Professional Documents
Culture Documents
Cardiovascular Risk Factors in Childhood and Left Ventricular Diastolic Function in Adulthood
Cardiovascular Risk Factors in Childhood and Left Ventricular Diastolic Function in Adulthood
Uploaded by
Luis David Herrera MolinaresCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular Risk Factors in Childhood and Left Ventricular Diastolic Function in Adulthood
Cardiovascular Risk Factors in Childhood and Left Ventricular Diastolic Function in Adulthood
Uploaded by
Luis David Herrera MolinaresCopyright:
Available Formats
Cardiovascular Risk Factors in
Childhood and Left Ventricular
Diastolic Function in Adulthood
Jarkko S. Heiskanen, MD,a,b Saku Ruohonen, PhD,a,b,c Suvi P. Rovio, PhD,a,b Katja Pahkala, PhD,a,b Ville Kytö, MD, PhD,a,b,d
Mika Kähönen, MD, PhD,e Terho Lehtimäki, MD, PhD,f Jorma S.A. Viikari, MD, PhD,g Markus Juonala, MD, PhD,g
Tomi Laitinen, MD, PhD,h Päivi Tossavainen, MD, PhD,i Eero Jokinen, MD, PhD,j Nina Hutri-Kähönen, MD, PhD,k
Olli T. Raitakari, MD, PhDa,b,l
Cardiovascular risk factors, such as obesity, blood pressure, and
BACKGROUND AND OBJECTIVES: abstract
physical inactivity, have been identified as modifiable determinants of left ventricular (LV)
diastolic function in adulthood. However, the links between childhood cardiovascular risk
factor burden and adulthood LV diastolic function are unknown. To address this lack of
knowledge, we aimed to identify childhood risk factors associated with LV diastolic function in
the participants of the Cardiovascular Risk in Young Finns Study.
METHODS: Study participants (N = 1871; 45.9% men; aged 34–49 years) were examined
repeatedly between the years 1980 and 2011. We determined the cumulative risk exposure in
childhood (age 6–18 years) as the area under the curve for systolic blood pressure, adiposity
(defined by using skinfold and waist circumference measurements), physical activity, serum
insulin, triglycerides, total cholesterol, and high- and low-density lipoprotein cholesterols.
Adulthood LV diastolic function was defined by using E/é ratio.
RESULTS: Elevated systolic blood pressure and increased adiposity in childhood were associated
with worse adulthood LV diastolic function, whereas higher physical activity level in
childhood was associated with better adulthood LV diastolic function (P , .001 for all). The
associations of childhood adiposity and physical activity with adulthood LV diastolic function
remained significant (both P , .05) but were diluted when the analyses were adjusted for
adulthood systolic blood pressure, adiposity, and physical activity. The association between
childhood systolic blood pressure and adult LV diastolic function was diluted to nonsignificant
(P = .56).
Adiposity status and the level of physical activity in childhood are independently
CONCLUSIONS:
associated with LV diastolic function in adulthood.
a WHAT’S KNOWN ON THIS SUBJECT: In adults, decreased left ventricular (LV)
Research Centre of Applied and Preventive Cardiovascular Medicine, University of Turku, Turku, Finland; bCentre
diastolic function is associated with several known cardiovascular risk
for Population Health Research, University of Turku and Turku University Hospital, Turku, Finland; cOrion Pharma, factors such as overweight, hypertension, and physical inactivity. However,
Turku, Finland; dHeart Center, Turku University Hospital, Turku, Finland; eDepartment of Clinical Physiology, the link between childhood cardiovascular risk factor burden and
Tampere University Hospital and Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland; adulthood LV diastolic function is unknown.
f
Department of Clinical Chemistry, Fimlab Laboratories, and Finnish Cardiovascular Research Center - Tampere,
Faculty of Medicine and Health Technology, Tampere University, Tampere, Finland; gDepartment of Medicine, WHAT THIS STUDY ADDS: This study reveals that lower LV diastolic function
University of Turku and Division of Medicine, Turku University Hospital, Turku, Finland; hDepartment of Clinical in adulthood is associated with an increased burden of adiposity and
Physiology, University of Eastern Finland and Kuopio University Hospital, Kuopio, Finland; iDepartment of decreased physical activity in childhood, supporting the benefits of avoiding
Pediatrics, PEDEGO Research Unit and Medical Research Center Oulu, Oulu University Hospital and University of high adiposity and adopting a physically active lifestyle from childhood.
Oulu, Oulu, Finland; jDepartment of Paediatric Cardiology, Hospital for Children and Adolescents, University of
Helsinki, Helsinki, Finland; kDepartment of Paediatrics, Tampere University Hospital and Faculty of Medicine and To cite: Heiskanen JS, Ruohonen S, Rovio SP, et al.
Health Technology, Tampere University, Tampere, Finland; and lDepartment of Clinical Physiology and Nuclear Cardiovascular Risk Factors in Childhood and Left
Medicine, Turku University Hospital, Turku, Finland
Ventricular Diastolic Function in Adulthood. Pediatrics.
2021;147(3):e2020016691
Downloaded from www.aappublications.org/news by guest on September 15, 2021
PEDIATRICS Volume 147, number 3, March 2021:e2020016691 ARTICLE
The prevalence of overweight and risk factor burden and adulthood LV and study protocol has been reported
low levels of physical activity are diastolic function are unknown. To earlier.11 The study protocol has been
rising across Western countries, with address this lack of knowledge, we approved by the ethics committee of
an increased need for active aimed to identify childhood risk the University of Turku and Turku
prevention.1,2 Cardiovascular risk factors associated with LV diastolic University Central Hospital, and
burden accumulated across the function in the 34- to 49-year-old informed consent was obtained from
lifetime contributes to cardiovascular participants of the Cardiovascular all participants. All authors had full
disease outcomes that are the leading Risk in Young Finns Study (YFS). The access to the data.
causes of death globally.3 The longitudinal study design with
decrease in left ventricular (LV) repeated risk factor measurements Echocardiographic Measurements
diastolic function is an early beginning from childhood allows us
Echocardiography was performed in
functional alteration of the heart. We the unique assessment of cumulative
2011 for 1994 participants according
have previously shown that higher risk factor burden from childhood.
to the joint American and European
waist circumference, systolic blood
guidelines.9,12 After excluding the
pressure, and smoking are associated
participants with severe
with lower LV diastolic function in METHODS cardiovascular diseases (including
adults.4 Adverse effects of childhood
Study Population stroke, myocardial infarction, atrial
obesity on adulthood LV mass has
fibrillation, unstable angina pectoris,
been previously shown in the The YFS is an ongoing multicenter,
cardiomyopathies, and regurgitation
Bogalusa Heart Study.5 Additionally, longitudinal, population-based study
or stenosis of the mitral or aortic
obese children have been reported to on cardiovascular risk factors from
valve), type 1 diabetes, or missing
have worse LV diastolic function childhood to adulthood, representing
echocardiographic measurements, the
compared with normal-weight the general Finnish population. The
study population of the current study
children.6 Conversely, achieving ideal baseline study was conducted in
consisted of 1871 participants (859
cardiovascular health, defined by the 1980 and included 3596 children and
men and 1012 women; mean age
American Heart Association, in adolescents (49.0% males aged 3, 6,
41.8 6 5.0 years).
childhood has been associated with 9, 12, 15, and 18 years). Extensive
better LV diastolic function in data on cardiovascular risk factors Trained ultrasound technicians
adulthood.7 were recorded at the baseline in performed the echocardiographic
1980, and all follow-up studies were examinations at 5 YFS study centers.
