Professional Documents
Culture Documents
ANS Before 24 Weeks
Uploaded by
madhuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ANS Before 24 Weeks
Uploaded by
madhuCopyright:
Available Formats
Review
Antenatal Corticosteroid Therapy Before
24 Weeks of Gestation
A Systematic Review and Meta-analysis
Christina K. Park, MSc, Tetsuya Isayama, MD, and Sarah D. McDonald, MD, MSc
OBJECTIVE: To evaluate the effectiveness of antenatal outcomes between neonates who received or did not
corticosteroids compared with placebo or no treatment receive antenatal corticosteroids born before 24 weeks
in neonates born before 24 weeks of gestation. of gestation.
DATA SOURCES: We searched MEDLINE, EMBASE, TABULATION, INTEGRATION, AND RESULTS: We per-
Cumulative Index to Nursing and Allied Health formed duplicate independent assessment of the title
Literature (CINAHL), and Cochrane Central Register of and abstracts, full-text screening, inclusion of articles,
Controlled Trials databases from 1990 to March 13, 2015, and data abstraction. We performed meta-analyses using
and ClinicalTrials.gov. random-effects models and quality assessment with the
METHODS OF STUDY SELECTION: Studies considered Grading of Recommendations Assessment, Develop-
were published randomized or quasirandomized con- ment, and Evaluation (GRADE) system. There were 17
trolled trials and observational studies that compared observational studies, and our primary outcome, mor-
tality to discharge in neonates receiving active intensive
From the Departments of Clinical Epidemiology & Biostatistics, Obstetrics &
treatment, had a total of 3,626 neonates. The adjusted
Gynecology, and Radiology, McMaster University, Hamilton, and the Neonatal odds of mortality to discharge were reduced by 52% in
Intensive Care Unit, Sunnybrook Health Science Centre, Toronto, Ontario, Canada. the antenatal corticosteroid group compared with the
The authors thank the authors of the primary studies who provided additional data control group (crude adjusted odds ratio [OR] 0.45, 95%
for the meta-analyses: Drs. Abdel-Latif Mohamed and Kei Lui (New South Wales confidence interval [CI] 0.36–0.56; adjusted OR 0.48, 95%
[NSW] and the Australian Capital Territory [ACT] NICUs Group); Dr. Cüneyt
Tayman (Fatih Universitesi); Drs. David Bader and Brian Reichman (Israel Neo-
CI 0.38–0.61; mortality to discharge 58.1% [intervention]
natal Network); Drs. Gustavo Rocha and Hercília Guimarães (Hospital de São compared with 71.8% [control]) with a “moderate” qual-
João/Faculdade de Medicina, Universidade do Porto); Dr. José Figueras-Aloy ity of evidence based on the GRADE system. There were
(SEN1500 Spanish Neonatal Network); Dr. Karel Marsal (Extremely Preterm no significant differences between the groups for severe
Infants in Sweden Study [EXPRESS] group); Dr. Lilia Vakrilova (Maichin Dom
Neonatology Clinic), Drs. Matthew Laughon, Michael O’Shea (Extremely Low morbidity.
Gestational Age Newborn [ELGAN] study), Elizabeth Allred, and Alan Leviton CONCLUSION: The available data, all observational,
(ELGAN study & Developmental Epidemiology Network); Dr. Reese Clark (Pe-
diatrix Medical Group); Dr. Rintaro Mori (Neonatal Research Network Japan);
show reduced odds of mortality to discharge in
and Dr. Soraya Abbasi and Mr. Emidio Sivieri (Pennsylvania Hospital, University neonates born before 24 weeks of gestation who
of Pennsylvania). The authors also thank the following individuals who have received antenatal corticosteroids and active intensive
assisted us with foreign language articles: Dr. Kari Tikkinen, Dr. Nigar Sekercio- treatment. Antenatal corticosteroids should be con-
glu, Mr. Pavel Roshanov, Dr. Premsyl Bercik, and Ms. Sorina Stef. We value the
contribution of Ms. Neera Bhatnager, BSc, MLIS, Head of Systems, Coordinator of sidered for women at risk of imminent birth before
Research and Graduate Education Support, Health Sciences Library, McMaster 24 weeks of gestation who choose active postnatal
University, for her assistance in developing the search strategies. resuscitation.
Corresponding author: Sarah D. McDonald, MD, MSc, Department of Obstetrics (Obstet Gynecol 2016;127:715–25)
and Gynecology, McMaster University, HSC 3N52B, 1280 Main Street, West,
DOI: 10.1097/AOG.0000000000001355
Hamilton, Ontario, Canada L8S 4K1; e-mail: mcdonals@mcmaster.ca.
Financial Disclosure
Ms. Park is supported by a Canadian Institutes of Health Research (CIHR)
Training Program in Reproduction, Early Development and the Impact on
Health (TGF-96122). Dr. McDonald is supported by a CIHR Canada Research
P reterm birth occurs in 5–18% of births worldwide
and remains the leading cause of neonatal mortal-
ity.1,2 Antenatal corticosteroid therapy is primarily
Chair (950–229920). Dr. Isayama did not report any potential conflicts of
interest. used to accelerate development of the lungs, enhanc-
ing survival of preterm neonates at risk of respiratory
© 2016 by The American College of Obstetricians and Gynecologists. Published
by Wolters Kluwer Health, Inc. All rights reserved. failure.3 The most recent Cochrane review from 2006,
ISSN: 0029-7844/16 which examined antenatal corticosteroids for women
VOL. 127, NO. 4, APRIL 2016 OBSTETRICS & GYNECOLOGY 715
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
at risk of preterm birth, found an overall reduction in STUDY SELECTION
neonatal death, but separate analyses for neonates We included all published observational studies, and
born before 24 weeks of gestation were not available.4 randomized controlled trials (RCTs) and quasi-RCTs,
Given the current evidence, obstetric organizations with no language restrictions. We selected a starting
worldwide5–7 currently advocate for a single course of point of 1990, because there have been substantial
corticosteroids for women between 24 and 34 weeks of advances in neonatal resuscitation in recent years.17
gestation at risk of preterm birth within 7 days. The The population included preterm neonates born
absence of guidance before 24 weeks of gestation is before 24 weeks of gestation. The intervention was
contributing to regional and international variation in the receipt of a single course of antenatal corticoste-
practice,8,9 although there are growing proportions of roids in utero before 24 weeks of gestation for women
neonates receiving intensive care at 22 and 23 weeks of at risk of preterm birth within 7 days before birth. The
gestation. Although these births occur in a small pro- comparator group included those who received no
portion of neonates, they represent a critical group for
treatment or a placebo treatment.
study as a result of its high mortality and morbidity,
Our primary outcome was neonatal mortality up
increased health care costs, and difficult ethical is-
until discharge from the hospital, the period when the
sues.10–13 Therefore, the objective of this systematic
vast majority of deaths occur and allows for robust
review was to estimate the association between neona-
rates of follow-up.18 For the adjusted analysis for mor-
tal mortality and morbidity and receiving antenatal
tality to discharge, we included only the studies with
corticosteroid therapy compared with not receiving
neonates who were given active intensive postnatal
antenatal corticosteroid therapy in neonates born
treatment (resuscitation) and not all liveborn neonates
before 24 weeks of gestation.
because the inclusion of neonates who did not receive
SOURCES treatment may bias the results to overestimate the
benefit of antenatal corticosteroid.19 If information
We followed the guidelines in the Cochrane Hand-
book for Systematic Reviews of Interventions (Ver- for this population was not available in the primary
sion 5.1.0)14 and the Preferred Reporting Items for studies, we contacted the study authors.
