Professional Documents
Culture Documents
The Laboratory Test Utilization Management Toolbox
Uploaded by
omaromranCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Laboratory Test Utilization Management Toolbox
Uploaded by
omaromranCopyright:
Available Formats
Review
The laboratory test utilization management toolbox
Geoffrey Baird
Department of Laboratory Medicine, University of Washington, Seattle, WA USA
*Corresponding author: gbaird@u.washington.edu
Abstract
Efficiently managing laboratory test utilization requires both ensuring adequate utilization of needed tests in some patients and discouraging su-
perfluous tests in other patients. After the difficult clinical decision is made to define the patients that do and do not need a test, a wealth of inter-
ventions are available to the clinician and laboratorian to help guide appropriate utilization. These interventions are collectively referred to here as
the utilization management toolbox. Experience has shown that some tools in the toolbox are weak and other are strong, and that tools are most
effective when many are used simultaneously. While the outcomes of utilization management studies are not always as concrete as may be desired,
what data is available in the literature indicate that strong utilization management interventions are safe and effective measures to improve patient
health and reduce waste in an era of increasing financial pressure.
Key words: clinical laboratory services; utilization; utilization review
Received: December 12, 2013 Accepted: March 27, 2014
Introduction
“(The) First Rule in government spending: Why (1). The reasons for overutilization are myriad, and
build one when you can have two at twice the may include as enabling factors even the technol-
price?” - S.R. Hadden in Contact, 1997 (written by ogy we use to perform laboratory testing. There
Carl Sagan). was once a time when it would be unthinkable
and impractical for a hospital inpatient to get mul-
S.R. Hadden, the wealthy industrialist in the Carl
tiple laboratory tests per day, every day (2), but in
Sagan drama Contact, may have been poking fun
the present day, high frequency testing is almost
at stereotypical government spending practices
the rule in resource-rich settings, rather than the
when he quipped the line above, but his state-
exception. Instrument vendors now advertise turn-
ment was more profound than it sounds, and it is
around times in minutes rather than hours or days
especially relevant to clinical laboratory test utili-
for clinical assays, automated platforms handle
zation. The health care payment systems operat-
hundreds to thousands of samples per hour, and
ing today in many countries remove the clinicians
data systems distribute the results of these tests
who make utilization decisions from the financial
electronically, directly to caregiver’s electronic in-
consequences of their actions, with the result that
boxes. In the outpatient care setting, testing may
some patients undergo at least twice the testing
not occur daily for each patient, but the barrier to
at twice the price, if not much more.
getting testing can be incredibly low; the standard
That test overutilization exists is no longer an item routine “physical” that a healthy adult might re-
of debate, and it is clearly an international problem ceive at a doctor visit can be accompanied by a
http://dx.doi.org/10.11613/BM.2014.025 Biochemia Medica 2014;24(2):223–34
©Copyright by Croatian Society of Medical Biochemistry and Laboratory Medicine. This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License
(http://creativecommons.org/licenses/by-nc-nd/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
223
Baird G. Utilization management
panel of tests, perhaps only a blood count and The problem of identifying inappropriate labora-
electrolytes, but possibly also any one of a myriad tory test utilization is outlined below in the form of
of large so-called “wellness” panels offered by three “Rules,” all of which are intended to provide
commercial laboratories that have financial incen- the general rationale and goals of a laboratory test
tives to drive frequent, high-cost testing. It does utilization management program. Afterwards, the
not simplify matters that additional technological laboratory test utilization management toolbox,
advances, especially the genomic revolution, have comprised of a collection of evidence-based tools
exponentially increased the number of possible available to the laboratorian and clinician alike, will
tests that are available. No one clinician can possi- be described, with emphasis on those tools that
bly know which novel test is appropriate in any are most appropriate for specific types of inappro-
given situation, and the problem compounds itself priate utilization.
daily as additional genetic tests, small molecule
mass spectrometry tests, or proteomic multivari-
The three rules of laboratory test
ate index assays are added to the global test menu.
Absent any guidance, it appears that clinicians are utilization
apt to order whatever seems most familiar, any or
all tests that sound like they might be appropriate, Rule 1: “If you ask a stupid question, you get a
or whatever has been touted most heavily by am- stupid answer”
bitious sales representatives. Another problem Rule 1, otherwise known to the statistician as
unique to academic settings is that one must al- Bayes’ Theorem, posits that the post-test probabil-
low for the fact that physicians in training may ity of something being true is a product of the pri-
need to order more than an optimal number of or probability that the thing is true and the likeli-
tests in order to learn how to use the results of this hood ratio provided by a test (4). In mathematical
testing in the practice of medicine. terms for laboratory testing, Bayes’ Theorem can
So, what is a laboratory director to do in the face be expressed as:
of this growing adversity? How do we ensure that P(B|A) P(A)
that patient’s interests come first, that neither in- P(A|B) =
P(B)
patients nor outpatients get the wrong tests at all
or the right tests too frequently, and that caregiv- This can be translated to the context of laboratory
ers are able to select tests appropriately so that medicine to mean that the conditional probability
they can most easily interpret the results? Labora- of disease (A) given the result of a test (B) (also
tory test utilization researchers, including this au- called the “positive predictive value”) is equal to
thor, have often summed up the literature in lec- the conditional probability of the result (B) given
tures or in private by stating that, “30% of labora- the disease (A) being present, multiplied by the
tory testing is likely wasteful,” and now this esti- probability of the disease (A) in the population
mate has been supported by a thorough meta- (also called the “prevalence”) and divided by the
analysis (3). However, it is has never been clear ex- probability of the test giving the result (B) in all
actly how laboratory directors or clinicians should members of the population.
go about identifying those 30% of tests, especially One consequence of Rule 1 in laboratory testing is
given that the wasted testing is not evenly distrib- that ordering a test to rule in a condition when the
uted across all patients or specific tests. What is prior probability is very low (i.e. a urine hCG test to
needed, therefore, is a standardized approach for assess pregnancy in an apparently male patient) is
identifying malutilisation in daily clinical practice, unlikely to be a fruitful endeavor, since negative
and once it has been identified, a common set of results were already expected and positive results
tools should be available to fix the problem. This is are most likely false positives. The same applies in
the approach taken in this review. the converse; one should not generally order a test
Biochemia Medica 2014;24(2):223–34 http://dx.doi.org/10.11613/BM.2014.025
224
Baird G. Utilization management
when it is extremely likely that the diagnosis in to impress or intimidate their peers (5), but we
question is present. Rule 1 exists not just to dis- should emphasize to our trainees that testing for
courage inappropriate ordering, but for the equal- many things simultaneously just because it’s pos-
ly important reason of saving one from the onus sible or because “…I saw a patient like that once”,
of interpreting highly unlikely test results. The true is no reason to embark upon an unnecessarily
power of testing in the setting of low pre-test costly diagnostic odyssey. Tests ordered out of
probability is ruling OUT a diagnosis; negative re- pure curiosity have a funny way of presenting later
sults in these settings can be trusted, but positive as unexplainable positive results, and the cost of
results will always be confusing. working up a false positive result is always larger
Rule 1 is not always easy to apply, however, for than not ordering the test in the first place.
three reasons. One, prior probabilities of disease Rule 2: “Laboratory testing is for sick people”
close to 0 or 1 or quite unusual, as clinical, radio-
logic, and historical findings do not always have If Rule 2 sounds like a restatement of Rule 1, that is
enough evidentiary value to allow one to cease a because it is. Indeed, all of laboratory test utiliza-
workup without laboratory testing. The prior prob- tion management stems from Bayes’ theorem, al-
ability of disease could also be completely un- though different restatements of the theorem pro-
known, in which case the Rule helps not at all. Two, vide windows into distinct aspects of the utiliza-
many physicians are not always able to estimate tion management problem. What Rule 2 focuses
prior probabilities with enough savvy to allow an on is the well patient, and specifically, the notion
accurate application of the Rule. Clinical decision of “Wellness Testing” (6,7). Wellness Testing com-
support and education can partly address this is- monly refers to single tests or panels of tests that
sue, but patients are all unique, so there can be no are intended to be performed on well patients,
absolute guide to prior probability assessment for usually self-selecting adults, with the goal of pre-
all situations. Three, human beings are curious, es- venting unwanted later complications of disease.