Heart failure with preserved ejection conducted in 1983, 1986, 1989, 2001, All ultrasound technicians were
fraction is a clinical syndrome 2007, and 2011.11 Population trained by a cardiac imaging
characterized by symptoms of heart characteristics from the year 2011 specialist. Transthoracic
failure without a decrease of LV are presented in Table 1. Detailed echocardiography was performed
systolic function.8 Instead, LV information on the YFS population with Acuson Sequoia 512 (Mountain
diastolic function is decreased,
including slow LV filling and TABLE 1 Population Characteristics (the Follow-up Year 2011)
increased diastolic LV stiffness.9 Women (n = 1012) Men (n = 859)
Currently, there is no evidence-based
Meana SD Meana SD
medicine that improves the prognosis
of the condition. Moreover, LV E/é ratio 5.0 1.0 4.6 0.9
Age, y 41.9 5.0 41.7 5.0
diastolic function is already
Systolic blood pressure, mm Hg 115.3 13.6 122.9 13.4
considerably decreased when the Height, cm 166.1 6.0 179.8 6.6
symptoms of heart failure appear. Waist circumference, cm 87.0 13.5 96.4 12.0
Therefore, it is important to Weight, kg 71.4 14.8 86.9 15.2
understand the role of risk burden BMI 25.9 5.2 26.8 4.2
Serum total cholesterol, mmol/L 5.1 0.9 5.3 1.0
acquired during the life course to be
Triglycerides, mmol/L 1.1 1.2 1.6 1.1
able to provide effective prevention. HDL-C, mmol/L 1.4 0.3 1.2 0.3
In adult populations, overweight, LDL-C, mmol/L 3.1 0.8 3.4 0.9
insulin resistance, and elevated Insulin, mU/I 8.8 10.8 10.1 9.6
systolic blood pressure are well- Physical activity (index score 5–15) 9.2 1.9 8.9 1.9
Overweight, % 30.5 — 44.4 —
known modifiable risk factors for
Obese, % 18.8 — 19.9 —
heart failure with preserved ejection Overweight or obese, % 49.3 — 64.3 —
fraction.10 However, the links Overweight defined as BMI between 25 and 30; obese defined as BMI $30. —, not applicable.
between childhood cardiovascular a Parameters with "%" indicate percentage rather than mean.
Downloaded from www.aappublications.org/news by guest on September 15, 2021
2 HEISKANEN et al
View, CA) ultrasonography by using skinfold measurements in triplicate adulthood LV diastolic function in the
a 3.5-MHz scanning frequency from the nondominant arm by using previous model (ie, adiposity, physical
phased-array transducer. Analysis of a Harpenden skinfold caliper.20 Using activity, and systolic blood pressure)
the echo images was done by one these adiposity measures, an area were entered into the same statistical
observer blinded to the clinical under the curve (AUC) variable was model (childhood model). Third,
details with the CommPACS 10.7.8 created for childhood adiposity a multivariable linear model
(MediMatic Solutions, Genova, Italy) (standardized mean = 100; SD = 15). (combined model) was created
analysis program.13 In the adulthood follow-up studies in adjusting the childhood model
2001, 2007, and 2011, waist additionally for corresponding
E/é ratio is a noninvasive circumference (centimeters) was adulthood parameters (ie, adulthood
measurement representing LV filling used to indicate adiposity. Data on adiposity, physical activity, and
pressure in early diastole.9 Pulsed- leisure-time physical activity were systolic blood pressure).
wave Doppler imaging was used to collected by using a validated self-
measure E. Pulsed-wave tissue To study the associations of
report questionnaire from
Doppler imaging was used to childhood cardiovascular risk factor
participants aged 9 to 18 years
measure é; E wave describes the clustering on adulthood LV diastolic
(Supplemental Information).21 The
mitral blood flow during the early questionnaire was administered in
function, we calculated a childhood
filling of the LV, and é measures connection with the medical
risk score using those childhood risk
mitral annular early diastolic velocity. factors that associated significantly
examination. For participants aged
In this study, E/é ratio (mean 4.8; with LV diastolic function in the
6 years, physical activity was
range 2.2–9.0) was calculated by multivariable models. The factors
collected by using parents’ ratings
using the average of lateral and septal included in the score were (1)
(Supplemental Information).21
values of é velocity.9 High E/é ratio childhood adiposity, (2) physical
reflects low LV diastolic function and To describe the long-term burden of activity, and (3) systolic blood
has been associated with all-cause the risk factors, we estimated pressure. First, for all 3 risk factors,
mortality in several disease participant-specific curves for age the participants were categorized into
states.14,15 The complete window between 6 and 18 years, those having the risk factor (1 point)
methodology of the cardiac imaging systolic blood pressure, adiposity, and those without the risk factor (0
and the off-line analysis of the cardiac physical activity, insulin, triglycerides, points). Having a risk factor was
measurements in the YFS have been total cholesterol, HDL-C, and LDL-C defined as having the AUC value
published earlier.13 by mixed-model regression splines.22 within the highest quartile for
For more detailed information on the adiposity and systolic blood pressure
Clinical Measurements and methodology, please see the and in the lowest quartile for physical
Questionnaires Supplemental Information. activity. The risk score was then
calculated by summing all 3 risk
Standard methods were used to
Statistical Analysis factors (range 0–3), resulting in 4
measure blood pressure, fasting
groups: 0 risk factors (n = 870), 1 risk
serum glucose, total cholesterol, and The distributions of the study
factor (n = 652), 2 risk factors (n =
high-density lipoprotein cholesterol variables were confirmed by visual
296), and 3 risk factors (n = 53).
(HDL-C) concentrations throughout evaluation and the Kolmogorov-
Finally, the mean E/é ratio was
the study.16 Low-density lipoprotein Smirnov test. Unmodifiable
calculated for each group by using
cholesterol (LDL-C) was calculated parameters with a strong association
least-squares means (The R Package
according to Friedewald et al.17 In with LV diastolic function, namely,
lsmeans)23 adjusting the analyses
1980, 1983, and 1986, serum insulin age, sex, and adulthood height,4 as
according to the combined model.