Systematic Reviews and Meta-Analyses statement15 The main secondary outcomes were respiratory
(Appendix 1, available online at http://links.lww. distress syndrome (RDS), severe intraventricular hem-
com/AOG/A786). We drafted the protocol for this orrhage (grades III and IV), necrotizing enterocolitis
systematic review before the literature search (Appen- (NEC), chronic lung disease at 36 weeks postmenstrual
dix 2, available online at http://links.lww.com/AOG/ age, retinopathy of prematurity, and neurologic impair-
A786) with the exception of the decision to use the ment. These outcomes were selected for the quality of
Newcastle-Ottawa Scale for individual study risk of evidence assessment using the Grading of Recommen-
bias assessment, which we made before commence- dations Assessment, Development, and Evaluation
ment of data extraction. (GRADE) system. Other secondary outcomes focused
We searched four databases: MEDLINE, EMBASE, on common major morbidities and long-term outcomes.
Cumulative Index to Nursing and Allied Health Liter- We excluded other types of publications (eg,
ature (CINAHL), and the Cochrane Central Register of reviews, editorials, commentaries, case studies, con-
Controlled Trials. We developed separate search strate- ference proceedings, studies published only as ab-
gies with the aid of an experienced research librarian for stracts), studies without sufficient data, and duplicated
each database, consisting of a combination of MeSH studies or data.
headings and multipurpose terms (.mp) (Appendix 3, Two reviewers (C.K.P. and T.I.) independently
available online at http://links.lww.com/AOG/A786). screened the titles and abstracts of all retrieved citations
We searched ClinicalTrials.gov to find completed with a low threshold for selecting studies for full-text
trials that were unpublished using the keywords “ante- review. We independently screened the full texts to
natal corticosteroid.” We consulted experts in mater- determine inclusion and recorded reasons for exclusion.
nal–fetal medicine and early preterm birth for We assessed interreviewer agreement study inclusion
knowledge on studies published in this area. We using k statistics. We considered a k statistic of less than
searched the references of included studies for addi- 0.00, 0.00–0.20, 0.21–0.40, 0.41–0.60, 0.61–0.80, and
tional articles of interest. 0.81–1.00 as “poor,” “slight,” “fair,” “moderate,” “sub-
We imported all citations into bibliographic stantial,” and “almost perfect” agreement, respectively.20
software (Endnote X7),16 removed duplicates, and as- We developed a data collection form and each
signed each article an identification number. reviewer piloted the form before data abstraction of
716 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks OBSTETRICS & GYNECOLOGY
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
included studies. We extracted the following character- interest was not present at the start of the study, was
istics from the included studies: first author and year of excluded, because neonatal outcomes would not have
publication, study design, country or region, years of been present at the time of administration of antenatal
study, final sample size, inclusion and exclusion criteria, corticosteroids. The most important confounder for
description of intervention, and outcome measures. We the comparability criteria was gestational age, and
resolved discrepancies between reviewers through secondary important confounders were inborn or
discussion and consensus. A third reviewer (S.D.M.) outborn status and mode of delivery (by adjustment,
resolved any disagreements or uncertainties. For the matching, stratification or exclusion) chosen in con-
primary outcome, we included only neonates who sultation with a high-risk obstetrician (S.D.M.) and
received active treatment to avoid a potential over- neonatologist (T.I.). Outcomes were assessed sepa-
estimation of the effect caused by including those who rately for the outcome criteria. Overall, modified
did not receive active treatment. Authors of primary awarded up to 8 points. We selected a score of greater
studies were contacted and the study was excluded if it than 5 as the cutoff for low risk of bias, because there
was not possible to obtain these data. are no validation studies that provide a cutoff score.
We summarized the data quantitatively. Because The GRADE system measures the quality of
between-study heterogeneity was anticipated, we a body of evidence, the confidence that an effect size
performed meta-analyses using random-effects mod- for a certain outcome is close to that of the inter-
els, implementing an inverse variance method, which vention’s true effect.14,25 We rated the quality of evi-
adjusts study weights according to the magnitude of dence for each outcome as high, moderate, low, or
variation among the intervention effects and could be very low.26 Randomized controlled trials initially
considered more conservative.14 We planned separate begin with a high quality of evidence and are down-
analyses for RCTs and observational studies. We gen- graded if necessary, whereas observational studies
erated summary effect estimates (relative risks or odds start with a low quality of evidence and could be up-
ratios and standardized mean differences) with associ- graded or downgraded.
ated 95% confidence intervals (CIs) for each outcome. The quality of evidence is downgraded in the
We pooled unadjusted (the raw number of events and presence of risk of bias, inconsistency, indirectness,
total) and adjusted analyses separately, if available. imprecision, and publication bias. We assessed risk of
The adjusted analyses were preferred because they bias with the modified Newcastle-Ottawa Scale; incon-
are an indication of the independent effect of antenatal sistency with high heterogeneity indicated by I2 values
corticosteroids after accounting for confounders. unexplained by subgroup analyses27; indirectness with
We performed all analyses using Review Man- differences in population, intervention, or outcome, or
ager 5.3.21 We estimated statistical significance using indirect comparison28; imprecision with whether opti-
a two-sided P value of .05. As is typical in meta- mal information sizes were met and whether the 95%
analyses, we did not adjust the P value for multiple CIs overlapped no effect or failed to exclude appreciable
secondary outcomes. benefit or harm29; and publication bias with funnel plots
We assessed heterogeneity using I2 statistics. I2 and industry sponsorships.30 The optimal information
values of 0–40%, 30–60%, 50–90%, and 75–100% size is the required sample size for a meta-analysis. We
were considered low, moderate, substantial, and con- calculated the optimal information sizes based on a 20%
siderable heterogeneity, respectively.14 The a priori relative risk reduction with a50.05 and b50.20.29 The
hypotheses of sources of significant heterogeneity quality of evidence is upgraded in the presence of a large
were gestational age or multiple birth. Therefore, effect size and a dose–response and if all plausible con-
where possible, we performed subgroup analyses for founding would reduce a demonstrated effect or would
gestational age and singleton or multiple pregnancies. suggest a spurious effect when results show no effect.26
Two of the authors (C.K.P. and T.I.) independently We summarized the results of the meta-analyses and
assessed risk of bias for each study using the Cochrane assessment of quality of evidence for each outcome
Collaboration’s tool for assessing risk of bias for RCTs across included studies using GRADEpro GDT.31
and quasi-RCTs and a modified version of the
Newcastle-Ottawa Scale for observational studies.22,23 RESULTS
We quantitatively assessed publication bias with a fun- The searches yielded 6,435 articles (MEDLINE51,929,
nel plot for outcomes with 10 or more studies.24 EMBASE53,887, Cochrane Central Register of Con-
The Newcastle-Ottawa Scale assesses selection, trolled Trials5173, CINAHL5446; March 13, 2015;
comparability, and outcome. One of the items to Fig. 1) with 12 additional articles from ClinicalTrials.
assess selection bias, demonstration that outcome of gov. After removing duplicates, 4,479 records
VOL. 127, NO. 4, APRIL 2016 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks 717
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
remained. There was full-text screening for 129 records, To ensure accuracy, we requested that the authors run
and 17 studies were included18,32–47 with “substantial” the same statistical analysis as the primary study with
agreement between reviewers (unweighted k50.62). the same data set used in the publication, but only with
The most common reason for exclusion was because neonates who received active intensive treatment. We
data were unavailable for neonates born before 24 specifically requested authors to not include additional
weeks of gestation. An RCT protocol was identified data collected in subsequent years after the primary
in ClinicalTrials.gov, but the recruitment start date study publication.
