Professional Documents
Culture Documents
Nutritional and Health Status of Tibetan Children Living at High Altitudes
Uploaded by
Giorgio CortassaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nutritional and Health Status of Tibetan Children Living at High Altitudes
Uploaded by
Giorgio CortassaCopyright:
Available Formats
N U T R I T I O N A L A N D H E A LT H STAT U S O F T I B ETA N C H I L D R E N L I V I N G AT H I G H A LT I T U D E S
NUTRITIONAL AND HEALTH STATUS OF TIBETAN CHILDREN
LIVING AT HIGH ALTITUDES
NANCY S. HARRIS, M.D., PATRICIA B. CRAWFORD, DR.P.H., YESHE YANGZOM, M.D., LOBSANG PINZO, M.D.,
PALDEN GYALTSEN, M.D., AND MARK HUDES, PH.D.
ABSTRACT health status, growth, or nutritional status of children
Background Children living at high altitudes often in this region. A 1986 study of 14,000 Tibetan chil-
have delayed growth, but whether growth retardation dren ranging in age from birth to seven years in Lhasa
is related to altitude or to other factors is not known. Prefecture concluded that the nutritional status of Ti-
Methods A multicultural health care team assessed betan children was “acceptable overall,” and the data
2078 Tibetan children 0 to 84 months of age for an- were used to generate reference ranges for the growth
thropometric and clinical signs of malnutrition. The of Tibetan children.18-20 However, in an unpublished
children lived in 11 counties, which contained more 1989 survey conducted by the People’s Republic of
than 50 diverse urban and nonurban (nomadic, agri- China in 16 Tibetan counties, the mortality rate
cultural, or periurban) communities in the Tibet Au-
tonomous Region of China. The height and weight of
among infants was 92 per 1000 in the Tibetan coun-
the children were compared with those of U.S. chil- ties, as compared with 68 per 1000 in the rest of Chi-
dren. Height and weight were expressed as z scores na; the mortality rate among children less than five
(the number of standard deviations from the median years old was 127 per 1000, as compared with 84 per
of the age- and sex-specific reference group). 1000; and the maternal mortality rate was 73 per
Results The mean z score for height fell from ¡0.5 10,000, as compared with 20 per 10,000.21 We eval-
to ¡1.6 in the first 12 months of life and generally uated the health status of Tibetan children to deter-
ranged from ¡2.0 to ¡2.4 in older children. Overall, mine whether their short stature is due to factors oth-
of 2078 children, 1067 (51 percent) had moderately or er than high altitude.
severely stunted growth, as defined by a z score of
¡2.0 or lower. Of the 1556 children 24 months of age METHODS
or older, 871 (56 percent) had stunted growth, which
Study Subjects
was severe (z score, ¡3.0 or lower) in 380 (24 percent).
Among the children in this age group, 787 of the During August through December of 1994 and 1995, we ex-
1313 nonurban children (60 percent) had stunting, as amined 2078 Tibetan children from birth to 84 months of age
compared with 84 of the 243 urban children (35 per- who were from 11 counties in five of the seven prefectures in the
cent). Stunting was associated with clinical conditions Tibet Autonomous Region. The 11 counties, which contained more
than 50 townships, were representative of the wide range of regions
such as rickets, abdominal distention, hair depigmen- (from urban to nomadic) in Tibet. For statistical purposes, the data
tation, and skin lesions and with a maternal history of were aggregated according to the type of region: urban (Lhasa and
hepatitis or goiter. Stunting was not associated with Chamdo), periurban (within 30 km of Lhasa or Chamdo), village,
altitude, after adjustment for the type of community. and nomadic. On the basis of census data provided by local health
Conclusions In Tibetan children, severe stunting workers in each county, approximately 90 percent of the eligible
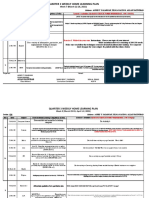
due to malnutrition occurs early in life, and morbidity children were surveyed. A map of the study sites and the distribu-
is high. (N Engl J Med 2001;344:341-7.) tions of the children according to age and location are shown in
Copyright © 2001 Massachusetts Medical Society.
Figure 1.
Data Collection
A team of three Tibetan physicians (two pediatricians and one
internist), one U.S. physician, a nutritional anthropologist, local
representatives of the Tibetan Maternal and Child Health Depart-
ment, and village health workers collected the data in all 11 coun-
M
ANY people who live at high altitudes ties, in accordance with protocols approved by the Tibetan health
are shorter than their lowland counter- authorities. Informed consent was obtained from a parent or care-
parts.1-6 However, well-nourished chil- taker of each child.
dren from diverse ethnic groups will at- Medical histories of children and mothers were collected from
tain a height within international reference ranges.7,8 parents with the use of a pretested questionnaire administered in
Tibetan by the pediatricians. Translators were used when local di-
Therefore, the short stature of children living at high alects differed. Birth-date information was collected with the use
altitudes should not be attributed to factors such as
genetics and altitude when it may represent growth
failure due to chronic undernutrition. Stunting of From the Tibet Child Nutrition and Collaborative Health Project, Pub-
lic Health Institute, Santa Cruz, Calif. (N.S.H.); the Department of Nutri-
growth as a consequence of chronic malnutrition is tional Sciences, University of California at Berkeley, Berkeley (P.B.C., M.H.);
often associated with irreversible neurodevelopmen- and the Department of Pediatrics and Medical Research (Y.Y., L.P.) and the
tal delay and increased morbidity and mortality.9-17 Tibet Medical Research Institute (P.G.), First People’s Hospital, Lhasa, Tibet
Autonomous Region of China. Address reprint requests to Dr. Crawford
The Tibet Autonomous Region of China is one at the Department of Nutritional Sciences and Toxicology, University of Cal-
such high-altitude area, and little is known about the ifornia at Berkeley, Berkeley, CA 94720, or at pbcraw@uclink4.berkeley.edu.
N Engl J Med, Vol. 344, No. 5 · February 1, 2001 · www.nejm.org · 341
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
Qinghai
Ngari Nagchu
Sichuan
Sogchen
Rioche
Dengchen
Nagchu Chamdo
Mt. Kailas Chamdo
Damshung
Bamda
Purang Lhasa Monkham
India Tulum Medrogonggar
KongpoF
Gyamda
Bayi Pome
Shigatse
Yangching
Shigatse Tsedang Nyingtri
Areas of studyF Xegar Gyantse
CitiesF Lhogar
Regional capitals Nepal Mt. EverestF
(8848 m) Yunnan
0 km 100 Kathmandu
Bhutan
0 62
mi
Myanmar
No. of Children Examined
AGE (mo) NOMADIC VILLAGE PERIURBAN URBAN TOTAL
0–11F 19F 150F 50F 27F 246F
12–23F 21F 155F 57F 33F 266F
24–35F 24F 204F 72F 38F 338F
36–47F 30F 184F 68F 50F 332F
48–59F 44F 165F 55F 69F 333F
60–71F 30F 165F 47F 59F 301F
»72F 38F 161F 36F 27F 262F
Total 206 1184 385 303 2078
Figure 1. Map of Tibet Autonomous Region Showing Study Sites and the Number of Children Examined According to Age and
Location (1035 Boys and 1043 Girls).