was measured with a modification of well as the study site, were used as
the immunoassay method of Herbert covariates in all statistical models. We used all available data in the
et al.18 The concentration of serum First, multivariable linear models analyses; therefore, the number of
insulin was determined with an were conducted separately for each participants varies between the
immunoassay in years 2001, 2007, childhood cardiovascular risk factor. models. Variance inflation factors
and 2011.19 At all follow-ups, the Variables were standardized (mean were used to detect multicollinearity
participants’ weight (kilograms) and 0 and SD 1) to ensure the in multivariable models (no
height (centimeters) were measured. comparability of the point estimates significant multicollinearities were
In the follow-up studies conducted in among the studied risk factors and to found). P values #.05 were
1980, 1983, and 1986, childhood visualize the results as a forest plot. considered statistically significant in
adiposity was measured by using Second, all childhood variables all analyses. Data were analyzed by
subscapular, biceps, and triceps revealing significant associations with using the R statistical package,
Downloaded from www.aappublications.org/news by guest on September 15, 2021
PEDIATRICS Volume 147, number 3, March 2021 3
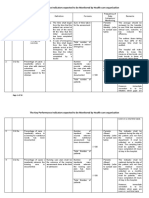
version 3.3.2. (R Foundation for TABLE 2 Associations Between LV Diastolic Function (E/é Ratio) and Childhood Risk Factors
Statistical Computing, Vienna, Childhood Model Combined Model
Austria) (http://www.R-project.org/). Estimate SE P Estimate SE P
Female sex 0.084 0.066 .202 20.217 0.072 .003
Age, y 0.093 0.022 ,.001 0.084 0.023 ,.001
RESULTS Height in adulthood, cm 20.140 0.031 ,.001 20.137 0.032 ,.001
Cumulative systolic blood pressure in childhood 0.100 0.022 ,.001 0.015 0.025 .557
Childhood Risk Factors and Cumulative physical activity in childhood 20.061 0.023 .007 20.053 0.024 .029
Adulthood LV Diastolic Function Cumulative adiposity in childhood 0.091 0.025 ,.001 0.075 0.028 .007
Systolic blood pressure in adulthood, mm Hg — — — 0.180 0.025 ,.001
The high cumulative burden of Physical activity in adulthood (index score 5–15) — — — 0.018 0.022 .410
childhood adiposity and systolic Adiposity in adulthood, cm — — — 0.039 0.028 .166
blood pressure were associated with Both models were additionally adjusted for study center. Childhood cumulative parameters were calculated as AUC
worse adulthood LV diastolic variables from estimated participant-specific curves (age window 6–18 y). Explanatory variables were standardized
function. The high cumulative (mean 0 and SD 1). —, not applicable.
childhood physical activity exposure
was associated with a better serum insulin, triglycerides, total including systolic blood pressure,
adulthood LV diastolic function cholesterol, HDL-C, or LDL-C with physical activity, and adiposity
(Fig 1). The results remained similar adult LV diastolic function (Fig 1). measurements from both childhood
when all 3 childhood risk factors and adulthood (Table 2, combined
were entered simultaneously in To study whether the associations of model). Childhood adiposity was
a multivariable linear model (Table 2, childhood risk factors remained found to have an association with
childhood model). No significant significant after controlling for the worse adulthood LV diastolic function
associations were found for the counterpart adulthood risk factors, independent of adulthood adiposity.
cumulative childhood burden of we conducted a multivariable model The adjustment with the counterpart
E/é Ratio
Systolic blood pressure
Adiposity
Physical activity
Insulin
Triglycerides
Total cholesterol
HDL-C
LDL-C
–0.2 –0.1 0.0 0.1 0.2 Estimate (95% CI)
FIGURE 1
Standardized b-estimates for the associations between each separate childhood (age 6–18 years) cumulative cardiovascular risk factor and adulthood E/
é ratio. Linear regression analyses were conducted separately for each cardiovascular risk factor adjusting for age, sex, study center (in the year 2011),
and adulthood height. Standardized cardiovascular risk factor variables (mean 0 and SD 1) are shown. Error bars denote 95% confidence intervals (CIs).
Downloaded from www.aappublications.org/news by guest on September 15, 2021
4 HEISKANEN et al
adulthood risk factors diluted the function (P = .007). Compared with metabolism.24 Moreover, both
effect estimate by ∼18%. Childhood the participants with no childhood childhood and adulthood obesity are
physical activity had an association risk factors, the participants with 2 or associated with myocardium
with better adulthood LV diastolic 3 childhood risk factors had a higher remodeling and alteration of LV
function independent of adulthood E/é ratio denoting worse LV diastolic systolic and diastolic function.25,26
physical activity. After further function (P = .047 and P = .0066, This deterioration in LV diastolic
adjustment with the counterpart respectively). function has been suggested to affect
adulthood risk factors, the effect the elastic properties of the
Finally, all multivariable models were
estimate of childhood physical myocardium through multifactorial
further adjusted for left atrial and
activity was diluted by ∼13%. The mechanisms.25,27,28 Our present
ventricular volume, ejection fraction,
association of childhood systolic results indicate that increased
and LV mass in separate models. The
blood pressure with adulthood LV childhood adiposity has an inverse
results of these analyses were similar
diastolic function was no longer association with LV diastolic function
to those of the main analyses
significant when the adulthood risk in adulthood and that this link
reported in Table 2 and Fig 2 (data
factors were taken into account (the remains significant after controlling
not shown), suggesting that the
effect estimate was diluted by 85%). for adulthood risk factor profile. This
results are not driven by changes in
suggests that excess childhood
Clustering of the Childhood Risk LV volume, LV mass, or LV systolic
adiposity may have long-term
Factors function.
adverse influences on LV diastolic
The results from the analyses for the Sensitivity Analyses function. Importantly, although
childhood risk factor score, indicating childhood adiposity was associated
the number of childhood risk factors, Sensitivity analyses were conducted independently with adulthood LV
are shown in Fig 2. A significant trend by using (1) arithmetic means instead diastolic function, the
was found between a higher number of least-squares means or (2) cutoff cardiometabolic markers closely
of childhood cardiovascular risk limits of 80th/20th for the risk linked to adiposity, including
factors and worse LV diastolic factors to calculate the childhood childhood insulin, triglycerides, total
cardiovascular risk score indicating cholesterol, HDL-C, and LDL-C, were
the childhood risk factor not. Therefore, our results suggest
6.0 accumulation. The results from the that the association between
sensitivity analyses were similar to childhood adiposity and adulthood LV
the main analyses (data not shown). diastolic function is not driven by
5.0
these cardiometabolic markers.
DISCUSSION
4.0 Previous studies have revealed that
This study reveals that the cumulative physical activity has numerous
E/é Ratio
burden of adiposity, physical activity, beneficial effects on cardiovascular
3.0 and systolic blood pressure in health.29,30 Physically active
childhood is associated with LV individuals have fewer cardiovascular
diastolic function at ages 34 to 49. comorbidities, including diabetes
2.0 Importantly, the associations of mellitus, hypertension, and
childhood adiposity and physical dyslipidemia, than those with low
1.0
activity with adulthood LV diastolic physical activity levels.31 Previous
function were independent of the studies have revealed that lower
adulthood levels of the same risk cardiorespiratory fitness is a risk
.47a .047a .0066a
0.0
0 1 2 3
factor. This is the first study to factor for worse LV diastolic function
Number of the Risk Factors indicate that the cumulative and heart failure with preserved
cardiovascular risk factor exposure ejection fraction and may contribute
FIGURE 2
Association between childhood cardiovascular already in childhood may to the prognosis of the disease.32–35
risk score and adjusted means for adulthood independently contribute to diastolic Furthermore, worse
E/é ratio. The analyses were adjusted for age, LV function in adulthood.