was April 2015 and thus was not considered for this Years of study were from 1991 to 2010 and
review. This RCT has since been withdrawn.48 When- published from 1999 to 2014 (Appendix 4, available
ever applicable, authors of the original studies were online at http://links.lww.com/AOG/A786). There
contacted by e-mail for data only on neonates born were three prospective and 14 retrospective observa-
before 24 weeks of gestation. Twelve research teams tional studies. Six studies were from the United States,
clarified data and, where requested, contributed unpub- two from Australia, and one each from the United
lished data on the less than 24 weeks of gestation Kingdom, Portugal, Spain, Sweden, Bulgaria, Canada,
population.33–39,41,42,44,45,47 For the primary outcome, Japan, Israel, and Turkey. There were 3,626 neonates
all of the data were contributed by the author of the for the primary outcome. Six studies had birth weight
primary studies, except for one study, which already as part of the inclusion criteria (eg, 1,500 g or
included only neonates who received active intensive less).18,33,35,36,38,47 Studies that included dosage had typ-
resuscitation in both intervention and control groups.18 ically two doses of betamethasone 24 hours apart or
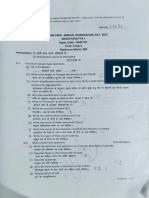
Fig. 1. Flow diagram of study selec-
tion process. CENTRAL, Cochrane
Central Register of Controlled Trials;
CINAHL, Cumulative Index to Nurs-
ing and Allied Health Literature.
Park. Antenatal Corticosteroid Therapy
Before 24 Weeks. Obstet Gynecol 2016.
718 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks OBSTETRICS & GYNECOLOGY
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Fig. 2. Summary of adjusted pooled odds ratios (95% confidence interval [CI]) for the association between mortality to
discharge and antenatal corticosteroid (ANCS) therapy compared with not receiving antenatal corticosteroid therapy. IV,
inverse variance; df, degrees of freedom.
Park. Antenatal Corticosteroid Therapy Before 24 Weeks. Obstet Gynecol 2016.
two to four doses of dexamethasone 12 hours apart, study, because 1) it provided a composite outcome of
totaling 24 mg.32,34,37,42–44,47 both intraventricular hemorrhage or periventricular
The data for two outcomes—severe intraventricular leukomalacia instead of only intraventricular hemor-
hemorrhage or periventricular leukomalacia and NEC— rhage; and 2) the study provided the rate of both out-
were not included from Carlo 2011,18 the largest comes among neonatal intensive care unit survivors
Fig. 3. Summary of adjusted pooled odds ratios (95% confidence interval [CI]) for the association between respiratory
distress syndrome and antenatal corticosteroid (ANCS) therapy compared with not receiving antenatal corticosteroid
therapy. IV, inverse variance; df, degrees of freedom.
Park. Antenatal Corticosteroid Therapy Before 24 Weeks. Obstet Gynecol 2016.
VOL. 127, NO. 4, APRIL 2016 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks 719
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Fig. 4. Summary of adjusted pooled odds ratios (95% confidence interval [CI]) for the association between severe intra-
ventricular hemorrhage (grades III and IV) and antenatal corticosteroid (ANCS) therapy compared with not receiving
antenatal corticosteroid therapy. IV, inverse variance; df, degrees of freedom.
Park. Antenatal Corticosteroid Therapy Before 24 Weeks. Obstet Gynecol 2016.
and not for all neonates including those who died. Neo- http://links.lww.com/AOG/A786). In the “selection”
nates with intraventricular hemorrhage, periventricular category: 1) most studies included an exposed cohort
leukomalacia, and NEC have a high risk of death after that was truly or at least somewhat representative of
developing these complications,49,50 and thus including average pregnant women in a community, and in all
only neonates who survived could lead to bias. studies; 2) the nonexposed cohort was always drawn
The outcomes of all but four studies had a low from the same community; and 3) the ascertainment of
risk of bias according to the modified Newcastle- receiving the antenatal corticosteroid therapy during
Ottawa Scale (Appendix 5, available online at pregnancy was assessed using secure records. For
Fig. 5. Summary of adjusted pooled odds ratios (95% confidence interval [CI]) for the association between necrotizing
enterocolitis and antenatal corticosteroid (ANCS) therapy compared with not receiving antenatal corticosteroid therapy. IV,
inverse variance; df, degrees of freedom.
Park. Antenatal Corticosteroid Therapy Before 24 Weeks. Obstet Gynecol 2016.
720 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks OBSTETRICS & GYNECOLOGY
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Fig. 6. Summary of adjusted pooled odds ratios (95% confidence interval [CI]) for the association between chronic lung
disease and antenatal corticosteroid (ANCS) therapy compared with not receiving antenatal corticosteroid therapy. IV,
inverse variance; df, degrees of freedom.
Park. Antenatal Corticosteroid Therapy Before 24 Weeks. Obstet Gynecol 2016.
“comparability”: 1) every study addressed gestational correspondence); but 2) only four studies controlled for
age, either through adjusted analysis or by stratifying inborn and outborn status or mode of delivery.18,33,45,46
data to 22–23 weeks of gestation (in publication or by Regarding “adequacy of follow-up”: Vakrilova et al36
Table 1. Summary of Adjusted Findings in a Systematic Review of Antenatal Corticosteroids in Neonates
Born Before 24 Weeks of Gestation (Grading of Recommendations Assessment, Development,
and Evaluation)
Anticipated Absolute Effects*
(95% CI)
No Adjusted OR No. of Participants Quality of
Outcome Corticosteroids Corticosteroids (95% CI) (No. of Studies) Evidence
Mortality before 718/1,000 555/1,000 (505–600) 0.48 (0.38–0.61)† 3,646 (4) Moderate
discharge
Respiratory distress NA NA 1.09 (0.69–1.73) 739 (2) Very low‡
syndrome
Intraventricular NA NA 0.82 (0.55–1.21) 737 (2) Very low§
hemorrhage
Necrotizing enterocolitis NA NA 1.46 (0.86–2.48) 917 (3) Very low¶
Chronic lung disease 785/1,000 756/1,000 (694–809) 0.85 (0.62–1.16) 1,184 (3) Very lowk
ROP, stages greater than 2 NA NA 0.76 (0.11–5.43) NA (1) Very low#
Neurologic impairment, 562/1,000 587/1,000 (490–680) 1.11 (0.75–1.66) 601 (1) Very low#
18–22 mo
CI, confidence interval; OR, odds ratio; NA, not available; ROP, retinopathy of prematurity.
* The risk in the intervention group is based on the assumed risk in the comparison group and the relative effect of the intervention.
†
Statistically significant.
‡
Optimal information sizes (OIS) was met, and CI overlapped no effect and failed to exclude appreciable benefit or harm.
§
OIS was not met, and CI overlapped no effect and failed to exclude appreciable benefit.
k
OIS was not met, and CI overlapped no effect and failed to exclude appreciable benefit or harm.
¶
OIS was met, but CI overlapped no effect and failed to exclude appreciable benefit.
#
Not enough information to calculate OIS, and CI overlapped no effect and failed to exclude appreciable benefit or harm.
