Professional Documents
Culture Documents
Complications: Acute Pancreatitis
Uploaded by
Nikey Lim0 ratings0% found this document useful (0 votes)
8 views2 pagesApproach to acute pancreatitis
Original Title
Acute Pancreatitis
Copyright
© © All Rights Reserved
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentApproach to acute pancreatitis
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
8 views2 pagesComplications: Acute Pancreatitis
Uploaded by
Nikey LimApproach to acute pancreatitis
Copyright:
© All Rights Reserved
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 2
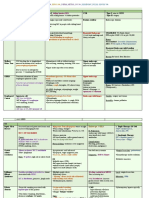
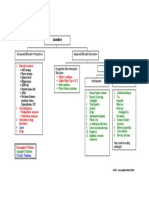
Acute Pancreatitis Abdominal aortic dissection Cholangitis
Basal pneumonia Acute cholecystitis
Pathophysiology
Progression Complications
Pancreatic complications
1. Acute oedematous pancreatitis: interstitial inflammation &
oedema with peripancreatic fat necrosis. Sparing of acinar cells
Pancreatic Initial fragile pseudocapsule matures into a fibrous capsule over 6 wks
pseudocyst Usually asymptomatic & resolves if small
2. Necrotising pancreatitis: destruction of acinar cells
Large pseudocyst may cause abdo pain, and compress / erode
3. Acute haemorrhagic pancreatitis: bleeding into pancreas and surrounding structures
retroperitoneum. Pancreatic ascites Leakage of pancreatic secretion into peritoneal cavity
Involvement of adjacent structures: CBD, duodenum, splenic veins, May leak into thoracic cavity causing pleural effusion or
transverse colon bronchopancreatic fistula
Severity dependent on balance between proteolytic enzymes & Abscess Infection of necrotic pancreatic tissue
antiproteolytic factors (eg trypsin inhibitor, 1-antitrypsin) Gastrointestinal complications
Factors influencing acute pancreatitis: UGI bleed Gastric / duodenal erosion
1. Defective intracellular tpt & secretion of pancreatic zymogens Variceal Splenic or portal vein thrombosis causes portal hpt, resulting in
haemorrhage oesophageal varices. Treat with thrombolysis.
2. Hyperstimulation of pancreas eg EtOH, fat erosion into colon
3. Pancreatic duct obstruction eg choledocholithiasis Duodenal Compression by pancreatic mass
4. Reflux of infected bile/duodenal contents into pancreatic duct eg obstruction
sphincter of Oddi, disruption by gallstones Obstructive Compression of CBD by pancreatic mass
jaundice
Causes: “GET SMASHED” Systemic complications
Gallstones Scorpion venom
Shock, renal Increased vascular permeability
failure, DIC
Ethanol Hyperlipidaemia / HyperCa / Hypoxia ARDS due to microthrombi in pulmonary vessels
Trauma Hypothermia Hyperglycaemia Disruption of Islets of Langerhans with altered insulin/glucagon axis
Steroids ERCP Hypocalcaemia Sequestration of Ca in fat necrosis resulting in decreased ionized Ca++
Mumps Drugs (azathioprine, thiazides serum albumin Increased capillary permeability
Autoimmune (PAN) diuretics, Na valproate)
Diagnosis
Clinical features Based on clinical pic, elevated serum amylase or lipase and U/S
Severe upper abdominal pain radiating Epigastric tenderness
evidence of pancreatic swelling
to back, better on sitting forward. Absent / quiet bowel sounds due to
Nausea / vomiting paralytic ileus
Fever Hypovolaemic shock + oliguria Investigations
Jaundice Signs of haemorrhagic pancreatitis – Serum > 1000 U/L or > 4 times the normal range. May be less in acute exacerbation of
Amylase chronic pancreatitis due to reduced vol. of functioning tissue.