sex, research center, adulthood height, systolic cardiorespiratory fitness in young
blood pressure, physical activity, and waist Childhood obesity is known to adulthood was found to associate
circumference. Study participants were divided associate with adverse changes in with higher LV diastolic filling
into 4 groups on the basis of the sum of the pressures independent of
risk factors in childhood (n): 0 = 870, 1 = 652, 2
cardiovascular risk factors, such as
= 296, and 3 = 53. a P values compared with the serum lipoproteins, systolic and cardiovascular risk factor burden in
group with 0 risk factors. diastolic blood pressure, and glucose a middle-aged population.36 Our
Downloaded from www.aappublications.org/news by guest on September 15, 2021
PEDIATRICS Volume 147, number 3, March 2021 5
findings, revealing that the childhood childhood risk factor clustering on worse LV diastolic dysfunction in the
cumulative physical activity is cardiovascular health and by follow-up examination. Our study
associated with better adulthood LV highlighting the role of lifestyle- population with no significant cardiac
diastolic function, extend these related childhood risk factors, the diseases strengthens the significance
previous observations by findings from our study underline the of these results because the
demonstrating that the beneficial need for guideline-recommended possibility for bias caused by cardiac
effects of childhood physical activity active prevention strategies targeted diseases is low.
may carry on to adulthood. to the individuals with several
Hypertension is considered a key risk cardiovascular risk factors beginning CONCLUSIONS
factor for LV diastolic dysfunction in from childhood.39
This study reveals that lower levels of
adults, deterring it through several The major strengths of this study adiposity and higher levels of physical
potential mechanistic pathways, include the longitudinal study design activity in childhood are beneficially
including pressure overload causing and the long follow-up of participants associated with LV diastolic function
LV hypertrophy and alterations in the who were well phenotyped in both in adulthood. Importantly, the
neurohumoral activity and childhood and adulthood. A potential clustering of cardiovascular risk
inflammation.14,37 In contrast, limitation of the study is a possible factors in childhood is associated
childhood systolic blood pressure has selection of the study population. As with worse LV diastolic function in
not been previously linked with in every longitudinal study, there is adulthood. These findings provide
adulthood LV diastolic function. In a loss in the follow-up. However, novel evidence on the childhood risk
our study, a higher cumulative burden detailed assessments of the factors of adulthood LV diastolic
of systolic pressure in childhood was representativeness have previously function, supporting the benefits of
associated with worse LV diastolic revealed no significant differences avoiding high adiposity and adopting
function in adulthood. However, the between the participants and a physically active lifestyle already
association diluted when adulthood nonparticipants in the age- and sex- from childhood.
systolic blood pressure was taken adjusted analyses.11,16 The YFS
into account, suggesting that population is racially homogeneous,
adulthood systolic blood pressure ACKNOWLEDGMENTS
therefore our results are
level is a more powerful determinant Expert technical assistance in data
generalizable to white European
for the adulthood LV diastolic management and statistical analyses
subjects. E/é ratio is a generally used
function compared to childhood by Johanna Ikonen, Noora Kartiosuo,
marker for LV diastolic function, but
systolic blood pressure. and Irina Lisinen is gratefully
it is not a consistent indicator of LV
acknowledged.
Cardiovascular risk factors tend to filling pressures in individual patients
cluster already in childhood, and the in specific clinical situations.15
clustering of risk factors is thought to However, at a population level, E/é
be a useful measure of cardiovascular ratio has been shown to associate ABBREVIATIONS
health in children.38 Our present with an increased incidence of heart AUC: area under the curve
study extends current knowledge by failure and has been used in multiple HDL-C: high-density lipoprotein
revealing that the cardiovascular risk studies to predict all-cause mortality, cholesterol
factor clustering (ie, an increasing cardiovascular death, and heart LDL-C: low-density lipoprotein
number of risk factors) already in failure hospitalizations in several cholesterol
childhood associates with lower LV diseases states.14,40 Additionally, in LV: left ventricular
diastolic function in adulthood. a population-based follow-up study YFS: Cardiovascular Risk in Young
Noteworthy, by broadening the by Kane et al,41 baseline E/é ratio was Finns Study
outlook to the long-term effects of found to be a predictive factor for
Deidentified individual participant data will not be made available.
Dr Heiskanen contributed to the conception and design of the work, contributed to acquisition, analysis, and interpretation of the data, and drafted the manuscript;
Drs Ruohonen and Raitakari contributed to the conception and design of the work, contributed to acquisition, analysis, and interpretation of the data, and critically
revised the manuscript; Drs Rovio, Pahkala, Kytö, Kähönen, Lehtimäki, Viikari, Juonala, Laitinen, Tossavainen, Jokinen, and Hutri-Kähönen contributed to the
acquisition, analysis, and interpretation of data for the work and critically revised the manuscript; and all authors approved the final manuscript as submitted and
agree to be accountable for all aspects of the work.
The preliminary results of this article were presented in a poster session of the American Heart Association Scientific Sessions; November 10–12, 2018; Chicago, IL.
Downloaded from www.aappublications.org/news by guest on September 15, 2021
6 HEISKANEN et al
DOI: https://doi.org/10.1542/peds.2020-016691
Accepted for publication Dec 4, 2020
Address correspondence to Jarkko S. Heiskanen, MD, Research Centre of Applied and Preventive Cardiovascular Medicine and Centre for Population Health
Research, University of Turku and Turku University Hospital, Kiinamyllynkatu 10, 20520, Turku, Finland. E-mail: jsheis@utu.fi
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2021 by the American Academy of Pediatrics
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: The Young Finns Study has been financially supported by the Academy of Finland: grants 322098, 286284, 134309 (Eye), 126925, 121584, 124282, 129378
(Salve), 117787 (Gendi), and 41071 (Skidi); the Social Insurance Institution of Finland; Competitive State Research Financing of the Expert Responsibility Area of
Kuopio, Tampere and Turku University Hospitals (grant X51001); Juho Vainio Foundation; Paavo Nurmi Foundation; Finnish Foundation for Cardiovascular Research;
Finnish Cultural Foundation; The Sigrid Jusélius Foundation; Tampere Tuberculosis Foundation; Emil Aaltonen Foundation; Yrjö Jahnsson Foundation; Signe and Ane
Gyllenberg Foundation; Diabetes Research Foundation of Finnish Diabetes Association; European Union Horizon 2020 (grant 755320 for TAXINOMISIS); European
Research Council (grant 742927 for MULTIEPIGEN project); Tampere University Hospital Supporting Foundation; and Aarne Koskelo Foundation and Diabetes
Research Foundation of Finnish Diabetes Association. The funders of this study had no role in the design and conduct of the study.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2020-025908.
