Professional Documents
Culture Documents
Alteration in Ventilatory
Uploaded by
jay camille buhanginOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alteration in Ventilatory
Uploaded by
jay camille buhanginCopyright:
Available Formats
Alteration in Ventilatory
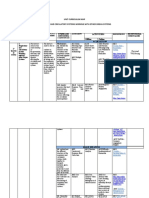
NCM 118
Respiratory Problems
Parameters
- Manifest coughing (facilitates removal of secretion or any foreign materials from the
tracheobronchial tree in the lungs)
- Problem in RR (tachypnea/tachycardia)
- Oxygen Saturation
- Cyanosis (hemoglobin is reduced to 5mg/dl or more)
o Peripheral cyanosis – normal torso but peripheries (extremities and nail beds) have
bluish discoloration Acrocyanosis – in newborn
o Central Cyanosis – bluish discoloration of the lips, mucus membrane, face, tongue and
always a pathologic (there is always an underlying problem such as heart problem)
- Dyspnea – difficulty of breathing
o Ask what was the task done, time, duration (after a rest, min)
- Abnormal breath sound upon auscultation
o Adventitious breath sound
o Rales, crackles, Ronchi, wheezing, friction rub
- Breathing problems
- Ask patient for presence of sputum/phlegm
o Sputum – secretion that came from tracheobronchial tree from mouth, pharynx, nose
and sinuses
o Phlegm – secretion of tracheobronchial tree and lungs and a healthy adult has a volume
of 100 ml for 24 hours
- Color of secretion
o Yellow/green – bacterial
o White – viral infection
DIAGNOSTIC ASSESSMENT
- Bronchoscopy – to check for the presence of mass
- Sputum Examination – best time for sputum examination is during morning
o Acid-fast bacilli smear- microscopic examination of a person's sputum or other specimen
that is stained to detect acid-fast bacteria. To check for presence of tubercle bacilli
- Spirometry – form of exercise and observation for post-covid
- Mantoux test – ID route, to check if patient is exposed to pulmonary tuberculosis, 48/72 hours
- Bronchogram – radiopaque dye
- ABG – identify acid base status of the patient
- CHEST X-Ray – to check for pneumonia, atelectasis, tumor
- Pulse oximetry – 98-100% good O2 sat
Chronic Obstructive Pulmonary Disease (COPD) /Chronic Airflow Limitation (CAL)
- Chronic – matagal na
- Considered as irreversible
- Chronic-Airflow Limitation (CAL)
- Characterized bby airflow limitation that is not fully reversible
- Progressive and inflammatory
Alteration in Ventilatory
NCM 118
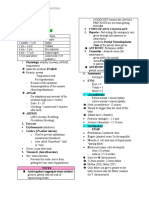
-Number 1 Etiology is cigarette smoking
-2 types of COPD/CAL
o Chronic bronchitis
Productive cough that lasts at least 3 months in each 3 consecutive years
Causes: cigarette smoking, environmental pollutant (urban/cities), occupational
exposure to hazardous airborne substances.
Inflammation of lung parenchyma and fibrotic changes in lung airways
There will be narrowing of airway which is irreversible leading to emphysema
and bronchiectasis (asthma is reversible)
Hypersecretion of mucus
o Emphysema
Presence of overdistended nonfunctional alveoli which may rupture which may
cause to
Causes: cigarette smoking
There is destruction of elastic recoil (inflate/deflate) resulting to retention of
carbon dioxide causing to hypoxia and respiratory acidosis
- MANIFESTATIONS
o Cough – due to inflammation which can lead to edema of mucus membrane
(hypersecretion of mucus) persistent cough
o Dyspnea
o Chest pain
o Adventitious breath sound (wheezing due to narrowing of airway)
Pursed lip breathing – allows pt to have carbon dioxide elimination
o Alteration in the level of consciousness (low oxygen going to the brain)
o Cyanosis
o Voice changes
o Clubbing of fingers – due to poor perfusion
o Polycythemia – low 02 levels triggers the production of erythropoietin in the kidneys.
