Professional Documents
Culture Documents
NCM 109 Reviewer 2
Uploaded by
Jerick PapoloniasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCM 109 Reviewer 2
Uploaded by
Jerick PapoloniasCopyright:
Available Formats
NCM 109
Reviewer 2
3-Genitourinary Infection o Symptomatic Bacteriuria – bacteriuria accompanied
by physical signs of UTI (s/sx manifestations)
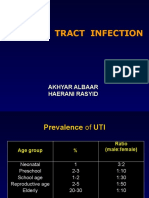
Urinary Tract Infection
o Recurrent UTI – repeated episode of bacteriuria or
The short urethra (4.8-5.1 cm in length) provides a ready
pathway for invasion of organisms. The closure of the symptomatic UTI
o Persistent UTI – persistence of bacteriuria despite
urethra at the end of micturition may return
contaminated urine (bacteria) to the bladder. If left antibiotic treatment
o Febrile UTI – bacteriuria accompanied by fever and
untreated, it can cause PTL (Preterm Labor); Sexual
Activity > UTI other physical signs of UTI; with seizures, high grade
fever
The single most important HOST factor is URINARY
o Cystitis – inflammation of the bladder (dysuria,
STASIS (stopping urine)
urgency, frequency, low grade fever); also known as
Urinary retention = multiplication of bacteria = UTI
honeymoonitis/honeymoon cystitis (term often
Caused by:
o E. Coli (Pathogenic; found in lower intestines; used when you get cystitis after sex); upper portion
caused by poor hygiene) of bladder is affected; severe infection
o Klebsiella (Gram negative bacteria; found o Urethritis – inflammation of the urethra
o Pyelonephritis – inflammation of the upper urinary
everywhere; spread thru person-to-person contact)
o Proteus (Found in the human digestive system; tract and kidneys (chills, fever, flank pain, dysuria,
spread thru contact with infected person or any low UO, elev. BP, N/V)
o Urosepsis – febrile UTI coexisting with systemic
contaminated object/surface; can move easily to
the affected area) signs of bacterial illness; blood culture reveals
presence of urinary pathogen; affects nearby organs
Dx Test:
o U/A (+Bacteria in urine cx) Preventive Measures:
o Perineal hygiene
Mid-stream urine collection means you don't
collect the first or last part of urine that comes Females: q4h change of sanitary pads, Vaginal
out; to reduce the risk of the sample being wash q8h, daily bath
contaminated with bacteria More moisture = more bacterial load
o Avoid tight clothing or diapers (wear cotton panties,
Normal urinalysis (U/A) result: No bacteria
present in the urine, WBC is ≤2-5 WBCs/hpf, rather than nylon)
o Avoid 'holding' urine; encourage to void frequently
Color – Yellow (light/pale to dark/deep amber)
o Empty bladder completely with each void
Abnormal U/A result: Concentrated urine, tea-
o Avoid straining during defecation and avoid
colored
constipation (simple exercise to defecate faster)
Presence of WBC indicates infection; infection
o Encourage generous fluid intake (8-12 glasses/day)
= inflamed /contaminated bladder
o SAFE MEDS DURING PREGNANCY: Bactrim
Urine Culture (cx): Detects the specific bacteria
that caused the UTI (flouroquinolone); small risk for birth defects;
helpful to the mother has UTI in 1st Trimester
NOTE: Filipinos are at risk for antibiotic
o UTI can increase risk of PTL
resistance therefore, it is imperative to comply
to this test to determine the specific bacteria
and administer the RIGHT ANTIBIOTICS Sexually Transmitted Diseases
S/Sx: Monilial Vaginal Infection (Candidiasis, Monilia, or
o Dysuria, suprapubic discomfort, scanty urine output Vaginal Yeast Infection)
o Caused by an overgrowth of a fungus that naturally
(<400 mL/day--lack of urine production because of
the inflammation), urinary frequency, hematuria (if lives in the vagina called Candida albicans
o S/Sx:
WBC count is elevated, it will irritate bladder
resulting to blood in urine), fever Thick white curdy discharge, severe itching,
dysuria, vaginal itching, pain with sex, redness
What to do:
o Avoid straining; do not delay urination around the vagina
o Dx Test:
Classifications:
o Bacteriuria – presence of bacteria in urine Wet Mount (Vaginal smear or wet prep)
o Asymptomatic Bacteriuria – significant bacteriuria Test to detect an infection of the vagina
To determine what fungus caused the
(more than 100,000 colony-forming units) with no
evidence of clinical infection infection
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
Wear PPE to avoid contamination of the
sample or cross-contamination bet. Trichomoniasis/Trich (Trichomonas Vaginalis)
sample and the examiner o A very common STD/STI caused by protozoan
Test result: Hyphae (fungal growth) Budding parasite Trichomonas Vaginalis
yeast o S/Sx:
o Risk Factors: 70% of the infected population don’t have sx
HIV, DM, Pregnancy, Stress; and when infected
Antibiotic Treatment – can cause an imbalance When Sx occur, they typically begin after 5-28
in the natural vaginal flora (lactic acid ---> days after exposure
inhibits the growth of fungus) Thin-greenish-yellow foamy or frothy foul-
o Treatment: smelling vaginal discharge in women and no
Antifungal suppository (Miconazole) @HS for symptoms in men, itching in the genital area,
1 week burning with urination, pain with sex
Oral antifungal Fluconazole (Diflucan) o Dx Test:
o Health Teaching: Microbiological culture or microbial culture
Yogurt in diet (Has lactobacillus content; Method of multiplying the
antimicrobial property) microorganisms by letting the collected
No douching (Douching is washing or cleaning sample reproduce in a predetermined
out the inside of the vagina with water or culture or medium; to detect the specific
other mixtures of fluids) causative agent
Cotton underwear (for free flow of air; no o Treatment:
moisture) Metronidazole (Safe in pregnancy)
Teach the couple, not only the infected o Risk for PTL and PROM
partner Chlamydia
o NOTE: Fetus may contact thrush during o The most common STD
delivery/treatment of baby with oral Nystatin 1cc o Caused by Bacterium Chlamydia Trachomatis
q6h o Can be transmitted during vaginal, anal, or oral sex;
Bacterial Vaginosis (BV, Gardnerella Vaginalis, Vaginitis) can be transmitted to infected mother to newborn
o Overgrowth of bacteria naturally found in the during childbirth; the greater the number of sex
vagina (normal vaginal flora); Transmitted thru partners, the greater the risk of infection
sexual contact; loss of protective lactobacilli o Can cause PID and infertility by blocking the tubes
bacteria o Hydrosalpinx – blocked fallopian tubes that may
o Risk Factors: make it difficult for you to become pregnant
Douching, new or multiple sex partners, o If there's an infection;
antibiotics, using an intrauterine device (e.g. Greater risk for infertility
IUD, tampons) they can also develop scar formations
o S/Sx: surrounding the fallopian tube that makes it
Thin-watery vaginal discharge with fishy odor difficult to pick up eggs during ovulation
(vaginal pH>5) Risk for Ectopic pregnancy (occurs when a