REFERENCES
1. Abarca-Gómez L, Abdeen ZA, Hamid ZA, 6. Sharpe JA, Naylor LH, Jones TW, et al. 11. Raitakari OT, Juonala M, Rönnemaa T,
et al.; NCD Risk Factor Collaboration Impact of obesity on diastolic function et al. Cohort profile: the cardiovascular
(NCD-RisC). Worldwide trends in body- in subjects , or = 16 years of age. Am risk in Young Finns Study. Int
mass index, underweight, overweight, J Cardiol. 2006;98(5):691–693 J Epidemiol. 2008;37(6):1220–1226
and obesity from 1975 to 2016:
7. Laitinen TT, Ruohonen S, Juonala M, 12. Lang RM, Badano LP, Mor-Avi V, et al.
a pooled analysis of 2416 population-
et al. Ideal cardiovascular health in Recommendations for cardiac chamber
based measurement studies in 128×9
childhood-longitudinal associations quantification by echocardiography in
million children, adolescents, and
with cardiac structure and function: the adults: an update from the American
adults. Lancet. 2017;390(10113):
Special Turku Coronary Risk Factor Society of Echocardiography and the
2627–2642
Intervention Project (STRIP) and the European Association of Cardiovascular
2. Guthold R, Stevens GA, Riley LM, Bull FC. Cardiovascular Risk in Young Finns Imaging. Eur Heart J Cardiovasc
Worldwide trends in insufficient Study (YFS). Int J Cardiol. 2017;230: Imaging. 2015;16(3):233–270
physical activity from 2001 to 2016: 304–309 13. Ruohonen S, Koskenvuo JW, Wendelin-
a pooled analysis of 358 population-
8. Borlaug BA, Paulus WJ. Heart failure Saarenhovi M, et al. Reference values
based surveys with 1×9 million
with preserved ejection fraction: for echocardiography in middle-aged
participants. Lancet Glob Health. 2018; population: the Cardiovascular Risk in
6(10):e1077–e1086 pathophysiology, diagnosis, and
treatment. Eur Heart J. 2011;32(6): Young Finns Study. Echocardiography.
3. World Health Organization. WHO 670–679 2016;33(2):193–206
Methods and Data Sources for Country- 14. Redfield MM, Jacobsen SJ, Burnett JC
Level Causes of Death 2000–2015. 9. Nagueh SF, Smiseth OA, Appleton CP,
et al.; Houston, Texas; Oslo, Norway; Jr., Mahoney DW, Bailey KR, Rodeheffer
Geneva, Switzerland: Department of RJ. Burden of systolic and diastolic
Information, Evidence and Research, Phoenix, Arizona; Nashville, Tennessee;
Hamilton, Ontario, Canada; Uppsala, ventricular dysfunction in the
World Health Organization; 2017 community: appreciating the scope of
Sweden; Ghent and Liège, Belgium;
4. Heiskanen JS, Ruohonen S, Rovio SP, Cleveland, Ohio; Novara, Italy; Rochester, the heart failure epidemic. JAMA. 2003;
et al. Determinants of left ventricular Minnesota; Bucharest, Romania; and St. 289(2):194–202
diastolic function-the Cardiovascular Louis, Missouri. Recommendations for 15. Mitter SS, Shah SJ, Thomas JD. A test in
Risk in Young Finns Study. the evaluation of left ventricular context: E/A and E/e9 to assess diastolic
Echocardiography. 2019;36(5):854–861 diastolic function by echocardiography: dysfunction and LV filling pressure.
an update from the American Society of J Am Coll Cardiol. 2017;69(11):
5. Lai CC, Sun D, Cen R, et al. Impact of
Echocardiography and the European 1451–1464
long-term burden of excessive adiposity
Association of Cardiovascular Imaging.
and elevated blood pressure from 16. Juonala M, Viikari JSA, Raitakari OT.
Eur Heart J Cardiovasc Imaging. 2016;
childhood on adulthood left ventricular Main findings from the prospective
17(12):1321–1360
remodeling patterns: the Bogalusa Cardiovascular Risk in Young Finns
Heart Study. J Am Coll Cardiol. 2014; 10. Braunwald E. Heart failure. JACC Heart Study. Curr Opin Lipidol. 2013;24(1):
64(15):1580–1587 Fail. 2013;1(1):1–20 57–64
Downloaded from www.aappublications.org/news by guest on September 15, 2021
PEDIATRICS Volume 147, number 3, March 2021 7
17. Friedewald WT, Levy RI, Fredrickson DS. 26. Tadic M, Cuspidi C. Childhood obesity Aldosterone Antagonist). Circulation.
Estimation of the concentration of low- and cardiac remodeling: from cardiac 2017;136(11):982–992
density lipoprotein cholesterol in structure to myocardial mechanics.
34. Brinker SK, Pandey A, Ayers CR, et al.
plasma, without use of the preparative J Cardiovasc Med (Hagerstown). 2015;
Association of cardiorespiratory fitness
ultracentrifuge. Clin Chem. 1972;18(6): 16(8):538–546
with left ventricular remodeling and
499–502
27. Spinale FG. Myocardial matrix diastolic function: the Cooper Center
18. Herbert V, Lau K-S, Gottlieb CW, Bleicher remodeling and the matrix Longitudinal Study. JACC Heart Fail.
SJ. Coated charcoal immunoassay of metalloproteinases: influence on 2014;2(3):238–246
insulin. J Clin Endocrinol Metab. 1965; cardiac form and function. Physiol Rev.
25(10):1375–1384 35. Pandey A, LaMonte M, Klein L, et al.
2007;87(4):1285–1342
Relationship between physical activity,
19. Suomela E, Oikonen M, Virtanen J, et al. 28. Borlaug BA, Kass DA. Ventricular- body mass index, and risk of heart
Prevalence and determinants of fatty vascular interaction in heart failure. failure. J Am Coll Cardiol. 2017;69(9):
liver in normal-weight and overweight Heart Fail Clin. 2008;4(1):23–36 1129–1142
young adults. The Cardiovascular Risk
in Young Finns Study. Ann Med. 2015; 29. Fletcher FG, Landolfo C, Niebauer J, 36. Pandey A, Allen NB, Ayers C, et al.
47(1):40–46 Ozemek C, Arena R, Lavie CJ. Promoting Fitness in young adulthood and long-
physical activity and exercise: JACC term cardiac structure and function:
20. Dahlström S, Viikari J, Akerblom HK, the CARDIA study. JACC Heart Fail. 2017;
Health Promotion Series. J Am Coll
et al. Atherosclerosis precursors in 5(5):347–355
Cardiol. 2018;72(14):1622–1639
Finnish children and adolescents. II.
Height, weight, body mass index, and 30. Piepoli MF, Hoes AW, Agewall S, et al. 37. Nadruz W, Shah AM, Solomon SD.
skinfolds, and their correlation to 2016 European guidelines on Diastolic dysfunction and hypertension.
metabolic variables. Acta Paediatr cardiovascular disease prevention in Med Clin North Am. 2017;101(1):
Scand Suppl. 1985;318:65–78 clinical practice: developed with the 7–17
21. Telama R, Yang X, Leskinen E, et al. special contribution of the European 38. Andersen LB, Wedderkopp N, Hansen
Tracking of physical activity from early Association for Cardiovascular HS, Cooper AR, Froberg K. Biological
childhood through youth into Prevention & Rehabilitation (EACPR). cardiovascular risk factors cluster in
adulthood. Med Sci Sports Exerc. 2014; Eur J Prev Cardiol. 2016;23(11):NP1- Danish children and adolescents: the
46(5):955–962 NP96 European Youth Heart Study. Prev Med.