pecially those who go into medicine. Curiosity Put in this way, Wellness Testing is in fact a misno-
manifests itself in the medical setting by explora- mer, in that the purpose of it is to discover that a
tion of unlikely possibilities, and while this may be patient is, or will become, unwell. In Bayesian
an important educational activity, it should not be terms, Wellness Testing poses a significant risk of
the basis for sound medical policy. diagnostic failure, or at least confusion, in the set-
ting of low prior probabilities. In financial terms,
The three challenges of Rule 1 notwithstanding, however, Wellness Testing creates a highly attrac-
the Rule can still be followed effectively by 1) us- tive market for laboratory vendors that earn mon-
ing Bayesian thinking to assign at least relative, ey on a fee for service basis.
rather than absolute, likelihoods to various diag-
noses to allow one to order sequential testing from Like all rules, however, Rule 2 has exceptions. Lipid
most to least beneficial; 2) ceasing repetitive daily testing, diabetes screening and newborn screen-
testing, or at least restricting testing to reflect our ing, for example, are reasonable uses of laboratory
understanding of intraindividual biological varia- testing in ostensibly healthy people, or at least
tion, because asking “too many questions” has the people with prior probabilities of disease that are
same effect as asking a single “stupid question”; equivalent to the general population risk. Like
and 3) always developing a plan for test interpre- many exceptions, these exceptions prove the rule.
tation PRIOR to ordering a test. This third point For lipid testing, one might argue that the stand-
cannot be stressed enough, especially during ard “healthy” patient in a population, for example
medical training, and even more critically in deal- a middle-aged male who is slightly overweight
ing with the most curious among us. Clinicians of- and exercises a tad too little, could reasonably be
ten construct large differential diagnoses in medi- considered “sick” in terms of the risk that lipid-re-
cine to avoid missing the occasional rare presenta- lated disorders pose to his long-term health. More
tion or to avoid anchoring bias, or perhaps simply importantly, however, the reason why lipid testing
http://dx.doi.org/10.11613/BM.2014.025 Biochemia Medica 2014;24(2):223–34
225
Baird G. Utilization management
and newborn screening are exceptions to Rule 2 is Rule 3: “Too many good tests are the same as
that there exists evidence demonstrating a benefit one bad test”
of the testing, when coupled with appropriate Although this idea has been hinted at in Rules 1
downstream therapeutic interventions. In a lipid and 2, a separate rule should be reserved for the
panel, we test for analytes (cholesterol, lipopro- idea that repetitive tests or large panels of tests,
teins, triglycerides) that we know to be causally re- even when comprised by individually reasonable
lated to cardiovascular disease and that we know tests, are a form of malutilisation. At the very least,
respond to therapy, and we understand much of too-frequent repetitive testing can come at odds
the risk-benefit relationship of either measuring or with the Nyquist-Shannon theorem, a fundamen-
not measuring lipids (8). Likewise, despite the fact tal principle of information theory (20). The math-
that inborn errors of metabolism are exceedingly ematical derivation of the Nyquist-Shannon theo-
rare, and the fact that the positive results from rem is beyond this discussion, but in words it can
many newborn screening tests are false positives, be said to define the appropriate relationship be-
the testing allows us an opportunity to confirm tween how often one should sample a varying sig-
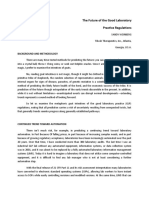
true positives and initiate therapy to avert diseases nal. In Figure 1, 4 potential situations are depicted,
with extremely high morbidity and mortality that in which the same oscillating laboratory value (the
would otherwise be devastatingly difficult and ex- “signal”) is measured at successively longer inter-
pensive to treat later in life. Numerous studies now vals (the “sampling”). Clearly, plots A and B indicate
indicate that newborn screening is cost-effective, oversampling, where far more laboratory tests
as well (9-13). The WHO criteria for mass screening were obtained relative to what was needed to de-
are a helpful resource for assessing the utility of fine the underlying signal, and plot D shows sig-
any screening proposal (14). nificant undersampling, leading to a misleading
The limits to Rule 2 have exceptions. Lipid testing impression that the value is oscillating slower than
is helpful when limited to those analytes that have it is in reality. Plot C, on the other hand, has pre-
been studied in large cohorts like the Framingham cisely as many sampling points as is necessary to
study (15). Newer expanded lipid panels, such as describe accurately the underlying signal. In clini-
those including genetic testing (16,17), additional cal terms, the Nyquist-Shannon theorem tells us
information about the size or chromatographic that repeated testing to assess a change in a labo-
mobility of lipoprotein particles (18,19), or addi- ratory parameter should occur at intervals on par
tional biochemical or proteomic biomarkers, run with the expected time it would take the analyte
afoul of both Rule 1 and Rule 2. In some cases, value to change.
these tests rely on evidence that is preliminary, One obvious clinical manifestation of Nyquist-
limited, proprietary or otherwise insufficient to Shannon theorem in clinical laboratory is in Hae-
support widespread utilization, and in other cases moglobin A1c (HbA1c) testing. Because the longev-
these tests may in fact eventually find a place in ity of red blood cells allows haemoglobin mole-
appropriate lipid panels, but are currently waiting cules to remain in circulation for several months, it
for evidence that shows us where to apply them makes no sense to assess HbA1c on a scale of days
most effectively. In the case of newborn screening, to weeks, but rather it should be measured on a
the calculus as to whether to include a test in a scale of 1-3 months to assess changes. Despite the
panel is actually fairly simple, as a test must be inherent logic of this conclusion, there is still sub-
paired with a treatment that prevents either a dis- stantial variation amongst physicians in ordering
ease or the squeal of that disease. If there is noth- HbA1c testing at rational intervals (21). It is also im-
ing to do with the result of a newborn screening portant to understand that undersampling is a sig-
test, then it does not make sense to do the test. nificant risk for HbA1c testing, as too-infrequent
That this truism extends to all laboratory testing tests (i.e. a year or years between determinations
should be obvious. in a poorly-controlled diabetic) can cause a physi-
cian to miss clinically significant variation.
Biochemia Medica 2014;24(2):223–34 http://dx.doi.org/10.11613/BM.2014.025
226
Baird G. Utilization management
6.5 A 6.5 B
Laboratory Value 6.0 6.0
Laboratory Value
5.5 5.5
5.0 5.0
4.5 4.5
4.0 4.0
3.5 3.5
0 50 100 150 200 250 0 50 100 150 200 250
Day Day
6.5 C 6.5 D
6.0 6.0
Laboratory Value
Laboratory Value
5.5 5.5
5.0 5.0
4.5 4.5
4.0 4.0
3.5 3.5
0 50 100 150 200 250 0 50 100 150 200 250
Day Day
Figure 1. A hypothetical oscillating laboratory value (signal) with a period of approximately 48 days is measured once every 1 (A), 4
(B), 12 (C) and 31 (D) days.
A second problem with too-frequent testing de- tives that require follow-up testing. The phenom-
rives from the statistics of repetitive applications enon creeps even into highly complex and expen-
of a single test. While the sensitivity for disease de- sive genetic testing panels performed at reputable
tection increases when testing repetitively, the laboratories. For example, there are numerous ge-
specificity must concomitantly decrease. It is often netic syndromes that are known to be each caused
pointed out, for example, that the chances of hav- by a number of different possible mutations, and
ing one abnormal value in a panel or series of 14 reference laboratories will often offer a panel of
tests whose reference ranges are defined by the tests that probes many or all possible mutations,
central 95% percentile of the health population causative or otherwise. In such cases, it is often the
approaches 50%, even when the patient in ques- case that one specific mutation is causative in the
tion is totally normal (7). This counterintuitive re- majority of cases, such that testing for a single mu-
sult is of course not entirely accurate, as it assumes tation first with a cheaper screening methodology
that all laboratory tests vary independently (they may obviate the need for the expensive full panel
do not), but it drives home the point that the more in a majority of patients, lowering the overall cost
testing is done, the more disease is discovered. of testing (22). Reflexive testing algorithms that al-
This is not always a bad thing, though, and repeti- low the providing laboratory to aid the clinician in
tive testing placed at appropriate intervals (i.e. for defining the optimal sequential testing pathway
lipid testing) can be highly beneficial to popula- are a key tool in the test utilization toolbox, and
tions. However, a disreputable laboratory vendor will be covered later.
