Professional Documents
Culture Documents
Dr. A. Samy TAG Bone Diseases - 1
Uploaded by
Herato MenaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dr. A. Samy TAG Bone Diseases - 1
Uploaded by
Herato MenaCopyright:
Available Formats
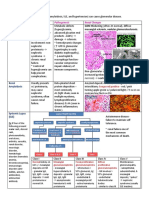
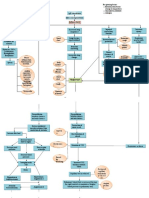
Nutritional Rickets (Vit D-Deficiency) Osteomalacia Osteoporosis
- Age-related decrease in bone mass 2ry to uncoupling of
- Defect in mineralization of osteoid matrix caused by inadequate - Defect in mineralization of osteoid matrix caused by inadequate Ca &
osteoclast-osteoblast activity & disrupted microarchitecture:
Ca & Ph before physeal closure Ph After physeal closure
Postmenopausal 50-70 yrs (Type 1) - Senile > 70 yrs (Type 2)
Risk Factors:
1. ↓ dietary intake of Vit D 4. Hypophosphatemia 1. Age
1. ↓ dietary intake of Vit D 2. Malabsorption syndromes 5. Chronic alcoholism 2. Endocrine abnormality
2. Malabsorption syndromes 3. Renal osteodystrophy 6. Tumor-induced osteomalacia 3. Idiopathic
3. Chronic parenteral nutrition 4. Inactivity
4. Premature infants 7. Drugs associated é Vit D deficiency: Phenytoin, Phenobarbital, 5. Chronic alcoholism
Rifampin & Glucocorticoids 6. Calcium deficiency
Pathophysiology:
- ↓Vit D levels lead to ↓intes nal absorp on of Ca - ↓Vit D levels lead to ↓intes nal absorp on of Ca - Quantitative, not qualitative disorder of bone mineralization 2ry
- ↓ Ca levels leads to a compensatory ↑ PTH & bone resorption - ↓ Ca levels leads to a compensatory ↑ PTH & bone resorption to uncoupling of osteoclast-osteoblast activity & disrupted
- Bone resorption leads to ↑ Alkaline phosphatase levels - Bone resorption leads to ↑ Alkaline phosphatase levels microarchitecture
C/P:
1. Generalized muscular hypotonia 1. Generalized bone & muscle pain 1. Fragility #s: Pain & tenderness at fracture site
2. Frontal bossing & delays í closure of í anterior fontanelle. 2. Long bones, ribs & vertebrae #s 2. Kyphotic deformity can arise from verteberal body #s
3. Lower limb deformities: Bowlegs, knock-knees or Windswept. 3. Proximal muscle weakness 3. Pelvic ring insufficiency #s
