Professional Documents
Culture Documents
RCPA Allowable Limits of Performance
Uploaded by
emmanuel alonsoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
RCPA Allowable Limits of Performance
Uploaded by
emmanuel alonsoCopyright:
Available Formats
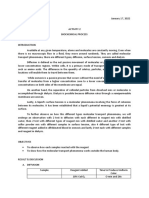
Appendix A
Programs, Analytes and Allowable Limits of Performance
ALCOHOL/AMMONIA ± 10% > 500 nmol/day CSF
Alcohol ± 2.2 ≤ 21.7 mmol/L Normetanephrine ± 1.0 ≤ 3.0 µmol/day Albumin ± 0.10 ≤ 1.00 g/L
± 10% > 21.7mmol/L ± 33% > 3.0 µmol/day ± 10% > 1.0 g/L
Ammonia ± 3 ≤ 30 µmol/L Serotonin ± 0.3 ≤ 1.0 µmol/day Glucose ± 1.0 ≤ 10 mmol/L
± 10% > 30 µmol/L ± 30% > 1.0 µmol/day ± 10% > 10 mmol/L
Immunoglobulin G ± 0.1 ≤ 1.00 g/L
± 10% > 1.00 g/L
ANTIBIOTICS BLOOD GASES Lactate ± 1.0 ≤ 10 mmol/L
Chloride ± 3.0 mmol/L ± 10% > 10.0 mmol/L
Amikacin ± 2.0 ≤ 20.0 mg/L
± 10% > 20.0 mg/L Glucose ± 1.0 ≤ 10.0 mmol/L Total Protein ± 0.10 ≤ 1.0 g/L
± 10% > 10.0 mmol/L ± 10% > 1.00 g/L
Gentamicin ± 0.5 ≤ 5.0 mg/L
± 10% > 5.0 mg/L Ionised Calcium ± 0.05 mmol/L
Tobramycin ± 0.5 ≤ 5.0 mg/L Lactate ± 1.0 ≤ 10.0 mmol/L
± 10% > 5.0 mg/L ± 10% > 10.0 mmol/L ENDOCRINE
Vancomycin ± 2.0 ≤ 20.0 mg/L pH ± 0.04 AFP ± 5 ≤ 25 kIU/L
± 10% > 20.0 mg/L pCO2 ± 2.0 ≤ 25.0 mm Hg ± 20% > 25 kIU/L
± 8% > 25.0 mm Hg Androstenedione ± 2.0 nmol/L
pO2 ± 5 ≤ 100 mm Hg CA125 ± 10 ≤ 50 kU/L
± 5% > 100 mm Hg ± 20% > 50 kU/L
BIOGENIC AMINES Potassium ± 0.2 mmol/L
Adrenaline ± 50 ≤ 150 nmol/day
CEA ± 2.0 ≤ 10.0 µg/L
Sodium ± 3.0 mmol/L ± 20% > 10.0 µg/L
± 33% > 150 nmol/day
Dopamine ± 0.25 ≤ 1.0 µmol/day Cortisol ± 30 ≤ 200 nmol/L
± 25% > 1.0 µmol/day ± 15% > 200 nmol/L
CO-OXIMETRY 11-Deoxycortisol ± 30.0 ≤ 200.0 nmol/L
5HIAA ± 20 ≤ 100 µmol/day
Haemoglobin Concentration ± 3 ≤ 100 g/L ± 15% > 200.0 nmol/L
± 20% > 100 µmol/day
± 3% > 100 g/L DHEA Sulphate ± 1.0 ≤ 10.0 µmol/L
HMMA ± 20 ≤ 100 µmol/day Fractional Oxyhaemoglobin ± 3 ≤ 75.0% ± 10% > 10.0 µmol/L
± 20% > 100 µmol/day ± 4% > 75.0% Ferritin ± 6.0 ≤ 40.0 µg/L
HVA ± 8 ≤ 32 µmol/day Fractional ± 2.0% ± 15% > 40.0 µg/L
± 25% > 32 µmol/day Carboxyhaemoglobin Folate ± 1.0 ≤ 4.0 nmol/L
Metanephrine ± 0.5 ≤ 1.5 µmol/day Fractional Methaemoglobin ± 1.0 ≤ 10.0% ± 25% > 4.0 nmol/L
± 33% > 1.5µmol/day ± 10% > 10% FSH ± 4.0 ≤ 20.0 IU/L
Noradrenaline ± 50 ≤ 500 nmol/day
± 20% > 20.0 IU/L
© RCPA-AACB Chemical Pathology Quality Assurance Programs Group – Appendix A – Page 26
Gastrin ± 25 ≤ 250 pmol/L Free PSA ± 1.5 ≤ 10 µg/L CK-MB ± 6 ≤ 40 U/L & µg/L
± 10% > 250 pmol/L ± 15% > 10 µg/L ± 15% > 40 U/L & µg/L
Growth Hormone ± 2 ≤ 10m U/L Aldosterone ± 75.0 ≤ 500.0 pmol/L Cortisol ± 30 ≤ 200 nmol/L
± 20% > 10 mU/L ± 15% > 500.0 pmol/L ± 15% > 200 nmol/L
HCG ± 3 ≤ 20 IU/L PTH ± 2.5 ≤ 10.0 pmol/L Creatinine ± 0.010 ≤ 0.100 mmol/L
± 15% > 20 IU/L ± 25% > 10.0 pmol/L ± 10% > 0.100 mmol/L
17-Hydroxyprogesterone ± 3.0 ≤ 15.0 nmol/L Plasma Renin Activity ± 1.0 ≤ 4.0 ng/mL/hr Ferritin ± 6.0 ≤ 40 µg/L
± 20% > 15.0 nmol/L ± 25% > 4.0 ng/mL/hr ± 15% > 40 µg/L
IgE ± 4.0 ≤ 20.0 IU/L Active Renin ± 1.0 ≤ 4.0 µU/mL Fructosamine ± 30 ≤ 300 µmol/L