No guarding/rebound (c.f. perforated discoloration of flanks (Grey Turner’s
peptic ulcer) sign) or periumbilicus (Cullen’s sign) Returns to normal within 24-48 hrs. Dx by raised urinary amylase: creatinine
ratio thereafter
Persistently elevated amylase suggests pseudocyst formation
DDx Mild elevations in intestinal ischaemia, perforated peptic ulcer & ruptured
Perforated viscus Perforated peptic ulcer ovarian cyst
Myocardial infarction Acute exacerbation of peptic ulcer NO prognostic value
Abdominal aortic aneurysm Biliary colic AXR Loss of psoas shadow (retroperitoneal fluid)
Sentinel loop of proximal jejunum (solitary air-filled dilatation) 8. pts with signs of cholangitis (fever, TWC, cholestatic LFT): Blood
U/S Confirm diagnosis C/S + start IV ABx (3rd generation cephalosporin eg ceftriaxone +
Show gallstones, biliary obstruction or pseudocysts metronidazole). ABx not necessary if not complicated.
Endoscopic DGIM – Last updated March 2005
Show gallstones, biliary obstruction or pseudocysts 9. I/O charting
U/S, ERCP
or MRCP
10. Admit
CT scan Assess viability of pancreas
Necrotising pancreatitis shows decreased enhancement on IV contrast injection Severe pancreatitis: CVP monitoring if in shock. Intubate and
Gas within necrotic material suggests infection and impending abscess ventilate if necessary, start prophylactic ABx
formation – percutaneous aspiration of material for culture required. Non-acute Mx:
Assess peripancreatic organ involvement Feeding: withhold enteral feeding, but start parenteral
Serial CRP Indicator of progress of pancreatitis nutrition early due to catabolic state
Thromboembolism prophylaxis: SQ heparin
Assessing severity Necrotising pancreatitis / pancreatic abscess: surgical
1. 3rd space fluid loss / clinical dehydration haemoconcentration >10% debridement + drainage
reduced end-organ confusion raised urea/creatinine
perfusion ascites metabolic acidosis
Pancreatic pseudocyst: drainage into stomach / duodenum
2. Signs of organ failure Coagulopathy (DIC screen +) after 6 wks when pseudocapsule has matured.
Renal failure ( creatinine, metab acidosis, K+) Pancreatic ascites: distal pancreatectomy
Respiratory distress & hypoxia ( PaO2 & SaO2) PT presenting with jaundice or cholangitis: ERCP to dx
3. Signs of sepsis Local septic Cx (eg pancreatic abscess, infected pancreatic and treat choledocholithiasis.
necrosis) usually occurs only after 1 wk
Consider non-pancreatic cause of sepsis eg cholangitis
secondary to biliary obstruction – look for cholestatic LFT Prognostic factors: Modified Glasgow Criteria (predicts mortality)
picture PO2 < 8kPa Glucose > 10mmol/L
4. Signs of severe Grey-Turner’s sign, Cullen’s sign WBC > 15 X 109/L Urea > 16mmol/L (post rehydration)
pancreatitis Signs of hypo Ca: carpopedal spasm, tetany
Albumin < 30 g/L ALT > 200U/L
Blood glucose <10 mmol/L
Serum Ca < 2 mmol/L (corrected) LDH > 600U/L
Acute Management c.f. Ranson’s criteria, which is only valid for alcoholic pancreatitis. However, Modified
Main aims: restore blood volume, rest gut, treat underlying cause Glasgow criteria does not allow for easy follow up assessment of PT’s progress.