The map is based on information from the Bureau of Survey of Tibet Autonomous Region22 and Dorje.23
of the Tibetan lunar calendar and was subsequently converted to and secondary infections, and angular stomatitis. Examination for
Gregorian calendar dates. For most children, parents or caretakers rickets included inspection for all major and minor signs of rickets.
provided health booklets in which the birth dates were recorded; The most common signs of rickets were craniotabes, frontal bossing,
complete birth-date information was available for 85 percent of rachitic rosary, delayed fontanelle closure, delayed dentition, occip-
the children. For the 161 children for whom the year and month ital alopecia, and thoracic deformities (Harrison’s grooves and pi-
of birth were known but the day of birth was unknown, the 15th geon chest).
of the month was used as the estimated birthday. For 158 children, Anthropometric measurements, performed with the use of stand-
the month of birth could not be determined, and a midyear birth ard methods,24 included measurements of height, weight, head cir-
date was used. The questionnaire used for the child’s history includ- cumference, chest circumference, and mid-upper-arm circumference.
ed specific questions about hepatitis (clinical jaundice), diarrhea or The children were weighed and measured with a calibrated, beam-
cough lasting longer than one month, night blindness, measles, and balance scale and stadiometer (Panda Model TGT-50, Shanghai Bao
otitis. The questionnaire for the mother’s history included questions Shen Measurement Factory, Shanghai, China) used by the United
about clinical jaundice and visible goiter. Nations Children’s Fund Maternal and Child Health programs
Four of us performed the physical examinations. The children throughout China. Children less than two years of age and those
were examined for hair depigmentation, abdominal distention, skin two to three years of age who were unable to stand were measured
abnormalities and sores,24 rickets,24,25 goiter,26 caries, and Kashin– while recumbent with the use of a standard calibrated board (Gold-
Beck disease.27-29 A crippling arthropathy affecting large joints, Kash- en Lion Model WB1, Beijing Tractor Company No. 6 Measuring
in–Beck disease is found in regions of Asia, primarily in China. Factory, Beijing, China). All children were weighed while they were
Physical examination for the disease was confined to inspection of wearing one layer of undergarments, without shoes. All these meas-
the wrist, a commonly involved site, for signs of deformity. Skin urements were performed by or in the presence of the same four
lesions included xerosis, intertriginous lesions, diffuse excoriations researchers, with good interobserver correlation.
342 · N Engl J Med, Vol. 344, No. 5 · February 1, 2001 · www.nejm.org
N U T R I T I O N A L A N D H E A LT H STAT U S O F T I B ETA N C H I L D R E N L I V I N G AT H I G H A LT I T U D E S
Statistical Analysis ble up to 84 months of age. Thus, age would have con-
The age in months was rounded down to the nearest integer and founded any analysis of a relation between the height-
examined as a categorical variable as follows: 0 to 11 months, 12 to for-age z score and other variables related to age.
23 months, 24 to 35 months, 36 to 47 months, 48 to 59 months,
60 to 71 months, and 72 months or more. Because some families
For this reason, data from children from birth to 24
included multiple siblings, the data were analyzed with the use of months of age were not included in further analyses.
a generalized estimating equation program to adjust for correlation Anthropometric measures of malnutrition were
within households.30 Height and weight were compared with nor- evaluated according to location. The mean height-for-
malized growth curves from the reference population of the U.S. age z score was lower than ¡2.0 for all groups of chil-
National Center for Health Statistics.31 For each category of age,
height for age, weight for age, and weight for height, z scores were dren except those living in urban areas. Nearly twice
computed by subtracting the age-specific median reference value as many children in nonurban areas (village, nomadic,
from the measured value and dividing the difference by the age-spe- or periurban) as children in urban areas had z scores of
cific standard deviation for the reference population.32 ¡2.0 or lower (60 percent vs. 34 percent), and more
Chi-square tests were performed to evaluate the relations of the
categorical height-for-age z score and clinical conditions with urban
than three times as many children in nonurban areas
or nonurban location. To compare height-for-age z scores among had z scores of ¡3.0 or lower (Table 1). The preva-
children with clinical conditions and those without clinical condi- lence of wasting, as indicated by the mean weight-for-
tions, two independent sample t-tests were used. All statistical tests height z score, was low (Table 2). This finding is not
were two-tailed. uncommon in malnourished populations with high
The z scores were compared according to community location
with one-way analysis of variance. After adjustments for correlation levels of stunting,34 since wasting is a result of short-
among siblings, Bonferroni techniques were used to determine the term nutritional deprivation.
overall type I error rates for all follow-up procedures.33 Fourteen percent of children less than 24 months
of age had a mid-upper-arm circumference of less than
RESULTS
11.5 cm. This value has been used as a predictor of
Prevalence of Malnutrition a significantly increased risk of death in young chil-
Overall, the prevalence of stunted growth (z score, dren.35 Furthermore, 75 percent of children 12 to
¡2.0 or lower) was 51 percent (1067 of 2078 chil- 23 months of age had a chest-to-head circumference
dren). The patterns of stunting according to age were ratio of less than 1.0, which indicates undernutrition.24
similar in girls and boys; however, girls had higher
z scores after 12 months of age (Fig. 2). Growth failure Children’s z Scores and Location
was most pronounced during the first 12 months of Of the children 24 months of age or older, 56 per-
life and was almost as pronounced from 12 through 23 cent had a height-for-age z score that was at least 2 SD
months, after which time z scores remained fairly sta- below the reference value (Table 1). Children in ur-
1.0
0.5
0.0
¡0.5
Mean z Score
¡1.0
¡1.5 Girls
F
¡2.0
Boys
¡2.5
¡3.0
¡3.5
0
9
11
1
3
8
4
5
5
7
7
–2
–5
–7
–2
6–
–1
–8
1–
–3
–1
–4
9–
18
48
60
21
12
72
24
15
36
Age (mo)
Figure 2. Mean Height-for-Age z Score According to Age and Sex.
A z score of zero indicates the mean of the reference group.