± 20% > 20.0 IU/L ± 25% > 4.0 µU/mL ± 10% > 300 µmol/L
Insulin ± 5.0 ≤ 20.0 mU/L Glucose ± 0.5 ≤ 5.0 mmol/L
± 25% > 20.0 mU/L ± 10% > 5.0 mmol/L
LH ± 2.0 ≤ 10.0 IU/L GGT ± 8 ≤ 60 U/L
± 20% > 10.0 IU/L ± 15% > 60 U/L
Oestradiol ± 100 ≤ 500 pmol/L GENERAL SERUM CHEMISTRY hCG-quantitative ± 3.0 ≤ 20.0I U/L
± 20% > 500 pmol/L Acid Phos (Total) ± 1.5 ≤ 10.0 U/L & ± 15% > 20.0 IU/L
Oestriol(Total) ± 20 ≤ 200 nmol/L µg/L hCG-qualitative neg. ≤ 20 IU/L
± 10% > 200 nmol/L ± 15% > 10.0 U/L & pos. > 30 IU/L
Oestriol(Unconjugated) ± 5.0 ≤ 25.0 nmol/L µg/L HDL Cholesterol ± 0.20 ≤ 2.00 mmol/L
± 20% > 25.0 nmol/L Acid Phos (Pros) ± 1.5 ≤ 10.0 U/L&µg/L ± 10% > 2.00 mmol/L
Progesterone ± 2 ≤ 10 nmol/L ± 15% > 10.0 U/L&µg/L Iron ± 5.0 µmol/L
± 25% > 10 nmol/L Albumin ± 2.0 ≤ 20.0 g/L Lactate Dehydrogenase ± 30 ≤ 200 U/L
Prolactin ± 20 ≤ 100 mIU/L ± 10% > 20.0 g/L ± 15% > 200 U/L
± 20% > 100 mIU/L Alkaline Phosphatase ± 15 ≤ 100 U/L Lactate ± 1.0 ≤ 10.0 mmol/L
SHBG ± 5 ≤ 50 nmol/L ± 15% > 100 U/L ± 10% > 10.0 mmol/L
± 10% > 50 nmol/L ALT ± 8 ≤ 60 U/L Lipase ± 40 ≤ 200 U/L
Testosterone ± 0.5 ≤ 2.5 nmol/L ± 15% > 60 U/L ± 20% > 200 U/L
± 20% > 2.5 nmol/L Amylase ± 15 ≤ 100 U/L Lithium ± 0.20 mmol/L
TSH ± 0.6 ≤ 4.0 mU/L ± 15% > 100 U/L
Magnesium ± 0.12 mmol/L
± 15% > 4.0 mU/L AST ± 8 ≤ 60 U/L
± 15% > 60 U/L Osmolality ± 8 mmol/kg
Free T3 ± 3 pmol/L
Free T4 ± 1.5 ≤ 10 pmol/L Bicarbonate ± 2.0 ≤ 20.0 mmol/L Phosphate ± 0.10 ≤ 1.00 mmol/L
± 15% > 10 pmol/L ± 10% > 20.0 mmol/L ± 10% > 1.00 mmol/L
Total T3 ± 0.3 ≤ 1.5 nmol/L Bilirubin-Total ± 5 ≤ 50 µmol/L Potassium ± 0.2 mmol/L
± 20% > 1.5 nmol/L ± 10% > 50 µmol/L Protein (Total) ± 5.0 g/L
Total T4 ± 8 ≤ 50 nmol/L Bilirubin Conjugated ± 10 ≤ 50 µmol/L Sodium ± 3 mmol/L
± 15% > 50 nmol/L ± 20% > 50 µmol/L Total T3 ± 0.3 ≤ 2.0 nmol/L
Vitamin B12 ± 20 ≤ 100 pmol/L Calcium ± 0.10 mmol/L ± 15% > 2.0 nmol/L
± 20% > 100 pmol/L Chloride ± 3 mmol/L Free T3 ± 3.0 pmol/L
Vitamin D3 ± 5 ≤ 20 nmol/L Cholesterol ± 0.50 ≤ 10.00 mmol/L Free T4 ± 3.0 ≤ 20.0 pmol/L
± 15 > 20 nmol/L ± 5% > 10.00 mmol/L ± 15% > 20.0 pmol/L
Total PSA ± 1.5 ≤ 10.0 µg/L Creatine Kinase ± 15 ≤ 100 U/L TSH ± 0.6 ≤ 4.0 mU/L
± 15% > 10.0 µg/L ± 15% > 100 U/L ± 15% > 4.0 mU/L
© RCPA-AACB Chemical Pathology Quality Assurance Programs Group – Appendix A – Page 27
Thyroxine ± 8 ≤ 100 nmol/L GLYCOHAEMOGLOBIN hCG-qualitative neg. ≤ 20 IU/L
± 15% > 100 nmol/L Haemoglobin A1c ± 0.5 ≤ 10.0% pos. > 30 IU/L
TIBC ± 10.0 µmol/L ± 5% > 10.0% HDL Cholesterol ± 0.20 ≤ 2.00 mmol/L
Transferrin ± 0.50 g/L ± 10% > 2.00 mmol/L
Triglyceride ± 0.20 ≤ 2.00 mmol/L Lactate Dehydrogenase ± 30 ≤ 200 U/L
± 10% > 2.00 mmol/L ± 15% > 200 U/L
IGF-1 / C PEPTIDE Magnesium ± 0.12 mmol/L
Troponin I ± 0.2 ≤ 2.0 ng/mL
± 10% > 2.0 ng/mL IGF-1 ± 3 ≤ 20 nmol/L Potassium ± 2.0 mmol/L
Troponin T ± 0.10 ≤ 1.0 ng/mL ± 15% > 20 nmol/L Protein (Total) ± 5.0 g/L
± 10% > 1.0 ng/mL C Peptide ± 1.0 ≤ 10 nmol/L Sodium ± 3 mmol/L
Urate ± 0.050 mmol/L ± 10% > 10 nmol/L Triglyceride ± 0.20 ≤ 2.00 mmol/L
Urea ± 1.0 ≤ 10.0 mmol/L ± 10% > 2.00 mmol/L