VOL. 127, NO. 4, APRIL 2016 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks 721
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
received 5 points for mortality, because there was no to have very low quality of evidence because they
information on the adequacy of follow-up, and 4 points were downgraded from low to very low because of
for severe intraventricular hemorrhage, because there serious or very serious imprecision (Table 1; Appen-
was no information provided for both the length and dix 7, http://links.lww.com/AOG/A786).
adequacy of follow-up. Abbasi et al37 received 4 points The risk of bias for all outcomes included for the
for RDS and severe intraventricular hemorrhage, the GRADE assessment was not serious. Inconsistency
former as a result of poor assessment of outcome and was considered not serious for all outcomes because
the latter as a result of inadequate follow-up of the they all had low values of heterogeneity. All outcomes
cohort. For mortality to discharge, all studies received received a not serious allocation for indirectness. The
points for the assessment of outcome, length of follow- imprecision for the outcomes other than mortality to
up, and follow-up. discharge was considered serious or very serious
The odds of mortality to discharge were halved because their optimal information sizes were not
(reduced by 52%) in the antenatal corticosteroid met or the 95% CI of the adjusted OR overlapped
group compared with the control group in the no effect and failed to exclude appreciable benefit
adjusted analysis among neonates who received active (adjusted OR 0.75) or harm (adjusted OR 1.25).29 No
intensive treatment (58.1% compared with 71.8%, outcome was downgraded for publication bias
adjusted OR 0.48 [95% CI 0.38–0.61]; Fig. 2). The because there were too few studies for funnel plots.
subgroup analysis stratified by gestational age (22 There were no industry sponsorships.
and 23 weeks of gestation) found no significant differ-
ence between the subgroups (P5.19; Fig. 2). Although DISCUSSION
the result became nonsignificant in 22 weeks of gesta- In our analysis, which consisted exclusively of
tion (adjusted OR 0.66, 95% CI 0.40–1.07), the 34% observational data, we found a halving of the odds
reduction of the adjusted OR estimate indicated of mortality to discharge in neonates before 24 weeks
a potential large effect of antenatal corticosteroids in of gestation who received antenatal corticosteroids
this group. In the unadjusted analyses, which included compared with those who did not. The subgroup
more studies, a similar significant reduction in the analysis at 22 compared with 23 weeks of gestation
odds of mortality was observed before 24 weeks of found no difference in mortality to discharge. How-
gestation (OR 0.45 [95% CI 0.36–0.46]) as well as ever, more data are needed, because the sample size
for each individual week of gestation (Appendix 6, for 22 weeks of gestation was small and the CIs
available online at http://links.lww.com/AOG/ around the adjusted, but not the unadjusted, odds
A786). Subgroup analyses for singleton compared included the null value. At 22 weeks of gestation, the
with multiples were not conducted because the pri- fetus has limited but detectable alveolar develop-
mary studies did not provide data, although some ment.51 The fetal lung at 22–23 weeks of gestation is
controlled for this in the adjusted analyses. at the end stage of the canalicular stage (16–24 weeks
There were no differences in secondary outcomes of gestation) of lung development followed by the
including RDS (adjusted OR 1.09 [95% CI 0.69– saccular stage (24–40 weeks of gestation). Because
1.73]), severe intraventricular hemorrhage (adjusted these critical lung developments start during the
OR 0.82 [95% CI 0.55–1.21]), NEC (adjusted OR end of the canalicular stage (22–24 weeks of gesta-
1.46 [95% CI 0.86–2.48]), chronic lung disease at 36 tion),52 neonates at 22–23 weeks of gestation are con-
weeks postmenstrual age (adjusted OR 0.85 [95% CI sidered potentially viable.
0.62–1.16]), severe retinopathy of prematurity No significant reduction in secondary outcomes
(adjusted OR 0.76 [95% CI 0.11–5.43]; for stages in the steroid group was contrary to a hypothesis that
greater than II only because data for all stages were the reduction of morbidities would lead to lower odds
not available), and neurodevelopmental impairment of mortality. This may be because the optimal
at 18–22 months corrected age (adjusted OR 1.11 information sizes were not met for these secondary
[95% CI 0.75–1.66]; Figs. 3–6). Data for pneumotho- outcomes, unlike the primary outcome, indicating
rax or air leak syndrome were not available. Data for insufficient sample sizes. Another possible explana-
all other secondary outcomes are in Appendices 6–41, tion may be the misdiagnosis of RDS. It may be
available online at http://links.lww.com/AOG/A786. difficult to ascertain RDS at 22–23 weeks of gestation
The primary outcome of mortality to discharge if neonates immediately intubated and administered
had a moderate quality of evidence because it was surfactant as would occur in many institutions.
upgraded from low to moderate as a result of the large Slightly more mature neonates are often managed
effect size. All secondary outcomes were considered without intubation, making the diagnosis of RDS
722 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks OBSTETRICS & GYNECOLOGY
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
potentially easier. A third possibility is that cortico- health care providers, the health care system, and society
steroids are not effective at lowering morbidity in neo- are challenged by births occurring in the periviable
nates delivered before 24 weeks of gestation. period in terms of both their health and other effects.10,11
Our results differed from two previous systematic The results of this systematic review indicate that ante-
reviews examining outcomes of extremely preterm natal corticosteroids may be effective in reducing mor-
birth, beginning at 24 weeks of gestation.4,53 The 2006 tality in neonates born before 24 weeks of gestation.
Cochrane review4 found that neonatal mortality was
significantly reduced with antenatal corticosteroids REFERENCES
before 32, 34, and 36 weeks of gestation, but not in 1. Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB,
the two studies of 89 neonates at 24 to less than 28 Narwal R, et al. National, regional, and worldwide estimates of
weeks of gestation (relative risk 0.79 [95% CI 0.56– preterm birth rates in the year 2010 with time trends since 1990
for selected countries: a systematic analysis and implications.
1.12]). A more recent 2011 systematic review,53 also Lancet 2012;379:2162–72.
of RCTs, did not find a significant reduction in neo-
2. Kramer MS, Demissie K, Yang H, Platt RW, Sauvé R, Liston R.
natal mortality in pooled analyses of two studies with The contribution of mild and moderate preterm birth to infant
173 neonates at 24–29 weeks of gestation (relative risk mortality. Fetal and Infant Health Study Group of the Canadian
0.86 [95% CI 0.48–1.53]). The point estimates of both Perinatal Surveillance System. JAMA 2000;284:843–9.
meta-analyses were similar, but the sample sizes were 3. Liggins GC, Howie RN. A controlled trial of antepartum glu-
cocorticoid treatment for prevention of the respiratory distress
modest. Further research is needed to investigate syndrome in premature infants. Pediatrics 1972;50:515–25.
short- and long-term morbidity. 4. Roberts D, Dalziel S. Antenatal corticosteroids for accelerating
A strength of this systematic review is the subgroup fetal lung maturation for women at risk of preterm birth. The
analysis for 22 and 23 weeks of gestation, which is Cochrane Database of Systematic Reviews 2006, Issue 3. Art.