could also exploit this phenomenon to generate Evidence that repetitive or daily testing is common
revenue from a very large panel of putative bi- abounds in the historical literature (23-31), yet few-
omarker assays guaranteed to generate false posi- er studies have shown how repetitive testing can
http://dx.doi.org/10.11613/BM.2014.025 Biochemia Medica 2014;24(2):223–34
227
Baird G. Utilization management
drive unnecessary and costly downstream activi- Applying the rules
ties. In a pair of large academic medical centres, Applying the 3 rules of laboratory test utilization is
for example, daily ionized calcium testing had be- a deceptively simple task, as identifying waste ap-
come ingrained into the culture of the house staff pears simple. However, the number of people who
and was ordered in nearly every patient. When have decried the third of laboratory testing that is
daily ionized calcium testing was reduced by ap- waste likely far outstrips the number of people
proximately 70% by introducing a reflexive testing who have ever successfully managed laboratory
strategy, doses of calcium administered by the
test utilization. Laboratory test malutilisation is
pharmacy in the hospitals decreased by a very
thus like the weather, in that “…everyone talks
similar fraction, as did the diagnoses of “hypocal-
about it, but no one does anything about it”. How
cemia” rendered by the providers (32). While not
can this be changed?
enumerated in the report, it is likely that the cost
savings of these downstream effects far out- First, in an institution desiring to curb inappropri-
stripped the laboratory-specific savings. No dis- ate test utilization, there must be “buy-in” amongst
cernible difference in morbidity or mortality was the key stakeholders. There must be at least one
discovered after this intervention, even amongst member of the laboratory staff, a laboratory direc-
diagnoses known to be associated with significant tor, who is willing and able to expend the time
hypocalcemia (tetany, seizures, myocardial infarc- needed to do the data analyses required to identi-
tion). In this case, a substantial burden of disease fy the problem areas. If this laboratory director is
(“hypocalcemia”) was being invented by daily ion- in academia, as often occurs, their efforts in man-
ized calcium testing practices, and it disappeared aging utilization should be both pursued and re-
within a month as testing practices were altered, warded as genuine scholarly activities, with all
raising the question of how many other fictitious work resulting in publications that allow others to
diagnoses and unnecessary treatments inpatients learn from their successes and failures. If an aca-
may receive when they undergo daily routine lab- demic department values contributions to test uti-
oratory testing. lization management below contributions to basic
In another study that drew upon a large dataset or applied sciences, then junior faculty with an in-
comprising 4 million common outpatient tests terest in the field will simply not participate for fear
performed in a large Canadian province (33), van of missing out on promotion, and the field will
Walraven et al. found that approximately 30% of stagnate. Outside of laboratory staff, however, co-
testing for eight common analytes was repeated operative medical staff are needed in the remain-
within a month. Potentially redundant testing, de- der of the hospital, especially those who are will-
fined as testing repeated within defined time in- ing and able to take the time and energy required
tervals, was estimated to have cost between $13.9 to participate in utilization review and quality im-
and $35.9 million (Canadian) annually. As this study provement activities. Second, as utilization man-
only focused on 8 common tests with low unit agement is a data-intensive activity, there must be
costs, it is likely that the true cost of all redundant adequate information technology resources avail-
testing to large health care systems is probably able to the project leader. At a minimum, program-
much larger, and perhaps even orders of magni- mers and/or individuals savvy in building, manag-
tude larger than what was observed in this study. ing and querying large databases are absolutely
Guidelines have been recently published describ- required to generate reports and analyses, or at
ing the “Minimum retesting interval”, i.e. the mini- the very least retrieve the raw data required to as-
mum time before a test should be repeated(34). sess utilization. The ability to correlate laboratory
While this guideline is not comprehensive of all test utilization data (orders) with test results and
laboratory tests and all clinical situations, it pro- other patient data (metadata such as gender and
vides a substantial, evidence-based list of recom- age, or potentially diagnostic or outcome-related
mendations that covers much of the current prac- data) is key for assessing the opportunities and po-
tice of medicine. tential risks of utilization management interven-
Biochemia Medica 2014;24(2):223–34 http://dx.doi.org/10.11613/BM.2014.025
228
Baird G. Utilization management
tions, meaning that large relational healthcare in- umn is not intended to be an exhaustive list of all
formation databases(35), although expensive, will published examples of a particular tool being put
be very valuable in future utilization studies. to use, for there are too many to include in this ta-
ble, but rather the cited example(s) are intended
to demonstrate an important strength or weak-
The laboratory test utilization
ness of the tool.
management toolbox
It is worth pointing out some tools that are not in-
The laboratory test utilization management tool- cluded in the toolbox because the available evi-
box is outlined in Table 1, with interventions that dence suggests that they are not terribly effective.
drive appropriate utilization sorted from strongest One of the common assumptions made about test
to weakest. For each tool, the intended target of utilization management is that clinicians would
the tool is listed, along with potential strengths behave more rationally if they saw the cost of the
and weaknesses, and finally a reference or exam- laboratory tests they ordered. The results of inter-
ple of how the tool can be used. The reference col- ventions that actually did this are mixed (36-38),
Table 1. The laboratory test utilization management toolbox.
Example/
Strength Tool Target Strengths Weaknesses
References
Obsolete tests,
“Quack” testing, This is the “Nuclear Only useful for tests with broad Bleeding time
Legitimate Option”, as it ensures consensus as to lack of utility, which and other
Strong Ban the test
tests used in a complete cease to is unusual. Specific individuals may “Antiquated”
inappropriate ordering destroy consensus. tests (42).
circumstances
All tests, A uniform policy
especially across a system can
those with be supported by a
utilization that formulary, in the same Requires authority and buy-in
Laboratory
is recognized, way as a pharmacy from multiple factions in a medical University of
Strong test
after analytics, formulary. Exceptions to system, and likely participation by Michigan (43).
formulary
to be above formulary can be vetted multiple specialties.
what is by a committee or
expected or individual tasked with
justifiable. these decisions.
Solomon
By far the most meta-analysis
effective, as the Logistically complex, as many (44),
Combined strengths of one parties (the laboratory, clinicians, Massachusetts
Strong Any test
intervention intervention often information services, payer systems, General Hospital
complement the etc…) need to be involved. Experience (45),
weaknesses of another. hematology
testing (46).
Depends on the payment system
present in the medical system.
Similar to banning Trends in
Perceived as unfair, especially if
Stop tests, this intervention reimbursement
the payer decides to stop paying
paying for is effective at nearly shown here
Strong Any test for something without adequate
unnecessary ceasing testing, (47), example of
justification. A physician may not
testing depending on who medical policy
know that a test will not be paid for,
decides to stop paying. here (40).
and the cost could be transferred to
the patient.
http://dx.doi.org/10.11613/BM.2014.025 Biochemia Medica 2014;24(2):223–34
229
Baird G. Utilization management
Table 1. The laboratory test utilization management toolbox.
Example/
Strength Tool Target Strengths Weaknesses
References
Make repeated
Worry amongst some physicians orders difficult
Powerful method of that they might “miss something”. through
reducing automatic Actual risk of missing something computerized
Ban repetitive Daily inpatient
Strong ordering that providers clinically important if a clinically order entry (48),
orders tests
often do not even know indicated repetitive test is disallowed ban standing
is occurring. (i.e. coagulation tests in patients on orders (49), limit
anticoagulants). tests to 24-hour
period (50).
Limiting testing to
Neurogenetic
physicians who know
Complex single testing diagnostic
how to use a test
Privilege tests, high Multiple physicians may want yield ~30% for
increases the prior
Strong ordering unit cost and/ privileges, even in the absence of very rare diseases
probability in the tested
providers or difficult to evidence that they deserve them. when expert
patients, increasing
interpret. providers order
cost effectiveness and
tests (51).
diagnostic yield.
Complex single Laboratory providers
tests, high can have more insight Time consuming for laboratory staff Large Genetics
Require high
Strong unit cost and/ into the utility of some or director, especially if there are no Sendout Testing
level approval
or difficult to tests than generalist laboratory housestaff to take calls. Intervention (52).
interpret. providers.