± 10% > 10.0 mmol/L Urate ± 0.050 mmol/L
NEAR PATIENT TESTING Urea ± 1.0 ≤ 10.0 mmol/L
Albumin ± 2.0 ≤ 20.0 g/L ± 10% > 10.0 mmol/L
± 10% > 20.0 g/L
GENERAL THERAPEUTIC DRUGS Alkaline Phosphatase ± 15 ≤ 100 U/L
Carbamazepine ± 2.0 ≤ 20.0 µmol/L ± 15% > 100 U/L NEONATAL BILIRUBIN
± 10% > 20.0 µmol/L ALT ± 8 ≤ 60 U/L
Total Bilirubin ± 15 ≤ 150 µmol/L
Digoxin ± 0.2 ≤ 2.0 nmol/L ± 15% > 60 U/L
± 10% > 150 µmol/L
± 10% > 2.0 nmol/L Amylase ± 15 ≤ 100 U/L
Conjugated Bilirubin ± 10 ≤ 50 µmol/L
Gentamicin ± 0.5 ≤ 5.0 mg/L ± 15% > 100 U/L
± 10% > 5.0 mg/L AST ± 8 ≤ 60 U/L ± 20% > 50 µmol/L
Paracetamol ± 20 ≤ 200 µmol/L ± 15% > 60 U/L
± 10% > 200 µmol/L Bicarbonate ± 2.0 ≤ 20.0 mmol/L
Phenobarbitone ± 3.0 ≤ 30.0 µmol/L ± 10% > 20.0 mmol/L PORPHYRINS
± 10% > 30.0 µmol/L Bilirubin ± 5 ≤ 50 µmol/L Urine ALA ± 5 ≤ 20 µmol/L
Phenytoin ± 3.0 ≤ 30.0 µmol/L ± 10% > 50 µmol/L ± 25% > 20 µmol/L
± 10% > 30.0 µmol/L Calcium ± 0.10 mmol/L Urine Porphobilinogen ± 5 ≤ 25 µmol/L
Quinidine ± 2.0 ≤ 20.0 µmol/L Chloride ± 3 mmol/L (Quantitative) ± 20% > 25 µmol/L
± 10% > 20.0 µmol/L Cholesterol ± 0.50 ≤ 10.00 mmol/L Urine Porphobilinogen neg ≤ 10 µmol/L
Salicylate ± 0.10 ≤ 1.00 mmol/L ± 5% > 10.00 mmol/L (Qualitative) + 10-50 µmol/L
± 10% > 1.00 mmol/L Creatine Kinase ± 15 ≤ 100 U/L ++ 51-100 µmol/L
Theophylline ± 3 ≤ 30 µmol/L ± 15% > 100 U/L +++ > 100 µmol/L
± 10% > 30 µmol/L Creatinine ± 0.010 ≤ 0.100 mmol/L Urine Total Porphyrin ± 15 ≤ 100 nmol/L
Valproate ± 25 ≤ 250 µmol/L ± 10% > 0.100 mmol/L ± 15% > 100 nmol/L
± 10% > 250 µmol/L Glucose ± 0.5 ≤ 5.0 mmol/L Faecal Percent Dry Weight ± 1 ≤ 10%
Vancomycin ± 2.0 ≤ 20.0 mg/L ± 10% > 5.0 mmol/L ± 10% > 10%
± 10% > 20.0 mg/L GGT ± 8 ≤ 60 U/L Faecal Total Porphyrin ± 15 ≤ 100 µmol/kg
± 15% > 60 U/L ± 15% > 100 µmol/kg
hCG-quantitative ± 3.0 ≤ 20.0 IU/L Plasma Total Porphyrin ± 3 ≤ 20 nmol/L
± 15% > 20.0 IU/L ± 15% > 20 nmol/L
© RCPA-AACB Chemical Pathology Quality Assurance Programs Group – Appendix A – Page 28
RBC Total Porphyrin ± 0.3 ≤ 2.0 µmol/L rc Chloride ± 2 ≤ 20 mmol/L DPD (Total) ± 15 ≤ 80 nmol/L
± 15% > 2.0 µmol/L rc ± 10% > 20 mmol/L ± 15% > 80 nmol/L
Sweat Conductivity ± 2 ≤ 20 mmol/L DPD (Free) ± 15 ≤ 80 nmol/L
± 10% > 20 mmol/L ± 15% > 80 nmol/L
SPECIAL LIPIDS Glucose ± 1.0 ≤ 10.0 mmol/L
Cholesterol ± 0.50 ≤ 10.00 mmol/L ± 10% > 10.0 mmol/L
hCG-quantitative ± 5 ≤ 50 IU/L
± 5% > 10.00 mmol/L TUMOUR MARKERS ± 10% > 50 IU/L
HDL Cholesterol ± 0.20 ≤ 2.00 mmol/L ACTH ± 2.0 ≤ 20 pmol/L
± 10% > 2.00 mmol/L hCG-qualitative neg. ≤ 20 IU/L
± 10% > 20 pmol/L pos. > 30 IU/L
Triglyceride ± 0.2 ≤ 2.0 mmol/L Alpha-fetoprotein ± 5 ≤ 25 kIU/L
± 10% > 2.0 mmol/L Hydroxyproline ± 10 ≤ 100 µmol/L
± 20% > 25 kIU/L ± 10% > 100 µmol/L
Apolipoprotein A1 ± 0.2 ≤ 2.0 g/L Calcitonin ± 2 ≤ 20 ng/L
± 10% > 2.0 g/L Magnesium (Serum) ± 0.12 mmol/L
± 10% > 20 ng/L
Apolipoprotein B ± 0.2 ≤ 2.0 g/L N-Telopeptides ± 80 ≤ 700 nmolBCE/L
CEA ± 2.0 ≤ 10.0 µg/L
± 10% > 2.0 g/L ± 20% > 10.0 µg/L ± 10% > 700 nmolBCE/L
CA125 ± 10 ≤ 50 kU/L
Osmolality ± 6 ≤ 300 mmol/kg
± 20% > 50 kU/L ± 2% > 300 mmol/kg