1. Keep pt fasted Overall mortality: 10%
2. ABC and monitoring Necrotising pancreatitis / pancreatic abscess mortality: 50%
3. Drip and suck
4. Supplemental O2 Ranson’s criteria:
5. Inx: Serum amylase, FBC, U/E/Cr, Ca, Glucose, LFT, LDH, ABG On admission After 48h
blood C/S; CXR – assess for respiratory compromise, exclude basal > 55 y.o Serum Ca < 2 mmol/L
pneumonia and perforated viscus, ECG + cardiac enzymes – bld glucose >11 mmol/L Bld urea increase by 10 mmol/L
exclude AMI/atypical angina TW > 16 x 10 ^9/L Hct falls by > 10%
LDH > 70 IU/L Base excess > -4
6. Analgesia – Pethidine (avoid NSAIDs due to nephrotoxicity), AST > 60 IU/L PaO2 < 60mmHg (8kPa)
antispamodics. Not advisable if PT is in shock. Estimated fluid sequestration > 6L
7. in pt w hx of PUD: Prophylactic acid suppressive Rx
DGIM – Last updated March 2005
You might also like
- Acute PancreatitisDocument31 pagesAcute PancreatitisAmoroso, Marian Corneth D.No ratings yet
- Pancreatitis & Pseudocyst in ChildrenDocument56 pagesPancreatitis & Pseudocyst in ChildrendrkiranmNo ratings yet
- 3-Pancreas-SG-2022-After Class-FinalDocument20 pages3-Pancreas-SG-2022-After Class-FinalTyler YounNo ratings yet
- Acute AbdomenDocument47 pagesAcute AbdomenDani LeeNo ratings yet
- Not Activity No. 7Document12 pagesNot Activity No. 7Patricia Marie Laman YadaoNo ratings yet
- MS A - Mod 1 Cont Hepatobiliary and Pancreatic DisorderDocument1 pageMS A - Mod 1 Cont Hepatobiliary and Pancreatic DisorderCrisanta Grace OpondaNo ratings yet
- Gastrointestinal SurgeryDocument12 pagesGastrointestinal SurgeryHafsa AliNo ratings yet
- Kidney Disorders Final PresentationDocument20 pagesKidney Disorders Final PresentationElla PaezNo ratings yet
- 116 Theory NotesDocument84 pages116 Theory NotesKirstie Goc-ongNo ratings yet
- Pancreatitis PresentationDocument41 pagesPancreatitis Presentationak2621829No ratings yet
- Emergency Medicine: Acute AbdomenDocument33 pagesEmergency Medicine: Acute AbdomenPrashant MishraNo ratings yet
- MS-2 GallbladderDocument2 pagesMS-2 Gallbladderelijahdale.guillergan-05No ratings yet
- Week 2Document5 pagesWeek 2Maica LectanaNo ratings yet
- Acute Pancreatitis: Chris Mathew KoshyDocument100 pagesAcute Pancreatitis: Chris Mathew KoshyabelNo ratings yet
- PathoDocument7 pagesPathoAnonymous 87fNoO2fhVNo ratings yet
- Hypovolemic Shock PathophysiologyDocument8 pagesHypovolemic Shock PathophysiologyKAYCEENo ratings yet
- Liver CirrhosisDocument44 pagesLiver CirrhosisaboubakarylwabukobaNo ratings yet
- Diseases of Pancreas Ug ClassDocument107 pagesDiseases of Pancreas Ug ClassSrinivas PamarthiNo ratings yet
- Disorders of PancreasDocument43 pagesDisorders of Pancreasindu mathiNo ratings yet
- Acute PancreatitisDocument12 pagesAcute Pancreatitissho bartNo ratings yet
- Biliary Tract Dis Pancreatitis 2015Document143 pagesBiliary Tract Dis Pancreatitis 2015eiad-mahmoudNo ratings yet
- Acute AbdomenDocument25 pagesAcute AbdomenAli TahirNo ratings yet
- Pemicu 1 KGD: Mustika Rukmana 405130182 Kel 6Document54 pagesPemicu 1 KGD: Mustika Rukmana 405130182 Kel 6tikaNo ratings yet
- SURG Abomen CLINICSDocument5 pagesSURG Abomen CLINICSMeg AmoonNo ratings yet
- Constipation in Adults Abdominal Pain, Acute: PathophysiologyDocument8 pagesConstipation in Adults Abdominal Pain, Acute: PathophysiologyimanuelNo ratings yet