Normal vaginal pH: 4.5 fertilized egg implants and grows outside the
o Dx Test: main cavity of the uterus) or tubal pregnancy
Whiff Test (most common ectopic pregnancy that occurs
Performed by adding a small amount of in the fallopian tube)
potassium hydroxide to a microscopic o S/Sx:
slide containing the vaginal discharge Often asymptomatic; often appears within 1-3
o Treatment: weeks after exposure
Flagyl (Metronidazole 500 mg BID x 7days) thin-purulent discharge; burning and
(oral or IV) frequency with urination; lower Abd'l. pain
Causative agent will resist if you will not o Dx Test:
complete or continue the medication regimen Nucleic Acid Amplification Test (NAAT)
(antibiotic resistance) technique used to detect a particular
o Risk for PTL and PROM nucleic acid sequence
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
detects and identifies a particular species Gonorrhea
or sub-species of an organism o A bacterial STI caused Neisseria Gonorrhea
oftentimes, virus or bacteria are the o Can lead to PID > infertility
pathogens present in the blood, tissues, o Often asymptomatic in females with green-frothy
and urine discharge; males have burning sensation with
Enzyme-linked Immunosorbent Assay (ELISA) urination and penile discharges (sira)
A serologic test (identifies the specific o Dx Test:
antibody present in the serum) Vaginal or urine cx (DOH notifies partners)
Enzyme is linked to a specific antibody to o Treatment:
detect the presence of protein; if protein Rocephin IM (Ceftriaxone)
is present in the sample, it is definitive Buttocks for faster absorption and effect
that chlamydia is positive Zithromax (Azithromycin) 1g SD
o Treatment: o S/Sx:
Azithromycin 1g single dose (Safe in Patient manifests cramping, fever, chills,
pregnancy) purulent discharge (heavy discharge and pus
Potent medication formation), N/V, uterine swelling, adnexal and
Function is to clear the infection by cervical tenderness (when performing IPPA)
preventing bacteria from producing the Severe manifestations compared to other STDs
protein that is essential for the bacteria o NOTE: Multiple sex partners with no condoms
to survive; prevents the causative agent should also be treated
to multiply Drugs of Choice (DOC): Doxycycline P.O. (for
Both the couple should be treated; they non-pregnant)
should be instructed to abstain from DOC: Rocephin IM, Clindamycin, Gentamycin
sexual intercourse until they have (for pregnant)
completed the treatment (re-infection if May need hospitalization
they will not abstain or not complete the Herpes (Herpes Simplex Virus)
regimen) o Viral infection
Having multiple infection increases the o HSV 1 – oral outer lesion (Cold Sore)
risk for infertility o HSV 2 – genital (painful, open lesions)
More infection or re-infection -> more o S/Sx:
scarring -> more chance to block the FT -> Blisters that break open and form small ulcers
female cant ovulate well = infertility Small pocket of body fluids or pus/blood
Doxycycline 2 caps a day for 1 week formation
o Complications: Appearance small bubbles bet. the layer
NB Conjunctivitis (Erythromycin ointment) of the skin that contains water /blood
Also known as Pink Eye Caused by infection
Inflammation of outer eye of the Fever, swollen lymph nodes (vesicles rupture
newborn & appear right after exposure or within 20
Blocked tear duct; eyelids becomes puffy days), burning sensation with urination (1st
with lots of rheum (muta); drainage from sign)
canthus (either corner of the eye where Tingling sensation occurs before new outbreak
the upper and lower eyelids meet) excess (outbreak several times/year)
tears can develop pus ( thick yellowish or o Dx Test:
greenish opaque liquid that oozes out of Viral culture test
the infected tissue) NAAT of a sample skin, crust, or fluid from a le
Can develop 1 day-2 weeks after birth sion
Neonatal Pneumonia o Treatment:
Cause: NB ingests bacteria during birth; if Anti-viral Meds: Acyclovir or Valtrex 500 mg
left untreated, whole respiratory can be OD; during pregnancy, reduces viral load
affected leading to distress of NB enough to deliver vaginally
PTL/Fetal death Hygiene is important
o NOTE: Perinatal transmission occurs in 50% infants Syphilis (Treponema Pallidum - Spirochete)
where mom is infected @ time of delivery
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
o Bacterial STI: causative agent is Treponema DOC: Ceftriaxone (1st Trimester)
Pallidum 40% chance of stillbirth or death; infant may
o Also known as great imitator because it imitates be born with congenital syphilis or
similar symptoms of other diseases; can't be easily Ophthalmia neonatorum that causes
detected without aid of Dx test blindness (appears as Conjunctivitis in NB)
o Stages: Give baby Penicillin (PCN) everyday x 10 days
Primary Stage: Genital Warts
Small painless sores (chancre/skin ulcer) o Condyloma, Condylomata Acuminata, Venereal
1-2cm in diameter, approx. 2-3 weeks Warts, Anal warts, Anogenital Warts
initial exposure o STI caused by certain types of Human
fever Papillomavirus (HPV)
malaise o Spread thru direct skin-to-skin contact, usually
Secondary Stage: during oral, genital, or anal sex with infected
6 weeks-6 months partner
A diffuse rash occurs, which frequently o Contact occurs during vaginal birth (infant may have
involves the palm of the hands and soles laryngeal warts)
of the feet, there may also be sores in the o Sx:
mouth or vagina Skin lesion that is generally pink and project
Latent Stage: outward
Can last for years Usual onset: 1-8 months ff. exposure
Few or no symptoms o Dx Method:
Tertiary Stage: Based on symptoms, can be confirmed by
Gumma – a soft, tumor-like growth of the biopsy (obtain sample, the warts itself)
tissues (granuloma) that occurs in people remove small amount of tissue and will be
with syphilis examined under the microscope
Infection ascends from genital area to the Gynecologic examination using speculum to
point of affecting the CNS magnify the internal organ
Neurological problems --> Neurosyphilis Colposcopy – a procedure to closely examine
Heart symptoms your cervix, vagina and vulva for signs of
o Congenital Syphilis disease; use of lighted speculum to view the
Transmitted during pregnancy or during birth gynecologic organ
Enlargement of the liver and spleen o Prevention:
(hepatosplenomegaly: life threatening), rash, HPV Vaccine
fever, neurosyphilis, and lung inflammation 40 types of HPV that can affect the
Enlargement of liver – hepatomegaly genital area
Enlargement of spleen – splenomegaly Usually, 3 doses
o Dx Test: 1st dose: on or before 15th birthday
Venereal Disease Research Laboratory (VDRL) 2nd dose: 1-2 months from 1st dose
Rapid Plasma Reagin (RPR) Tests 3rd dose: 6 months from 1st dose
o Treatment: Done via routine vaccination if 13-26 y/o
Syphilis is curable with the right (sexually active young adults bracket)
antibiotic/right medication regimen Most effective not yet sexually active at 9
Can be cured but the damage in the genital y/o
will not be totally repaired Condoms