In the absence of a cultural change
Computerized order supporting modification of ordering Reducing testing
Change Any test in a
changes can be made practices, a complete stop to a in coronary care
computerized system with
Strong far more difficult to specific order may increase provider unit (53). Change
order entry computerized
subvert than paper abrasion. Unintended consequences to routine testing
options ordering.
order form changes. can result if one is not careful in menu (54).
designing the intervention.
Can work for
computerized or paper Requires an analyte for which a
ordering. Is a form of cheaper screening test exists. If
Any test where decision support that using paper forms, one must realize
a cheaper allows physician to that paper forms have a significant Reflexive ionized
Offer reflexive screening test follow correct testing half-life in medical systems, and calcium (32),
Strong
testing. can be used algorithm with one forms usually allow providers to coagulation
before a more order or click. Increases “write in” tests that they cannot find panels (55).
costly test. pre-test probability on the form, thus allowing clinicians
for more costly tests, to subvert the intent of the reflexive
making them more panel.
interpretable.
Provides data on
ordering to providers
who may otherwise
have no idea how they
Routine Outpatient
order tests, and thus
outpatient No one has to read the report card, report cards
Moderate/ Utilization may allow them to make
panel testing, especially if it is not associated with (56), intermittent
Strong report cards informed decisions.
daily testing on an incentive. feedback for
Can be paired with
inpatients. physicians (57,58).
reimbursement/financial
penalties, or associated
with peer feedback for
added strength.
Biochemia Medica 2014;24(2):223–34 http://dx.doi.org/10.11613/BM.2014.025
230
Baird G. Utilization management
Table 1. The laboratory test utilization management toolbox.
Example/
Strength Tool Target Strengths Weaknesses
References
Magnesium
Selected tests intervention (41),
“Pop-up fatigue” occurs if too many
Computerized with moderate Can provide support in 1,25 dihydroxy
reminders are implemented, leading
reminders/ volume and real time to physicians Vitamin D email
Moderate to provider abrasion. Providers
decision high likelihood to increase prior reminder (59)
will also cease to continue to read
support of being probabilities. [cited example
pop-ups after some time.
misordered. also uses
privileging].
Selected tests
with moderate
volume and
Redesigning test
Post high likelihood Can provide support in As opposed to pop-ups on
requisitions and
guidelines on of being real time to physicians computerized forms, written
Weak promulgation
paper order misordered, to increase prior guidelines on a paper are likely
of factsheets
forms but no probabilities. easier to ignore.
(46,60).
computerized
ordering
available.
Required as a
component of nearly
all successful utilization Example showing
management efforts. effect wearing off
Education Almost never works alone, or when
Interventions lacking an after time (38),
alone/call for it does, the effect wears off over time
Weak Any test educational component mixed effects
enhanced or completely disappears if new staff
risk failure due to lack of of reminding
vigilance takes over (i.e. in a teaching hospital).
buy-in from interested physicians of test
parties who do not costs (36-38).
understand the purpose
of the change.
however, and do not support whether or not pro- should be shown to ordering physicians, the truth
vision of cost information has any true effect on of the matter is that the most overutilised routine
ordering. While it does make sense that some in- laboratory tests do not have high unit costs, as the
formation about cost might influence physician variable cost for additional reagents needed to run
ordering behavior, the potential for a successful in- a test on a large automated platform are miniscule
tervention based on this information is confound- compared to the difficult-to-assess fixed costs of
ed by the fact that the true costs of laboratory maintaining that instrument and staffing required
tests are actually quite small, compared to more to run it. What we might want to show physicians
expensive items like radiologic scans, and perhaps at the time of order would be the potential down-
more frustrating, it is often very difficult to deter- stream costs associated with following up unnec-
mine what the actual cost of a laboratory test is in essary testing or the potential harm that could
some health care delivery systems. In the United arise to their patients, but those costs and harms
States, for example, specific laboratory tests are are difficult or impossible to tabulate.
not usually reimbursed by third party payers for Another financially-based tool that has been pro-
inpatient stays (adults with rare diseases and some posed is to simply pay physicians to stop ordering
children are notable exceptions), and the list prices laboratory testing. This is a difficult tool to admin-
of tests are often wildly inflated and/or kept secret. ister or evaluate ethically, but it has been done us-
Therefore, while it is isn’t even clear what cost ing trainees. In this study (39), medical residents
http://dx.doi.org/10.11613/BM.2014.025 Biochemia Medica 2014;24(2):223–34
231
Baird G. Utilization management
were paid in “book money” on a scale commensu- ducing serum magnesium testing was found to
rate with the size of their collective percentage re- paradoxically increase magnesium testing, for ex-
ductions in laboratory and radiology test ordering. ample, by inadvertently encouraging physicians to
Notably, residents were not individually rewarded order serum magnesium together with serum cal-
for their individual performance, but rather for the cium and phosphorus (41). The paradoxical effect
performance of a group. There were overall mod- found in this study was observed through con-
est reductions in test ordering through this inter- stant utilization monitoring, allowing the investi-
vention, but they were comparable to the control gators to institute a new, successful intervention,
group, and they rebounded to pre-intervention highlighting the fact that monitoring is a neces-
levels after the study ceased. Residents who par- sary part of all utilization management tools. With-
ticipated in simple chart reviews to study their out ongoing monitoring of utilization, it is impos-
own utilization patterns in this study had more sig- sible to assess the effectiveness of any utilization
nificant and longer-lasting reductions in test utili- management intervention. As was indicated in
zation. Rule 3 above, test utilization should be monitored
Whether or not tools based on provision of finan- on a timescale similar to how fast it is expected to
cial information or cash bonuses can be consid- change; it is not enough to measure utilization at
ered effective is perhaps not as important as the the end of a project or the end of the year.
fact that third party payers or health care systems A final critical factor required for using the utiliza-
are already implementing interventions based on tion toolbox is the development of a rapport be-
financial incentives (mostly negative incentives), tween the laboratory and the rest of the hospital.
and they will continue to implement more such in- Clinicians who order tests are rightfully wary of
centives. While early targets are likely to be areas mysterious and draconian utilization management
where the motivations for overutilization are pri- interventions forced upon them by unknown enti-
marily financially driven, i.e. fee-for-service reim- ties. Making things worse, in this author’s experi-
bursement of tests with negligible or no clinical ence, clinicians are often surprised to learn that
utility, US insurers are already starting to write there are doctoral-level scientists and clinicians
medical policies that incorporate test utilization employed by the laboratory who are concerned
principles (40). with optimal utilization of laboratory tests. As edu-
cation is a key tool in the toolbox, we in the labora-
Using the toolbox tory must therefore embrace our roles as educa-
While banning tests entirely or codifying a labora- tors to ensure that the ideas we have are under-
tory test formulary are listed in the toolbox as the stood and appreciated by clinicians and patients
strongest interventions, it must be restated that alike. When done appropriately, utilization man-
the most successful interventions in laboratory agement interventions can lead to improved mo-
test utilization management are those that com- rale not just amongst laboratory staff, but amongst
bine various tools. One can hardly expect an inter- all parties involved in the process. Without all three
vention that bans a physician’s favourite test to entities (laboratory, clinician, patient) having ade-
succeed without an educational component aimed quate information and interest in participation,
at explaining to that physician why the test is no optimal utilization of laboratory testing cannot be
longer available. The same goes for computerized achieved.
order entry changes. While these changes seem
the least disruptive, i.e. a single check box might Potential conflict of interest
disappear, the interconnectedness of health infor- Dr. Geoffrey Baird is a paid consultant and head of
mation systems is such that small changes to a lab- the clinical advisory board (paid positions) to Aval-
oratory’s ordering interface can have unexpected on Healthcare Solutions, a company based in the
and profound downstream changes. A computer- US that provides laboratory test utilization manage-
ized order entry-based intervention targeted at re- ment services to insurance companies in the US.