22. Welham SJ, Cullis BR, Kenward MG, 31. Lee IM, Shiroma EJ, Lobelo F, Puska P, 2003;37(4):363–367
Thompson R. The analysis of Blair SN, Katzmarzyk PT; Lancet Physical 39. Barlow SE; Expert Committee. Expert
longitudinal data using mixed model Activity Series Working Group. Effect of Committee recommendations
L-splines. Biometrics. 2006;62(2): physical inactivity on major non- regarding the prevention, assessment,
392–401 communicable diseases worldwide: an and treatment of child and adolescent
23. Lenth RV. Least-squares means: the R analysis of burden of disease and life overweight and obesity: summary
package lsmeans. J Stat Softw. 2016; expectancy. Lancet. 2012;380(9838): report. Pediatrics. 2007;120(suppl 4):
69(1):1–33 219–229 S164–S192
24. Skinner AC, Perrin EM, Moss LA, Skelton 32. Pandey A, Patel KV, Vaduganathan M, 40. Halley CM, Houghtaling PL, Khalil MK,
JA. Cardiometabolic risks and severity et al. Physical activity, fitness, and Thomas JD, Jaber WA. Mortality rate in
of obesity in children and young adults. obesity in heart failure with preserved patients with diastolic dysfunction and
N Engl J Med. 2015;373(14):1307–1317 ejection fraction. JACC Heart Fail. 2018; normal systolic function. Arch Intern
6(12):975–982 Med. 2011;171(12):1082–1087
25. Lavie CJ, Laddu D, Arena R, Ortega FB,
Alpert MA, Kushner RF. Healthy weight 33. Hegde SM, Claggett B, Shah AM, et al. 41. Kane GC, Karon BL, Mahoney DW, et al.
and obesity prevention: JACC health Physical activity and prognosis in the Progression of left ventricular diastolic
promotion series. J Am Coll Cardiol. TOPCAT trial (Treatment of Preserved dysfunction and risk of heart failure.
2018;72(13):1506–1531 Cardiac Function Heart Failure With an JAMA. 2011;306(8):856–863
Downloaded from www.aappublications.org/news by guest on September 15, 2021
8 HEISKANEN et al
Cardiovascular Risk Factors in Childhood and Left Ventricular Diastolic
Function in Adulthood
Jarkko S. Heiskanen, Saku Ruohonen, Suvi P. Rovio, Katja Pahkala, Ville Kytö, Mika
Kähönen, Terho Lehtimäki, Jorma S.A. Viikari, Markus Juonala, Tomi Laitinen, Päivi
Tossavainen, Eero Jokinen, Nina Hutri-Kähönen and Olli T. Raitakari
Pediatrics 2021;147;
DOI: 10.1542/peds.2020-016691 originally published online February 8, 2021;
Updated Information & including high resolution figures, can be found at:
Services http://pediatrics.aappublications.org/content/147/3/e2020016691
References This article cites 40 articles, 12 of which you can access for free at:
http://pediatrics.aappublications.org/content/147/3/e2020016691#BI
BL
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Epidemiology
http://www.aappublications.org/cgi/collection/epidemiology_sub
Preventive Medicine
http://www.aappublications.org/cgi/collection/preventative_medicine
_sub
Cardiology
http://www.aappublications.org/cgi/collection/cardiology_sub
Permissions & Licensing Information about reproducing this article in parts (figures, tables) or
in its entirety can be found online at:
http://www.aappublications.org/site/misc/Permissions.xhtml
Reprints Information about ordering reprints can be found online:
http://www.aappublications.org/site/misc/reprints.xhtml
Downloaded from www.aappublications.org/news by guest on September 15, 2021
Cardiovascular Risk Factors in Childhood and Left Ventricular Diastolic
Function in Adulthood
Jarkko S. Heiskanen, Saku Ruohonen, Suvi P. Rovio, Katja Pahkala, Ville Kytö, Mika
Kähönen, Terho Lehtimäki, Jorma S.A. Viikari, Markus Juonala, Tomi Laitinen, Päivi
Tossavainen, Eero Jokinen, Nina Hutri-Kähönen and Olli T. Raitakari
Pediatrics 2021;147;
DOI: 10.1542/peds.2020-016691 originally published online February 8, 2021;
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://pediatrics.aappublications.org/content/147/3/e2020016691
Data Supplement at:
http://pediatrics.aappublications.org/content/suppl/2021/02/05/peds.2020-016691.DCSupplemental
Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
has been published continuously since 1948. Pediatrics is owned, published, and trademarked by
the American Academy of Pediatrics, 345 Park Avenue, Itasca, Illinois, 60143. Copyright © 2021
by the American Academy of Pediatrics. All rights reserved. Print ISSN: 1073-0397.
Downloaded from www.aappublications.org/news by guest on September 15, 2021
You might also like
- Cardiovascular Risk Factors in Childhood and Carotid Artery Intima-Media Thickness in AdulthoodDocument7 pagesCardiovascular Risk Factors in Childhood and Carotid Artery Intima-Media Thickness in AdulthoodDharmanna RathodNo ratings yet
- Effects of Gestational and Pregestational Diabetes Mellitus On The Foetal Heart: A Cross-Sectional StudyDocument6 pagesEffects of Gestational and Pregestational Diabetes Mellitus On The Foetal Heart: A Cross-Sectional StudyGabyliz Gonzalez CastilloNo ratings yet
- Daniels - 2009 - Complications of Obesity in Children and AdolescenDocument6 pagesDaniels - 2009 - Complications of Obesity in Children and AdolescenrootNo ratings yet
- A1111111111 A1111111111 A1111111111 A1111111111 A1111111111: BackgroundDocument11 pagesA1111111111 A1111111111 A1111111111 A1111111111 A1111111111: BackgroundSidonia CatalinaNo ratings yet
- Impact of Low Birth Weight and Cardiovascular Risk Factors On Endothelial Function in Early Adult LifeDocument5 pagesImpact of Low Birth Weight and Cardiovascular Risk Factors On Endothelial Function in Early Adult LifeChris BoviaNo ratings yet
- 1993 - BARKER Et Al - Fetal Nutrition and Cardiovascular Disease in Adult LifeDocument4 pages1993 - BARKER Et Al - Fetal Nutrition and Cardiovascular Disease in Adult LifeSamanta MonteiroNo ratings yet
- FentonDocument6 pagesFentonjessicaesmrldaNo ratings yet
- Godfrey2000 Godfrey, K. M., & Barker, D. J. (2000) - Fetal Nutrition and Adult Disease.Document9 pagesGodfrey2000 Godfrey, K. M., & Barker, D. J. (2000) - Fetal Nutrition and Adult Disease.Nancy Aidée Reyes MéndezNo ratings yet
- Unique Features of Infective Endocarditis in Childhood: AHA Scientific StatementDocument13 pagesUnique Features of Infective Endocarditis in Childhood: AHA Scientific StatementAbdi KebedeNo ratings yet