N Engl J Med, Vol. 344, No. 5 · February 1, 2001 · www.nejm.org · 343
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
Prevalence of Clinical Conditions
TABLE 1. HEIGHT-FOR-AGE Z SCORE FOR
CHILDREN 24 MONTHS OF AGE OR OLDER,
The prevalence of clinical conditions and details of
ACCORDING TO LOCATION.* the medical histories of urban and nonurban children
24 months of age or older are shown in Table 3. Clin-
ical signs of rickets were detected in 66 percent of the
URBAN NONURBAN
Z SCORE (N=243) (N=1313)† children, most of whom were in nonurban areas. The
serum concentration of 25-hydroxyvitamin D, which
no. of children (%)
was measured in 130 children from all locations, was
«¡3.0 (Severe stunting) 18 (7) 362 (28) less than 10 ng per milliliter (25 nmol per liter) in 110
¡2.9 to ¡2.0 (Moderate stunting) 66 (27) 425 (32) children (85 percent).
¡1.9 to ¡1.0 86 (35) 349 (27) Children in nonurban areas were significantly more
¡0.9 to 0.0 48 (20) 127 (10)
likely than those in urban areas to have depigmented
>0.0 25 (10) 50 (4)
hair, abdominal distention, skin lesions, goiter, and a
*The z score is the number of standard deviations from maternal history of goiter. Children in urban areas
the median value for the reference group. The height-for-age were significantly more likely to have caries and a his-
distribution differed significantly according to urban or non-
urban status (P<0.001 by the chi-square test). Because of tory of measles (Table 3).
rounding, percentages do not total 100. Goiter was found in 3 percent of the children. Al-
†The nonurban group included children living in village, though Kashin–Beck disease is known to occur in sev-
nomadic, and periurban areas. eral of the areas studied, early signs of this disease were
found in only 1 percent of the children. The arthrop-
athy that characterizes the disease usually becomes
ban areas had the lowest risk of stunting, which dif- clinically evident after five years of age. Deformity of
fered significantly from the risk for those in village and the limbs in the children we studied was usually post-
periurban areas (Table 2). Nomadic children had a sig- traumatic. Stunting was associated with signs of rick-
nificantly greater risk of stunting than did all other ets, hair depigmentation, abdominal distention, and
children. skin lesions and with a maternal history of hepatitis
Both children in urban areas and nomadic children or goiter (Table 4).
had a significantly lower prevalence of rickets than did
children in village and periurban areas (Table 2), sug- Association between Altitude and Stunting
gesting that factors other than rickets play a part in There was no linear association between height-
the stunted growth of nomadic children. for-age z scores and altitude. The children 24 months
TABLE 2. MEAN ANTHROPOMETRIC MEASUREMENTS AND THE PREVALENCE OF RICKETS ACCORDING TO LOCATION.*
AGE »24 MO AGE <24 MO AGE 12 TO 23 MO
RATIO OF CHEST-
MID-UPPER-ARM TO-HEAD
NO. OF HEIGHT FOR WEIGHT FOR WEIGHT FOR NO. OF CIRCUMFERENCE NO. OF CIRCUMFERENCE
LOCATION CHILDREN AGE†‡§¶¿ HEIGHT‡¿** AGE†‡§¶** RICKETS†‡¶¿** CHILDREN <11.5 CM† CHILDREN <1.0
z score % % %
Nomadic 165 ¡2.8 ¡0.1 ¡1.8 44 40 32 21 80
Village 871 ¡2.2 0.02 ¡1.4 78 305 11 155 77
Periurban 277 ¡2.1 0.3 ¡1.1 63 107 15 57 72
Urban 243 ¡1.5 ¡0.1 ¡1.1 38 60 15 33 70
Total 1556 ¡2.2 0.03 ¡1.3 66 512 14 266 75
*Height for age, weight for height, weight for age, and the presence or absence of rickets were determined in children 24 months of age or older. Mid-
upper-arm circumference was measured in children less than 24 months of age, and the ratio of chest-to-head circumference was determined for children
between 12 and 23 months. Multiple comparisons were made with the use of Bonferroni techniques at a significance level of 0.05. Therefore, differences
between any two groups were considered statistically significant at P<0.008 (P<0.05 divided by 6, the number of comparisons).
†Values for nomadic locations were significantly different from those for villages.
‡Values for nomadic locations were significantly different from those for periurban locations.
§Values for nomadic locations were significantly different from those for urban locations.
¶Values for villages were significantly different from those for urban locations.
¿Values for periurban locations were significantly different from those for urban locations.
**Values for villages were significantly different from those for periurban locations.
344 · N Engl J Med, Vol. 344, No. 5 · February 1, 2001 · www.nejm.org
N U T R I T I O N A L A N D H E A LT H STAT U S O F T I B ETA N C H I L D R E N L I V I N G AT H I G H A LT I T U D E S
TABLE 3. CLINICAL STATUS OF CHILDREN 24 MONTHS OR OLDER TABLE 4. HEIGHT-FOR-AGE Z SCORE FOR CHILDREN 24 MONTHS
ACCORDING TO LOCATION. OF AGE OR OLDER ACCORDING TO CLINICAL STATUS.
TOTAL URBAN NONURBAN P TOTAL
CLINICAL STATUS (N=1556) (N=243) (N=1313) VALUE* CLINICAL STATUS (N=1556) HEIGHT-FOR-AGE Z SCORE
WITH WITHOUT P
no. (%) CONDITION CONDITION VALUE*
Condition no. (%)
Rickets 1024 (66) 93 (38) 931 (71) <0.001
Hair depigmentation 672 (43) 37 (15) 635 (48) <0.001 Condition
Abdominal distention 855 (55) 44 (18) 811 (62) <0.001 Rickets 1024 (66) ¡2.3 ¡2.0 <0.001
Skin lesions† 134 (9) 13 (5) 121 (9) 0.02 Hair depigmentation 672 (43) ¡2.4 ¡2.0 <0.001
Caries 615 (40) 111 (46) 504 (38) 0.04 Abdominal distention 855 (55) ¡2.3 ¡2.0 <0.001
Kashin–Beck disease 15 (1) 0 15 (1) 0.15‡ Skin lesions 134 (9) ¡2.4 ¡2.2 0.04
Goiter 49 (3) 1 (<1) 48 (4) 0.007 Caries 615 (40) ¡2.1 ¡2.2 0.07
Medical history Kashin–Beck disease 15 (1) ¡2.5 ¡2.2 0.27
Hepatitis 77 (5) 12 (5) 65 (5) 0.88 Goiter 49 (3) ¡2.3 ¡2.2 0.47
Maternal history of 72 (5) 10 (4) 62 (5) 0.82 Medical history
hepatitis Hepatitis 77 (5) ¡2.4 ¡2.2 0.08
Maternal history of goiter 225 (14) 4 (2) 221 (17) <0.001 Maternal history of 72 (5) ¡2.6 ¡2.2 0.002
Diarrhea for >1 mo 146 (9) 17 (7) 129 (10) 0.20 hepatitis
Cough for >1 mo 171 (11) 35 (14) 136 (10) 0.06 Maternal history of goiter 225 (14) ¡2.4 ¡2.1 <0.001
Night blindness 11 (1) 0 11 (1) 0.39‡ Diarrhea for >1 mo 146 (9) ¡2.3 ¡2.2 0.08
Measles 77 (5) 26 (11) 51 (4) 0.001 Cough for >1 mo 171 (11) ¡2.2 ¡2.2 0.86
Otitis 214 (14) 29 (12) 185 (14) 0.52 Night blindness 11 (1) ¡2.5 ¡2.2 0.33
Measles 77 (5) ¡2.2 ¡2.2 0.78
*P values were calculated by chi-square tests for independence unless Otitis 214 (14) ¡2.3 ¡2.2 0.07
otherwise noted.