Biochemia Medica 2014;24(2):223–34 http://dx.doi.org/10.11613/BM.2014.025
232
Baird G. Utilization management
References
1. Smellie WS. Demand management and test request ratio- 17. Li Y, Iakoubova OA, Shiffman D, Devlin JJ, Forrester JS, Su-
nalization. Ann Clin Biochem 2012;49:323-36. http://dx.doi. perko HR. Kif6 polymorphism as a predictor of risk of co-
org/10.1258/acb.2011.011149. ronary events and of clinical event reduction by sta-
2. Griner PF, Liptzin B. Use of the laboratory in a teaching hos- tin therapy. Am J Cardiol 2010;106:994-8. http://dx.doi.
pital. Implications for patient care, education, and hospi- org/10.1016/j.amjcard.2010.05.033.
tal costs. Ann Intern Med 1971;75:157-63. http://dx.doi. 18. Krauss RM. Lipoprotein subfractions and cardiovascular di-
org/10.7326/0003-4819-75-2-157. sease risk. Curr Opin Lipidol 2010;21:305-11. http://dx.doi.
3. Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Arnaout R. The org/10.1097/MOL.0b013e32833b7756.
landscape of inappropriate laboratory testing: A 15-ye- 19. Kulkarni KR. Cholesterol profile measurement by vertical
ar meta-analysis. PLoS One 2013;8:e78962. http://dx.doi. auto profile method. Clin Lab Med 2006;26:787-802. http://
org/10.1371/journal.pone.0078962. dx.doi.org/10.1016/j.cll.2006.07.004.
4. Efron B. Mathematics. Bayes’ theorem in the 21st century. 20. Shannon C. Communication in the presence of noi-
Science 2013;340:1177-8. http://dx.doi.org/10.1126/scien- se. Proceedings of the IRE 1949;37:10-21. http://dx.doi.
ce.1236536. org/10.1109/JRPROC.1949.232969.
5. Brancati FL. The art of pimping. JAMA 1989;262:89-90. 21. Lyon AW, Higgins T, Wesenberg JC, Tran DV, Cembrowski
http://dx.doi.org/10.1001/jama.1989.03430010101039. GS. Variation in the frequency of hemoglobin A1c (HbA1c)
6. Witte DL. Wellness testing. Design and experience of an testing: Population studies used to assess compliance with
established program. Clin Lab Med 1993;13:481-90. clinical practice guidelines and use of hba1c to screen for
diabetes. J Diabetes Sci Technol 2009;3:411-7. http://dx.doi.
7. Jørgensen LG, Brandslund I, Hyltoft Petersen P. Should we
org/10.1177/193229680900300302.
maintain the 95 percent reference intervals in the era of
wellness testing? A concept paper. Clin Chem Lab Med 22. Miller C. Making sense of genetic tests. Clinical Laboratory
2004;42:747-51. http://dx.doi.org/10.1515/CCLM.2004.126. News 2012;38:15.
8. Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, 23. Bates DW, Boyle DL, Rittenberg E, Kuperman GJ, Ma’Luf N,
Hunninghake DB, et al. Implications of recent clinical trials Menkin V, et al. What proportion of common diagnostic
for the national cholesterol education program adult trea- tests appear redundant? Am J Med 1998;104:361-8. http://
tment panel iii guidelines. J Am Coll Cardiol 2004;44:720- dx.doi.org/10.1016/S0002-9343(98)00063-1.
32. http://dx.doi.org/10.1016/j.jacc.2004.07.001. 24. Branger PJ, Van Oers RJ, Van der Wouden JC, van der Lei J.
9. Tiwana SK, Rascati KL, Park H. Cost-effectiveness of expan- Laboratory services utilization: A survey of repeat investi-
ded newborn screening in texas. Value Health 2012;15:613- gations in ambulatory care. Neth J Med 1995;47:208-13.
21. http://dx.doi.org/10.1016/j.jval.2012.02.007. http://dx.doi.org/10.1016/0300-2977(95)00100-8.
10. Carroll AE, Downs SM. Comprehensive cost-utility analysis 25. Baigelman W, Bellin SJ, Cupples LA, Dombrowski D, Coldi-
of newborn screening strategies. Pediatrics 2006;117:S287-95. ron J. Overutilization of serum electrolyte determinations
in critical care units. Savings may be more apparent than
11. Pollitt RJ, Green A, McCabe CJ, Booth A, Cooper NJ, Leo-
real but what is real is of increasing importance. Inten-
nard JV, et al. Neonatal screening for inborn errors of me-
sive Care Med 1985;11:304-8. http://dx.doi.org/10.1007/
tabolism: Cost, yield and outcome. Health Technol Assess
BF00273541.
1997;1:i-iv, 1-202.
26. Dixon RH, Laszlo J. Ultilization of clinical chemistry ser-
12. Simpson N, Anderson R, Sassi F, Pitman A, Lewis P, Tu K, La-
vices by medical house staff. An analysis. Arch In-
nnin H. The cost-effectiveness of neonatal screening for cy-
tern Med 1974;134:1064-7. http://dx.doi.org/10.1001/
stic fibrosis: An analysis of alternative scenarios using a de-
archinte.1974.00320240098012.
cision model. Cost Eff Resour Alloc 2005;3:8. http://dx.doi.
org/10.1186/1478-7547-3-8. 27. Sox HC. Repeated testing. An overview and analysis. Int J
Technol Assess Health Care 1997;13:512-20. http://dx.doi.
13. Venditti LN, Venditti CP, Berry GT, Kaplan PB, Kaye EM, Glick
org/10.1017/S0266462300009983.
H, Stanley CA. Newborn screening by tandem mass spectro-
metry for medium-chain acyl-coa dehydrogenase deficien- 28. Bülow PM, Knudsen LM, Staehr P. [duplication in a medical
cy: A cost-effectiveness analysis. Pediatrics 2003;112:1005- department of tests previously performed in a primary sec-
15. http://dx.doi.org/10.1542/peds.112.5.1005. tor]. Ugeskr Laeger 1992;154:2497-501.
14. Wilson J, Jungner G. Principles and practice of mass scree- 29. Valenstein P, Leiken A, Lehmann C. Test-ordering by multi-
ning for disease. WHO Chronicle 1968;22. ple physicians increases unnecessary laboratory examina-
tions. Arch Pathol Lab Med 1988;112:238-41.
15. Kannel WB, Castelli WP, Gordon T. Cholesterol in the pre-
diction of atherosclerotic disease. New perspectives based 30. Rix DB, Stump G. Is there duplication of diagnostic test re-
on the framingham study. Ann Intern Med 1979;90:85-91. sults? Can Med Assoc J 1975;112:237-8, 41, 44.
http://dx.doi.org/10.7326/0003-4819-90-1-85. 31. Kwok J, Jones B. Unnecessary repeat requesting of tests: An
16. Roberts R. A customized genetic approach to the num- audit in a government hospital immunology laboratory.
ber one killer: Coronary artery disease. Curr Opin Cardi- J Clin Pathol 2005;58:457-62. http://dx.doi.org/10.1136/
ol 2008;23:629-33. http://dx.doi.org/10.1097/HCO.0b013e jcp.2004.021691.
32830e6b4e.
http://dx.doi.org/10.11613/BM.2014.025 Biochemia Medica 2014;24(2):223–34
233
Baird G. Utilization management
32. Baird G, Rainey P, Wener M, Chandler W. Reducing routine 46. Bareford D, Hayling A. Inappropriate use of laboratory ser-
ionized calcium measurement. Clin Chem 2009;55:533-40. vices: Long term combined approach to modify request pa-
http://dx.doi.org/10.1373/clinchem.2008.116707. tterns. BMJ 1990;301:1305-7. http://dx.doi.org/10.1136/
33. van Walraven C, Raymond M. Population-based study of bmj.301.6764.1305.
repeat laboratory testing. Clin Chem 2003;49:1997-2005. 47. Shahangian S, Alspach TD, Astles JR, Yesupriya A, Dettwyler
http://dx.doi.org/10.1373/clinchem.2003.021220. WK. Trends in laboratory test volumes for medicare part b re-
34. The association for clinical biochemistry and laboratory imbursements, 2000-2010. Arch Pathol Lab Med 2014;138:189-
medicine, national minimum retesting interval project: a 203. http://dx.doi.org/10.5858/arpa.2013-0149-OA.
final report detailing consensus recommendations for mi- 48. Neilson E, Johnson K, Rosenbloom S, Dupont W, Talbert D,
nimum retesting intervals for use in clinical biochemistry. Giuse D, et al. The impact of peer management on test-or-
Available at: http://www.acb.org.uk/docs/default-sour- dering behavior. Ann Intern Med 2004;141:196-204. http://
ce/guidelines/acb-mri-recommendations-a4-computer. dx.doi.org/10.7326/0003-4819-141-3-200408030-00008.
pdf?sfvrsn=2, ed., Vol., 2013. Accessed October 25, 2013.