Happen also to patient with cardiac problems. Compensatory mechanism for low
perfusion
MANAGEMENT
- Rest – reduce o2 demand of tissues
- Increase fluid intake – to liquify mucus secretion
- Good oral care – to remove sputum and prevent infection
- DIET:
o high calorie (source of energy),
o high protein (helps to maintain the integrity of alveoli walls due to overdistention or loss
of elasticity of alveoli),
o low carbohydrates (it limits carbon dioxide production because carbon is end product
metabolism of carbohydrates
- Oxygen therapy (1-3 L/min) safest is 2L/ min
o It may not trigger the hypoxic drive
- Smoking cessation is the single most and cost-effective prevention and risk of COPD
PHARMACOTHERAPY
Alteration in Ventilatory
NCM 118
- Mucolytic – liquify the secretions
o Examples: Ambroxol, mucomyst, carbocisteine
o Given in the morning, do not give at night because pt may cough overnight
- Antitussive
o Cough suppressant
o Given at night to nut disturb
o Robitussin, dextrometorphan, codaine
o Can cause drowsiness
o Avoid activities with mental stimulation (driving)
o Decrease peristalsis causing constipation (Codaine)
- Bronchodilators
o Aminophylline, Ventolin, Salbutamol
o Dilates the bronchioles – increases the diameter of bronvhioles
- Antimicrobials
- Steroids
o For anti-inflammatory effects
You might also like
- PN21 Health and Healing - Pre-Class Activities - Test 2 PDFDocument33 pagesPN21 Health and Healing - Pre-Class Activities - Test 2 PDFRachel HomesNo ratings yet
- Essentials of Human Diseases and Conditions Unit 1 OutlineDocument7 pagesEssentials of Human Diseases and Conditions Unit 1 Outlinecindyfuller68No ratings yet
- Regional Obstetric Early Warning Score ChartDocument2 pagesRegional Obstetric Early Warning Score ChartDaeng Farahnaz100% (2)
- Respiratory Nursing #1Document19 pagesRespiratory Nursing #1shenric16100% (12)
- Med Surge 2 - RESP SYSTEM NOTESDocument26 pagesMed Surge 2 - RESP SYSTEM NOTESlorrainenxumalo75% (4)
- Veterinary Drug FormularyDocument87 pagesVeterinary Drug FormularyAklilu AsmelashNo ratings yet
- Chapter 27Document6 pagesChapter 27monster40lbsNo ratings yet
- Medical Surgical (MS) Rle Pulmonary/ Lung AssessmentDocument8 pagesMedical Surgical (MS) Rle Pulmonary/ Lung AssessmentYman Gio BumanglagNo ratings yet
- Normal Changes of AgingDocument9 pagesNormal Changes of AgingGiselle EstoquiaNo ratings yet
- Tina ThankachanDocument50 pagesTina ThankachanBharat JamodNo ratings yet
- The Process of OxygenationDocument7 pagesThe Process of OxygenationMich CercadoNo ratings yet
- Interventions To Promote OxygenationDocument19 pagesInterventions To Promote OxygenationMary Ann SacramentoNo ratings yet
- Copd 555Document79 pagesCopd 555ikram ullah khanNo ratings yet
- CODPDocument34 pagesCODPNeeraja M SureshNo ratings yet
- Onchi & CopdDocument8 pagesOnchi & CopdAngellene GraceNo ratings yet
- Scenario 5: Group 6Document51 pagesScenario 5: Group 6Gd SuarantaNo ratings yet
- Prelims Oxygenation Handout#2Document5 pagesPrelims Oxygenation Handout#2ApRil Anne BalanonNo ratings yet
- RespiratoryDocument31 pagesRespiratoryRebecca Hughes100% (4)
- Acute & Chronic Bronchitis & COPDDocument49 pagesAcute & Chronic Bronchitis & COPDHendraDarmawanNo ratings yet
- The Process of OxygenationDocument5 pagesThe Process of Oxygenationapi-3744683100% (3)
- Patho Respiratory - KatherineDocument9 pagesPatho Respiratory - KatherineKayla MayerNo ratings yet
- Pulmonary FailureDocument29 pagesPulmonary FailureWengel RedkissNo ratings yet