†Skin lesions included xerosis, sores, and intertriginous lesions. *P values were calculated from two independent-sample t-tests with ad-
justment for interclass correlation within households.
‡The P values were calculated by Fisher’s exact test.
of age or older who lived at the highest altitude in an urban area and 91.5 cm if he lived in a nonur-
(greater than 4000 m) and those who lived at the ban area. For the 1994–1995 period, the respective
lowest altitude (less than 3000 m) had the lowest values were 93.0 cm and 89.8 cm. Thus, over the nine-
mean z scores (¡2.6 and ¡2.2, respectively). The year period from 1986 to 1995, the average height of
children who lived at an altitude of 3000 to 4000 m a 42-month-old boy declined by 1.7 cm (P<0.001)
had the highest mean z score (¡1.9). Within each in both urban and nonurban areas.
category of altitude, urban children had higher height-
Death Rate among Children
for-age z scores than did nonurban children living at
the same altitude. Although the death rates for children could not be
obtained, mothers were asked how many times they
Trends in Stunting had given birth and how many of their children were
With the use of the technique described by Shen still living. The age of a child at death could not always
et al.,36 sex-specific z scores were calculated and com- be determined. A mean of 3.2 children were born to
pared with those from a regional survey conducted each of the 1499 women surveyed; a mean of 2.8 chil-
in 1986.19 The z scores for children 24 months of dren were still living and a mean of 0.4 had died. The
age or older in the 1986 survey and in ours were mortality rate among all children born to all women
pooled and weighted to reflect the distribution of ages surveyed was 13.2 percent.
in each survey. The mean z scores were then convert-
ed back to reflect a hypothetical, statistically standard- DISCUSSION
ized case of a boy 42 months old and 99.1 cm tall. A We found evidence of substantial malnutrition
comparison of the results of the earlier survey with among Tibetan children. Over 50 percent of the chil-
the present data is not ideal because of possible un- dren we examined had moderate-to-severe stunting of
known differences in methodology. Although neither growth. The proportion of children with stunted
large survey is technically representative of Tibetan growth was greater in nonurban areas than in urban
children because of the sampling methods, together areas. The association between community location,
they allow an approximate comparison of growth altitude, and stunting was partially confounded by the
trends among children in Tibet. In 1986 the average fact that all the nomadic children were in the highest-
height of a 42-month-old boy was 94.7 cm if he lived altitude group and all urban and periurban children
N Engl J Med, Vol. 344, No. 5 · February 1, 2001 · www.nejm.org · 345
The Ne w E n g l a nd Jo u r n a l o f Me d ic i ne
were in the middle altitude group. However, children partment, Medrogonggar; the Shue Day Care Center, Lhasa; the
who lived in villages were represented in all three al- Maternal and Child Health Department, Nagchu; the County Health
Department, Lyingchi County; and the County Health Department,
titude groups, and for them we found no association Chamdo Prefecture; to Nancy Nielsen, R.N., Jay Narayan, and Miye-
between altitude and stunting, indicating that the ef- ko Teranishi, Seton Medical Center; to Dr. Elizabeth Burri, U.S. De-
fect of altitude is not the determining factor in growth partment of Agriculture Western Human Nutrition Research Cen-
failure. ter; to Dr. Jean-Pierre Habicht for his thoughtful suggestions; to Drs.
Elizabeth Hartka, Margaret Meites, Frank Falkner, and Sheldon Mar-
Our data show that Tibetan children are not “small gen for their review of the manuscript; to R. Marcus Choy for assist-
but healthy.”37-39 They have clinical signs of malnutri- ance with graphics; and to Carol Guion, Harriet Beinfield, Kristina
tion as well as high morbidity and mortality. Measure- Hamel, Nicole Lordi, Claudia Olague, Cindy Caffery, and Sheila
ments of mid-upper-arm circumference alone suggest Stern for their editorial assistance.
that up to 14 percent of children less than 24 months
of age have a level of malnutrition that has been as- REFERENCES
sociated with a significantly increased risk of death in 1. Haas JD, Moreno-Black G, Frongillo EA Jr, et al. Altitude and infant
growth in Bolivia: a longitudinal study. Am J Phys Anthropol 1982;59:
young children.34 Delayed development, as indicated 251-62.
by a low ratio of chest-to-head circumference, is fur- 2. Frisancho AR. Perspectives on functional adaptation of the high altitude
ther evidence of growth failure in these children early native. Prog Clin Biol Res 1983;136:383-407.
3. Leonard WR. Nutritional determinants of high-altitude growth in
in life. Although standard mortality rates could not be Nunoa, Peru. Am J Phys Anthropol 1989;80:341-52.
calculated, the mortality rate among all children born 4. Singh SP. Growth patterns of children of Tibetan origin living at mod-
to all the women surveyed can be compared with sim- erate altitudes, India. Z Morphol Anthropol 1980;71:187-95.
5. Pawson IG. Growth characteristics of populations of Tibetan origin in
ilar rates in other developing countries. For example, Nepal. Am J Phys Anthropol 1977;47:473-82.
in India the comparable mortality rate is 15 percent.40 6. Majumder PP, Gupta R, Mukhopadhyay B, et al. Effects of altitude,
ethnicity-religion, geographical distance, and occupation on adult anthro-
The decline in the average height of children be- pometric characteristics of eastern Himalayan populations. Am J Phys An-
tween 1986 and 1995 is similar to trends in other poor thropol 1986;70:377-93.
regions in China,36,41,42 which may be masked in ag- 7. Martorell R, Lechtig A, Yarbrough C, et al. Small stature in developing
nations: its causes and implications. In: Margen S, Ogar RA, eds. Sympo-
gregated data by the increase in the average height of sium on the biological and cultural sources of variability in human nutri-
children in more affluent regions of the country. A tion. Vol. 2 of Progress in human nutrition. Westport, Conn.: AVI Pub-
1991 study of 7-to-18-year-old children in Lhasa re- lishing, 1978:142-56.