No.: CD004454.
clinically relevant. Studies were from diverse settings,
which increased generalizability. We performed the risk 5. Periviable birth. Obstetric Care Consensus No. 3. American
College of Obstetricians and Gynecologists. Obstet Gynecol
of bias in individual studies and the quality of evidence 2015;126:e82–94.
for outcomes. Our primary outcome was well powered, 6. Crane J, Armson A, Brunner M, De La Ronde S, Farine D,
exceeding the optimal information size. For the primary Keenan-Lindsay L, et al. Antenatal corticosteroid therapy for
outcome, we included only neonates who received fetal maturation [in English, French]. J Obstet Gynaecol Can
2003;25:45–52.
active treatment to avoid a potential overestimation of
7. Antenatal corticosteroids to reduce neonatal morbidity and
the effect caused by including those who did not receive mortality. Green-top Guideline No. 7. London (UK): Royal
active treatment. Including only neonates who received College of Obstetricians and Gynaecologists; 2010.
active intensive treatment rather than expectant man- 8. Miracle X, Di Renzo GC, Stark A, Fanaroff A, Carbonell-
agement in both antenatal corticosteroid and control Estrany X, Saling E, et al. Guideline for the use of antenatal
groups minimizes selection bias favoring corticoste- corticosteroids for fetal maturation. J Perinat Med 2008;36:191–6.
roids. Adjusted data were pooled separately from 9. Leviton LC, Goldenberg RL, Baker CS, Schwartz RM,
Freda MC, Fish LJ, et al. Methods to encourage the use of
unadjusted data to estimate the independent effect of antenatal corticosteroid therapy for fetal maturation: a random-
antenatal corticosteroids to understand the absolute and ized controlled trial. JAMA 1999;281:46–52.
relative effects for survival. A limitation was that many 10. Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al.
of the secondary outcomes lacked data with some Between-hospital variation in treatment and outcomes in
extremely preterm infants. N Engl J Med 2015;372:1801–11.
outcomes only containing one study, and all had “very
low” quality of evidence. The studies that contributed to 11. Salihu HM, Salinas-Miranda AA, Hill L, Chandler K. Survival
of pre-viable preterm infants in the United States: a systematic
the adjusted analyses did not always control for the review and meta-analysis. Semin Perinatol 2013;37:389–400.
same confounding variables. Some clinically relevant 12. Institute of Medicine (US) Committee on Understanding Pre-
aspects of care not reported included the time from mature Birth and Assuring Healthy Outcomes; Behrman RE,
administration of steroids to birth, use of surfactant, Butler AS, editors. Preterm Birth: Causes, Consequences, and
Prevention. Washington (DC): National Academies Press (US);
and use of magnesium sulfate for neonatal neuroprotec- 2007.
tion. Only observational studies have been published, 13. Fanaroff JM, Hascoet JM, Hansen TW, Levene M, Norman M,
which are not as robust as RCTs. Papageorgiou A, et al. The ethics and practice of neonatal resus-
Although variation exists in the literature on the citation at the limits of viability: an international perspective.
Acta Paediatr 2014;103:701–8.
survival rates of neonates born before at 24 weeks of
14. Higgins JPT, Green S. Cochrane handbook for systematic re-
gestation, it is agreed that family counseling and planning
views of interventions version 5.1.0. Available at: www.co-
of services are essential for these births,11,54 because ad- chrane-handbook.org. 2011. Retrieved February 12, 2016.
vances in care have opened the possibility of survival at 15. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group.
progressively early gestations. Increasingly, parents, Preferred reporting items for systematic reviews and
VOL. 127, NO. 4, APRIL 2016 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks 723
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 34. Rocha G, Guimarães H. On the limit of viability extremely low
62:1006–12. gestational age at birth. Acta Med Port 2011;24(suppl 2):181–8.
16. EndNote X7. Available at: http://endnote.com/product-de- 35. Tayman C, Tonbul A, Uras N, Kahveci H, Koseoglu B,
tails/X7. Thomson Reuters; 2014. Retrieved February 12, Mansur Tatli M. Evaluation of risk factors for necrotizing
2016. enterocolitis in preterm infants [in Turkish]. Guncel Pediatri
17. Morley CJ, Davis PG. Advances in neonatal resuscitation: support- 2011;9:7–13.
ing transition. Arch Dis Child Fetal Neonatal Ed 2008;93:F334–6. 36. Vakrilova L, Nikolov A, Yankova Y, Slancheva B,
Popivanova A, Frandeva B, et al. Short term outcome after
18. Carlo WA, McDonald SA, Fanaroff AA, Vohr BR, Stoll BJ,
active obstetric management of very low birthweight infants
Ehrenkranz RA, et al. Association of antenatal corticosteroids
[in Bulgarian]. Akush Ginekol (Sofiia) 2011;50:13–20.
with mortality and neurodevelopmental outcomes among in-
fants born at 22 to 25 weeks’ gestation. JAMA 2011;306: 37. Abbasi S, Oxford C, Gerdes J, Sehdev H, Ludmir J. Antenatal
2348–58. corticosteroids prior to 24 weeks’ gestation and neonatal out-
come of extremely low birth weight infants. Am J Perinatol
19. Litmanovitz I, Reichman B, Arnon S, Boyko V, Lerner-Geva L,
2010;27:61–6.
Bauer-Rusak S, et al. Perinatal factors associated with active
intensive treatment at the border of viability: a population- 38. Bader D, Kugelman A, Boyko V, Levitzki O, Lerner-Geva L,
based study. J Perinatol 2015;35:705–11. Riskin A, et al. Risk factors and estimation tool for death among
extremely premature infants: a national study. Pediatrics 2010;
20. Landis JR, Koch GG. The measurement of observer agreement
125:696–703.
for categorical data. Biometrics 1977;33:159–74.
39. Garg P, Abdel-Latif ME, Bolisetty S, Bajuk B, Vincent T, Lui K.
21. Zhang J, Yu KF. What’s the relative risk? A method of correct-
Perinatal characteristics and outcome of preterm singleton, twin
ing the odds ratio in cohort studies of common outcomes. JA-
and triplet infants in NSW and the ACT, Australia (1994-2005).
MA 1998;280:1690–1.
Arch Dis Child Fetal Neonatal Ed 2010;95:F20–4.
22. Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D,
40. Manktelow BN, Lal MK, Field DJ, Sinha SK. Antenatal cortico-
Oxman AD, et al. The Cochrane Collaboration’s tool for as-
steroids and neonatal outcomes according to gestational age:
sessing risk of bias in randomised trials. BMJ 2011;343:d5928.
a cohort study. Arch Dis Child Fetal Neonatal Ed 2010;95:
23. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, F95–8.
et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality
41. EXPRESS Group, Fellman V, Hellström-Westas L, Norman M,
of nonrandomised studies in meta-analyses. Available at: http://
Westgren M, Källén K, et al. One-year survival of extremely
www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Ottawa
preterm infants after active perinatal care in Sweden. JAMA
Hospital Research Institute; Retrieved February 12, 2016.
2009;301:2225–33.
24. Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J,
42. Laughon M, O’Shea MT, Allred EN, Bose C, Kuban K, Van
et al. Recommendations for examining and interpreting funnel
Marter LJ, et al. Chronic lung disease and developmental delay
plot asymmetry in meta-analyses of randomised controlled tri-
at 2 years of age in children born before 28 weeks’ gestation.
als. BMJ 2011;343:d4002.
Pediatrics 2009;124:637–48.
25. The GRADE working group. GRADE working group.
43. Hayes EJ, Paul DA, Stahl GE, Seibel-Seamon J, Dysart K,
Available at: http://www.gradeworkinggroup.org/index.htm.
Leiby BE, et al. Effect of antenatal corticosteroids on survival
Retrieved February 12, 2016.
for neonates born at 23 weeks of gestation. Obstet Gynecol
26. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. 2008;111:921–6.
GRADE guidelines: 1. Introduction-GRADE evidence profiles
44. Figueras-Aloy J, Serrano MM, Rodriguez JP, Pérez CF,
and summary of findings tables. J Clin Epidemiol 2011;64:383–94.