<1yr. 2.4 million units Benzathine Penicillin x 1 o Treatment:
dose Cryotherapy – medical therapy using extreme
IM, right & left buttocks (2 doses) cold to freeze and remove abnormal tissue;
1 vial = 600 000 units (4 vials in total is cryoablation (A procedure in which an
needed) extremely cold liquid or an instrument called a
2 vials for each side of buttocks cryoprobe is used to freeze and destroy
>1yr. Same medication 1x/week for 3 weeks abnormal tissue)
Treat both the couple Trichloroacetic Acid – act by inflicting burn to
o NOTE: Sexual partners screened and treated the warts
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
Gardasil Vaccine (3 doses) – The HPV vaccine; incompetent cervix, exposure to radiation, &
Initial dose at age ≥ 15 years: A 3-dose series is infection)
given at 0, 1 to 2 months, and 6 months If exposed to radiation, wear protective suits;
loose-fitting apparel (e.g. satin or silk) can be
Preventing Sexually Transmitted Diseases effective to protect the person since it reflects
(STDs) the radiation
Consider that not having sex is the only sure way to Types of Abortion:
prevent STD (abstain from all intimate contact) o Missed Abortion
Only have sex within a mutually monogamous Retention of all products of conception after
relationship the death of the fetus in the uterus
Make all sex safer sex by use of condom No FHT
Consider vaccination Signs of pregnancy disappear
o Inevitable Abortion
Bleeding Disorders of Pregnancy The loss of the products of conception cannot
Bleeding d/o according to: be prevented
o 1st Trimester Bleeding Moderate to profuse bleeding, moderate to
Abortion severe uterine cramping
Ectopic Pregnancy Open cervix – can't hold the developing fetus
o 2nd Trimester Bleeding Rupture of Membrane
Hydatidiform Mole o Septic Abortion
Incompetent Cervix Abortion complicated by infection
o 3rd Trimester Bleeding Foul smelling vaginal discharge
Placenta Previa Uterine cramping
Abruptio Placenta Fever in relation to the infection
Common Terms: o Habitual Abortion
o Abortion – most common bleeding d/o of early Abortion occurring in 3 or more successive
pregnancy; termination of pregnancy before pregnancies
viability (before 20 weeks) Most common cause is a significant genetic
o Abortus – a fetus that is aborted before it is 500g in abnormality of the conceptus (fertilized egg)
weight (23 week of pregnancy); Fetus normally o Threatened Abortion
reaches 3500-3800g (41-42 weeks) Possible loss of product of conception
o Blighted Ovum – a small macerated fetus, If there is threatened abortion, the OB-GYN
sometimes there is no fetus surrounded by a fluid will prescribe tocolytic agents (designed to
inside the sac inhibit contractions to avoid miscarriage; e.g.
o Maceration – a dead fetus undergoing necrosis Magnesium Sulfate, Terbutaline, Nifedipine
(decay); change in the skin of the fetus due to the which are calcium ion antagonists)
loss of vernix caseosa, skin will peel off Light vaginal bleeding
o Early Abortion – termination of pregnancy before 16 None to mild uterine cramping
weeks (avocado-sized: 4.6 inches) Vaginal exam at this stage usually reveals a
o Late abortion – abortion that occurs between 16-20 closed cervix (25%-50% results in loss of
weeks pregnancies)
Fetal Causes of Abortion: Complete bed rest, provide commode
o Most common cause of early spontaneous abortion o Incomplete Abortion
is abnormal development of zygote, embryo, and Expulsion of some parts & retention of other
fetus parts of conceptus in uterus
o These abnormalities are incompatible with life and Needs a dilation and curettage procedure, also
would have resulted to severe congenital called a D&C to expel retained body parts
anomalies if pregnancy has not been aborted Medications: Misoprostol & Mifepristone via
Maternal Causes of Abortion: vagina
o Congenital or acquired conditions of the mother & Heavy vaginal bleeding
environmental factor that had adversely affected Severe uterine cramping
the pregnancy outcome & led to abortion (e.g. DM, Open cervix
Passage of tissue
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
o Complete Abortion
Spontaneous expulsion of the products of Risk Factors:
conception after the fetus has died in the o Increasing maternal age (30-35 y/o)
utero 30 is the ideal maternal age since it is the time
Light bleeding, mild uterine cramping, passage when egg production is good quality
of tissue, closed cervix o Increasing parity (5 gravida onwards)
Close watch: risk for excess bleeding o Nutritional factors
Development of Abortion Increased CHON, Folic Acid, Iron, Low-Fat Low-
Salt
o Pituitary gonadotropin
o Infertility therapy
30-35 eggs/day for adults
AMA – 100 to 150/year
o Assisted reproductive therapy
o Genetic, hereditary
o Race, b>w
Caucasians have higher chance of multiple
pregnancy
Dizygotic Twins
o Heteropaternal superfecundation – Phenomenon of
Nursing Responsibilities
having two different fathers for twins
o Save all tissue passed (histopathology
o Results from fertilization of two ova, most likely
exam)
rupture from two distinct graafian follicles usually
o Strict Bed Rest (SBR), provide bedside
the same or one from each ovary, by two sperms
commode, & monitor bleeding q4h to check
during single ovarian cycle
if there's an active bleeding or not o There are two placentae either completely
o Increased oral fluid or IV solution as
separated or more commonly fused at the margin
ordered o Each fetus is surrounded by a separate amnion and
Excessive bleeding: Plain LR
chorion
(isotonic solution, same o Sex of the fetus may differ
concentration of our bodily fluids) o Genetic features, blood group, finger prints also
o Prepare client for surgical intervention (D&C
differs
or suction evacuation) if needed o The earlier splitting of the single zygote occurs, the
o Maternal Sepsis if procedure is not
more independently the twins will develop
performed o Most common; represents 2/3 of cases
o Fertilization of more than one egg by more than one
4-Multiple Pregnancy sperm
Definition of Terms o Nonidentical, may be of different sex
Multiple pregnancy – occurs when more than one fetus o Two chorion, two amnion
simultaneously develop in the uterus o Fetus Papyraceous – is when intrauterine fetal
Twin pregnancy – simultaneous development of two demise of a twin occurs early in pregnancy
fetuses Monozygotic Twins
Although rare, development of three fetus (triplets), four o The twinning may occur at different periods after
(quadruplets), five (quintuplets), six (sextuplets) may fertilization
also occur o Constant incidence of 1:250 births
o Not affected by heredity
Twin Pregnancy o Not related to induction of ovulation
Most common variety of multiple pregnancy o Constitutes 1/3 of twins
Two types: o 70% are Diamniotic monochorionic
o Dizygotic Twins (80%) – results from fertilization of o 30% are Diamniotic dichorionic
two ova leading to fraternal twin o Division of fertilized egg:
o Monozygotic Twins (20%) – results from fertilization 0-72 hrs –> Diamniotic dichorionic
of one ova leading to identical twin 4-8 days –> Diamniotic monochorionic
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
9-12 days –> Monoamniotic monochorionic Increased minor disorders of pregnancy
>12 days –> Conjoined Twins (e.g. back ache, leg pain, inability to walk
o Conjoint Twins properly, hemorrhoids, palpitations,
Anterior (Thoracopagus) dyspnea, and varicosities)
Posterior (Pygopagus) Anemia and placenta previa
Cephalic (Craniopagus) Preterm Labor and delivery (PTL)
Caudal (Ischiopagus) Risk of hypertensive disease
Diagnosis of Twins Pregnancy Antepartum Hemorrhage (APH)
o History: During Labor:
History of ovulation inducing drugs PROM
ART and FD Cord prolapse – when the umbilical cord
Family history of twinning (maternal side) comes out of the uterus with or before
o Sx: the presenting part of the baby
Minor ailments of normal pregnancy are Prolonged Labor
often exaggerated. Some of the symptoms are Increased OP Interference
related to the undue enlargement of uterus Bleeding (intrapartum) – IPH
Increased N/V in early months PPH
HCG – hormone During Puerperium:
that triggers N/V Subinvolution – a medical condition in
and cravings which after childbirth, the uterus does
Cardiorespiratory embarrassment not return to its normal size
(palpitations and shortness of breath) Increased risks of infections
Tendency of swelling legs, varicose veins, Lactation failure
and hemorrhoids is greater o Fetus
Unusual rate of abdominal enlargement Stillbirth/neonatal death
and excessive fetal movement may be Abortion
noticed Single fetal death in twin pregnancy
o General Examination: Intrauterine Growth Restriction (IUGR)
Increased prevalence of anemia Small for Gestational Age (SGA)
Check capillary refill Higher risks of congenital anomalies
Pale conjunctiva and lips Death of one Fetus
Unusual weight gain not explained by Prognosis of the surviving twin depends
preeclampsia or obesity on the gestational age at the time of the
Evidence of preeclampsia is a common demise, the chorionicity, and the length
association of time between the demise and delivery
o Abdominal Examination: of surviving twin
Elongated shape of normal pregnant uterus is Early demise such as vanishing twin does
changed to a more barrel shape and the not appear to increase the risk of death in
abdomen is unduly enlarged the surviving fetus after the first
Height of the uterus is more than the gestation trimester
age Management
Fetal bulk seems disproportionally larger in o Antenatal Management
relation to the size of fetal head Diet about 350 kcal/day
Palpation of too many fetal parts Increased rest at home and early cessation of
Finding two fetal heads work
Two distinct fetal heart sounds at separate Increased number of antenatal visit
spots with a silent area in between Supplementally therapy Fe increase 100-
Complications of Twin Pregnancy 200mg/day, vitamins, calcium, and folic acids
o Maternal o During Labor
During Pregnancy: Vaginal delivery – both or at least one baby in
Exaggerated early symptoms vertex presentation
Increased miscarriage risk Bed rest – prevent early rupture of membrane
Malpresentation Electronic Fetal monitoring
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
Internal examination should be done soon anesthesiologist skilled in providing anesthesia
after the rupture of membrane to exclude cord to effectively relax the uterus for vaginal
prolapse delivery of an noncephalic second twin to
Ringer’s Lactate and 1 unit for BT ready obtain a favorable outcome.
Delivery of Twin Fetuses o Interval Between First and Second Twins
o Vertex-vertex (50%) – vaginal delivery, interval The American college of obstetricians and
between twins not to exceed 20 minutes gynecologist (1998) has determine that the
o Vertex-Breech (20%) – vaginal delivery by senior interval between delivery of twins is not
obstetrician critical in determining the outcome of the twin
o Breech-Vertex (20%) – safer to deliver by CS to delivered second.
avoid the rare interlocking twins (1:1000 twins) Cesarean Delivery
o Breech-Breech (10%) – usually by CS o The American College of Obstetricians and
Vaginal Delivery Gynecologists (1998) has concluded that in general,
o When the first twin is cephalic, delivery can usually CS delivery is the method of choice when the first
be accomplished spontaneously or with forceps twin is noncephalic.
o As in singletons, when the first fetus presents as o It is important to place the patients in a left lateral
breech, major problems are most likely to develop tilt so as to deflect the uterine weight off the aorta
if: to avoid hypotension
Fetus is unusually large and the aftercoming o The uterine incision should be large enough to allow
head is larger than the capacity of the birth a traumatic delivery of both fetuses
canal o It is important that the uterus remain well
Fetus is sufficiently small so that the contracted during completion of the cesarean
extremities and trunk are delivered through a delivery and thereafter
cervix inadequately effaced and dilated to o Remarkable blood loss may be concealed within the
allow the head to escape easily uterus and vagina and beneath the drapes during
Umbilical cord prolapses the time taken to close the incisions
VD of Second Twin o Delivery of the First Baby
o If the fetal head of the breech is fixed in the birth: Babies are small – pose less difficulties
Moderate fundal pressure is applied and Forceps delivery – if necessary, should be
membranes are ruptured. under Pudendal block anesthesia, avoid
Digital examination of the cervix is repeated general anesthesia as the 2nd baby may be
to exclude prolapse of the cord. subjected effect of prolong anesthesia
Labor is allowed to resume, and the fetal heart Don’t give Ergometrine
rate is monitored. Leave 8-10 cm of the cord for admin of any
With reestablishment of labor there is no need drugs or transfusion
to hasten delivery unless a non-reassuring o Delivery of Second Baby
fetal heart rate or bleeding develops. After delivery of the first; the lie, presentation,
If contractions do not resume within and size of the 2nd baby is ascertained
approximately 10 minutes, dilute oxytocin be through abdominal examination
used to stimulate contractions Perform vaginal exam to exclude cord prolapse
o If the occiput or the breech presents immediately and ascertain membrane status
over the pelvic inlet but is not fixed in the birth Delivery of the second baby as required
canal
Presenting part can often be guided into the Additional Info
pelvis by one hand in the vagina while a After the onset of the menstrual cycle, women release
second hand on the uterine fundus exerts about 1,000 immature eggs per month, about 30-35 per
moderate pressure caudally day.
Alternatively, an assistant can maneuver the
presenting part into the pelvis using
ultrasonography for guidance and to monitor
heart rate.