4. Rachitic rosary: Prominent rib heads at í osteochondral junction 4. Fatigue
5. Harrison sulcus (Flaring over í diaphragm) & Pot belly 5. Waddling gait: due to hip pain & thigh weakness
6. Sternum may be pulled into a pigeon-breast deformity. 6. Difficulty rising from chair & climbing stairs
7. Kyphoscoliosis.
8. Joint Swelling around í ankle, wrist & elbows.
9. Dental disease
Imaging:
1. Physeal widening - Radiology: - Radiology: usually not helpful unless > 30% bone loss
2. Metaphyseal cupping 1. Fractures (Appendicular # predominance) 1. Fractures (Axial # predominance)
3. Decreased bone density 2. Looser's zones (Pseudo#): Medial femoral cortex & pubic ramus 2. Thinned cortices
4. Looser's zones: Pseudo# on í compression side of bone 3. Biconcave vertebral bodies 3. Loss of trabecular bone
5. Rachitic rosary: Prominent rib heads at í osteochondral junction 4. Trefoil pelvis 4. Kyphosis
6. Bowing (Often genu varum) 5. Protrusio acetabuli 5. Codfish vertebra
7. Codfish vertebrae - Bone scan: ↑ Activity - Dexa Scan: Measures BMD & compiles scores - Most accurate
Investigations:
- ↓ Vit D - ↓ Vit D - Normal Vit D
- ↑ Alkaline Phosphatase - ↑ Alkaline Phosphatase
- ↓ to Normal Serum Ca - ↓ Serum Ca - Normal Serum Ca & Ph
- ↑ PTH - ↑ PTH
- ↓ Serum Ph - ↓ Serum Ph - Normal Alkaline Phosphatase & PTH
Treatment:
1. Bisphosphonates: 1st line therapy
- Vit D: Daily dosage differs from 2000 - 5000 IU for 4-6 wks (till 2. Ca & Vit D: Px 1200 to 1500 mg/d Ca & 800 -1000 IU Vit D
- Large doses of oral Vit D (1000 IU/day), treat underlying cause
gaining therapeutic effect) then maintenance dose 500 IU daily 3. Estrogen replacement therapy: Postmenopausal osteoporosis
- Patients é renal disease : Supplement 1,25(OH)2 Vit D
for 3 yrs 4. Calcitonin, Raloxifene (Evista), Teriparatide (Forteo),
Denosumab (Prolia)
Dr. A. Samy TAG Bone Diseases | 1
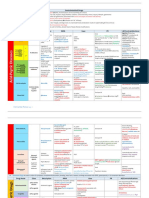
Hyperparathyroidism
Definition: Increased PTH production that may be of 1ry, 2ry or 3ry causes
Epidemiology: Pathophysiology: Associated conditions:
- 0.1% of í population - PTH indirectly stimulates osteoclasts by binding to its receptor on osteoblasts, inducing RANK-L & - Brown tumor: resembles a giant cell tumor of bone relating
- ♀> ♂ M-CSF synthesis to focal demineralization of bone in í setting of
- 90% result from a single adenoma - Excessive PTH leads to over-stimulation of bone resportion: Cortical bone > Cancellous bone hyperparathyroidism.
- 10% from parathyroid hyperplasia - Hyperparathyroidism & malignancy make up í majority of patients é hypercalcemia
Classification: Serum Ca Serum Ph Serum PTH
- Caused by hypersecretion of PTH by a Parathyroid adenoma or hyperplasia
Primary: ↑ ↓ ↑
- May result in Osteitis Fibrosa Cystica: Breakdown of bone, predominently subperiosteal bone, commonly involves í jaw
- Caused as a compensation from hypocalcemia (↓ gut Ca absorp on) or hyperphosphatemia (↑ Phosphorous)
Secondary: - Chronic renal disease: Causes hypovitaminosis D → leads to ↓ Ca absorption Normal or ↓ ↑ ↑
- Associated conditions:
- Renal Osteodystrophy: Bone lesions due to 2ry hyperparathyroidism
Tertiary: - Parathyroid glands become dysregulated after 2ry hyperparathyroidism (Secrete PTH regardless of Ca level) ↑ ↑ ↑
C/P: Investigation:
- Often asymptomatic Serology:
- Bone pain - 1ry: ↑ Ca & ↑ PTH
- Constipations - 2ry: ↓ Ca / Normocalcemia & ↑ PTH
- Weakness - Malignancy: ↓ PTH & ↑ Alkaline Phosphatase
- Kidney stones Urinalysis:
- Uncommon cause of 2ry hypertension - 1ry: Hypercalciuria (Renal stones) & ↑ cAMP
Radiograph:
- Cystic bone spaces (Salt & Pepper) Often in í skull
- Loss of phalange bone mass (↑ concavity)
- Brown Tumors
Treatment:
- Acute hypercalcemia: IV fluids + Loop diuretics