- Gi HyDocument2 pagesGi HyAbhineeth BhatNo ratings yet
- Cholelithiasis CholecystitisDocument1 pageCholelithiasis Cholecystitissamliebareng77No ratings yet
- Obstructive JaundiceDocument15 pagesObstructive JaundiceUjas Patel100% (4)
- Pancreatitis: M.N. Homoeopathic Medical College & Research Institute, Bikaner B.H.M.S. III YearDocument36 pagesPancreatitis: M.N. Homoeopathic Medical College & Research Institute, Bikaner B.H.M.S. III YearYamini SoniNo ratings yet
- Acute Inflammation of Abdominal TigerDocument100 pagesAcute Inflammation of Abdominal TigerJu Lie AnnNo ratings yet
- Curs 9 Digestiv 2.ppsxDocument45 pagesCurs 9 Digestiv 2.ppsxCiceu AdrianaNo ratings yet
- Acute Pancreatitis: Dr. Ali Raza Dr. Talha Javed CHDocument31 pagesAcute Pancreatitis: Dr. Ali Raza Dr. Talha Javed CHahmad frazNo ratings yet
- Bile, Bile Duct and Pancreatic DiseaseDocument82 pagesBile, Bile Duct and Pancreatic Diseaseshahrul rahmanNo ratings yet
- Final CC EdemaDocument31 pagesFinal CC EdematabatchNo ratings yet
- Acute Pancreatitis NOTESDocument17 pagesAcute Pancreatitis NOTESsameeha semiNo ratings yet
- Critical Disorders and Complications of The GDocument2 pagesCritical Disorders and Complications of The GVictor MurilloNo ratings yet
- ACUTE ABDOMEN by DR NajamDocument65 pagesACUTE ABDOMEN by DR NajamdasdasfNo ratings yet
- Surgery EORDocument76 pagesSurgery EORAndrew BowmanNo ratings yet
- Sunday, 30 August 2020 1:54 PM: Whitcomb-D-NEJM-2006 PDFDocument2 pagesSunday, 30 August 2020 1:54 PM: Whitcomb-D-NEJM-2006 PDFMichelle De FreitasNo ratings yet
- Liver abscess: Ext. กันตา เพชรชนะ B5760206Document11 pagesLiver abscess: Ext. กันตา เพชรชนะ B5760206nontapat paesarochNo ratings yet
- Group 3 - Acute PancreatitisDocument5 pagesGroup 3 - Acute Pancreatitismelba040510No ratings yet
- Cirrhosis of LiverDocument106 pagesCirrhosis of LiveraahadNo ratings yet
- Acute PancreatitisDocument19 pagesAcute PancreatitisFloida Rose KatterNo ratings yet
- CholelithiasisDocument8 pagesCholelithiasissaranya amuNo ratings yet
- Acute Abdomen FinalDocument105 pagesAcute Abdomen FinalAizul AzmiNo ratings yet
- Liver Curs 2009Document215 pagesLiver Curs 2009Mohammad_Islam87No ratings yet
- PancreatitisDocument2 pagesPancreatitisJelica ConsultadoNo ratings yet
- Gall StoneDocument64 pagesGall Stonepoonam advaniNo ratings yet
- Acute Pancreatitis: Sudden Severe Abdominal Pain Systemic UpsetDocument40 pagesAcute Pancreatitis: Sudden Severe Abdominal Pain Systemic UpsetcoolcaesarNo ratings yet
- Trans Hepatobiliary SystemDocument5 pagesTrans Hepatobiliary SystemJulie CatianNo ratings yet
- Chronic Pancreatitis: Causes ComplicationsDocument1 pageChronic Pancreatitis: Causes ComplicationsNikey LimNo ratings yet
- Angel Problem 4a GITDocument48 pagesAngel Problem 4a GITMaxend Arselino SilooyNo ratings yet
- Materi Kep. Kritis Acute GI BleedingDocument35 pagesMateri Kep. Kritis Acute GI Bleedingharsani auroraNo ratings yet
- PP PancreatitisDocument25 pagesPP PancreatitisBrahmayda Wiji LestariNo ratings yet
- Ward CallsDocument17 pagesWard Callsdewitt.bernardNo ratings yet
- Chronic Pancreatitis 1Document21 pagesChronic Pancreatitis 1Bala DhanaNo ratings yet
- Gastrointestinal System (Letu Da) PDFDocument74 pagesGastrointestinal System (Letu Da) PDFNafiul Islam100% (4)