It is essential to have an obstetrician skilled in
intrauterine fetal manipulation and an
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
5-Bleeding during Pregnancy o Management:
First Trimester Bleeding If not yet ruptured, Therapeutic Abortion is
performed
Ectopic Pregnancy
o Sites: If ruptured, removal or repair of ruptured
tube (many physician choose to remove the
ruptured tube because the presence of scar
if the tube is repaired and left, can lead to
another tubal pregnancy)
Prevent and treat hemorrhage which is the
main danger of EP
Prevent infection – loss of too much blood is
susceptible to infection
Prep client for surgery
Institute measures to control and treat shock
if hemorrhage is severe and continue to
monitor post-op
Allow client to express feelings about loss of
Most frequent site is in the fallopian tube, so
pregnancy and concern about future
rupture of the site usually occurs before 12
pregnancy
weeks
o The Classic Symptom Triad:
Second Trimester Bleeding
Amenorrhea Hydatidiform Mole (H. Mole)
Vaginal Bleeding o Also known as Molar Pregnancy, Gestational
Abdominal Pain Trophoblastic Disease
o Assessment Findings o It is the growth of an abnormal fertilized egg or an
History of missed periods & Symptoms of overgrowth of tissue from the placenta (women
Early Pregnancy appears to be pregnant) and uterus enlarges much
Abdominal pain, may be localized on one more rapidly much more than a normal pregnancy
side o It is an alteration of early embryonic growth
Rigid. Tender abdomen; sometimes causing placental disruption, rapid proliferation of
abnormal pelvic mass abnormal cells, and destruction of the embryo .
Bleeding: If severe may lead to shock o Types:
Low Hgb & Hct, rising WBC count Complete Mole – the chromosomes are
o Signs of Hemorrhage: either 46XX or 46XY but are contributed by
Cullen's sign – bluish discoloration of the only one parent and the chromosome
umbilicus due to the presence of blood in the material duplicated. This type usually leads
peritoneal cavity to choriocarcinoma.
Hard rigid board like abdomen due to Partial Mole – has 69 chromosomes. There
presence of blood in the peritoneal cavity are three chromosomes for every pair
Signs of shock: cyanosis, pallor, cold clammy instead of two. This type of mole rarely leads
skin, rapid pulse, decreased BP to choriocarcinoma.
o Etiology:
Unknown
o Pathophysiology
A hydatidiform mole is a placental tumor
that develops after pregnancy has occurred;
it may be benign or malignant. The risk of
malignancy is greater with a complete mole.
The embryo dies and the trophoblastic cells
continue to grow, forming an invasive
tumor.
It is characterized by proliferation of
placental tissues that become edematous
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
and form grapelike clusters. The fluid-filled recommended because they suppress
vesicles grow rapidly, causing the uterus to pituitary luteinizing hormone, which
be larger than expected for the duration of may interfere with serum hCG
pregnancy. measurement
Blood Vessels are absent (no fetal skeleton) Describe and emphasize s/sx that must
o S/Sx: be reported (e.g., irregular vaginal
Vaginal bleeding (may contain some of the bleeding, persistent secretion from the
edematous villi or tissues) breast, hemoptysis, and severe
Uterus larger than expected for the duration persistent headaches). These may
of the pregnancy indicate spread of the disease to other
Abdominal cramping from uterine distention organs
Signs and symptoms of preeclampsia before Address emotional and psychosocial needs
20 weeks gestation Hyperemesis Gravidarum
Severe nausea and vomiting o Is intractable vomiting
o Is severe N/V during pregnancy, which leads to
o Dx: electrolyte, metabolic, and nutritional imbalances
UTZ – reveals: no fetal skeleton, in the absence of medical problems
characteristics appearance of molar growth o It occurs in 1 of every 1000 pregnancies
hCG serum levels are abnormally high o Causative Factors:
o Management: High levels of hCG in early pregnancy
D&C to remove the mole Metabolic or nutritional deficiencies
If the woman is >40, hysterectomy since she More common on first pregnancies
has a higher chance of developing Ambivalence toward the pregnancy or family-
choriocarcinoma related stress
Anticancer drug prescribed to the woman Thyroid dysfunction (hyperthyroidism –
for one year to prevent development of overactive thyroid)
malignant or cancer cells in the uterus o Pathophysiology
o Nursing Responsibilities/Management: Continued vomiting results in dehydration and
Ensure physical well-being of the client ultimately decreases the amount of blood and
through accurate assessment and nutrients circulated to the developing fetus
interventions Hospitalization may be required for severe
Review pertinent history and history of symptoms when the client needs IV hydration
this pregnancy and correction of metabolic imbalance
Provide pre-operative care for o Assessment Findings:
evacuation of uterus (usually suction S/Sx occur during the first 16 weeks of
curettage) pregnancy and are intractable
Induction of labor with oxytocic agents o Clinical Manifestations:
or prostaglandins is not recommended Unremitting N/V (>3 episodes of vomiting/day)
because of the increased risk of Vomitus initially containing undigested food,
hemorrhage bile, and mucus; later containing blood and
Administer IV fluid as prescribed material that resembles coffee grounds
Provide client and family teaching Loss of weight (LOW) 5% or 3kg has occurred
Ensure appropriate follow-up and self- ketones are present in the uterine
care by explaining that frequent o S/Sx:
possibility of recurrence of the problem Pale, dry skin
or progression to choriocarcinoma; Rapid pulse
explain that hCG levels should be Fetid, fruity breath odor from acidosis
monitored for 1 year CNS effects such as confusion, delirium,
Discuss the need to prevent pregnancy headache, lethargy, stupor, or coma
for at least 1 year after diagnosis and N/V –> dehydration –> nutritional deficiency –>
treatment fluid-electrolyte imbalance
Inform the client that oral (and
injectable) birth control agents are not
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
Symptoms often get better after the 20th week
of pregnancy; there are also instances that it
may last the entire pregnancy
o Risk Factors:
First preg., Multiple preg., obesity, hx of an
eating d/o
o Nursing Management:
Promote resolution of the complication.
Make sure that the client is NPO until
cessation of vomiting.
Administer intravenous fluids as
prescribed;
Measure and record fluid intake and o Etiology (Predisposing Factors)
output. Multiparity (80% of affected clients are
Encourage small frequent meals and snacks multiparous)
once vomiting has subsided. Multiple pregnancy
Medical: replacement of fluids, Advance Maternal Age (over 35 y/o in 33% of
electrolytes, and vitamins, along with cases)
tranquilizer or antiemetic. Administer Smoking
antiemetics for pregnancy as prescribed. Previous cesarean section and abortion
Prochlorperazine (Compazine) Uterine incision
Trimethobenzamide (Tigan) Prior PP (incidence is 12 times greater in women
NPO for 48 hours; after condition improves, 6 with previous PP)
small feedings are alternated with liquid o Pathophysiology
nourishment in small amount every 1-2 hors Pathologic process seems to be related to the
If vomiting recurs, NPO status is resumed and conditions that alter the normal function of the
administration of IV is restarted uterine decidua and its vascularization
Address emotional and psychosocial needs. Bleeding, which results from tearing of the
Maintain a non-judgmental atmosphere in which placenta villi from the uterine wall as the lower
the client and family can express concerns and uterine segment contracts and dilates, can be
resolve some of their fears. slight of profuse
o Assessment Findings:
Third Trimester Bleeding Associated Findings:
Placenta Previa (PP) In cases of suspected PP, a vaginal
o It is the most common bleeding disorder of the 3rd examination is delayed until UTZ results are
trimester available and the client is moved to the
o The placenta implants in the lower uterine segment, operating room (OR) for what is termed a
near the cervical os. double set-up procedure. The OR is needed
o The degree to which it covers the os leads to three because the examination can cause further
different classifications: tearing of the villi and hemorrhage, which
Total PP – occurs when the placenta completely can be fatal to the client and fetus
covers the internal os Common Clinical Manifestations (S/Sx):
Partial PP – occurs when the placenta partially Bright red, painless vaginal bleeding
covers the internal os Soft, nontender abdomen, relaxes between
Low-lying or low implantation PP – occurs when contractions, if present
the placenta partially covers the placental FHR stable and within normal limits
border Laboratory and Diagnostic Study Findings
Transabdominal utz confirms suspicion of
PP
o Placenta Previa Care
Painless bright red bleeding
Replace blood loss
Evident in lower segment
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
Vitals indicated shock Watchful waiting – delay delivery until fetus is
Inspect FHR mature enough
Avoid Vaginal Exam No IE is performed in diagnosed PP
o Nursing Management: Abruptio Placenta (AP)
Ensure the physiologic well-being of the client o Is premature separation of a normally implanted
and fetus placenta after the 20th week of pregnancy, typically
Take and record v/s, assess bleeding, and with severe hemorrhage.