- Symptomatic hypercalcemia: Treated surgically é Parathyroidectoy
- Complications include Post-op hypocalcemia
- Manifests as numbness, tingling & muscle cramps
- Should be treated é IV calcium gluconate
Complications:
- Peptic ulcer disease: ↑ gastrin produc on s mulated by ↑ Ca
- Acute pancreatitis: ↑ lipase ac vity s mulated by ↑ Ca
- CNS dysfunction: Anxiety, confusion & coma result of metastatic calcification of í brain
- Osteoporsis: Bone loss occurs as result of bone resorption due to excess PTH
Dr. A. Samy TAG Bone Diseases | 1
You might also like
- MS General Surgery Question BankDocument98 pagesMS General Surgery Question BankPrashant Singh100% (10)
- Family Medicine NotesDocument32 pagesFamily Medicine Noteslalee704100% (8)
- Spine PDFDocument7 pagesSpine PDFDRAHMEDFAHMYORTHOCLINIC100% (1)
- Endocrine 50 Questions & AnswersDocument28 pagesEndocrine 50 Questions & AnswersBrooke Susac100% (1)
- Sanjay Sharma's Notes For MRCPDocument7 pagesSanjay Sharma's Notes For MRCPMoe Zaw Lin100% (2)
- 4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangDocument4 pages4.1d - Pathology of The Pituitary - Nov.10 - Dr. GalangMiel Raphael AranillaNo ratings yet
- Diseases - BiochemDocument4 pagesDiseases - BiochemJay FeldmanNo ratings yet
- LeukemiaDocument2 pagesLeukemiaAyeshaArifNo ratings yet
- Toxicology USMLE NotesDocument15 pagesToxicology USMLE NotesDuncan JacksonNo ratings yet
- Week 7. Renal Pathology Continued.Document9 pagesWeek 7. Renal Pathology Continued.Amber LeJeuneNo ratings yet
- Acute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmDocument1 pageAcute Myeloproliferative Acute Lymphoproliferative Chronic Myeloproliferative Chronic Lymphoproliferative Plasma Cell NeoplasmAudreySlitNo ratings yet
- Clinical Medicine - Lecture: - Topic: - DateDocument3 pagesClinical Medicine - Lecture: - Topic: - DateqselmmNo ratings yet
- Pharmacology TableDocument9 pagesPharmacology TableMaryam KhushbakhatNo ratings yet
- Pathogens of The Vagina-Annie Espinosa - This Is The Revised VersionDocument1 pagePathogens of The Vagina-Annie Espinosa - This Is The Revised VersionMicroposterNo ratings yet
- Table of Genetic DisordersDocument3 pagesTable of Genetic DisordersEliNo ratings yet
- Cocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeDocument2 pagesCocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeKimberly KanemitsuNo ratings yet
- Test LFTsDocument2 pagesTest LFTsostarburstoNo ratings yet
- OPTOMED-HW2-Diabetic Retinopathy PDFDocument3 pagesOPTOMED-HW2-Diabetic Retinopathy PDFDanalie SalvadorNo ratings yet
- Small Intestine 01 PDFDocument9 pagesSmall Intestine 01 PDFfadoNo ratings yet
- Genitourinary System: Renal FailureDocument6 pagesGenitourinary System: Renal FailureEn ConejosNo ratings yet
- First Aid PharmacoDocument61 pagesFirst Aid PharmacogirNo ratings yet
- Ninja On Fleek - Fern Charts MT2 SLAY Most UpdatedDocument56 pagesNinja On Fleek - Fern Charts MT2 SLAY Most UpdatedyenniNo ratings yet
- Antivirals, Rubella, Peecorna VIRUSDocument3 pagesAntivirals, Rubella, Peecorna VIRUSErnie G. Bautista II, RN, MDNo ratings yet
- Patho Common Stuff - RobbinsDocument7 pagesPatho Common Stuff - RobbinsMaf BNo ratings yet
- ENDOCRINE PATHOLOGY WebpathDocument35 pagesENDOCRINE PATHOLOGY Webpathapi-3766657No ratings yet
- Anemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDocument15 pagesAnemia Type Pathogenesis Clinical Manifestations Diagnosis Peripheral Blood Lab FindingsDanielle FosterNo ratings yet
- Nephrotic Nephritic SyndromsDocument4 pagesNephrotic Nephritic SyndromsKimiwari100% (2)
- Genetic Disorders-Www - Qworld.co - inDocument13 pagesGenetic Disorders-Www - Qworld.co - inQworld100% (1)