Serradilla VR, Jimenez JQ, et al. Antenatal glucocorticoid treat-
27. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, ment decreases mortality and chronic lung disease in survivors
Helfand M, et al. GRADE guidelines: 7. Rating the quality of among 23- to 28-week gestational age preterm infants. Am J
evidence–inconsistency. J Clin Epidemiol 2011;64:1294–302. Perinatol 2005;22:441–8.
28. Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, 45. Guthrie SO, Gordon PV, Thomas V, Thorp JA, Peabody J,
Helfand M, et al. GRADE guidelines: 8. Rating the quality of Clark RH. Necrotizing enterocolitis among neonates in the
evidence–indirectness. J Clin Epidemiol 2011;64:1303–10. United States. J Perinatol 2003;23:278–85.
29. Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, 46. Chien LY, Ohlsson A, Seshia MM, Boulton J, Sankaran K,
Rind D, et al. GRADE guidelines 6. Rating the quality of evi- Lee SK, et al. Variations in antenatal corticosteroid therapy:
dence–imprecision. J Clin Epidemiol 2011;64:1283–93. a persistent problem despite 30 years of evidence. Obstet Gy-
30. Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, necol 2002;99:401–8.
et al. GRADE guidelines: 5. Rating the quality of evidence– 47. Leviton A, Dammann O, Allred EN, Kuban K, Pagano M,
publication bias. J Clin Epidemiol 2011;64:1277–82. Van ML, et al. Antenatal corticosteroids and cranial ultrasono-
31. McMaster University and Evidence Prime Inc. GRADEpro graphic abnormalities. Am J Obstet Gynecol 1999;181:1007–17.
GDT. Available at: http://gradepro.org/. Retrieved February 48. Mednax Center for Research EaQ. Effectiveness of ACS in
12, 2016. extreme preemies. Available at: https://clinicaltrials.gov/ct2/
32. Wong D, Abdel-Latif M, Kent A; NICUS Network. Antenatal show/NCT02351310. Retrieved February 12, 2016.
steroid exposure and outcomes of very premature infants: 49. Kono Y, Mishina J, Yonemoto N, Kusuda S, Fujimura M; NI-
a regional cohort study. Arch Dis Child Fetal Neonatal Ed CU Network, Japan. Neonatal correlates of adverse outcomes
2014;99:F12–20. in very low-birthweight infants in the NICU Network. Pediatr
33. Mori R, Kusuda S, Fujimura M; Neonatal Research Network Int 2011;53:930–5.
Japan. Antenatal corticosteroids promote survival of extremely 50. Fitzgibbons SC, Ching Y, Yu D, Carpenter J, Kenny M,
preterm infants born at 22 to 23 weeks of gestation. J Pediatr Weldon C, et al. Mortality of necrotizing enterocolitis expressed
2011;159:110–114.e1. by birth weight categories. J Pediatr Surg 2009;44:1072–5.
724 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks OBSTETRICS & GYNECOLOGY
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
51. Chetty A, Andersson S, Lassus P, Nielsen HC. Insulin-like a systematic review of randomized controlled trials. Am J Peri-
growth factor-1 (IGF-1) and IGF-1 receptor (IGF-1R) expres- natol 2011;28:33–44.
sion in human lung in RDS and BPD. Pediatr Pulmonol 2004;
54. Raju TN, Mercer BM, Burchfield DJ, Joseph GF. Periviable
37:128–36.
birth: executive summary of a Joint Workshop by the Eunice
52. Blackmon LR. Biologic limits of viability. NeoReviews 2003;4: Kennedy Shriver National Institute of Child Health and Human
e140–6. Development, Society for Maternal-Fetal Medicine, American
53. Onland W, de Laat MW, Mol BW, Offringa M. Effects of Academy of Pediatrics, and American College of Obstetricians
antenatal corticosteroids given prior to 26 weeks’ gestation: and Gynecologists. J Perinatol 2014;34:333–42.
ACOG Fellows and Journal Subscribers:
Get Obstetrics & Gynecology for Free on your iPad
The Green Journal app is available for the iPad® from Apple’s App StoreSM. To view journal
content, ACOG Fellows and journal subscribers must first register and activate an account
at www.greenjournal.org.
If You Have Not Registered at GreenJournal.org:
1. On www.greenjournal.org, click on the gear box at the top right corner of the screen
and select Register.
2. On the registration screen, choose a username and password and enter your e-mail
address. (Usernames must be at least 6 characters in length and contain no spaces or
symbols; passwords must be at least 8 characters in length and contain at least one
number and one letter.)
3. Click Continue to go to the next step of user registration.
4. On the next screen, enter your name and address and click Continue.
5. The next registration screen asks for additional information about you and your
practice to help us recommend articles and rich media that suit your area of specialty.
After entering this information, indicate your acceptance of the End User License
Agreement and click Complete Registration.
6. After you complete the registration, you will receive an e-mail from the site asking you
to confirm your registration. Click on the link in the e-mail within 48 hours.
7. The link in the e-mail leads to a web page where you will be asked if you want to
activate your online subscription. Click on Yes! I am a subscriber and want to activate
my online subscription.
8. Enter your ACOG Member ID or subscriber ID in the field at the bottom of the next
screen. Be sure to enter all characters; note that the last digit for ACOG members is the
letter “I,” not the number “1.” Then click on Activate Subscription.
If You Have Registered at GreenJournal.org But Not Activated Your Subscription:
1. On www.greenjournal.org, click on the gear box at the top right corner of the screen
and select Register.
2. Click on Activate Your Subscription at the top right of the page.
3. Enter your ACOG Member ID or subscriber ID in the field at the bottom of the next
screen. Be sure to enter all characters; note that the last digit for ACOG members is the
letter “I,” not the number “1.” Then click on Activate Subscription.
You are now registered for full-text access on both the app and the journal web site!
When you access the Green Journal app on your iPad, you will be asked to enter the
username and password that you created at www.greenjournal.org.
Need Help? Contact the Editorial Office at 202-314-2317 or obgyn@greenjournal.org.
Apple and iPad are trademarks of Apple Inc., registered in the U. S. and other countries. App Store is a service mark of Apple Inc.