maintain a perineal pad count; weigh o Usually occurs after 20 weeks of gestation and before
perineal pads before and after use to delivery of the fetus
estimate blood loss
Observe for shock, which is characterized
by a rapid pulse, pallor, cold moist skin,
and a drop in BP
Monitor the FHR
Enforce strict bed rest to minimize risk to
the fetus
Observe for additional bleeding episodes
Maintain sterile conditions for any invasive
procedure
Make provisions for emergency cesarean
birth
Continue to monitor maternal/fetal vital o Etiology: unknown
signs o Risk Factors:
Provide client and family teaching Uterine anomalies
Explain the condition and management Multiparity
options. To ensure an adequate blood Preeclampsia
supply to the mother and fetus, place the Previous cesarean delivery
woman at bed rest in a side-lying position Renal or vascular disease
Anticipate the order for a sonogram to Trauma to the abdomen
localize the placenta. If the condition of the Previous 3rd trimester bleeding
mother or fetus deteriorates, a cesarean Abnormally large placenta
birth will be required Short umbilical cord
Prepare the client for ambulation and Maternal hypertension
discharge (may be within 48 hours of last Advance Maternal Age
bleeding episode) Trauma to the uterus
Discuss the need to have transportation to Cigarette smoking and cocaine abuse
the hospital available at times o Pathophysiology:
Instruct the client to return to the hospital The placenta detaches in a whole or in part from
if bleeding recurs and to avoid intercourse the implantation site. This occurs in the area of
until after birth the deciduas basalis
Instruct client proper handwashing and o Assessment Findings:
toileting to prevent infection Associated Findings:
Address Emotional and Psychosocial Needs Severe abruption placentae may produce
Offer emotional support to facilitate the complications such as:
grieving process if need Renal failure
After birth of the newborn, provide Disseminated intravascular coagulation
frequent visits with the new born that Maternal and Fetal death
mother can be certain of the infants Common Clinical Manifestations:
condition Intense, localized uterine pain, with or
o Management: without vaginal bleeding
Cesarian is the delivery of choice for all kinds of Concealed or external dark red bleeding
placenta previa Uterus firm to board-like, with severe
Manage bleeding episodes continuous pain
Stepanie Bryn Agustero
BSN 2A
02/24/23
NCM 109
Reviewer 2
Uterine contractions Vaginal delivery if there is no sign of fetal
Uterine outline possibly enlarged or distress, CS if bleeding is severe and fetus can't
changing shape be delivered with vaginal method
FHR present or absent
Fetal presenting part may be engaged
Board-like abdomen caused by
accumulation of blood behind the
placenta with fetal parts hard to
palpate
Sharp pain over the fundus as the
placenta separates
Signs of shock and fetal distress if
bleeding is severe
Laboratory and Diagnostic Study Findings:
UTZ may be able to identify the extent
of abruption. However, the absence of
an utz finding doesn't rule out the Additional Info
presence of abruption Medical Terms:
o o Lavage – washing out of a body cavity, such as the
Nursing Intervention:
Continuously evaluate maternal and fetal colon or stomach with water or a medicated solution
o Gavage – the administration of food or drugs by
physiologic status, particularly:
Vital signs force, especially to an animal, typically through a tube
Bleeding leading down the throat to the stomach
Electronic fetal and maternal monitoring An hCG level of less than 5 mIU/mL is considered
tracings negative for pregnancy, and anything above 25 mIU/mL
Signs of shock-rapid pulse, pallor, cold and is considered positive for pregnancy. An hCG level
most skin, decrease in blood pressure between 6 and 24 mIU/mL is considered a grey area,
Decreasing urine output and you'll likely need to be retested to see if your levels
Never perform a vaginal or rectal examination rise to confirm a pregnancy.
or take any action that would stimulate uterine Consume PRBC w/in 4 hours
activity. Tramadol Ketorolac infused in D5W (?)
Ensure bed rest BP Reading:
o 130/80 is borderline for hypertension
Assess the need for immediate delivery. If the
o If 1st reading 130/80, rest for 30 mins. then take 2nd
client is in active labor and bleeding cannot be
stopped with bed rest, emergency cesarean reading
o If after 2nd reading is still high, pt is considered
delivery may be indicated.
Provide appropriate management. hypertensive
On admission, place the woman on bed Chemoreceptor Trigger Zone (CTZ) – A zone in the
rest in a lateral position to prevent medulla that is sensitive to certain chemical stimuli.
pressure on the vena cava. Stimulation of this zone may produce n/v.
Insert a large gauge IV cath. into a large Lactated Ringer's and Normal Saline Solution – used for
vein for fluid replacement. Obtain a blood fluid resuscitation in hemorrhagic shock
sample for fibrinogen level. Lactated Ringer IV Fluid if active labor
Monitor the FHR externally and measure Methergine (methylergometrine) is a vasoconstrictor
maternal vital signs every 5 to 15 minutes. and often used in obstetrics to control bleeding after a
Administer oxygen to the mother by mask. delivery or spontaneous or induced abortion.
Prepare for cesarean section, which is the Pudendal Block – is anesthesia given in the second stage
method of choice for the birth. of labor and is used to relieve pain in the perineum area.
Provide client and family teaching.
Address emotional and psychosocial needs.
Outcome for the mother and fetus depends on
the extent of the separation, amount of fetal
hypoxia, and amount of bleeding.