- Acute Gi Bleeding: Rohman AzzamDocument34 pagesAcute Gi Bleeding: Rohman AzzamgebyarayuNo ratings yet
- Chronic Liver DiseaseDocument3 pagesChronic Liver DiseaseNikey LimNo ratings yet
- Sleep-Related Upper Airway Obstruction in ChildrenDocument1 pageSleep-Related Upper Airway Obstruction in ChildrenNikey LimNo ratings yet
- Resp 5Document2 pagesResp 5Nikey LimNo ratings yet
- Resp 3Document2 pagesResp 3Nikey LimNo ratings yet
- Resp 3Document2 pagesResp 3Nikey LimNo ratings yet
- Jaundice Classification in AdultsDocument1 pageJaundice Classification in AdultsNikey LimNo ratings yet
- History: Clinical ManifestationsDocument2 pagesHistory: Clinical ManifestationsNikey LimNo ratings yet
- Chronic Pancreatitis: Causes ComplicationsDocument1 pageChronic Pancreatitis: Causes ComplicationsNikey LimNo ratings yet
- Paeds Surgery 4Document2 pagesPaeds Surgery 4Nikey LimNo ratings yet
- Paeds Surgery 3Document2 pagesPaeds Surgery 3Nikey LimNo ratings yet
- Resp 1Document2 pagesResp 1Nikey LimNo ratings yet
- Section 04: Being A ManagerDocument2 pagesSection 04: Being A ManagerNikey LimNo ratings yet
- Paeds Surgery 2Document2 pagesPaeds Surgery 2Nikey LimNo ratings yet
- Ideas From The One-Minute Manager: Strategic ManagementDocument2 pagesIdeas From The One-Minute Manager: Strategic ManagementNikey LimNo ratings yet
- Paeds Surgery 1Document2 pagesPaeds Surgery 1Nikey LimNo ratings yet
- Doctor/Patient Communication: Family SupportDocument2 pagesDoctor/Patient Communication: Family SupportNikey LimNo ratings yet
- Inborn Errors of MetabolismDocument2 pagesInborn Errors of MetabolismNikey LimNo ratings yet
- Heart Failure 2Document2 pagesHeart Failure 2Nikey LimNo ratings yet
- Proteus: Boys Girls (Form Phosphate Stone) Pseudomonas: Structural Abnormality in UT Plastic CathetersDocument2 pagesProteus: Boys Girls (Form Phosphate Stone) Pseudomonas: Structural Abnormality in UT Plastic CathetersNikey LimNo ratings yet
- Care of The Patient and His FamilyDocument2 pagesCare of The Patient and His FamilyNikey LimNo ratings yet
- Section 03 Concepts of Family MedicineDocument2 pagesSection 03 Concepts of Family MedicineNikey LimNo ratings yet
- Care of The Patient and His FamilyDocument2 pagesCare of The Patient and His FamilyNikey LimNo ratings yet
- Heart Failure 1Document2 pagesHeart Failure 1Nikey LimNo ratings yet
- Salivary Gland TumoursDocument2 pagesSalivary Gland TumoursNikey LimNo ratings yet
- Salivary Gland TumoursDocument2 pagesSalivary Gland TumoursNikey LimNo ratings yet
- Respiratory DiseaseDocument1 pageRespiratory DiseaseNikey LimNo ratings yet
- Bradycardia and Conduction Disorders Sinus Bradycardia (Fig. 1.6)Document2 pagesBradycardia and Conduction Disorders Sinus Bradycardia (Fig. 1.6)Nikey LimNo ratings yet
- Arrhythmia 3Document2 pagesArrhythmia 3Nikey LimNo ratings yet
- Respiratory DiseaseDocument2 pagesRespiratory DiseaseNikey LimNo ratings yet
- BS en 13369-2018 - TC - (2020-11-30 - 09-45-34 Am)Document164 pagesBS en 13369-2018 - TC - (2020-11-30 - 09-45-34 Am)Mustafa Uzyardoğan100% (1)
- IIRDocument2 pagesIIRJagan FaithNo ratings yet
- Factors Affecting Pakistani English Language LearnersDocument19 pagesFactors Affecting Pakistani English Language LearnersSaima Bint e KarimNo ratings yet