SPECIAL THERAPEUTIC DRUGS CA15-3 ± 3 ≤ 20 kU/L
Potassium ± 2 ≤ 20 mmol/L
Amiodarone ± 0.2 ≤ 2.0 µmol/L ± 15% > 20 kU/L ± 10% > 20 mmol/L
± 10% > 2.0 µmol/L Phosphate ± 2.5 mmol/L
CA19-9 ± 3 ≤ 20 kU/L
Amitriptyline ± 10 ≤ 100 µmol/L ± 15% > 20 kU/L
Sodium ± 2 ≤ 20 mmol/L
± 10% > 20 mmol/L
± 10% > 100 µmol/L hCG ± 3 ≤ 20 IU/L
± 15% > 20 IU/L
Total Protein ± 0.10 ≤ 1.00 g/L
Disopyramide ± 2.0 ≤ 20.0 µmol/L
± 10% > 1.00 g/L
± 10% > 20.0 µmol/L Beta-2-Microglobulin ± 0.2 ≤ 2.0 mg/L
Urate ± 0.3 mmol/L
Ethosuximide ± 3 ≤ 30 µmol/L ± 10% > 2.0 mg/L
Urea ± 20 ≤ 200 mmol/L
± 10% > 30 µmol/L NSE ± 2.0 ≤ 20 µg/L
± 10% > 200 mmol/L
Lignocaine ± 2.0 ≤ 20.0 µmol/L ± 10% > 20 µg/L
± 10% > 20.0 µmol/L Prolactin ± 20 ≤ 100 mU/L
Methotrexate ± 0.10 ≤ 1.00 µmol/L ± 20% > 100 mU/L URINE PREGNANCY TESTING
± 10% > 1.00 µmol/L Total PSA ± 1.5 ≤ 10.0 µg/L hCG neg. ≤ 20 IU/L
Nortriptyline ± 10 ≤ 100 nmol/L ± 15% > 10.0 µg/L pos. > 30 IU/L
± 10% > 100 nmol/L
Quinidine ± 2.0 ≤ 20.0 µmol/L
± 10% > 20.0umol/L VITAMINS
URINE CHEMISTRY
Tricyclic Antidepressants ± 10 ≤ 100 nmol/L Vitamin A ± 0.3 ≤ 3.0 µmol/L
Albumin ± 0.10 ≤ 1.0 g/L
± 10% > 100 nmol/L ± 10% > 3.0 µmol/L
± 10% > 1.0 g/L
Calcium ± 0.20 mmol/L
Vitamin E ± 5.0 ≤ 50.0 µmol/L
Chloride ± 2 ≤ 20 mmol/L ± 10% > 50 µmol/L
SWEAT ELECTROLYTES ± 10% > 20 mmol/L β Carotene ± 0.2 ≤ 20 µmol/L
Sodium ± 2 ≤ 20 mmol/L Creatinine ± 0.5 ≤ 5.0 mmol/L ± 10% > 20 µmol/L
± 10% > 20 mmol/L ± 10% > 5.0 mmol/L Total Carotenoids ± 0.4 ≤ 4.0 µmol/L
± 10% > 4.0 µmol/L
© RCPA-AACB Chemical Pathology Quality Assurance Programs Group – Appendix A – Page 29
Appendix B
Allowable Limits of Performance
The estimation of quality in an external quality assurance program can be relative or considering an improvement by moving to a broad based clinical strategy such as
absolute. Relative quality is achieved by comparing a laboratories performance limits based on biological variability. These limits are freely available in the
against their peers. Examples include ranking precision and the reporting of a literatureiii.
median as the ‘target’ for accuracy. Absolute quality is a difficult concept. The setting
of an absolute level for accuracy, relies on having absolute calibration standards However before we make any changes in this program we should be considering
and/or reference methodologies. However to set absolute quality levels for precision, these questions: Should we be aiming to have a minimum (safety) standard i.e. a
standards are even more difficult to define. The ISO Technical Committee 212 task standard that if laboratories are performing below it is unacceptable or an optimal
force classified a hierarchy of approaches in defining analytical quality specificationi (ideal) standard i.e. a standard that some laboratories are achieving and all
which are listed in Table 1. laboratories should be aiming for?
The most appropriate quality standard is one that is based on clinical need. Clinical need based on biological variability would, in general, have some of our