Stepanie Bryn Agustero
BSN 2A
02/24/23
You might also like
- Urinary Tract InfectionDocument9 pagesUrinary Tract InfectionTom Mallinson100% (1)
- Urinary Tract InfectionsDocument6 pagesUrinary Tract Infectionspat_tienmin4552No ratings yet
- Lesson Plan UTIDocument5 pagesLesson Plan UTITopeshwar TpkNo ratings yet
- Fetal Growth RestrictionDocument13 pagesFetal Growth Restrictionantoniovilmo100% (2)
- 2014 Group Case StudyDocument42 pages2014 Group Case StudyBrian100% (1)
- To Promote Good Hygiene and Physical Comfort.: Coli (E. Coli), NormallyDocument2 pagesTo Promote Good Hygiene and Physical Comfort.: Coli (E. Coli), NormallyFran LanNo ratings yet
- Multiple Pregnancy Risks and ManagementDocument49 pagesMultiple Pregnancy Risks and Managementvarshasharma05No ratings yet
- Stages of LaborDocument43 pagesStages of LaborMASII100% (1)
- Urinary Tract Infection in Children - Classification, Diagnosis and TreatmentFrom EverandUrinary Tract Infection in Children - Classification, Diagnosis and TreatmentNo ratings yet
- Nursing Care for High-Risk Labor and DeliveryDocument170 pagesNursing Care for High-Risk Labor and DeliveryLongyapon Sheena Stephanie100% (2)
- Rinary Ract Nfections: Classification Pathophysiology Risk Factors Clinical Manifestation DiagnosticsDocument27 pagesRinary Ract Nfections: Classification Pathophysiology Risk Factors Clinical Manifestation DiagnosticsDARYmagpantayNo ratings yet
- Urinary Tract InfectionDocument19 pagesUrinary Tract Infectionjajaler100% (2)
- The Sims 4 Cheats: Full List of Cheat Codes & Console Commands For Pc/MacDocument26 pagesThe Sims 4 Cheats: Full List of Cheat Codes & Console Commands For Pc/MacElissa WilksNo ratings yet
- Everything You Need to Know About Urinary Tract Infections (UTIsDocument10 pagesEverything You Need to Know About Urinary Tract Infections (UTIsMira Mariana UlfahNo ratings yet
- Multiple Pregnancy LectureDocument33 pagesMultiple Pregnancy Lecturefarid_nchep100% (1)
- IskDocument35 pagesIskfadliNo ratings yet
- @medicalbookpdf Preeclampsia PDFDocument286 pages@medicalbookpdf Preeclampsia PDFgalihsupanji111_2230No ratings yet
- Retig Erick Angelo Computation Aog EdcDocument3 pagesRetig Erick Angelo Computation Aog EdcAngelo RetigNo ratings yet
- Urinary Tract Infections (UTI): Causes, Symptoms and TreatmentDocument58 pagesUrinary Tract Infections (UTI): Causes, Symptoms and TreatmentafdaliaNo ratings yet
- The Pathophysiology of Urinary Tract Infections: Practical Interpretations of Commonly Used TermsDocument6 pagesThe Pathophysiology of Urinary Tract Infections: Practical Interpretations of Commonly Used TermsPaullette SanjuanNo ratings yet
- Urinary Tract InfectionDocument6 pagesUrinary Tract InfectionYalc LapidNo ratings yet
- Urinary - Tract - Infection 3Document35 pagesUrinary - Tract - Infection 3DEARY BERRYNo ratings yet
- Bacterial Urinary Tract InfectionDocument17 pagesBacterial Urinary Tract InfectionROSANNA BUCAGNo ratings yet
- 02 Urinary Tract InfectionDocument5 pages02 Urinary Tract InfectionElijah GarciaNo ratings yet
- Microbiology of The Kidneys and Urinary SystemDocument20 pagesMicrobiology of The Kidneys and Urinary Systemflugeliaa14No ratings yet
- Renal DisDocument166 pagesRenal DisCharles MutaiNo ratings yet
- URINARY TRACT INFECTIONS: AN OVERVIEWDocument49 pagesURINARY TRACT INFECTIONS: AN OVERVIEWrolly riksantoNo ratings yet
- UTI Microbiology and DiagnosisDocument11 pagesUTI Microbiology and Diagnosisoxford_commaNo ratings yet
- Cystitis Guide: Symptoms, Causes & TreatmentDocument10 pagesCystitis Guide: Symptoms, Causes & TreatmentJeffNo ratings yet
- Urinary Tract InfectionDocument5 pagesUrinary Tract InfectionDRANo ratings yet
- Urinary Tract InfectionsDocument71 pagesUrinary Tract Infectionsdayibon499No ratings yet
- URINARY TRACT INFECTION GUIDEDocument52 pagesURINARY TRACT INFECTION GUIDERahmawati HamudiNo ratings yet
- Pharmacotherapy of Infectious Disease:: 6. Urinary Tract Infections and ProstatitisDocument26 pagesPharmacotherapy of Infectious Disease:: 6. Urinary Tract Infections and ProstatitisDigafe TolaNo ratings yet
- Seminar On: Urinary Tract Infections and NephritisDocument34 pagesSeminar On: Urinary Tract Infections and NephritisGargi MPNo ratings yet
- Ids Trans and SamplexDocument93 pagesIds Trans and SamplexPrincess Cate MercadoNo ratings yet
- Definitions EtiologyDocument85 pagesDefinitions EtiologyPrincess Cate MercadoNo ratings yet
- Renal - MedbulletsDocument74 pagesRenal - Medbulletssmian08No ratings yet
- Urinary Complaints: Aviva Romm, Eric L. Yarnell, David WinstonDocument16 pagesUrinary Complaints: Aviva Romm, Eric L. Yarnell, David WinstonIoana Mădălina BrînzăNo ratings yet
- UTI Urinary Tract Infections: Causes, Symptoms, DiagnosisDocument3 pagesUTI Urinary Tract Infections: Causes, Symptoms, Diagnosisjishu baruaNo ratings yet
- Notes On UtiDocument15 pagesNotes On UtiSaleh Mohammad ShoaibNo ratings yet
- Urinary Tract Infection (UTI) : Omega Mellyana Sub Bag. Nefrologi Anak FK UNDIP-RSUP Dr. KariadiDocument24 pagesUrinary Tract Infection (UTI) : Omega Mellyana Sub Bag. Nefrologi Anak FK UNDIP-RSUP Dr. KariadiRastia AlimmattabrinaNo ratings yet
- Urinary Tract Infection Guide: Symptoms, Causes, Diagnosis and TreatmentDocument44 pagesUrinary Tract Infection Guide: Symptoms, Causes, Diagnosis and TreatmentrintyosoNo ratings yet
- Urinary Tract Infection (UTI)Document6 pagesUrinary Tract Infection (UTI)Anonymous iG0DCOfNo ratings yet
- Includes: Urinary Tract Infections Genital Tract Infections Viral Sexually Transmitted Diseases Bacterial Sexual Transmitted DiseasesDocument37 pagesIncludes: Urinary Tract Infections Genital Tract Infections Viral Sexually Transmitted Diseases Bacterial Sexual Transmitted DiseasesDon Pelicio NgohoNo ratings yet