8. Habicht J-P, Martorell R, Yarbrough C, Malina RM, Klein RE. Height
vealed that these urban children were taller than chil- and weight standards for preschool children: how relevant are ethnic dif-
dren in that group in 1985.43 This finding may sup- ferences in growth potential? Lancet 1974;1:611-4.
9. Garn SM. Stature norms and nutritional surveys. Ecol Food Nutr 1973;
port the hypothesis that, with adequate nutrition, 2:79-81.
Tibetan children who live past the vulnerable early ages 10. Allen LH. The nutrition CRSP: what is marginal malnutrition, and
are reaching their growth potential. does it affect human function? Nutr Rev 1993;51:255-67.
11. Grantham-McGregor SM. Assessments of the effects of nutrition on
This study was cross-sectional, and therefore direct mental development and behavior in Jamaican studies. Am J Clin Nutr
causality cannot be determined, but it appears that 1993;57:Suppl:303S-309S.
malnutrition and illness between 12 and 24 months 12. Burger SE, Haas JD, Habicht J-P. Testing the effects of nutrient defi-
ciencies on behavioral performance. Am J Clin Nutr 1993;57:Suppl:295S-
of age are important determinants of subsequent 302S.
height-for-age z scores. This information is useful for 13. DeLong GR. Effects of nutrition on brain development in humans.
Am J Clin Nutr 1993;57:Suppl:286S-290S.
those planning health interventions for children. 14. Chen LC, Chowdhury A, Huffman SL. Anthropometric assessment of
Generalizations about the growth of children living energy-protein malnutrition and subsequent risk of mortality among pre-
at high altitudes may deflect attention from the urgent school aged children. Am J Clin Nutr 1980;33:1836-45.
15. Pelletier DL. The potentiating effects of malnutrition on child mor-
need for maternal and child health programs in Ti- tality: epidemiologic evidence and policy implications. Nutr Rev 1994;52:
bet.44,45 Malnutrition and common childhood illness- 409-15.
es can be modified by changes in health education and 16. Victora CG, Barros FC, Kirkwood BR, Vaughan JP. Pneumonia, diar-
rhea, and growth in the first 4 years of life: a longitudinal study of 5914
health care. Culturally specific programs should be urban Brazilian children. Am J Clin Nutr 1990;52:391-6.
implemented to address the constellation of physio- 17. Victora CG. The association between wasting and stunting: an inter-
national perspective. J Nutr 1992;122:1105-10.
logic, socioeconomic, agricultural, and environmental 18. China: feasibility study for an integrated rural development project in
factors that affect the health of children on the Tibet- Pa Nam County, Tibet: appraisal and feasibility report. Annex 7. Luxem-
an plateau. bourg: Commission of the European Communities, September 1994.
19. Zhou AH, Hou SY, Qiang B, Bu Q, Wu ZWM. Survey and study on
nutritional and growth status of children, ages 0-84 months, living in
Supported in part by grants from the Audrey Hepburn Children’s Fund, Lhasa Municipal area, Tibet. Lhasa, China: Maternal and Child Hospital
the Columbia Foundation, the Cummings Foundation, the Seton Institute of Lhasa Municipality, 1986.
for International Development and Seton Hospital, the Thrasher Founda- 20. Kolsteren P, Atkinson S, Maskall K. Nutrition, health, water and san-
tion, the Tides Foundation, and the Trace Foundation. itation assessment in the Lhasa Valley: report of Save the Children UK and
the Lhasa Municipal Health Bureau. London: Save the Children, May–
We are indebted to our Tibetan colleagues Dr. Du Teng, Director June 1990.
21. National Center of Health Information and Statistics. MCH baseline
of the Tibetan Regional Health Bureau, Dr. Li Cheng Song, Direc- study. People’s Republic of China: National Ministry of Public Health,
tor of the First People’s Hospital, Madame Wang Yu Shu, Vice Direc- 1989.
tor of the First People’s Hospital, and Dr. Ke Sang, Director of Scien- 22. Bureau of Survey of Tibet Autonomous Region. The atlas of Tibet Au-
tific Training at the First People’s Hospital; to the staffs of the Health tonomous Region. Beijing, China: China Map Press, 1995.
Department, Medrogonggar; the Maternal and Child Health De- 23. Dorje G. Tibet handbook. Bath, England: Footprint Handbooks, 1999.
346 · N Engl J Med, Vol. 344, No. 5 · February 1, 2001 · www.nejm.org
N U T R I T I O N A L A N D H E A LT H STAT U S O F T I B ETA N C H I L D R E N L I V I N G AT H I G H A LT I T U D E S
24. Jelliffe DB. The assessment of the nutritional status of the community. weight-for-height as an indicator of nutritional status. Am J Clin Nutr
Geneva: World Health Organization, 1966. 1987;46:411-8.
25. Muhe L, Lulseged S, Mason KE, Simoes EA. Case-control study of 35. Trowbridge FL, Sommer A. Nutritional anthropometry and mortality
the role of nutritional rickets in the risk of developing pneumonia in Ethi- risk. Am J Clin Nutr 1981;34:2591-2.
opian children. Lancet 1997;349:1801-4. 36. Shen T, Habicht J-P, Chang Y. Effect of economic reforms on child
26. Delange F, Bastani M, Benmiloud M, et al. Definitions of endemic growth in urban and rural areas of China. N Engl J Med 1996;335:400-6.
goiter and cretinism, classification of goiter size and severity of endemias, 37. Seckler D. The “small but healthy” hypothesis: a basic hypothesis in
and survey techniques. In: Dunn JT, Pretell EA, Daza CH, Viteri FE, eds. the theory, measurement and policy of malnutrition. In: Sukhatme PV, ed.
Towards the eradication of endemic goiter, cretinism, and iodine deficiency. Newer concepts in nutrition and their implication for policy. Pune, India:
Washington, D.C.: Pan American Health Organization, 1986:373-6. (Sci- Maharashtra Association for the Cultivation of Science Research Institute,
entific publication no. 502.) 1982:127-37.
27. Mathieu F, Begaux F, Lan ZY, Suetens C, Hinsenkamp M. Clinical 38. Gopalan C. “Small but healthy?” For the poor, not the rich! New Del-
manifestations of Kashin-Beck disease in Nyemo Valley, Tibet. Int Orthop hi, India: Nutrition Foundation of India, October 1983:1-8.