- Patofisiologi Batuk: Risna Halim Bagian Ilmu Penyakit Dalam Universitas HasanuddinDocument28 pagesPatofisiologi Batuk: Risna Halim Bagian Ilmu Penyakit Dalam Universitas HasanuddinSitti Nur FadillahNo ratings yet
- Passive Smoking: CarcinogensDocument3 pagesPassive Smoking: Carcinogensapi-296833859No ratings yet
- Week 3 Obstructive DisorderDocument79 pagesWeek 3 Obstructive Disorderdelrosariojm87No ratings yet
- CopdDocument4 pagesCopdapi-3739910100% (2)
- What Went Wrong?: Acute Respiratory Distress Syndrom (Ards)Document6 pagesWhat Went Wrong?: Acute Respiratory Distress Syndrom (Ards)niki estuNo ratings yet
- ARDSDocument53 pagesARDSrani asfiyaNo ratings yet
- DR M Ushashree 1 Yr PG Gandhi Medical CollegeDocument58 pagesDR M Ushashree 1 Yr PG Gandhi Medical CollegeRaghu NadhNo ratings yet
- LaryngitisDocument9 pagesLaryngitisjonna casumpangNo ratings yet
- Respiratory SystemDocument19 pagesRespiratory Systemtheodore_estradaNo ratings yet
- Copd 200412082048Document139 pagesCopd 200412082048Richard ArceNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument23 pagesChronic Obstructive Pulmonary Diseasev_vijayakanth7656No ratings yet
- Interventions For Critically Ill Patients With Respiratory Problems HandoutsDocument115 pagesInterventions For Critically Ill Patients With Respiratory Problems HandoutsDemuel Dee L. BertoNo ratings yet
- COPD:RLDDocument11 pagesCOPD:RLDKhiara Yapha AlfarNo ratings yet
- Chapter 2 Respiratory AssessmentDocument9 pagesChapter 2 Respiratory AssessmentKathleen Dela CruzNo ratings yet
- Reviewer For Management of Common IllnessDocument27 pagesReviewer For Management of Common Illnessmarie vennis hamchawanNo ratings yet
- Sistem PernafasanDocument87 pagesSistem Pernafasantaufik HidayatNo ratings yet
- Respi Anaphy Day 1Document128 pagesRespi Anaphy Day 1Tracy Megan RusillonNo ratings yet
- Chronic Obstructive Pulmonary Disease: Christine Loren T. Laya BSN 3-1Document41 pagesChronic Obstructive Pulmonary Disease: Christine Loren T. Laya BSN 3-1Kristine CastilloNo ratings yet
- CH 25 Respiratory AssessmentDocument14 pagesCH 25 Respiratory Assessmentهدوء النسمةNo ratings yet
- COPDDocument73 pagesCOPDBroken OreosNo ratings yet
- Oxygenation NotesDocument23 pagesOxygenation NoteschikaycNo ratings yet
- Mechanical IntubationDocument5 pagesMechanical IntubationBAILEN AYNNA PEARLNo ratings yet
- Slides. Disturbances in Oxygen Utilization 2 1Document101 pagesSlides. Disturbances in Oxygen Utilization 2 1SHARMAINE ANNE POLICIOSNo ratings yet
- Nursing Management of Patient With Respiratory ProblemsDocument151 pagesNursing Management of Patient With Respiratory ProblemsAbirajan100% (2)
- Obstructive DisordersDocument23 pagesObstructive DisordersMartha ChaseNo ratings yet
- Nursing Care Management - 112Document67 pagesNursing Care Management - 112Ong KarlNo ratings yet
- Epidemiology: Several Diseases Airflow ObstructionDocument11 pagesEpidemiology: Several Diseases Airflow ObstructionBharat Singh BanshiwalNo ratings yet
- Patholpgic Change in EmphysemiaDocument16 pagesPatholpgic Change in Emphysemiafenil1194No ratings yet
- COPDDocument6 pagesCOPDAubrey PerezNo ratings yet
- Resp Lecture NotesDocument18 pagesResp Lecture Notessurviving nursing schoolNo ratings yet
- Respiratory DisordersDocument18 pagesRespiratory Disordersjdigal100% (4)
- Resp Medicine NotesDocument95 pagesResp Medicine Noteshugolucas182100% (1)
- Chronic Obstructive Pulmonary DiseaseDocument48 pagesChronic Obstructive Pulmonary DiseaseddallasNo ratings yet