Unfortunately studies that define analytical performance in terms of clinical outcome assays performing at a minimum standard e.g. calcium and sodium while other
are few. An example is the setting of desirable performance for HbA1c based on assays generally exceed optimal standards e.g. triglyceride and most enzymes. We
DCCT trial requirements. would not want to set goals that are not generally achievable, neither would we want
to set goals that are significantly below what most laboratories can achieve.
Broad clinical need can be defined in two ways; A clinicians survey may give an idea Nevertheless we will be reviewing our allowable limits over the next couple of years
if what would be required clinically, however the process of collecting that to more clearly reflect what is desirable for the profession and ultimately for the need
information needs to be rigorous and may still be biased by the clinicians historical of our patients.
experience of laboratory performance. Another broad based clinical approach is to
have analytical precision that can generally reveal the typical variability in patients Table 1. Heirarchical listing of procedures available for the determination of
results. These biological variability requirements can further be defined as minimal, analytical quality.
desirable and optimal standards of analytical performance in terms of the ability to
LEVEL APPROACH PROCEDURE
track patients changesii.
I Specific Clinical Need Clinical Outcome Studies
The profession defined method, or a set of analytical standards defined by an group II Broad Clinical Need Biological Variation
of experts in the profession, is the way that this programs ‘Allowable Limits of Clinician Survey
Performance’ have been defined. They have been defined over the last decade or III Profession Defined Expert Committee
more with the assistance of the advisory and target setting committees that the IV Proficiency Testing EQA survey
program relies on. State of the art
Proficiency Testing approaches are different. They are based on setting the V Other Existing practice
standard in terms of the results from proficiency testing e.g. setting a minimum Publications
standard on what most laboratories are able to achieve, or an optimal standard on
the state of the art as measured within the program.
i
Kaplan L.A., “Determination and application f desirable analytical performance goals: the
Finally when none of the above information is available, a quality standard may be ISO/TC 212 approach.” Scand J Clin Lab Invest 1999; 59: 479-482.
based on some other estimate of performance that has been recorded by a group or ii
Fraser C.G., “General Strategies to set quality specifications for reliability performance
even an individual laboratory in a publication. characteristics.” Scand J Clin Lab Invest 1999; 59: 487-490.
iii
Ricos C. et al “Current databases on biological variation: pros, cons and progress.” Scand J
Therefore, the QAP’s Allowable Limits of Performance are a good approach,
Clin Lab Invest. 1999; 59: 491-500.