rev 2/2015
VOL. 127, NO. 4, APRIL 2016 Park et al Antenatal Corticosteroid Therapy Before 24 Weeks 725
Copyright ª by The American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
You might also like
- Antenatal Corticosteroids: An Assessment of Anticipated Benefits and Potential RisksDocument13 pagesAntenatal Corticosteroids: An Assessment of Anticipated Benefits and Potential RiskssaryindrianyNo ratings yet
- Antenatal CorticosteroidsDocument17 pagesAntenatal CorticosteroidsRolando DiazNo ratings yet
- Antenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?Document8 pagesAntenatal Corticosteroids Beyond 34 Weeks Gestation: What Do We Do Now?XIMENAGILDANo ratings yet
- Maduracion Pulmonar Jurnal Obstetric CanadaDocument21 pagesMaduracion Pulmonar Jurnal Obstetric CanadaSoy PatoNo ratings yet
- Grabovac 2017Document12 pagesGrabovac 2017Karindha Handayani HelisusantoNo ratings yet
- Maternal and Perinatal Outcomes After Elective Labor Induction at 39 Weeks in Uncomplicated Singleton Pregnancies - A Meta-Analysis-sotiriadis2018Document27 pagesMaternal and Perinatal Outcomes After Elective Labor Induction at 39 Weeks in Uncomplicated Singleton Pregnancies - A Meta-Analysis-sotiriadis2018trongnguyen2232000No ratings yet
- Antenatal Betamethasone For Women at RiskDocument10 pagesAntenatal Betamethasone For Women at RiskThapakorn JalearnyingNo ratings yet
- Pi Is 0002937813006170Document7 pagesPi Is 0002937813006170Raisa AriesthaNo ratings yet
- Antenatal Dexamethasone For Early Preterm Birth in Low-Resource CountriesDocument12 pagesAntenatal Dexamethasone For Early Preterm Birth in Low-Resource CountriesMemento MoriNo ratings yet
- Uog 20140Document11 pagesUog 20140vincentharlling90No ratings yet
- Pi Is 0002937810000815 JournallDocument12 pagesPi Is 0002937810000815 JournallRaisa AriesthaNo ratings yet
- Walters - Et - Al-2022-Cochrane - Database - of - Systematic - Reviews (1) - Digabungkan-DikonversiDocument5 pagesWalters - Et - Al-2022-Cochrane - Database - of - Systematic - Reviews (1) - Digabungkan-DikonversiSulung AnugrahNo ratings yet
- Corticoides PrenatalesDocument13 pagesCorticoides PrenatalesGraciela FissoreNo ratings yet
- Clinical Assessment of Fetal Well-Being and FetalDocument12 pagesClinical Assessment of Fetal Well-Being and Fetalhenri kaneNo ratings yet
- Antenatal Corticosteroids For Accelerating Fetal Lung Maturation For Women at Risk of Preterm Birth - McGoldrick, E - 2020 Cochrane LibraryDocument88 pagesAntenatal Corticosteroids For Accelerating Fetal Lung Maturation For Women at Risk of Preterm Birth - McGoldrick, E - 2020 Cochrane Libraryjavier dauvergneNo ratings yet
- Nejme2032499 PDFDocument2 pagesNejme2032499 PDFBladimir CentenoNo ratings yet
- Al Riyami-2020-Respiratory Distress Syndrome IDocument6 pagesAl Riyami-2020-Respiratory Distress Syndrome IHidayatt NurulNo ratings yet
- 9 Antenatal Corticosteroid Green Top PDFDocument13 pages9 Antenatal Corticosteroid Green Top PDFangela_karenina_1No ratings yet
- Safety of Vaginal Birth After Cesarean: A Systematic ReviewDocument10 pagesSafety of Vaginal Birth After Cesarean: A Systematic ReviewAnonymous EfZtL8No ratings yet
- Antenatal Betamethasone For WomenDocument10 pagesAntenatal Betamethasone For WomenMarcela Garzon O VelezNo ratings yet
- Between-Hospital Variation in Treatment and Outcomes in Extremely Preterm InfantsDocument11 pagesBetween-Hospital Variation in Treatment and Outcomes in Extremely Preterm InfantsAstri Faluna SheylavontiaNo ratings yet
- Risk and Benefit of CSDocument22 pagesRisk and Benefit of CSbudi haryadiNo ratings yet
- Risk and Benefit of CSDocument22 pagesRisk and Benefit of CSbudi haryadiNo ratings yet
- Preeclampsia Screening Evidence Report and Systematic Review For The US Preventive Services Task ForceDocument16 pagesPreeclampsia Screening Evidence Report and Systematic Review For The US Preventive Services Task ForceRoberto López MataNo ratings yet
- Steroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanDocument23 pagesSteroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanMichaela Vania TanujayaNo ratings yet
- Journal Pone 0248588Document21 pagesJournal Pone 0248588Intan FairuzNo ratings yet
- Esteroides Canada 2019Document21 pagesEsteroides Canada 2019Ana Isabel Rincon GalvezNo ratings yet
- 9 PDFDocument9 pages9 PDFAnggun SetiawatiNo ratings yet
- Jean-Charles Pasquier, Olivier Claris, Muriel Rabilloud, René Ecochard, Jean-Charles Picaud, Stéphanie Moret, Danielle Buch, Georges MellierDocument8 pagesJean-Charles Pasquier, Olivier Claris, Muriel Rabilloud, René Ecochard, Jean-Charles Picaud, Stéphanie Moret, Danielle Buch, Georges Mellierclara giovaniNo ratings yet
- BMJ f6398Document13 pagesBMJ f6398Luis Gerardo Pérez CastroNo ratings yet
- The Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationDocument17 pagesThe Effects of Betamethasone On Clinical Outcome of The Late Preterm Neonates Born Between 34 and 36 Weeks of GestationjeffyNo ratings yet
- Sibai PDFDocument2 pagesSibai PDFAdriana PajueloNo ratings yet
- Parto Prematuro ACOGDocument10 pagesParto Prematuro ACOGAngela_Maria_M_7864No ratings yet
- Pregnancy HypertensionDocument9 pagesPregnancy Hypertensionabi tehNo ratings yet
- ViabilityDocument10 pagesViabilityapi-282195779No ratings yet
- Debate GUIDE PDFDocument8 pagesDebate GUIDE PDFBlesse PateñoNo ratings yet
- A Cluster-Randomized Trial To Reduce Cesarean Delivery Rates in QuebecDocument12 pagesA Cluster-Randomized Trial To Reduce Cesarean Delivery Rates in QuebecVandy IkraNo ratings yet
- Eficácia de Um Programa Intensivo de Visitação Domiiliar Liderado Por Enfermeiras para Mães Adolescentes de Primeira ViagemDocument10 pagesEficácia de Um Programa Intensivo de Visitação Domiiliar Liderado Por Enfermeiras para Mães Adolescentes de Primeira ViagemMarcia RodriguesNo ratings yet
- The Who Action IIIDocument2 pagesThe Who Action IIIMoses mong'areNo ratings yet
- DownloadDocument6 pagesDownloadKai GgNo ratings yet
- Care in Pregnancies Subsequent To Stillbirthor Perinatal DeatDocument12 pagesCare in Pregnancies Subsequent To Stillbirthor Perinatal DeatgalalNo ratings yet
- Elective Delivery Versus Expectant Management For Pre-Eclampsia: A Meta-Analysis of RctsDocument16 pagesElective Delivery Versus Expectant Management For Pre-Eclampsia: A Meta-Analysis of RctsErliana Damayanti100% (1)
- Leitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseDocument7 pagesLeitich, 2003 Antibiotico No Tratamento de VB Meta AnaliseEdgar SimmonsNo ratings yet
- App Acog 2012Document10 pagesApp Acog 2012jimedureyNo ratings yet
- Early Prediction of Preterm Birth For Singleton, Twin, and Triplet PregnanciesDocument6 pagesEarly Prediction of Preterm Birth For Singleton, Twin, and Triplet PregnanciesNi Wayan Ana PsNo ratings yet
- Exercicio IIIDocument6 pagesExercicio IIIccarmogarciaNo ratings yet