- Unique Features of Infective Endocarditis in Childhood: AHA Scientific StatementDocument13 pagesUnique Features of Infective Endocarditis in Childhood: AHA Scientific Statementmirashabrina12No ratings yet
- 4 - Health Consequences of Obesity 2012Document5 pages4 - Health Consequences of Obesity 2012Mateus CarvalhoNo ratings yet
- Art InglesDocument8 pagesArt InglesJose C Alvarez PerezNo ratings yet
- Laas 2012 (Inglês)Document11 pagesLaas 2012 (Inglês)André Toga Machado CoelhoNo ratings yet
- Maternal Hemodynamics: A Method To Classify Hypertensive Disorders of PregnancyDocument23 pagesMaternal Hemodynamics: A Method To Classify Hypertensive Disorders of PregnancyaulianmediansyahNo ratings yet
- Vascular Health in Children and Adolescents: Effects of Obesity and DiabetesDocument18 pagesVascular Health in Children and Adolescents: Effects of Obesity and DiabetesDANNYS PAOLA CARRASCAL PAREJONo ratings yet
- Aogs 12070Document6 pagesAogs 12070anon_118437533No ratings yet
- Dilated Ascendin Ao in The FetusDocument7 pagesDilated Ascendin Ao in The Fetusis_julieNo ratings yet
- Effect of Congenital Heart Disease On Child Growth: Dr. Deia K Khalaf, Dr. Yusra K Al-Rawi and Dr. Laith A Abdul HadiDocument7 pagesEffect of Congenital Heart Disease On Child Growth: Dr. Deia K Khalaf, Dr. Yusra K Al-Rawi and Dr. Laith A Abdul HadimuhammadrikiNo ratings yet
- History of Childhood Kidney Disease and Risk of Adult End-Stage Renal DiseaseDocument11 pagesHistory of Childhood Kidney Disease and Risk of Adult End-Stage Renal DiseasePaula Gomez RuidiazNo ratings yet
- Early Predictors of Cardiac Dysfunction in Egyptian Children With Chronic Kidney DiseaseDocument8 pagesEarly Predictors of Cardiac Dysfunction in Egyptian Children With Chronic Kidney DiseaseNensy AnggrainyNo ratings yet
- 1 s2.0 S0828282X22001271 MainDocument11 pages1 s2.0 S0828282X22001271 MainLilianne Mbengani LaranjeiraNo ratings yet
- Maternal and Fetal Outcomes in Pregnancy Complicated With Eisenmenger SyndromeDocument5 pagesMaternal and Fetal Outcomes in Pregnancy Complicated With Eisenmenger SyndromeRizka AdiNo ratings yet
- Rossano2014 PDFDocument6 pagesRossano2014 PDFAditya SanjayaNo ratings yet
- Reviews: Prenatal Screening For Structural Congenital Heart DiseaseDocument12 pagesReviews: Prenatal Screening For Structural Congenital Heart DiseaseAzis YunalNo ratings yet
- 29-Years Old Woman Presenting With ST Elevation Myocardial InfarctionDocument6 pages29-Years Old Woman Presenting With ST Elevation Myocardial InfarctionArikahDyahLamaraNo ratings yet
- J BCMD 2017 03 003Document46 pagesJ BCMD 2017 03 003aliakbar178No ratings yet
- Transitional Hemodynamics in Infants of Diabetic Mothers by Targeted Neonatal Echocardiography Electrocardiography and Peripheral Flow StudyDocument9 pagesTransitional Hemodynamics in Infants of Diabetic Mothers by Targeted Neonatal Echocardiography Electrocardiography and Peripheral Flow StudyEttore PiroNo ratings yet
- Evaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusDocument7 pagesEvaluation of Right Side Foetal Myocardial Performance Index in Pregestational and Gestational Diabetes MellitusGabyliz Gonzalez CastilloNo ratings yet
- Differences in Morbidity and Mortality in Down Syndrome Are Related To The Type of Congenital Heart DefectDocument10 pagesDifferences in Morbidity and Mortality in Down Syndrome Are Related To The Type of Congenital Heart DefectMaría BonettiNo ratings yet
- 86 FullDocument8 pages86 FullAsri RachmawatiNo ratings yet
- Cobas 6000Document8 pagesCobas 6000Dr SabaNo ratings yet
- Hsu 2020 Pediatric Heart FailureDocument2 pagesHsu 2020 Pediatric Heart Failurefitrumanama PlusNo ratings yet
- Loop Diuretics in Infants With Heart FailureDocument13 pagesLoop Diuretics in Infants With Heart FailureNATALY HASTAMORY VANEGASNo ratings yet
- De Boo Barker HypothesisDocument11 pagesDe Boo Barker HypothesisIamJmlingconNo ratings yet
- Pulmonary Embolism in Children: Cme R ADocument11 pagesPulmonary Embolism in Children: Cme R Azemenum temesgenNo ratings yet
- Barnes 1998. Central Adiposity and Hemodynamic Functioning at Rest andDocument9 pagesBarnes 1998. Central Adiposity and Hemodynamic Functioning at Rest andnaiarahsanzNo ratings yet
- HF-Pediatric Heart Failure - An Evolving Public Health ConcernDocument5 pagesHF-Pediatric Heart Failure - An Evolving Public Health ConcernRamaNo ratings yet
- Antenatal ProfileDocument6 pagesAntenatal ProfileSinchan GhoshNo ratings yet
- Aggoun 2007Document7 pagesAggoun 2007Messias FilhoNo ratings yet
- Daniel Slip Id Screening 2008Document13 pagesDaniel Slip Id Screening 2008Heart of the Valley, Pediatric CardiologyNo ratings yet
- Emotional Neglect in Childhood and Cerebral Infarction in Older AgeDocument8 pagesEmotional Neglect in Childhood and Cerebral Infarction in Older AgeOlward TôNo ratings yet
- Articulo 1 PDFDocument23 pagesArticulo 1 PDFAndrea HermosaNo ratings yet
- 10 1017@s1047951123004146Document5 pages10 1017@s1047951123004146Amir NaghshzanNo ratings yet
- Congenital Heart Defects: Amazing Advances and Ongoing ChallengesDocument2 pagesCongenital Heart Defects: Amazing Advances and Ongoing ChallengesNia WillyNo ratings yet
- Develop Med Child Neuro - 2022 - Houwen Van Opstal - Long Term Outcomes For Females With Early Onset DystrophinopathyDocument12 pagesDevelop Med Child Neuro - 2022 - Houwen Van Opstal - Long Term Outcomes For Females With Early Onset DystrophinopathyJessica CampoNo ratings yet
- Current Features of Infective Endocarditis in Elderly PatientsDocument9 pagesCurrent Features of Infective Endocarditis in Elderly PatientsNesri muskananNo ratings yet
- Coronary Heart Disease Risk Factors and Atherosclerosis in Young PeopleDocument9 pagesCoronary Heart Disease Risk Factors and Atherosclerosis in Young PeopleHadi KuriryNo ratings yet
- Telomere Length and Vascular PhenotypesDocument21 pagesTelomere Length and Vascular PhenotypesJohnNo ratings yet
- Seminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientDocument5 pagesSeminars in Pediatric Surgery: Progress in Anesthesia and Management of The Newborn Surgical PatientAsif KhanNo ratings yet
