic and Cognitive Research Article in Italian Journal of LinguisticsRodrigo SanzNo ratings yet
- SCHOOL-WORKWEEK-PLAN-FOR-ASATIDZ NORMALIA - SeptemberDocument6 pagesSCHOOL-WORKWEEK-PLAN-FOR-ASATIDZ NORMALIA - SeptemberIban GuiamalodinNo ratings yet
- Final-DSC-2024-District Wise DR VacancyDocument37 pagesFinal-DSC-2024-District Wise DR VacancyanilkonakatiamarNo ratings yet
- Laoag City, Ilocos Norte - Phrases and ClausesDocument6 pagesLaoag City, Ilocos Norte - Phrases and ClausesIvyne Jenica GuerreroNo ratings yet