49. Studnicki J, Bradham D, Marshburn J, Foulis P, Straumford
35. Plaisant C, Lam S, Lam SJ, Shneiderman B, Smith MS, Rose-
J. Measuring the impact of standing orders on laboratory
man D, et al. Searching electronic health records for tem-
poral patterns in patient histories: A case study with micro- utilization. Laboratory Medicine 1992;23:24-8.
soft amalga. AMIA Annu Symp Proc 2008:601-5. 50. May TA, Clancy M, Critchfield J, Ebeling F, Enriquez A, Galla-
36. Cummings KM, Frisof KB, Long MJ, Hrynkiewich G. The ef- gher C, et al. Reducing unnecessary inpatient laboratory te-
fects of price information on physicians’ test-ordering be- sting in a teaching hospital. Am J Clin Pathol 2006;126:200-6.
havior. Ordering of diagnostic tests. Med Care 1982;20:293- http://dx.doi.org/10.1309/WP59YM73L6CEGX2F.
301. http://dx.doi.org/10.1097/00005650-198203000-00006. 51. Edlefsen KL, Tait JF, Wener MH, Astion M. Utilization and di-
37. Bates DW, Kuperman GJ, Jha A, Teich JM, Orav EJ, agnostic yield of neurogenetic testing at a tertiary care faci-
Ma’luf N, et al. Does the computerized display of char- lity. Clin Chem 2007;53:1016-22. http://dx.doi.org/10.1373/
ges affect inpatient ancillary test utilization? Arch In- clinchem.2006.083360.
tern Med 1997;157:2501-8. http://dx.doi.org/10.1001/ 52. Dickerson J, Cole B, Conta J, Wellner M, Wallace S, Jack R, et
archinte.1997.00440420135015. al. Improving the value of costly genetic reference labora-
38. Miyakis S, Karamanof G, Liontos M, Mountokalakis TD. Fac- tory testing with active utilization management. Arch Pa-
tors contributing to inappropriate ordering of tests in an thol Lab Med 2014;138:110-3. http://dx.doi.org/10.5858/
academic medical department and the effect of an edu- arpa.2012-0726-OA.
cational feedback strategy. Postgrad Med J 2006;82:823-9. 53. Wang TJ, Mort EA, Nordberg P, Chang Y, Cadigan ME,
http://dx.doi.org/10.1136/pgmj.2006.049551. Mylott L, et al. A utilization management intervention to
39. Martin AR, Wolf MA, Thibodeau LA, Dzau V, Braunwald E. A reduce unnecessary testing in the coronary care unit. Arch
trial of two strategies to modify the test-ordering behavior Intern Med 2002;162:1885-90. http://dx.doi.org/10.1001/
of medical residents. N Engl J Med 1980;303:1330-6. http:// archinte.162.16.1885.
dx.doi.org/10.1056/NEJM198012043032304.
54. Shalev V, Chodick G, Heymann AD. Format change of a la-
40. Kansas BCBSo. Medical policy: Testing for vitamin d defici- boratory test order form affects physician behavior. Int J
ency. Available at: http://www.bcbsks.com/customerser- Med Inform 2009;78:639-44. http://dx.doi.org/10.1016/j.
vice/providers/MedicalPolicies/policies/policies/Testing_ ijmedinf.2009.04.011.
VitaminDDeficiency_2011-12-21.pdf. Accessed October 25,
2013. 55. Amukele TK, Baird GS, Chandler WL. Reducing the use of coa-
gulation test panels. Blood Coagul Fibrinolysis 2011;22:688-
41. Rosenbloom S, Chiu K, Byrne D, Talbert D, Neilson E, Miller
R. Interventions to regulate ordering of serum magnesi- 95. http://dx.doi.org/10.1097/MBC.0b013e32834b8246.
um levels: Report of an unintended consequence of decisi- 56. Staff LE. Improving laboratory test utilization through
on support. J Am Med Inform Assoc 2005;12:546-53. http:// physician report cards: An interview with dr. Kim riddell. La-
dx.doi.org/10.1197/jamia.M1811. boratory Errors and Patient Safety 2005;2:2-6.
42. Wu AH, Lewandrowski K, Gronowski AM, Grenache DG, So- 57. Bunting PS, Van Walraven C. Effect of a controlled feed-
koll LJ, Magnani B. Antiquated tests within the clinical pat- back intervention on laboratory test ordering by commu-
hology laboratory. Am J Manag Care 2010;16:e220-7. nity physicians. Clin Chem 2004;50:321-6. http://dx.doi.
43. Warren JS. Laboratory test utilization program: Structure org/10.1373/clinchem.2003.025098.
and impact in a large academic medical center. Am J Clin 58. Studnicki J, Bradham DD, Marshburn J, Foulis PR, Straum-
Pathol 2013;139:289-97. http://dx.doi.org/10.1309/AJCP4- fjord JV. A feedback system for reducing excessive labora-
G6UAUXCFTQF. tory tests. Arch Pathol Lab Med 1993;117:35-9.
44. Solomon DH, Hashimoto H, Daltroy L, Liang MH. Techniqu- 59. Dickerson JA, Jack RM, Astion ML, Cole B. Another labora-
es to improve physicians’ use of diagnostic tests: A new con- tory test utilization program: Our approach to reducing
ceptual framework. JAMA 1998;280:2020-7. http://dx.doi. unnecessary 1,25-dihydroxyvitamin d orders with a sim-
org/10.1001/jama.280.23.2020. ple intervention. Am J Clin Pathol 2013;140:446-7. http://
45. Kim JY, Dzik WH, Dighe AS, Lewandrowski KB. Utilization dx.doi.org/10.1309/AJCPQS40FZTLTQDH.
management in a large urban academic medical center: 60. Emerson JF, Emerson SS. The impact of requisition design
A 10-year experience. Am J Clin Pathol 2011;135:108-18. on laboratory utilization. Am J Clin Pathol 2001;116:879-
http://dx.doi.org/10.1309/AJCP4GS7KSBDBACF. 84. http://dx.doi.org/10.1309/WC83-ERLY-NEDF-471E.