- Ajol-File-Journals 563 Articles 252250 64cba8c4c41a6Document9 pagesAjol-File-Journals 563 Articles 252250 64cba8c4c41a6Dr. Ashwin Raja MBBS MSNo ratings yet
- Jurnal s2Document6 pagesJurnal s2da8427164No ratings yet
- 10 3389@fsurg 2020 00047Document9 pages10 3389@fsurg 2020 00047Hana Nuraisa BasyaNo ratings yet
- Fetal Origins of Adult Disease Strength of Effect and Biological Basis PDFDocument5 pagesFetal Origins of Adult Disease Strength of Effect and Biological Basis PDFHervi LaksariNo ratings yet
- Left Ventricular Diastolic Dysfunction Among Youth With Obesity and History of Elevated Blood PressureDocument8 pagesLeft Ventricular Diastolic Dysfunction Among Youth With Obesity and History of Elevated Blood PressureVedith KumarNo ratings yet
- Heart Failure in ChildrenDocument27 pagesHeart Failure in ChildrendenakarinaNo ratings yet
- Brheartj00013 0001Document2 pagesBrheartj00013 0001Ramadhan Yudha PratamaNo ratings yet
- Breast Milk Consumption in Preterm Neonates and Cardiac Shape in AdulthoodDocument29 pagesBreast Milk Consumption in Preterm Neonates and Cardiac Shape in AdulthoodAsyha KantifaNo ratings yet
- Arterial Ischemic Stroke in Children: Risk Factors and EtiologiesDocument9 pagesArterial Ischemic Stroke in Children: Risk Factors and EtiologiesErick DjuandaNo ratings yet
- Hypertension in Children and Adolescents: New PerspectivesFrom EverandHypertension in Children and Adolescents: New PerspectivesEmpar LurbeNo ratings yet
- Insulin Resistance: Childhood Precursors of Adult DiseaseFrom EverandInsulin Resistance: Childhood Precursors of Adult DiseasePhilip S. ZeitlerNo ratings yet
- National Perinatal Hepatitis B Prevention Program: 2009 - 2017Document10 pagesNational Perinatal Hepatitis B Prevention Program: 2009 - 2017Suwandi ChangNo ratings yet
- PIIS0022347620315432Document8 pagesPIIS0022347620315432Suwandi ChangNo ratings yet
- Cost Analysis of Emergency Department Criteria For Evaluation of Febrile Infants Ages 29 To 90 DaysDocument10 pagesCost Analysis of Emergency Department Criteria For Evaluation of Febrile Infants Ages 29 To 90 DaysSuwandi ChangNo ratings yet
- Articles: OriginalDocument9 pagesArticles: OriginalSuwandi ChangNo ratings yet
- New England Journal Medicine: The ofDocument12 pagesNew England Journal Medicine: The ofSuwandi ChangNo ratings yet
- Perspective: New England Journal MedicineDocument3 pagesPerspective: New England Journal MedicineSuwandi ChangNo ratings yet
- Blood Test Normal ValuesDocument6 pagesBlood Test Normal Valueschristophe1967No ratings yet
- Miscarriage and Its Types: Farhad Ali 15 - 177 3 Year MBBSDocument21 pagesMiscarriage and Its Types: Farhad Ali 15 - 177 3 Year MBBSmarviNo ratings yet
- KPI - Foruth EditionDocument30 pagesKPI - Foruth EditionAnonymous qUra8Vr0SNo ratings yet
- APP765 FinishedDocument20 pagesAPP765 FinishedSimonTheRussianNo ratings yet
- Competitive Intelligence AcceraDocument29 pagesCompetitive Intelligence AcceranarenebiowebNo ratings yet
- Training Manual For Counselors PDFDocument197 pagesTraining Manual For Counselors PDFمخلص منيب اللهNo ratings yet
- New Classification PerioDocument15 pagesNew Classification Periokhaled alahmadNo ratings yet
- PEDro Scale Kelompok KLDocument3 pagesPEDro Scale Kelompok KLKelompok L Ayu Anjali Diah PNo ratings yet
- NZREX Clinical Handbook For Candidates 201 New ZealandDocument14 pagesNZREX Clinical Handbook For Candidates 201 New Zealandlaroya_31No ratings yet
- Course in The WardDocument7 pagesCourse in The WardKevin CalaraNo ratings yet
- Ways To Maintain A Good HealthDocument1 pageWays To Maintain A Good Healthaileeneo76No ratings yet
- Option Com - Content&view Section&layout Blog&id 3 &itemid 60 FaqsDocument7 pagesOption Com - Content&view Section&layout Blog&id 3 &itemid 60 FaqsJig GamoloNo ratings yet
- Approach To Patients With High Anion Gap Metabolic Acidosis Core Curriculum 2021Document11 pagesApproach To Patients With High Anion Gap Metabolic Acidosis Core Curriculum 2021hossein kasiriNo ratings yet
- Care Plan For SchizophreniaDocument6 pagesCare Plan For SchizophreniaAllea Likestolaugh Brown100% (2)
- Psoriatis ArthritisDocument14 pagesPsoriatis Arthritisferdinan goutamaNo ratings yet
- Diabetic Neuropathies: The Nerve Damage of DiabetesDocument12 pagesDiabetic Neuropathies: The Nerve Damage of DiabetestaqiedaNo ratings yet
- JCSO 2021 ReviewDocument67 pagesJCSO 2021 ReviewENo ratings yet
- Blast Injury: Steven A. Santanello, DO Grant Medical Center Trauma Medical DirectorDocument19 pagesBlast Injury: Steven A. Santanello, DO Grant Medical Center Trauma Medical DirectorRich AdamsNo ratings yet
- Bautista, Raphael Ephraime P. (Peh Lesson Plan)Document8 pagesBautista, Raphael Ephraime P. (Peh Lesson Plan)Raph BautistaNo ratings yet
- B&B Videos and UWorld QIDs No DuplicatesDocument17 pagesB&B Videos and UWorld QIDs No Duplicatesوائل عبداللطيف عبدالقادرNo ratings yet
- Sample Letter - Recommended For: Day Care Center/Preschool/ Elementary School/Middle SchoolDocument2 pagesSample Letter - Recommended For: Day Care Center/Preschool/ Elementary School/Middle SchoolbatambintanNo ratings yet
- Pediatric Autonomic DisorderDocument15 pagesPediatric Autonomic DisorderaimanNo ratings yet
- Hagi Ruiz Lopez ResumeDocument1 pageHagi Ruiz Lopez Resumeapi-661322418No ratings yet
- Heatstroke HTPDocument4 pagesHeatstroke HTPshainakyllebarbonNo ratings yet
- June 2018 QP - Biology 1 (H) Edexcel Science GCSEDocument24 pagesJune 2018 QP - Biology 1 (H) Edexcel Science GCSESHOABNo ratings yet
- Journal Pre-Proof: International Journal of Antimicrobial AgentsDocument9 pagesJournal Pre-Proof: International Journal of Antimicrobial AgentsBeatrizNo ratings yet
- Ijms 21 00431 v2Document9 pagesIjms 21 00431 v2mikhaelyosiaNo ratings yet
- EFG Healthcare - BrochureDocument2 pagesEFG Healthcare - BrochuremikewiesenNo ratings yet
- Adult Intake Form-New ClientDocument7 pagesAdult Intake Form-New ClientKelvin NuñezNo ratings yet
- Komunikasi Perawat Dengan Motivasi Pasien Menjalani Perawatan Stroke Rsu Herna MedanDocument8 pagesKomunikasi Perawat Dengan Motivasi Pasien Menjalani Perawatan Stroke Rsu Herna Medanfredy resmanaNo ratings yet