1997;21:151-6. 39. Beaton GH. Small but healthy? Are we asking the right question? Eur
28. Chasseur C, Suetens C, Nolard N, Begaux F, Haubruge E. Fungal J Clin Nutr 1989;43:863-75.
contamination in barley and Kashin-Beck disease in Tibet. Lancet 1997; 40. National Family Health Survey (MCH and family planning), India
350:1074. 1992-93. Bombay, India: International Institute for Population Sciences,
29. Moreno-Reyes R, Suetens C, Mathieu F, et al. Kashin–Beck osteoar- 1995.
thropathy in rural Tibet in relation to selenium and iodine status. N Engl 41. Shi L. Health care in China: a rural-urban comparison after the socio-
J Med 1998;339:1112-20. economic reforms. Bull World Health Organ 1993;71:723-36.
30. Karim MR , Zeger SL. GEE: a SAS macro for longitudinal data analy- 42. Chang Y, Xian ZD, He W, Chang SY, Ma HJ, Chen CM. Child mal-
sis (version-1). Baltimore: Johns Hopkins University, 1988 (software). nutrition in China — present status and changing trend. Biomed Environ
31. Dibley MJ, Goldsby JB, Staehling NW, Trowbridge FL. Development Sci 1996;9:164-80.
of normalized curves for the international growth reference: historical and 43. Huo L. Comparing student growth in Lhasa 1985-1991, ages 7-18:
technical considerations. Am J Clin Nutr 1987;46:736-48. special report. J Res Child Health 1991:1-13. (In Chinese.)
32. Dibley MJ, Staehling NW, Nieburg P, Trowbridge FL. Interpretation 44. Haas JD, Frongillo EA Jr, Stepick CD, Beard JL, Hurtado L. Altitude,
of z-score anthropometric indicators derived from the international growth ethnic and sex differences in birth weight and length in Bolivia. Hum Biol
reference. Am J Clin Nutr 1987;46:749-62. 1980;52:459-77.
33. Kirk RE. Experimental design: procedures for the behavioral sciences. 45. Beall CM. Growth in a population of Tibetan origin at high altitude.
Belmont, Calif.: Brooks/Cole Publishing, 1968. Ann Hum Biol 1981;8:31-8.
34. Trowbridge FL, Marks JS, Lopez de Romana G, Madrid S, Boutton
TW, Klein PD. Body composition of Peruvian children with short stature
and high weight-for-height. II. Implications for the interpretation for Copyright © 2001 Massachusetts Medical Society.
IMAGES IN CLINICAL MEDICINE
The Journal has resumed consideration of new submissions for Images in
Clinical Medicine. Instructions for authors and procedures for submissions
can be found on the Journal’s Web site at www.nejm.org. At the discretion
of the editor, images that are accepted for publication may appear in the
print version of the Journal, the electronic version, or both.
N Engl J Med, Vol. 344, No. 5 · February 1, 2001 · www.nejm.org · 347
You might also like
- A Survey of Undernutrition in Children Under Three Years of Age in Rural Western ChinaDocument10 pagesA Survey of Undernutrition in Children Under Three Years of Age in Rural Western ChinaCherryNo ratings yet
- Rise in Childhood Obesity With Persistently High Rates of Undernutrition Among Urban School-Aged Indo-Asian ChildrenDocument6 pagesRise in Childhood Obesity With Persistently High Rates of Undernutrition Among Urban School-Aged Indo-Asian ChildrenAli HaiderNo ratings yet
- A Study of Protein Energy Malnutrition With Respect To Breast Feeding Practices in Less Than Six Year ChildrenDocument3 pagesA Study of Protein Energy Malnutrition With Respect To Breast Feeding Practices in Less Than Six Year ChildrenMuhamad RockystankiNo ratings yet
- Journal 4Document13 pagesJournal 4intan wahyuNo ratings yet
- Am J Clin Nutr 1981 Butte 2216 28Document13 pagesAm J Clin Nutr 1981 Butte 2216 28Samuel AkrahNo ratings yet
- 206-Article Text-204-1-10-20130822 PDFDocument7 pages206-Article Text-204-1-10-20130822 PDFxSyawx-ONo ratings yet
- 1 PBDocument4 pages1 PBizzul widadNo ratings yet
- Breastfeeding and Mortality Under 2 Years of Age in Sub-Saharan AfricaDocument11 pagesBreastfeeding and Mortality Under 2 Years of Age in Sub-Saharan AfricaMuhammad Arief SaputraNo ratings yet
- Characteristics of Children 2 To 5 Years of Age With Severe ObesityDocument10 pagesCharacteristics of Children 2 To 5 Years of Age With Severe ObesityIvan BurgosNo ratings yet
- Feeding Proem.xDocument4 pagesFeeding Proem.xMuhammad Yusril JalilNo ratings yet
- ArticleDocument8 pagesArticleAstrid Abrahams PakelNo ratings yet
- ResearchDocument10 pagesResearchGildred Rada BerjaNo ratings yet
- Neonatal Mortality, Risk Factors and Causes - A Prospective Population-Based Cohort Study in Urban PakistanDocument7 pagesNeonatal Mortality, Risk Factors and Causes - A Prospective Population-Based Cohort Study in Urban PakistanDavid OlarinloyeNo ratings yet
- Untitled 1Document8 pagesUntitled 1Sri HariNo ratings yet
- Agbedeyi GO, Eke GK, Nte AR - Feeding Pattern of Children in Day Care Centres in Port Harcourt MetropolisDocument4 pagesAgbedeyi GO, Eke GK, Nte AR - Feeding Pattern of Children in Day Care Centres in Port Harcourt MetropolisRenato De Carvalho FerreiraNo ratings yet
- Harry Potter and The Deathly Hallows (Russian)Document5 pagesHarry Potter and The Deathly Hallows (Russian)Te HineahuoneNo ratings yet
- Nutritional Status and Its Relationship With Blood Pressure Among Children and Adolescents in South ChinaDocument7 pagesNutritional Status and Its Relationship With Blood Pressure Among Children and Adolescents in South ChinautarinuNo ratings yet
- Who NeonatalDocument9 pagesWho NeonatalRexy NunuhituNo ratings yet
- Association Between in Utero Organophosphate Pesticide Exposure and Abnormal Reflexes in NeonatesDocument11 pagesAssociation Between in Utero Organophosphate Pesticide Exposure and Abnormal Reflexes in NeonatesJorge Ernesto Garcia JimenezNo ratings yet