Biochemia Medica 2014;24(2):223–34 http://dx.doi.org/10.11613/BM.2014.025
234
You might also like
- Lectures in Waste Water Analysis Preface: Genium Publishing CorporationDocument29 pagesLectures in Waste Water Analysis Preface: Genium Publishing Corporationmkra_natNo ratings yet
- Principles and Applications of Clinical Mass Spectrometry: Small Molecules, Peptides, and PathogensFrom EverandPrinciples and Applications of Clinical Mass Spectrometry: Small Molecules, Peptides, and PathogensNader RifaiNo ratings yet
- Inappropriateness in Laboratory Medicine An Elephant in The RoomDocument4 pagesInappropriateness in Laboratory Medicine An Elephant in The RoomomaromranNo ratings yet
- Responding To Large-Scale Testing Errors: Paul N. Valenstein, MD, G. Ann Alpern, MD, and David F. Keren, MDDocument7 pagesResponding To Large-Scale Testing Errors: Paul N. Valenstein, MD, G. Ann Alpern, MD, and David F. Keren, MDBanburryNo ratings yet
- CC IfccDocument11 pagesCC IfccRolando MaticNo ratings yet
- Westgard - Practica QC Pe Glob 2017Document20 pagesWestgard - Practica QC Pe Glob 2017anastasia buzaNo ratings yet
- Establishing Reference Intervals For Clinical Laboratory Test Results (2010)Document7 pagesEstablishing Reference Intervals For Clinical Laboratory Test Results (2010)Duy HoangNo ratings yet
- Gestión de Las Fases de Pre y Post-Analítica de La PDFDocument12 pagesGestión de Las Fases de Pre y Post-Analítica de La PDFUlises Saldías RoaNo ratings yet
- FDA Involvement and Lab Automation TrendsDocument5 pagesFDA Involvement and Lab Automation Trendsmartabak_polkadotNo ratings yet
- Ejifcc2008vol19no2pp095 105Document11 pagesEjifcc2008vol19no2pp095 105Chamara Nishshanka KasturirathnaNo ratings yet
- Nuclear Medicine AIDocument8 pagesNuclear Medicine AIdistruckNo ratings yet
- Oup Accepted Manuscript 2016Document11 pagesOup Accepted Manuscript 2016Alvionita AnggrainyNo ratings yet
- Evaluation of Analytical Methods Used For Regulation of Foods and DrugsDocument10 pagesEvaluation of Analytical Methods Used For Regulation of Foods and DrugsrenatoandaraNo ratings yet
- Errors Beyond the Lab: Understanding Errors in the Total Testing ProcessDocument10 pagesErrors Beyond the Lab: Understanding Errors in the Total Testing ProcessDiegoMaradónNo ratings yet
- Plebani 2006Document10 pagesPlebani 2006ami190No ratings yet
- 2021 Poor Labs Guide SampleDocument38 pages2021 Poor Labs Guide Samplelaboratorium spektrumNo ratings yet
- Validation Protocol For New Methods or Instruments in The Clinical LaboratoryDocument6 pagesValidation Protocol For New Methods or Instruments in The Clinical LaboratorymohammedNo ratings yet
- Pi Is 0895435617302998Document5 pagesPi Is 0895435617302998Fernando FernandezNo ratings yet
- Raise Standards For Preclinical Cancer ResearchDocument3 pagesRaise Standards For Preclinical Cancer ResearchMiguel CastroNo ratings yet
- Understand How It Works - NatureDocument2 pagesUnderstand How It Works - Naturehp2020No ratings yet
- Copia de Hartung2009Document6 pagesCopia de Hartung2009mjkoNo ratings yet
- Automation in The Clinical Microbiology Laboratory PAPERDocument7 pagesAutomation in The Clinical Microbiology Laboratory PAPERobakhit91No ratings yet
- Comparing and Optimizing Ultraviolet Germicidal IrDocument7 pagesComparing and Optimizing Ultraviolet Germicidal IrBachtiar HerdiantoNo ratings yet
- 10.1515 - CCLM 2018 0059Document8 pages10.1515 - CCLM 2018 0059Chris PaulNo ratings yet
- Errors in Laboratory Testing: Reducing Mistakes Throughout the Total Testing ProcessDocument11 pagesErrors in Laboratory Testing: Reducing Mistakes Throughout the Total Testing ProcessShahid HussainNo ratings yet
- Literature Review On Cleaning ValidationDocument7 pagesLiterature Review On Cleaning Validationiimytdcnd100% (1)
- Analysis of Environmental Microbiology Data From Cleanroom SamplesDocument5 pagesAnalysis of Environmental Microbiology Data From Cleanroom SamplesFran141985No ratings yet
- Study Limitations: Information Bias Misclassification BiasDocument30 pagesStudy Limitations: Information Bias Misclassification Biasjaydoc_paed@yahoo.co.inNo ratings yet
- HHS Public AccessDocument20 pagesHHS Public AccessdajcNo ratings yet
- Chodankar2021 Real World Evidence Vs RCTDocument4 pagesChodankar2021 Real World Evidence Vs RCTMumtaz MaulanaNo ratings yet
- Preanalytical Requirements of Urinalysis: Biochemia Medica February 2014Document17 pagesPreanalytical Requirements of Urinalysis: Biochemia Medica February 2014MARIO ALVARADONo ratings yet
- Bioburden ALERT Levels PDFDocument17 pagesBioburden ALERT Levels PDFRudhy21No ratings yet
- Pan American Society For Clinical Virology Position Statement On Fda Oversight of Laboratory-Developed Tests (LDTS)Document5 pagesPan American Society For Clinical Virology Position Statement On Fda Oversight of Laboratory-Developed Tests (LDTS)fdablogNo ratings yet
- Theory and Application in Transfusion Medicine at A Tertiary-Care InstitutionDocument6 pagesTheory and Application in Transfusion Medicine at A Tertiary-Care InstitutionfegariasNo ratings yet
- JOURNAL Errors in Clinical Laboratories or Errors in LaboratoryDocument11 pagesJOURNAL Errors in Clinical Laboratories or Errors in LaboratoryVincent ReyesNo ratings yet
- Positioning Inventory in Clinical Trial Supply Chains: Adam FleischhackerDocument21 pagesPositioning Inventory in Clinical Trial Supply Chains: Adam FleischhackerJohn AcidNo ratings yet
- Bertholf2017 Chapter LaboratoryStructureAndFunctionDocument23 pagesBertholf2017 Chapter LaboratoryStructureAndFunctionci8084102No ratings yet
- (Panic) Laboratory (Parameter) : PolicyDocument1 page(Panic) Laboratory (Parameter) : Policymy accountNo ratings yet
- Horwitz 1982Document6 pagesHorwitz 1982jhoelmcgNo ratings yet
- Forum - Test SafetyDocument2 pagesForum - Test SafetyhhhNo ratings yet
- The Changing Landscape of Product Development and Randomized TrialsDocument7 pagesThe Changing Landscape of Product Development and Randomized TrialsAymen BekirNo ratings yet
- Favaloro 2010Document13 pagesFavaloro 2010Yohana SetiawanNo ratings yet
- BMJ I6 FullDocument5 pagesBMJ I6 FullRobertoNo ratings yet
- 1986 - A Framework For Clinical Evaluation of Diagnostic TechnologiesDocument8 pages1986 - A Framework For Clinical Evaluation of Diagnostic TechnologiesA CNo ratings yet
- Apps To Help You Manage Your Ballya in Vitro Diagnostics Rapid Test ManufacturerDocument3 pagesApps To Help You Manage Your Ballya in Vitro Diagnostics Rapid Test ManufacturerdenopehecpNo ratings yet
- validacion PCR COVID 19Document11 pagesvalidacion PCR COVID 19Rodolfo VelazcoNo ratings yet
- Using Routine Comparative Data To Assess The Quality of Health Care: Understanding and Avoiding Common PitfallsDocument7 pagesUsing Routine Comparative Data To Assess The Quality of Health Care: Understanding and Avoiding Common Pitfallsujangketul62No ratings yet
- Linical Aboratory O: S H, MT (Ascp) SH B A. K, E D, Mls (Ascp), Cls (Nca)Document5 pagesLinical Aboratory O: S H, MT (Ascp) SH B A. K, E D, Mls (Ascp), Cls (Nca)Tito LeopardoNo ratings yet
- Ro-Ils Project 1Document4 pagesRo-Ils Project 1api-633652323No ratings yet
- J PH & Bio AnalysisDocument9 pagesJ PH & Bio AnalysisMaría Belén OlivarezNo ratings yet
- General Chapters - 1211 - STERILIZATION AND STERILITY ASSURANCE OF COMPENDIAL ARTICLESDocument11 pagesGeneral Chapters - 1211 - STERILIZATION AND STERILITY ASSURANCE OF COMPENDIAL ARTICLESHaythemOrabiNo ratings yet
- Accuracy of Plate CountDocument5 pagesAccuracy of Plate CountApar DholakiaNo ratings yet
- Verification of Quantitative RT PCR MethodsDocument12 pagesVerification of Quantitative RT PCR Methodsanastasia buzaNo ratings yet