especially as clinical outcome studies are so few and far between. We have been
© RCPA-AACB Chemical Pathology Quality Assurance Programs Group – Page 30
You might also like
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- SMILE Validation Requirements for Chemistry TEaDocument6 pagesSMILE Validation Requirements for Chemistry TEabenchmark InnovationNo ratings yet
- Total Allowable ErrorDocument16 pagesTotal Allowable ErrorSmilja Salazar CortezNo ratings yet
- CLIA Waived Codes ListDocument41 pagesCLIA Waived Codes ListKarunanidhi PalaniveluNo ratings yet
- Reference Intervals - Direct Priori MethodDocument5 pagesReference Intervals - Direct Priori MethodMWNo ratings yet
- Conversion PDFDocument2 pagesConversion PDFGavin TexeirraNo ratings yet
- Desirable Biological Variation Database Specifications - WestgardDocument10 pagesDesirable Biological Variation Database Specifications - WestgardElmyLiantika MaranantanNo ratings yet
- Beckman Coulter Cellavision DM96Document166 pagesBeckman Coulter Cellavision DM96Al Joseph Malinay AndaNo ratings yet
- Clinical Biochemistry Reference Ranges HandbookDocument18 pagesClinical Biochemistry Reference Ranges HandbookMurali DathanNo ratings yet
- EP Evaluator-CLIA EE-CLIA For Evaluating ClinicalDocument3 pagesEP Evaluator-CLIA EE-CLIA For Evaluating ClinicalKamal JaoniNo ratings yet
- Adjusting Quality Control Chart Limits For WBC, RBC, HB, and PLT Counts To Reduce Daily Control Risks in Hospital LaboratoryDocument11 pagesAdjusting Quality Control Chart Limits For WBC, RBC, HB, and PLT Counts To Reduce Daily Control Risks in Hospital LaboratoryHerbanu PramonoNo ratings yet
- XN-L - Reference Interval From General Information 2017Document4 pagesXN-L - Reference Interval From General Information 2017widiawaty100% (1)
- Quality Control: An OverviewDocument12 pagesQuality Control: An OverviewabufathiNo ratings yet
- Statistics For Anal. Chem. - Lecture Notes - Xu Ly So LieuDocument157 pagesStatistics For Anal. Chem. - Lecture Notes - Xu Ly So LieuLiên Hương100% (1)
- Clia & Cap Regulatory TrainingDocument23 pagesClia & Cap Regulatory TrainingWilliam David HommelNo ratings yet
- Tests Affected by Haemolysed, Icteric and Lipemic Samples, W5-SOP-1-1-1Document2 pagesTests Affected by Haemolysed, Icteric and Lipemic Samples, W5-SOP-1-1-1Dejan BodetićNo ratings yet
- Prof. Joy V. Lorin-Picar Davao Del Norte State College: New Visayas, Panabo CityDocument91 pagesProf. Joy V. Lorin-Picar Davao Del Norte State College: New Visayas, Panabo CityJeLo ReaNdelarNo ratings yet
- Biological Variation Database Structure and Criteria Used For Generation and UpdateDocument7 pagesBiological Variation Database Structure and Criteria Used For Generation and UpdateFede0No ratings yet
- Introduction To Laboratory Management ModulesDocument2 pagesIntroduction To Laboratory Management ModulesEman BayoumiNo ratings yet
- 108590202A GU Basic Laboratory Skills A4 en LRDocument92 pages108590202A GU Basic Laboratory Skills A4 en LRΔΑΝΑΗ ΓΙΑΝΝΑΡΗNo ratings yet
- Basic Statistics in Laboratory Quality Control: QC Workbook SeriesDocument40 pagesBasic Statistics in Laboratory Quality Control: QC Workbook SeriesYaser MNo ratings yet
- An Introduction To Proteomics: The Protein Complement of The GenomeDocument40 pagesAn Introduction To Proteomics: The Protein Complement of The GenomeJohn Louie BarquerosNo ratings yet
- Chemical Pathology HODocument17 pagesChemical Pathology HOMurali TiarasanNo ratings yet
- Validate Qualitative Test Method ResultsDocument2 pagesValidate Qualitative Test Method ResultsShaheer BadarNo ratings yet
- Gradient HPLCDocument20 pagesGradient HPLCharoonjdasanNo ratings yet
- Flow Cell Wash Kit Exp wsh004 WFC - 9120 - v1 - Revb - 08dec2020 MinionDocument9 pagesFlow Cell Wash Kit Exp wsh004 WFC - 9120 - v1 - Revb - 08dec2020 MinionErikk DangNo ratings yet
- EP15-A3 Example 2Document4 pagesEP15-A3 Example 2Jenny RosaliNo ratings yet
- Basics of Laboratory Internal Quality Control, Ola ElgaddarDocument27 pagesBasics of Laboratory Internal Quality Control, Ola ElgaddarOla ElgaddarNo ratings yet