- E20151662 FullDocument11 pagesE20151662 FullMichael OlaleyeNo ratings yet
- Congenital Hypothyroidism in The Southern Bangladesh: Original ArticleDocument5 pagesCongenital Hypothyroidism in The Southern Bangladesh: Original ArticleSajjad Hossain ShuvoNo ratings yet
- 06 Original 02Document7 pages06 Original 02normanahmad92No ratings yet
- Bulan Madu Ala IslamDocument7 pagesBulan Madu Ala IslamAsror El-RomlyNo ratings yet
- Wales 2004Document6 pagesWales 2004Subha ManivannanNo ratings yet
- Jafree2015 Factors Associated With Low Birth Weight of Children Among Employed Mothers in PakistanDocument10 pagesJafree2015 Factors Associated With Low Birth Weight of Children Among Employed Mothers in Pakistanwulan raraNo ratings yet
- Anderson Et Al. - 2016 - Indigenous and Tribal Peoples' Health (The Lancet-Lowitja Institute Global Collaboration) A Population StudyDocument27 pagesAnderson Et Al. - 2016 - Indigenous and Tribal Peoples' Health (The Lancet-Lowitja Institute Global Collaboration) A Population StudyLEISY CRUZ RODRIGUEZNo ratings yet
- Stunting, Prevalence, Associated Factors, Wondo Genet, EthiopiaDocument14 pagesStunting, Prevalence, Associated Factors, Wondo Genet, EthiopiaJecko BageurNo ratings yet
- Association of Picky Eating With Growth, Nutritional Status, Development, Physical Activity, and Health in Preschool ChildrenDocument9 pagesAssociation of Picky Eating With Growth, Nutritional Status, Development, Physical Activity, and Health in Preschool Childrenyeremias setyawanNo ratings yet
- The Difference Factors of Underweight Prevalence On Children Underfives Years in Low Poverty AreaDocument10 pagesThe Difference Factors of Underweight Prevalence On Children Underfives Years in Low Poverty AreaXenilitiurahmi RimadeiraniNo ratings yet
- Nutritional Status of Adolescent Girls in Rural Coastal Area of Tangerang DistrictDocument6 pagesNutritional Status of Adolescent Girls in Rural Coastal Area of Tangerang DistrictNoviana ZaraNo ratings yet
- Complementary Feeding and Childhood Adiposity in Preschool-Aged Children in A Large Chinese CohortDocument8 pagesComplementary Feeding and Childhood Adiposity in Preschool-Aged Children in A Large Chinese CohortLinda JajauuooNo ratings yet
- Iajt 00 I 2 P 79Document4 pagesIajt 00 I 2 P 79api-3702148No ratings yet
- 17 Dipendra EtalDocument7 pages17 Dipendra EtaleditorijmrhsNo ratings yet
- 2019 Article 1336Document6 pages2019 Article 1336Eduardo LimaNo ratings yet
- The Relationship of Food Consumption With Nutritional Status of Children Under Two Years at Tolaki Tribe Families in Sub District of AbeliDocument11 pagesThe Relationship of Food Consumption With Nutritional Status of Children Under Two Years at Tolaki Tribe Families in Sub District of AbeliikaNo ratings yet
- Early Childhood Diarrhea Predicts Cognitive Delays in Later Childhood Independently of MalnutritionDocument7 pagesEarly Childhood Diarrhea Predicts Cognitive Delays in Later Childhood Independently of MalnutritionYatil HidayaniNo ratings yet
- Malnutrition Among Under-Five Children of Kadukuruba Tribe: Need To Reach The UnreachedDocument4 pagesMalnutrition Among Under-Five Children of Kadukuruba Tribe: Need To Reach The UnreachedayuNo ratings yet
- Maternal Hypothyroidism During Pregnancy and The Risk of Pediatric Endocrine Morbidity in The OffspringDocument6 pagesMaternal Hypothyroidism During Pregnancy and The Risk of Pediatric Endocrine Morbidity in The OffspringlananhslssNo ratings yet
- Janssen 2016Document6 pagesJanssen 2016Carla VieiraNo ratings yet
- Gender Variance Among Youth With Autism Spectrum Disorders: A Retrospective Chart ReviewDocument7 pagesGender Variance Among Youth With Autism Spectrum Disorders: A Retrospective Chart ReviewMilo DueNo ratings yet
- 1 s2.0 S0140673608614002 Main PDFDocument8 pages1 s2.0 S0140673608614002 Main PDFMarco Andres Moscoso ChavezNo ratings yet
- Lamichhane 2016Document11 pagesLamichhane 2016Emilee Joice Rochelle MalutoNo ratings yet
- Literature ReviewDocument7 pagesLiterature ReviewsarasNo ratings yet
- The Problems of Moderate Preterm Infants: Seminars in PerinatologyDocument4 pagesThe Problems of Moderate Preterm Infants: Seminars in Perinatologysam crushNo ratings yet
- Neonatal Mortality, Risk Factors and Causes: A Prospective Population-Based Cohort Study in Urban PakistanDocument10 pagesNeonatal Mortality, Risk Factors and Causes: A Prospective Population-Based Cohort Study in Urban PakistanchinafiNo ratings yet
- A Study of Community Based Nutritional Intervention and Prevention of MalnutritionDocument8 pagesA Study of Community Based Nutritional Intervention and Prevention of MalnutritionMd UmerNo ratings yet
- Influence of Breast-Feeding On Weight Loss, Jaundice, and Waste Elimination in NeonatesDocument8 pagesInfluence of Breast-Feeding On Weight Loss, Jaundice, and Waste Elimination in NeonatesCristina SánchezNo ratings yet
- qt9gq0c883Document10 pagesqt9gq0c883Ena EppirtaNo ratings yet
- The Normal Anthropometric Measurements For HealthyDocument43 pagesThe Normal Anthropometric Measurements For HealthyAli Mohamed BurhanNo ratings yet
- Nutritional Status and Anemia in Suruí Indian Children, Brazilian AmazonDocument6 pagesNutritional Status and Anemia in Suruí Indian Children, Brazilian AmazonMarinete36No ratings yet
- Health Care in PunoDocument13 pagesHealth Care in Punomario osorioNo ratings yet
- The Health and Well-Being of Adopted ChildrenDocument9 pagesThe Health and Well-Being of Adopted ChildrenAbdi ChimdoNo ratings yet