- Jamapediatrics Ninan 2022 Oi 220012 1653493573.16134cdkDocument11 pagesJamapediatrics Ninan 2022 Oi 220012 1653493573.16134cdkfitriNo ratings yet
- Emergency Contraception: Knowledge and Attitudes of Family Physicians of A Teaching Hospital, Karachi, PakistanDocument6 pagesEmergency Contraception: Knowledge and Attitudes of Family Physicians of A Teaching Hospital, Karachi, PakistanNaveed AhmadNo ratings yet
- Induction of Labour For Improving Birth Outcomes For Women at or Beyond TermDocument3 pagesInduction of Labour For Improving Birth Outcomes For Women at or Beyond TermCitaNo ratings yet
- Early Hydrocortisone Dosing and Mortality in Premature InfantsDocument13 pagesEarly Hydrocortisone Dosing and Mortality in Premature InfantsIntan Karnina PutriNo ratings yet
- Maternal Morbidity Associated With Multiple Repeat Cesarean DeliveriesDocument7 pagesMaternal Morbidity Associated With Multiple Repeat Cesarean Deliveriesdewi wahyuniNo ratings yet
- Dexamethasone Versus Betamethasone For Preterm Birth: A Systematic Review and Network Meta-AnalysisDocument14 pagesDexamethasone Versus Betamethasone For Preterm Birth: A Systematic Review and Network Meta-AnalysisalexandraNo ratings yet
- Pone 0198447Document23 pagesPone 0198447Erdhika PradigmaNo ratings yet
- Kohn 2019Document8 pagesKohn 2019Elita RahmaNo ratings yet
- Good18.Prenatally Diagnosed Vasa Previa A.30Document9 pagesGood18.Prenatally Diagnosed Vasa Previa A.30wije0% (1)
- The Impact of The Antenatal Late Preterm Steroids Trial On The Administration of Antenatal CorticosteroidsDocument15 pagesThe Impact of The Antenatal Late Preterm Steroids Trial On The Administration of Antenatal Corticosteroidsprinter bersamaNo ratings yet
- The Impact of The Antenatal Late Preterm Steroids Trial On The Administration of Antenatal CorticosteroidsDocument15 pagesThe Impact of The Antenatal Late Preterm Steroids Trial On The Administration of Antenatal CorticosteroidsabelNo ratings yet
- Effect of Dydrogesterone On Treatment of Threatened Miscarriage: A Systematic Review and Meta-AnalysesDocument10 pagesEffect of Dydrogesterone On Treatment of Threatened Miscarriage: A Systematic Review and Meta-AnalysesShirleyNo ratings yet
- Contraception for the Medically Challenging PatientFrom EverandContraception for the Medically Challenging PatientRebecca H. AllenNo ratings yet
- Emery and Rimoin’s Principles and Practice of Medical Genetics and Genomics: Clinical Principles and ApplicationsFrom EverandEmery and Rimoin’s Principles and Practice of Medical Genetics and Genomics: Clinical Principles and ApplicationsReed E. PyeritzNo ratings yet
- 2020 State Wide Program To Reduce Preterm Birth WADocument18 pages2020 State Wide Program To Reduce Preterm Birth WAmadhuNo ratings yet
- Azithromycin in Labor Lowers Clinical Infections in Mothers and NewbornsDocument13 pagesAzithromycin in Labor Lowers Clinical Infections in Mothers and NewbornsmadhuNo ratings yet
- Antenatal Neurodevelopmental Test andDocument8 pagesAntenatal Neurodevelopmental Test andmadhuNo ratings yet
- Antenatal Corticosteroids For Accelerating Fetal LungDocument68 pagesAntenatal Corticosteroids For Accelerating Fetal LungmadhuNo ratings yet
- Family Support Boosts Pregnancy Risk AwarenessDocument12 pagesFamily Support Boosts Pregnancy Risk AwarenessPutri AzizahNo ratings yet
- 3rd Proff Previous QuestionsDocument14 pages3rd Proff Previous QuestionsHardik PuniaNo ratings yet
- Efficacy and Safety of Indomethacin Therapy For PolyhydramniosDocument6 pagesEfficacy and Safety of Indomethacin Therapy For PolyhydramniosdoctorkwekkwekNo ratings yet
- Activity 2. MODULE 1Document12 pagesActivity 2. MODULE 1Rujiyana P. UliNo ratings yet
- Representation of Sexual Behaviour in Books, Pictures, Statues, Films, and Other Media That Is Intended To Cause Sexual ExcitementDocument8 pagesRepresentation of Sexual Behaviour in Books, Pictures, Statues, Films, and Other Media That Is Intended To Cause Sexual ExcitementShelleyNo ratings yet
- Caring for Women with Mental Health ProblemsDocument32 pagesCaring for Women with Mental Health ProblemsDaniela Hathor TerapiasNo ratings yet
- Understanding The SelfDocument53 pagesUnderstanding The SelfJames TacordaNo ratings yet
- Pale Exercises For StudentsDocument4 pagesPale Exercises For StudentsjanaNo ratings yet
- Problems With The PassagewayDocument2 pagesProblems With The PassagewayPrilay Pring AlcopraNo ratings yet
- Class Xii Biology Questions ChapterwiseDocument42 pagesClass Xii Biology Questions Chapterwiseashok pradhanNo ratings yet
- Health Teaching Plan (Brochure)Document2 pagesHealth Teaching Plan (Brochure)Hana ParkNo ratings yet
- Aphrodisiac Mother & Aunty: XyshivaDocument13 pagesAphrodisiac Mother & Aunty: XyshivaAnonymous pmVnncYJ60% (5)
- Embryological Development of The Human BrainDocument17 pagesEmbryological Development of The Human BrainErika LmNo ratings yet
- NCM 109 Reviewer 2Document13 pagesNCM 109 Reviewer 2Jerick PapoloniasNo ratings yet
- The Significance of Ante-Natal Care (Anc) Toward Improving Maternal Health Care DeliveryDocument53 pagesThe Significance of Ante-Natal Care (Anc) Toward Improving Maternal Health Care DeliveryUsman Ahmad TijjaniNo ratings yet
- TAWAKAL Exam BankDocument86 pagesTAWAKAL Exam BankMohamed LibanNo ratings yet
- PD 442 Labor Code Article 95. Right To Service Incentive LeaveDocument6 pagesPD 442 Labor Code Article 95. Right To Service Incentive LeaveMenchie Ann Sabandal SalinasNo ratings yet
- Regodos Stages of LaborDocument91 pagesRegodos Stages of LaborIan Cyrus RegodosNo ratings yet
- Developmental Biology - Oogenesis (Reviewer)Document2 pagesDevelopmental Biology - Oogenesis (Reviewer)shizuNo ratings yet
- Health Talk On Antenatal AnemiaDocument12 pagesHealth Talk On Antenatal AnemiaPriya50% (2)
- Tazneen Hossain Tani - Applied Ethics - Quiz 2Document3 pagesTazneen Hossain Tani - Applied Ethics - Quiz 2Tazneen Hossain TaniNo ratings yet
- Soal ToeflDocument43 pagesSoal ToeflSafita AndrianiNo ratings yet
- Concept Paper JulesDocument6 pagesConcept Paper JulesMARVINS FILMNo ratings yet
- Preterm Labour and PROMDocument25 pagesPreterm Labour and PROMNinaNo ratings yet
- Offline Quiz No. 1-3 Reproductive SystemDocument18 pagesOffline Quiz No. 1-3 Reproductive SystemJelly Rose ApondarNo ratings yet
- MOOT PROPOSITION Rashmi RanaDocument4 pagesMOOT PROPOSITION Rashmi RanaScribdNo ratings yet
- Obstetrics MCQ: Amanda Leow AFP NHS Lothian 20 Jan 2021Document62 pagesObstetrics MCQ: Amanda Leow AFP NHS Lothian 20 Jan 2021Amanda LeowNo ratings yet
- Pelvic Inflammatory Disease (PID)Document16 pagesPelvic Inflammatory Disease (PID)CHRISTIAN RAY ALPAS PASILIAONo ratings yet
- Origin of Germ Cells.Document12 pagesOrigin of Germ Cells.علیزہ نعیمNo ratings yet
- Cephalopelvic Disproportion and Obstructed LabourDocument40 pagesCephalopelvic Disproportion and Obstructed Labournighat khanNo ratings yet