- Point-Of-Care Analyzers, Blood Gas - PH - Chemistry - Electrolyte - 050315065814Document3 pagesPoint-Of-Care Analyzers, Blood Gas - PH - Chemistry - Electrolyte - 050315065814Carlos Ferro100% (1)
- Methods Comparison 5th Sept'18 DR PriyaDocument65 pagesMethods Comparison 5th Sept'18 DR Priyaamit danielNo ratings yet
- LC Ms Training Protocol 2Document26 pagesLC Ms Training Protocol 2Hóa Học K64 Tài NăngNo ratings yet
- CLIAbrochure8 PDFDocument12 pagesCLIAbrochure8 PDFAlexandr Chuvakov100% (1)
- Westgard Rules - and Multirules - WestgardDocument13 pagesWestgard Rules - and Multirules - Westgardhan-didiiNo ratings yet
- How To Be A Lab Director 2017Document200 pagesHow To Be A Lab Director 2017pieterinpretoria391No ratings yet
- Clia & Individualized Quality Control Plan (IQCP) : Mls (Ascp)Document66 pagesClia & Individualized Quality Control Plan (IQCP) : Mls (Ascp)dragussetiawan2841No ratings yet
- Quality Control2Document32 pagesQuality Control2Mustafa KhandgawiNo ratings yet
- IQCPDocument1 pageIQCPPrabhu Selvaraj100% (1)
- Manual Differential Cell Count LabDocument9 pagesManual Differential Cell Count LabFatima Mae LusanNo ratings yet
- Interferences From Blood Collection Tube Components On Clinical Chemistry Assays - Biochemia MedicaDocument8 pagesInterferences From Blood Collection Tube Components On Clinical Chemistry Assays - Biochemia MedicaBeatThe BeadNo ratings yet
- 1 - Fluoroscopy-36063022Document6 pages1 - Fluoroscopy-36063022Sinta Dewi P.No ratings yet
- Lab Math Lec (Prelims)Document7 pagesLab Math Lec (Prelims)Merra VenzuelaNo ratings yet
- Cells in The Urine SedimentDocument3 pagesCells in The Urine SedimentTaufan LutfiNo ratings yet
- Laboratory ScopesDocument67 pagesLaboratory ScopesNash Si100% (1)
- NABL 112 Effective From 01.06.2019 PDFDocument102 pagesNABL 112 Effective From 01.06.2019 PDFSp PpvNo ratings yet
- 1.01.05 ValidationDocument16 pages1.01.05 ValidationVina PerawatiNo ratings yet
- Tips and Tricks HPLC Troubleshooting AgilentDocument30 pagesTips and Tricks HPLC Troubleshooting AgilentverajaNo ratings yet
- 3.1.1 HBsAg Testing (ELISA Method)Document6 pages3.1.1 HBsAg Testing (ELISA Method)Jeevan VkiNo ratings yet
- Imprecision, Bias and Tot Error of AnalyserDocument7 pagesImprecision, Bias and Tot Error of AnalyserShubho BiswasNo ratings yet
- Calculation and Preparation of Standard Solutions in Food AnalysisDocument5 pagesCalculation and Preparation of Standard Solutions in Food AnalysisMahi HarixNo ratings yet
- Specimen Collection Manual January 2015Document35 pagesSpecimen Collection Manual January 2015ARIF AHAMMED PNo ratings yet
- Chemistry and Tox InfoDocument129 pagesChemistry and Tox InfoGodstruthNo ratings yet
- TE, TEa, Six-SigmaDocument36 pagesTE, TEa, Six-SigmaDr. Pillala KrishnaveniNo ratings yet
- Analytical Method Validation ForDocument21 pagesAnalytical Method Validation ForBLUEPRINT Integrated Engineering ServicesNo ratings yet
- Care Maintenance and HPLC Column TroubleshootingDocument52 pagesCare Maintenance and HPLC Column TroubleshootingducngoctrinhNo ratings yet
- Automated Hematology Cell Counters - ImpedanceDocument14 pagesAutomated Hematology Cell Counters - ImpedanceNoth MT Bnk100% (1)
- Calibrating and validating analytical methodsDocument32 pagesCalibrating and validating analytical methodsHaziq KhairiNo ratings yet
- Post-Analytical Best PracticesDocument48 pagesPost-Analytical Best PracticesSaravnan RajendranNo ratings yet
- Order of DrawDocument1 pageOrder of Drawighiunghius100% (1)
- BD Tritest™ CD3/CD4/CD45: 50 Tests Per Kit-Catalog No. 342413 50 Tests Per Kit With BD Trucount™ Tubes-Catalog No. 342444Document31 pagesBD Tritest™ CD3/CD4/CD45: 50 Tests Per Kit-Catalog No. 342413 50 Tests Per Kit With BD Trucount™ Tubes-Catalog No. 342444winarsitaswinNo ratings yet
- Requerimientos de Calidad 2008 95%, 97% y 99%Document18 pagesRequerimientos de Calidad 2008 95%, 97% y 99%emmanuel alonsoNo ratings yet
- Especificaciones de Calidad CLIADocument2 pagesEspecificaciones de Calidad CLIAemmanuel alonsoNo ratings yet