- Gagal Nafas & Kedaduratan Sis - RespDocument53 pagesGagal Nafas & Kedaduratan Sis - Respthe_jokosNo ratings yet
- Case Discussion - CopdDocument63 pagesCase Discussion - CopdrajeshNo ratings yet
- Biochemical Case 1Document2 pagesBiochemical Case 1Affie SaikolNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to the Asthma and Lung DiseasesFrom EverandA Simple Guide to the Asthma and Lung DiseasesRating: 5 out of 5 stars5/5 (1)
- Pedia TranscriptDocument18 pagesPedia TranscriptUma CrespoNo ratings yet
- 10 1016@j Cmi 2019 12 013Document25 pages10 1016@j Cmi 2019 12 013akuNo ratings yet
- Role of Mother Tincture in OncologyDocument4 pagesRole of Mother Tincture in OncologyEditor IJTSRD100% (1)
- Vac CertDocument4 pagesVac Certnewyoke3No ratings yet
- RITE Practice QuestionsDocument28 pagesRITE Practice QuestionsDesiree Mejica100% (2)
- Thesis PresentationDocument44 pagesThesis Presentationberhe59076362No ratings yet
- Mitral Stenosis: Mustafizul Aziz Assistant Professor NicvdDocument42 pagesMitral Stenosis: Mustafizul Aziz Assistant Professor NicvdNavojit ChowdhuryNo ratings yet
- Aero-Digestive & Respiratory Changes Post TraheostomyDocument36 pagesAero-Digestive & Respiratory Changes Post Traheostomyrahaf abusalahNo ratings yet
- Approach To Respiratory Distress in NewbornDocument79 pagesApproach To Respiratory Distress in NewbornNikhil100% (1)
- Biting Activities of Filariasis Vector Mosquitoes in Buton District (Full Paper - Final Revised)Document12 pagesBiting Activities of Filariasis Vector Mosquitoes in Buton District (Full Paper - Final Revised)sri wahyuniNo ratings yet
- (Cô Vũ Mai Phương) Tài liệu LIVESTREAM - Tổng ôn 2 tuần cuối - Chủ đề nóng Covid 19Document3 pages(Cô Vũ Mai Phương) Tài liệu LIVESTREAM - Tổng ôn 2 tuần cuối - Chủ đề nóng Covid 19Mon MonNo ratings yet
- Cancer of The LarynxDocument16 pagesCancer of The Larynxhelaley_1983No ratings yet
- Workbook of 5 Day ProgramDocument49 pagesWorkbook of 5 Day Programchetan sharmaNo ratings yet
- OSCE Checklists (History and Examination)Document33 pagesOSCE Checklists (History and Examination)Waleed MohmmedNo ratings yet
- INFECTION Control and PREVENTION-1Document49 pagesINFECTION Control and PREVENTION-1Jerry AbleNo ratings yet
- Goboy - Risk For Infection NCPDocument3 pagesGoboy - Risk For Infection NCPLouise GermaineNo ratings yet
- Nephrotic SyndromeDocument56 pagesNephrotic Syndromeapi-19916399No ratings yet
- Endocrine Hypothyroidism HyperthyroidismDocument16 pagesEndocrine Hypothyroidism HyperthyroidismJeel MohtaNo ratings yet
- Triple Warmer Meridian Acupoint Chart PDFDocument1 pageTriple Warmer Meridian Acupoint Chart PDFVicaas VSNo ratings yet
- 18 Hematological Conditions in NewbornDocument25 pages18 Hematological Conditions in NewbornRana VandanaNo ratings yet
- APA Draft Practice Guidelines Eating DisordersDocument139 pagesAPA Draft Practice Guidelines Eating DisordersGaby ZavalaNo ratings yet
- Immunization Decline CASE STUDYDocument9 pagesImmunization Decline CASE STUDYRon Isabelle D. TabelonaNo ratings yet
- Exfoliative Cytology PatDocument29 pagesExfoliative Cytology PatAly Bint Smbs100% (1)
- Canine Parvovirus Fact Sheet 2018-07-0Document5 pagesCanine Parvovirus Fact Sheet 2018-07-0WDIV/ClickOnDetroitNo ratings yet
- Grade 9 Curriculum MapDocument4 pagesGrade 9 Curriculum MapZnar nabinagnap100% (1)
- Thromboangiitis ObliteransDocument5 pagesThromboangiitis Obliteransklinik mandiriNo ratings yet
- Adhd NCPDocument2 pagesAdhd NCPGooph Buster83% (6)