- Cardio Block 3Document62 pagesCardio Block 3Maya LaPradeNo ratings yet
- Antifungal Agents: EchinocandinsDocument2 pagesAntifungal Agents: EchinocandinsCourtney TownsendNo ratings yet
- DNA Viruses: P P P A H H PDocument2 pagesDNA Viruses: P P P A H H PKimberly KanemitsuNo ratings yet
- Pharmacology Main DrugsDocument14 pagesPharmacology Main DrugsSabir KhanNo ratings yet
- Pharmayield: Must Know Pharmacology NotesDocument2 pagesPharmayield: Must Know Pharmacology NotesBianca Desiree VergaraNo ratings yet
- Table of Genetic DisordersDocument9 pagesTable of Genetic DisordersjeslymailNo ratings yet
- Classification of The Epilepsies: Purpose: For Clinical DiagnosisDocument25 pagesClassification of The Epilepsies: Purpose: For Clinical Diagnosisayu rifqiNo ratings yet
- Step 1 DrugsDocument46 pagesStep 1 DrugsZebram ZeeNo ratings yet
- Bipolar Disorder Background: Hypomania Has The Same Symptoms of Mania Without Psychotic SymptomsDocument2 pagesBipolar Disorder Background: Hypomania Has The Same Symptoms of Mania Without Psychotic SymptomshumdingerNo ratings yet
- Chart - WBC DisordersDocument1 pageChart - WBC DisordersSamuel RothschildNo ratings yet
- General Pathology 4.03 Endocrine System Super SummaryDocument15 pagesGeneral Pathology 4.03 Endocrine System Super SummaryJade MonrealNo ratings yet
- Systemic Effects of Inflammation The Acute Phase ResponseDocument3 pagesSystemic Effects of Inflammation The Acute Phase ResponseJenward Hostallero100% (1)
- Haematology-Summary My NotesDocument24 pagesHaematology-Summary My NotesToria053No ratings yet
- Gene Related DiseaseDocument3 pagesGene Related Diseasevivek govardhanamNo ratings yet
- 7sgdfgf PDFDocument438 pages7sgdfgf PDFPratik JadhavNo ratings yet
- Chapter 3 Genetic VariationDocument21 pagesChapter 3 Genetic VariationAbdulkarimNo ratings yet
- Bone TumorsDocument2 pagesBone TumorsDrashty DesaiNo ratings yet
- GI + Renal OSCE: AMSA Edinburgh X IMU Y4Document41 pagesGI + Renal OSCE: AMSA Edinburgh X IMU Y4Abby LiewNo ratings yet
- Mnemonic of Some Rare Genetic Disease PDFDocument9 pagesMnemonic of Some Rare Genetic Disease PDFfaraz100% (1)
- ChemotherapyDocument11 pagesChemotherapyNedaAbdullahNo ratings yet
- SketchyPath ChecklistDocument1 pageSketchyPath ChecklistFajar Raza100% (1)
- Pharm TableDocument35 pagesPharm TableHannah BaldwinNo ratings yet
- Antimycobacterial Drugs PDFDocument3 pagesAntimycobacterial Drugs PDFCas BuNo ratings yet
- 1 Ge Stimulations Mast Cell Degeneration Asthma AttackDocument4 pages1 Ge Stimulations Mast Cell Degeneration Asthma Attacknebbie06No ratings yet
- Breast CancerDocument6 pagesBreast Cancersarguss14No ratings yet
- Parkinson's Disorder - Classification and MechanismDocument1 pageParkinson's Disorder - Classification and MechanismVương TúNo ratings yet
- Respiratory Tract InfectionsDocument1 pageRespiratory Tract InfectionsShannon RamsumairNo ratings yet
- Semester 2 Drug ListDocument7 pagesSemester 2 Drug ListNam_Pham_6481No ratings yet
- Hi Stop Hath Ology 2Document22 pagesHi Stop Hath Ology 2vivek govardhanamNo ratings yet
- GI Diarrheal Micro ChartDocument3 pagesGI Diarrheal Micro ChartEvan MillerNo ratings yet
- Kidney NewDocument4 pagesKidney NewParth BhayanaNo ratings yet
- Retinoblastoma Cognitive Concept Map - DR Kumar Ponnusamy and DR Jegathambigai RN - Problem Based Learning (PBL) For Large Groups Medical StudentsDocument1 pageRetinoblastoma Cognitive Concept Map - DR Kumar Ponnusamy and DR Jegathambigai RN - Problem Based Learning (PBL) For Large Groups Medical StudentsPonnusamy Kumar100% (1)
- Neurology Musculoskeletal (MedicalBooksVN - Com)Document4 pagesNeurology Musculoskeletal (MedicalBooksVN - Com)Jonathan AiresNo ratings yet
- Casts inDocument1 pageCasts ingregoryvoNo ratings yet