- Notes On Genitourinary Tract InfectionsDocument9 pagesNotes On Genitourinary Tract InfectionsSaleh Mohammad ShoaibNo ratings yet
- Cases of Group 3 LC 1Document13 pagesCases of Group 3 LC 1abdul basithNo ratings yet
- Prevalence and Bacteriology of Culture-Positive UTI in Pregnant WomenDocument28 pagesPrevalence and Bacteriology of Culture-Positive UTI in Pregnant Womenmiir ikbalNo ratings yet
- Urinary Tract InfectionDocument10 pagesUrinary Tract InfectionditaNo ratings yet
- Urinary Tract InfectionsDocument24 pagesUrinary Tract InfectionsTom TsouNo ratings yet
- RLE Urinary Tract InfectionDocument13 pagesRLE Urinary Tract InfectionAliza AlyyNo ratings yet
- Urinary Tract Infections (UTIs): Causes, Symptoms & TreatmentDocument22 pagesUrinary Tract Infections (UTIs): Causes, Symptoms & TreatmentNoor AliNo ratings yet
- Pathogens of The Gut - Christine ProchnowDocument1 pagePathogens of The Gut - Christine ProchnowMicroposterNo ratings yet
- Nephrology: Dr. LuDocument2 pagesNephrology: Dr. LuShams JailaniNo ratings yet
- Urinary Tract InfectionDocument10 pagesUrinary Tract Infectionjaah diazNo ratings yet
- UTI Pediatric NotesDocument2 pagesUTI Pediatric NotesSanya BNo ratings yet
- UTI SeminarDocument3 pagesUTI SeminarAmbi KNo ratings yet
- Urinary Tract Infection in ChildrenDocument45 pagesUrinary Tract Infection in ChildrenMuhammad HaziqNo ratings yet
- Lecture 8. Urinary Tract Infection (Uncomplecated Aspect)Document41 pagesLecture 8. Urinary Tract Infection (Uncomplecated Aspect)krisnadewirahadiNo ratings yet
- Urinary Tract Infection (Book) : NephrologyDocument4 pagesUrinary Tract Infection (Book) : NephrologyVon HippoNo ratings yet
- Urinary Tract Infection GuideDocument56 pagesUrinary Tract Infection GuideRicky JalecoNo ratings yet
- UTI LecDocument24 pagesUTI LecFizzy ImranNo ratings yet
- UTI in Children: Prevalence, Etiology, Manifestations and ComplicationsDocument4 pagesUTI in Children: Prevalence, Etiology, Manifestations and ComplicationsAmanda Aldilla MeutiadiNo ratings yet
- Infectious Diseases - 04Document21 pagesInfectious Diseases - 04Arthur YanezNo ratings yet
- Pathophysiology (Book-Based) : CystitisDocument9 pagesPathophysiology (Book-Based) : CystitisIrish EspinosaNo ratings yet
- Tai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuDocument3 pagesTai Lieu Tieng Anh Cho Sinh Vien Bai Nhiem Khuan Duong Tiet NieuLê Mỹ Khánh LyNo ratings yet
- Urinary Tract Infections: Dr. Shweta Naik Assistant ProfessorDocument62 pagesUrinary Tract Infections: Dr. Shweta Naik Assistant ProfessorMeenakshisundaram CNo ratings yet
- Urinary Tract Infection in PregnancyDocument49 pagesUrinary Tract Infection in PregnancyBALMERA, DANIELLA B.No ratings yet
- Pediatric Urinary Tract Infection: Aprianda Saputra/ANSDocument34 pagesPediatric Urinary Tract Infection: Aprianda Saputra/ANSAkbar DarajatNo ratings yet
- Female Urinary Tract Infections in Clinical PracticeFrom EverandFemale Urinary Tract Infections in Clinical PracticeBob YangNo ratings yet
- Jurnal Ultrasound 1Document6 pagesJurnal Ultrasound 1weniNo ratings yet
- Babson and Benda's ChartDocument10 pagesBabson and Benda's ChartZasly WookNo ratings yet
- Multiple Pregnancy Definition and DiagnosisDocument24 pagesMultiple Pregnancy Definition and DiagnosisNura BamaiyiNo ratings yet
- Prophylactic Cervical Cerclage (Modified Shirodkar Operation) For Twin and Triplet Pregnancies After Fertility TreatmentDocument8 pagesProphylactic Cervical Cerclage (Modified Shirodkar Operation) For Twin and Triplet Pregnancies After Fertility TreatmentAiraNo ratings yet
- Multiple Pregnancies: Determining Chorionicity and AmnionicityDocument16 pagesMultiple Pregnancies: Determining Chorionicity and AmnionicityRyan IlhamNo ratings yet
- Multiple Birth FactsDocument6 pagesMultiple Birth FactsElliotPianoNo ratings yet
- Signs of PregnancyDocument4 pagesSigns of Pregnancybreanna zyreNo ratings yet
- Multiplepregnancy 100515015745 Phpapp01Document29 pagesMultiplepregnancy 100515015745 Phpapp01haisureshNo ratings yet
- Daftar Diagnosa ObgynDocument8 pagesDaftar Diagnosa Obgynrm ferinaNo ratings yet
- Obstetric History & Examination SheetDocument8 pagesObstetric History & Examination SheetVaibhav BhatiaNo ratings yet
- Frequently Asked Questions (Faqs) (Central Civil Services) : 1. Pension PolicyDocument36 pagesFrequently Asked Questions (Faqs) (Central Civil Services) : 1. Pension PolicyStanleyNo ratings yet
- Osmanabadi Goat Breed Status PaperDocument7 pagesOsmanabadi Goat Breed Status PaperShaikh Tausif AhmedNo ratings yet
- Wwssw&ilwsa Frocess, Consent: AgreementDocument16 pagesWwssw&ilwsa Frocess, Consent: AgreementklarckkentNo ratings yet
- Sims 4 ChecksDocument5 pagesSims 4 ChecksUdei SchikhauiNo ratings yet
- Lau y Murnighan - 1998 - Demographic Diversity and Faultlines The CompositDocument17 pagesLau y Murnighan - 1998 - Demographic Diversity and Faultlines The CompositRMADVNo ratings yet
- Multiple Pregnancy NOR PosterDocument1 pageMultiple Pregnancy NOR PosterbigbossNo ratings yet
- Admissions Policy 2024-25Document7 pagesAdmissions Policy 2024-25isleworthsyonNo ratings yet
- Bayesian Analysis of Infant Mortality in Oyo State, NigeriaDocument6 pagesBayesian Analysis of Infant Mortality in Oyo State, NigeriaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Can Your Baby Get Pregnant If You Have Sex While PregnantDocument6 pagesCan Your Baby Get Pregnant If You Have Sex While Pregnanteng-scribd100% (2)
- In Vitro FertilizationDocument4 pagesIn Vitro Fertilizationapi-3712326No ratings yet
- The Starkville Dispatch Eedition 12-27-13Document16 pagesThe Starkville Dispatch Eedition 12-27-13The DispatchNo ratings yet