- VW 60330 2009 12 eDocument29 pagesVW 60330 2009 12 eAmir Borhanipour100% (1)
- IQX Controller & I/O ModulesDocument12 pagesIQX Controller & I/O ModulesAnonymous XYAPaxjbYNo ratings yet
- Group3 The Development of Moral Character of Moral Agent EspantoHipolitoLepitinNamoc 1Document5 pagesGroup3 The Development of Moral Character of Moral Agent EspantoHipolitoLepitinNamoc 1Novelyn DuyoganNo ratings yet
- Sample CISSP ResumeDocument4 pagesSample CISSP ResumeAskia MappNo ratings yet
- Cebex 305: Constructive SolutionsDocument4 pagesCebex 305: Constructive SolutionsBalasubramanian AnanthNo ratings yet
- Aeroacoustic Optimization of Wind Turbine Airfoils by Combining Thermographic and Acoustic Measurement DataDocument4 pagesAeroacoustic Optimization of Wind Turbine Airfoils by Combining Thermographic and Acoustic Measurement DatamoussaouiNo ratings yet
- 990XP Bandit ChipperDocument5 pages990XP Bandit ChipperFrancisco ConchaNo ratings yet
- Boot Time Memory ManagementDocument22 pagesBoot Time Memory Managementblack jamNo ratings yet
- Proceso Gmaw (RMD)Document8 pagesProceso Gmaw (RMD)Wilfredo RamirezNo ratings yet
- Understanding EarsDocument1 pageUnderstanding EarsmerkyworksNo ratings yet
- Teacher Survey - Outdoor Classroom Feedback: Please Circle All That ApplyDocument3 pagesTeacher Survey - Outdoor Classroom Feedback: Please Circle All That ApplyBrooke Doran RoeNo ratings yet
- Group 6G Revised Research Manuscript 1Document57 pagesGroup 6G Revised Research Manuscript 1Mc Rollyn VallespinNo ratings yet
- Can We Define Ecosystems - On The Confusion Between Definition and Description of Ecological ConceptsDocument15 pagesCan We Define Ecosystems - On The Confusion Between Definition and Description of Ecological ConceptsKionara SarabellaNo ratings yet
- Affidavit of Insurance ClaimsDocument2 pagesAffidavit of Insurance Claimsشزغتحزع ىطشفم لشجخبهNo ratings yet
- CCTV Proposal Quotation-1 Orine EdutechDocument5 pagesCCTV Proposal Quotation-1 Orine EdutechĄrpit Rāz100% (1)
- English The Smiles and Tears of RasoolullahDocument130 pagesEnglish The Smiles and Tears of RasoolullahwildqafNo ratings yet
- Advanced Calculus For Applications - Francis B Hilderand 1962Document657 pagesAdvanced Calculus For Applications - Francis B Hilderand 1962prabu201No ratings yet
- Papaer JournelDocument6 pagesPapaer JournelsonalisabirNo ratings yet
- Additional Clinical Case Study TemplatesDocument4 pagesAdditional Clinical Case Study TemplatesMikhaela Andree MarianoNo ratings yet
- SN Quick Reference 2018Document6 pagesSN Quick Reference 2018pinakin4uNo ratings yet
- Naaladiyar: Watch Free MoviesDocument6 pagesNaaladiyar: Watch Free MoviesVijayaLakshmi IyerNo ratings yet
- 02 - Consumerism Then and NowDocument28 pages02 - Consumerism Then and NowGeorge TsangNo ratings yet
- Table of Contents and Company Profile of JPCOM CARES STAC5Document4 pagesTable of Contents and Company Profile of JPCOM CARES STAC5Ch Ma100% (1)
- 2.HVT Terminacion InstrDocument18 pages2.HVT Terminacion Instrelectrica3No ratings yet
- CanagliflozinDocument7 pagesCanagliflozin13201940No ratings yet
- Sources of InnovationDocument22 pagesSources of Innovationm umair zahirNo ratings yet
- Fish SilageDocument4 pagesFish Silagesooriya_giri100% (1)