- Parvo BacteriaDocument2 pagesParvo BacteriaErnie G. Bautista II, RN, MDNo ratings yet
- Poliomyelitis Haemophilus Influenzae Type B VariecellaDocument4 pagesPoliomyelitis Haemophilus Influenzae Type B VariecellaJeanna Chong100% (1)
- Hetal Patel GROUP - 631: RicketsDocument28 pagesHetal Patel GROUP - 631: RicketsRahul MunikrishnaNo ratings yet
- Dr. A. Samy TAG Upper Limb - 1Document20 pagesDr. A. Samy TAG Upper Limb - 1DRAHMEDFAHMYORTHOCLINICNo ratings yet
- Dr. A. Samy TAG Pediatric - 1Document7 pagesDr. A. Samy TAG Pediatric - 1Herato MenaNo ratings yet
- Spine #Document5 pagesSpine #Herato MenaNo ratings yet
- The Ukfpo Clinical Assessment Examination Guide by Sarishka Singh Plab ResourcesDocument112 pagesThe Ukfpo Clinical Assessment Examination Guide by Sarishka Singh Plab ResourcesWonjoo LeeNo ratings yet
- Rickets and OsteomalaciaDocument6 pagesRickets and OsteomalaciaHabib UllahNo ratings yet
- Roberts Week 7 HyperparathyroidismDocument17 pagesRoberts Week 7 Hyperparathyroidismjackie robertsNo ratings yet
- DeletedDocument354 pagesDeletedshalom1413No ratings yet
- مذكرة مايوSMLE-2019Document514 pagesمذكرة مايوSMLE-2019Abidi HichemNo ratings yet
- 216093371Document48 pages216093371khuzaima933% (15)
- Elecsys PTH (1-84) : Cobas e 801 English System InformationDocument5 pagesElecsys PTH (1-84) : Cobas e 801 English System Informationsyafiq_82No ratings yet
- E-bOOK Causes-And-Treatment-Of-Vitamin-D-DeficiencyDocument15 pagesE-bOOK Causes-And-Treatment-Of-Vitamin-D-DeficiencyPoongkodi KNo ratings yet
- Surgery Rotation NotesDocument18 pagesSurgery Rotation NotesNadiim Rajabalee100% (2)
- Cme Endocrinology Saqs (80447) : Self-Assessment QuestionnaireDocument3 pagesCme Endocrinology Saqs (80447) : Self-Assessment QuestionnaireAbu AhmedNo ratings yet
- Hiperparatiroidism SarcinaDocument7 pagesHiperparatiroidism SarcinaClaudia IrimieNo ratings yet
- Agents Affecting Bone Mineral Homeostasis LectureDocument71 pagesAgents Affecting Bone Mineral Homeostasis LectureNabilah DENo ratings yet
- Secondary Hyperparathyroidism - Pathogenesis, Disease Progression, and Therapeutic OptionsDocument9 pagesSecondary Hyperparathyroidism - Pathogenesis, Disease Progression, and Therapeutic OptionsJuanita GonzálezNo ratings yet
- Endocrine New EditionDocument150 pagesEndocrine New Editiondigracia manatigaNo ratings yet
- Endocrine System Prepared By: Prof. Mike Chavez RN, USRNDocument7 pagesEndocrine System Prepared By: Prof. Mike Chavez RN, USRNMeiJoyFlamianoIINo ratings yet
- Mechanisms and Treatment of Hypercalcemia of MalignancyDocument8 pagesMechanisms and Treatment of Hypercalcemia of MalignancyDebby Christiana SNo ratings yet
- Revised Mrcs Syl Lab UsDocument68 pagesRevised Mrcs Syl Lab Usshafa_atNo ratings yet
- Parathyroid: Calcium and Vitamin DDocument135 pagesParathyroid: Calcium and Vitamin DPhysiology by Dr RaghuveerNo ratings yet
- Osteomyelitis Metabolic Bone DisordersDocument36 pagesOsteomyelitis Metabolic Bone DisordersVishesh JainNo ratings yet
- Bailey CH 7 81-120Document82 pagesBailey CH 7 81-120melaniaNo ratings yet
- Parathyroid Diseases: Kristine Mae FernandezDocument27 pagesParathyroid Diseases: Kristine Mae Fernandeznurse_on_duty13No ratings yet
- UntitledDocument82 pagesUntitledJahnavi SNo ratings yet
- Vitamin D Deficiency in AdultsDocument15 pagesVitamin D Deficiency in AdultsAnabel Pinedo Carrasco100% (1)
- CPC Calciphylaxis Nejmcpc069038Document9 pagesCPC Calciphylaxis Nejmcpc069038sdalez1No ratings yet
- Clinical Biochemistry - Clinical Pathology and Procedures - VetDocument9 pagesClinical Biochemistry - Clinical Pathology and Procedures - VetHimmet AslanNo ratings yet
- Metabolic Jaw DiseasesDocument55 pagesMetabolic Jaw DiseasesoladunniNo ratings yet