- Breast vs. Bottle: Differences in The Growth of Croatian InfantsDocument9 pagesBreast vs. Bottle: Differences in The Growth of Croatian InfantsBernadette Grace RetubadoNo ratings yet
- Wellness BehaviourDocument2 pagesWellness BehaviourJohn Paul Ta PhamNo ratings yet
- Journal of Biosocial ScienceDocument14 pagesJournal of Biosocial ScienceOpen mindNo ratings yet
- Congenital Anomalies in Infant With Congenital HypothyroidismDocument4 pagesCongenital Anomalies in Infant With Congenital HypothyroidismAtika SugiartoNo ratings yet
- 1 s2.0 S0033350603001872 MainDocument8 pages1 s2.0 S0033350603001872 MainAybüke ÖztürkNo ratings yet
- JN 214346Document9 pagesJN 214346lada emmanuelNo ratings yet
- Pediatric Dysphagia: Challenges and ControversiesFrom EverandPediatric Dysphagia: Challenges and ControversiesJulina OngkasuwanNo ratings yet
- Evo-Devo of Child Growth: Treatise on Child Growth and Human EvolutionFrom EverandEvo-Devo of Child Growth: Treatise on Child Growth and Human EvolutionNo ratings yet
- Consultation WorksheetDocument4 pagesConsultation WorksheetToni MaddoxNo ratings yet
- Noninvasive Assessment of Hepatic Fibrosis - Overview of Serologic Tests and Imaging Examinations - UpToDateDocument35 pagesNoninvasive Assessment of Hepatic Fibrosis - Overview of Serologic Tests and Imaging Examinations - UpToDatepopasorinemilianNo ratings yet
- A. KMC Introduction Components BenefitsDocument25 pagesA. KMC Introduction Components BenefitsJenness VillanuevaNo ratings yet
- IEP Example ElementaryDocument13 pagesIEP Example ElementaryArthur DumanayosNo ratings yet
- Skills For An InterviewDocument5 pagesSkills For An InterviewAkhwand SaulatNo ratings yet
- Violeta Vs Insular LifeDocument2 pagesVioleta Vs Insular LifeajdgafjsdgaNo ratings yet
- Notarized Affidavit of Religious Belief For Exemption From COVID VaccinationDocument3 pagesNotarized Affidavit of Religious Belief For Exemption From COVID VaccinationAshishNo ratings yet
- Week 7 (March 22-26, 2021)Document2 pagesWeek 7 (March 22-26, 2021)Achievers IntelligencesNo ratings yet
- BLS IntroductionDocument28 pagesBLS IntroductionMUKESH SUNDARARAJANNo ratings yet
- (Routledge Anthropology Handbooks) Lenore Manderson (Editor), Elizabeth Cartwright (Editor), Anita Hardon (Editor) - The Routledge Handbook of Medical Anthropology-Routledge (2016)Document424 pages(Routledge Anthropology Handbooks) Lenore Manderson (Editor), Elizabeth Cartwright (Editor), Anita Hardon (Editor) - The Routledge Handbook of Medical Anthropology-Routledge (2016)Phuong HaNo ratings yet
- CDT Ipsita Paikaray. Od-19-Sw-A-304-336. The Role of NCC in Covid-19Document4 pagesCDT Ipsita Paikaray. Od-19-Sw-A-304-336. The Role of NCC in Covid-19Ē Vì LNo ratings yet
- Pengaruh Terapi Bermain Ular Tangga Terhadap Kecemasan Pasien Anak Usia PraschoolDocument9 pagesPengaruh Terapi Bermain Ular Tangga Terhadap Kecemasan Pasien Anak Usia PraschoolSulfa Afiat storeNo ratings yet
- Medication-Assisted Treatment (MAT) in The Emergency DepartmentDocument79 pagesMedication-Assisted Treatment (MAT) in The Emergency DepartmentPedro Carlos Martinez SuarezNo ratings yet
- Manila Emergency HotlinesDocument2 pagesManila Emergency HotlinesHarlem AgnoteNo ratings yet
- 2019 GLFVM - Marathon Quest For Improvement ProgramDocument7 pages2019 GLFVM - Marathon Quest For Improvement Programapi-200426445No ratings yet
- Abuses of Children in ClassroomDocument120 pagesAbuses of Children in ClassroomJulius de la CruzNo ratings yet
- Common Tools and Equipment in Taking Vital Sign Thermometer: Lesson 3Document3 pagesCommon Tools and Equipment in Taking Vital Sign Thermometer: Lesson 3Skye CheonNo ratings yet
- Cappa-Enit12-r01-A4fr SM Ez Eur BioairDocument187 pagesCappa-Enit12-r01-A4fr SM Ez Eur Bioairaldo giovNo ratings yet
- Milk and Dairy Products EngDocument2 pagesMilk and Dairy Products EngSar OyaNo ratings yet
- Wilkins Clinical Assessment in Respiratory Care 7th Edition by Heuer - Test BankDocument37 pagesWilkins Clinical Assessment in Respiratory Care 7th Edition by Heuer - Test BankalishcathrinNo ratings yet
- Clean Up and Flourish or Pile Up and PerishDocument30 pagesClean Up and Flourish or Pile Up and Perishnehabhilare100% (1)
- Life Span - ReadingsDocument37 pagesLife Span - ReadingsSarozNo ratings yet
- In The Supreme Court of Bermuda: Civil Jurisdiction 2021: No. 162Document38 pagesIn The Supreme Court of Bermuda: Civil Jurisdiction 2021: No. 162BernewsAdminNo ratings yet
- Abnormal Psychology 6th Edition Nolen-Hoeksema Solutions Manual 1Document36 pagesAbnormal Psychology 6th Edition Nolen-Hoeksema Solutions Manual 1jonathanjohnsongfbykwatdc100% (23)
- Study Instruments For 13/14 Year Olds: 7.1 Instructions For Completing Questionnaire and Demographic QuestionsDocument11 pagesStudy Instruments For 13/14 Year Olds: 7.1 Instructions For Completing Questionnaire and Demographic QuestionsNur Hidayati AzharNo ratings yet
- 1-Hemorrage in Oral SurgeryDocument31 pages1-Hemorrage in Oral SurgeryrayaimNo ratings yet
- Files 1673253509Document150 pagesFiles 1673253509Indri Wulandari99No ratings yet
- Col Zulfiquer Ahmed Amin: M Phil (HHM), MPH (HM), PGD (Health Economics), MBBS Armed Forces Medical Institute (AFMI)Document60 pagesCol Zulfiquer Ahmed Amin: M Phil (HHM), MPH (HM), PGD (Health Economics), MBBS Armed Forces Medical Institute (AFMI)Manav Suman SinghNo ratings yet
- Policy Remit 1 - Review of NZNO Strategies For Safe StaffingDocument3 pagesPolicy Remit 1 - Review of NZNO Strategies For Safe StaffingGrant BrookesNo ratings yet
- Authorized Test Center - Policies and Procedures PDFDocument365 pagesAuthorized Test Center - Policies and Procedures PDFNarra Venkata KrishnaNo ratings yet