- Ethical Considerations of Preclinical Testing: Allen GoldenthalDocument3 pagesEthical Considerations of Preclinical Testing: Allen GoldenthalTh MaNo ratings yet
- Clinical Chemistry - Quality Management and InformaticsDocument5 pagesClinical Chemistry - Quality Management and Informaticsrosellae.No ratings yet
- Quality Control in LaboratoriesDocument31 pagesQuality Control in LaboratoriesMona MostafaNo ratings yet
- Virtual Trials and Real-World Evidence: Understanding Foundational NeedsDocument4 pagesVirtual Trials and Real-World Evidence: Understanding Foundational NeedsRoopali AggarwalNo ratings yet
- Dissertation ErstgutachterDocument6 pagesDissertation ErstgutachterPurchaseCollegePapersUK100% (1)
- Parenteral Quality ControlDocument388 pagesParenteral Quality Controlsaeedazadi1352No ratings yet
- 1-Vitamin K Antagonist:: A - WarfarinDocument20 pages1-Vitamin K Antagonist:: A - WarfarinomaromranNo ratings yet
- 2 - Selective Media:: Type of Enriched MediaDocument4 pages2 - Selective Media:: Type of Enriched MediaomaromranNo ratings yet
- Incubation The Coagulase in Tube Over Night##Document5 pagesIncubation The Coagulase in Tube Over Night##omaromranNo ratings yet
- 19Document8 pages19omaromranNo ratings yet
- Incubation The Coagulase in Tube Over Night##Document5 pagesIncubation The Coagulase in Tube Over Night##omaromranNo ratings yet
- 20Document11 pages20omaromranNo ratings yet
- Mohamed SulimanDocument6 pagesMohamed SulimanomaromranNo ratings yet
- 1-The Body Obtain Energy From Lipid or Protein Called: A-B - CDocument11 pages1-The Body Obtain Energy From Lipid or Protein Called: A-B - ComaromranNo ratings yet
- Lysosymes Are Found in The Following ExceptDocument17 pagesLysosymes Are Found in The Following ExceptomaromranNo ratings yet
- 7Document5 pages7omaromranNo ratings yet
- Hereditary Fructose Tolerance By:: 1 - G-6-P 2 - Fructose - 6 - P Aldose 3-1-2-6 - P 4 - FructokinaseDocument2 pagesHereditary Fructose Tolerance By:: 1 - G-6-P 2 - Fructose - 6 - P Aldose 3-1-2-6 - P 4 - FructokinaseomaromranNo ratings yet
- اسئلة الهيئة نموذج 4Document14 pagesاسئلة الهيئة نموذج 4حمزة الفنينيNo ratings yet
- 68-The Immunoglobin That Has Smallest Amount in The Serum IsDocument7 pages68-The Immunoglobin That Has Smallest Amount in The Serum IsomaromranNo ratings yet
- Urine Blood Stool Skin Scraping#: 1/ Sample For ScabiesDocument6 pagesUrine Blood Stool Skin Scraping#: 1/ Sample For ScabiesomaromranNo ratings yet
- Bone Marrow Aspirate: Psedomomas AeruginosaDocument5 pagesBone Marrow Aspirate: Psedomomas AeruginosaomaromranNo ratings yet
- Done By:lola Elgaily: Influenza Viruses AreDocument9 pagesDone By:lola Elgaily: Influenza Viruses AreomaromranNo ratings yet
- Finding of A Typical Fertilized Egg in Stool #Document3 pagesFinding of A Typical Fertilized Egg in Stool #omaromranNo ratings yet
- Reduction in Unnecessary Clinical Laboratory Testing Throgh UtilizationDocument10 pagesReduction in Unnecessary Clinical Laboratory Testing Throgh UtilizationomaromranNo ratings yet
- Acid Base Balance: Respiratory A - Pco2Document1 pageAcid Base Balance: Respiratory A - Pco2omaromranNo ratings yet
- 8Document2 pages8omaromranNo ratings yet
- 10Document1 page10omaromranNo ratings yet
- 1 / RH Antigen: DceceDocument5 pages1 / RH Antigen: DceceomaromranNo ratings yet
- 2019 Managing Inappropriate Utilization of Laboratory Resources9Document9 pages2019 Managing Inappropriate Utilization of Laboratory Resources9omaromranNo ratings yet
- 22Document3 pages22omaromranNo ratings yet
- The Role of Laboratory in Ensuring Appropriate Test RequestsDocument21 pagesThe Role of Laboratory in Ensuring Appropriate Test RequestsomaromranNo ratings yet
- Laboratory Test InappropriatenessDocument14 pagesLaboratory Test InappropriatenessomaromranNo ratings yet
- Reduction in Unnecessary Clinical Laboratory TestingDocument10 pagesReduction in Unnecessary Clinical Laboratory TestingomaromranNo ratings yet
- Strategies To Promote Rational Clinical Chemistry Test UtilizationDocument9 pagesStrategies To Promote Rational Clinical Chemistry Test UtilizationomaromranNo ratings yet
- The Laboratory Test Utilization Management ToolboxDocument12 pagesThe Laboratory Test Utilization Management ToolboxomaromranNo ratings yet
- Decision Model Using ExcelDocument236 pagesDecision Model Using Excelসামিউল ইসলাম রাজু100% (3)
- Inductive Proximity Sensors: Brett Anderson ECE 5230 Assignment #1Document27 pagesInductive Proximity Sensors: Brett Anderson ECE 5230 Assignment #1Rodz Gier JrNo ratings yet
- PEA ClocksDocument50 pagesPEA ClocksSuresh Reddy PolinatiNo ratings yet
- Basic C MCQ - FinalDocument51 pagesBasic C MCQ - FinalDhivya DharshniNo ratings yet
- Anchor BayDocument56 pagesAnchor BayAnonymous dHyxmDNo ratings yet
- Solidworks Flow SimulationDocument7 pagesSolidworks Flow SimulationpatrickNX94200% (1)
- Kollidon 30 Technical InformationDocument10 pagesKollidon 30 Technical InformationhomarearisugawaNo ratings yet
- MCB and ELCB PDFDocument35 pagesMCB and ELCB PDFChris AntoniouNo ratings yet
- Effect of Bond Administration On Construction Project DeliveryDocument7 pagesEffect of Bond Administration On Construction Project DeliveryOlefile Mark MolokoNo ratings yet
- Lubricants For Cement ProductionDocument21 pagesLubricants For Cement Productiongrameshkreddy2013100% (1)
- D Lucky Labeling of Graphs PDFDocument6 pagesD Lucky Labeling of Graphs PDFtony augustineNo ratings yet
- Conceptual Data Modeling and Database Design Volume 1 - The Shortest Advisable Path A Fully Algorithmic ApproachDocument662 pagesConceptual Data Modeling and Database Design Volume 1 - The Shortest Advisable Path A Fully Algorithmic ApproachErkan50% (2)
- T24 IN2 RoutinesDocument29 pagesT24 IN2 RoutinesKhalil ArifiNo ratings yet
- Booklet Momentum BWFDocument22 pagesBooklet Momentum BWFReem AshrafNo ratings yet
- Prepare and Interpret Technical DrawingDocument5 pagesPrepare and Interpret Technical DrawingDwin Rosco75% (4)
- Er DiagramsDocument20 pagesEr DiagramsMatthew BloomfieldNo ratings yet
- Design of Three Span Steel Composite FlyoverDocument85 pagesDesign of Three Span Steel Composite FlyoverStructural SpreadsheetsNo ratings yet
- General Physics1 Q2 W8 Module8 ThermodynamicsDocument23 pagesGeneral Physics1 Q2 W8 Module8 ThermodynamicsRegine Ann ViloriaNo ratings yet
- ME4111 Engineering and Mechanical PrinciplesDocument5 pagesME4111 Engineering and Mechanical PrinciplesEdvard StarcevNo ratings yet
- Writing Iap Smarten Up in Maths Age 7 8Document38 pagesWriting Iap Smarten Up in Maths Age 7 8lphoune100% (1)
- Lectures Accompanying The Book - Solid State Physics - An (PDFDrive)Document148 pagesLectures Accompanying The Book - Solid State Physics - An (PDFDrive)Raza Ali RazaNo ratings yet
- Manuscript 123Document46 pagesManuscript 123Datuzuharto Sultan100% (1)
- Chapter 3 Step Wise An Approach To Planning Software Projects 976242065Document31 pagesChapter 3 Step Wise An Approach To Planning Software Projects 976242065RiajiminNo ratings yet
- PT32 12Document3 pagesPT32 12sergiuserbanNo ratings yet
- IOP Conference Series: Materials Science and EngineeringDocument9 pagesIOP Conference Series: Materials Science and EngineeringMahesh MNo ratings yet
- Jm-10 Operation Manual Rev02 UnlockedDocument121 pagesJm-10 Operation Manual Rev02 UnlockedAlan Jimenez GonzalezNo ratings yet
- SamplingDocument12 pagesSamplingΔημητρηςΣαρακυρουNo ratings yet
- A Git Cheat Sheet (Git Command Reference) - A Git Cheat Sheet and Command ReferenceDocument14 pagesA Git Cheat Sheet (Git Command Reference) - A Git Cheat Sheet and Command ReferenceMohd AzahariNo ratings yet
- It Tigear2Document2 pagesIt Tigear2rrobles011No ratings yet
- Z 80 HelptopicsDocument5 pagesZ 80 HelptopicsEverly NNo ratings yet