- Bio Database 2014Document5 pagesBio Database 2014yousrazeidan1979No ratings yet
- Especificaciones de Calidad CLIADocument2 pagesEspecificaciones de Calidad CLIAemmanuel alonsoNo ratings yet
- RCPA Allowable Limits of PerformanceDocument5 pagesRCPA Allowable Limits of Performanceemmanuel alonsoNo ratings yet
- Requerimientos de Calidad 2008 95%, 97% y 99%Document18 pagesRequerimientos de Calidad 2008 95%, 97% y 99%emmanuel alonsoNo ratings yet
- HermanYeung DSE Bio CH 3E Temp NoteDocument5 pagesHermanYeung DSE Bio CH 3E Temp NoteliNo ratings yet
- Lipids Chem MBBSDocument57 pagesLipids Chem MBBSUmar JibrinNo ratings yet
- Etas Mcqs 2019 PlusDocument1,569 pagesEtas Mcqs 2019 PlusSally dossNo ratings yet
- CBSE Class 9 Science Notes On TissuesDocument6 pagesCBSE Class 9 Science Notes On TissuesShubh MantriNo ratings yet
- Adobe Scan 16-Jul-2023Document6 pagesAdobe Scan 16-Jul-2023Vipul KannojiaNo ratings yet
- Structural Organisation in Animals Mind MapDocument3 pagesStructural Organisation in Animals Mind MapAstha AgrawalNo ratings yet
- Anatomical Charaterization of Pilosocereus Pachycladus F. Ritter RootsDocument6 pagesAnatomical Charaterization of Pilosocereus Pachycladus F. Ritter RootsAnne KarolineNo ratings yet
- Laboratory Activity No. 10: Frog Circulatory and Excretory SystemDocument5 pagesLaboratory Activity No. 10: Frog Circulatory and Excretory SystemMaricris GuillermoNo ratings yet
- NCM 108 - Nursing Care During Normal Pregnancy and Care of The Developing FetusDocument5 pagesNCM 108 - Nursing Care During Normal Pregnancy and Care of The Developing FetusKristine BartsNo ratings yet
- Lesson Plan 2020-2021Document7 pagesLesson Plan 2020-2021MELIE BAGARESNo ratings yet
- Primer: Frozen ShoulderDocument16 pagesPrimer: Frozen ShoulderJose PerezNo ratings yet
- Activity 2 Biochemical Process Written Report - ArabDocument5 pagesActivity 2 Biochemical Process Written Report - Arabtrisha estrellaNo ratings yet
- Bio X Control and Coordination AssignmentDocument2 pagesBio X Control and Coordination AssignmentdevanshiNo ratings yet
- Bio T4 DLP KSSM Chapter 11Document59 pagesBio T4 DLP KSSM Chapter 11fadilahNo ratings yet
- Biochemistry Exam 2 (Outline)Document9 pagesBiochemistry Exam 2 (Outline)stanly sotoNo ratings yet
- AMORC Index Degrees 5 and 6Document48 pagesAMORC Index Degrees 5 and 6Alois HaasNo ratings yet
- Assigning Site of Origin in Metastatic NeuroendocrineDocument30 pagesAssigning Site of Origin in Metastatic NeuroendocrineGuan-Ying WuNo ratings yet
- Prof. N. Syabbalo: MB., CHB., PHD., FCCP., FRS., Fiba Professor of Physiology & MedicineDocument50 pagesProf. N. Syabbalo: MB., CHB., PHD., FCCP., FRS., Fiba Professor of Physiology & MedicineHomeground entertainmentNo ratings yet
- Institute Log # 4 PDFDocument1 pageInstitute Log # 4 PDFTim MinNo ratings yet
- Borer (2013) Advanced Exercise Endocrinology PDFDocument272 pagesBorer (2013) Advanced Exercise Endocrinology PDFNicolás Bastarrica100% (1)
- TISSUESDocument19 pagesTISSUESHARETASREE GANESANNo ratings yet
- Muscular System Lesson OverviewDocument31 pagesMuscular System Lesson OverviewBe CalmNo ratings yet
- NCP For Diabetic KetoacidosisDocument2 pagesNCP For Diabetic KetoacidosisLovely Cacapit100% (1)
- Red Urine: Basic (Routine) UrinalysisDocument4 pagesRed Urine: Basic (Routine) UrinalysisMonica DomingoNo ratings yet
- Introduction To Pituitary GlandDocument7 pagesIntroduction To Pituitary GlandRoman KhanNo ratings yet
- Jurnal UtamaDocument9 pagesJurnal UtamarekaNo ratings yet
- Research Paper 1 2Document12 pagesResearch Paper 1 2api-549249381No ratings yet
- The Factors That Affect Plant Growth Can Be Classified As Genetic or EnvironmentalDocument16 pagesThe Factors That Affect Plant Growth Can Be Classified As Genetic or EnvironmentalshadoworacleNo ratings yet
- Developmental Biology GametogenesisDocument14 pagesDevelopmental Biology Gametogenesispragyamaharjan2No ratings yet
- WBC Count: RBC Count, HB, HCT, Blood Indices WBC Count & PLT CountDocument36 pagesWBC Count: RBC Count, HB, HCT, Blood Indices WBC Count & PLT CountppcarpediemNo ratings yet