Professional Documents
Culture Documents
Repair of Articular Cartilage Defects With Intra-A
Uploaded by
hashim_716108627Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Repair of Articular Cartilage Defects With Intra-A
Uploaded by
hashim_716108627Copyright:
Available Formats
Jia
et al. J Transl Med (2018) 16:123
https://doi.org/10.1186/s12967-018-1485-8 Journal of
Translational Medicine
RESEARCH Open Access
Repair of articular cartilage defects
with intra‑articular injection of autologous
rabbit synovial fluid‑derived mesenchymal stem
cells
Zhaofeng Jia1,2,3†, Qisong Liu2,3†, Yujie Liang4,5, Xingfu Li2,3, Xiao Xu1,2,3, Kan Ouyang2,3, Jianyi Xiong2,3,
Daping Wang1,2,3* and Li Duan2,3*
Abstract
Background: The role of rabbit synovial fluid-derived mesenchymal stem cells (rbSF-MSCs) in cartilage defect repair
remains undefined. This work evaluates the in vivo effects of rbSF-MSCs to repair knee articular cartilage defects in a
rabbit model.
Methods: Cartilage defects were made in the patellar grooves of New Zealand white rabbits. The rbSF-MSCs were
generated from the knee cavity by arthrocentesis. Passage 5 rbSF-MSCs were assayed by flow cytometry. The multi-
potency of rbSF-MSCs was confirmed after 3 weeks induction in vitro and the autologous rbSF-MSCs and prediffer-
entiated rbSF-MSCs were injected into the synovial cavity. The intra-articular injection was performed once a week
for 4 weeks. The animals were euthanized and the articular surfaces were subjected to macroscopic and histological
evaluations at 8 and 12 weeks after the first intra-articular injection.
Results: Hyaline-like cartilage was detected in the defects treated with rbSF-MSCs, while fibrocartilage tissue formed
in the defects treated with chondrocytes induced from rbSF-MSCs.
Conclusions: Our results suggest that autologous undifferentiated rbSF-MSCs are favorable to articular cartilage
regeneration in treating cartilage defects.
Keywords: Mesenchymal stem cells, Autologous, Rabbit synovial fluid, Chondrogenic differentiation,
Cartilage defect, Cellular therapy, Intra-articular injection
Background implantation (ACI) has been the gold standard for carti-
Articular cartilage is a non-vascular and non-innervated lage repair in the clinic [2]. However, de-differentiation of
tissue. Because of this unusual structure, injured cartilage chondrocytes while culturing cells in vitro compromises
has poor healing capacity. Therefore, without treatment, efficacy [3]. Thus, alternative cell sources are needed.
most cases of cartilage injuries result in osteoarthritis Mesenchymal stem cells (MSCs) are promising can-
(OA) [1]. Numerous techniques are commonly used for didates for cartilage repair because they are multi-
cartilage repair. Among them, autologous chondrocyte potent and highly proliferative. MSC based therapies
have been widely investigated for cartilage repair in
both preclinical and clinical settings [4, 5]. Because
*Correspondence: dapingwang1963@qq.com; 825343512@qq.com
† there is no risk of immune rejection and host tissue
Zhaofeng Jia and Qisong Liu contributed equally to this work
2
Shenzhen Key Laboratory of Tissue Engineering, Shenzhen Laboratory engraftment occurs more readily, autologous bone
of Digital Orthopeadic Engineering, Shenzhen Second Peoples Hospital marrow-derived MSCs (BM-MSCs) are commonly
(The First Hospital Affiliated to Shenzhen University), Shenzhen 518035,
used for cartilage repair. However, conflicting results
Guangdong Province, China
Full list of author information is available at the end of the article
© The Author(s) 2018. This article is distributed under the terms of the Creative Commons Attribution 4.0 International License
(http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium,
provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license,
and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/
publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 2 of 12
have been reported for using BM-MSCs in a collagen- Rabbit synovial fluid collection
induced arthritis mouse model [6]. The hair on an area about 3 × 3 cm in size within the rab-
Synovial fluid-derived MSCs (SF-MSCs) are another bit knee area was shaved using a safety electric shaver.
well-studied autologous MSC type used for cartilage The site was disinfected three times with the povidone
repair. Compared to BM-MSCs, SF-MSCs can be eas- iodine solution and 75% ethanol. Sterile drape application
ily and non-invasively obtained during diagnosis or was used to thoroughly dry the area. Isotonic saline solu-
treatment [7]. The population of SF-MSCs in synovial tion (2 mL) was injected into the rabbit knee joint cavity
fluid greatly increases with joint disease and injury from the lateral articular space and the knee was moved
[8]. Therefore, SF-MSCs are likely to be an ideal cell to full extension and flection several times. Synovial fluid
source for cartilage repair [9, 10]. was collected along with the saline solution using a ster-
Both MSCs and differentiated MSCs can repair car- ile injection syringe. The synovial fluid was labeled cor-
tilage injury after implantation in the lesion. A predif- responding to each rabbit.
ferentiation procedure prior to treatment has had
favorable results probably due to similarities to ACI rbSF‑MSC isolation and culture
[11]. While the cartilage injury environment may not The synovial fluid was filtered through a 40 μm nylon
favor chondrogenic differentiation, MSCs are more cell strainer (Cell Strainer, BD Falcon) to remove debris
active than seed cells in vivo. The paracrine effect of within 4 h of collection. The filtered fluid was collected in
inflammatory factors is more critical for MSC therapy sterilized centrifuge tubes and then spun at 1500 rpm for
when it comes to inflammatory diseases [12–15]. Jun- 10 min at room temperature. The supernatant was dis-
stunlin et al. observed comparable results using MSCs carded after centrifugation. The pellet was washed with
with or without predifferentiation in their animal PBS and resuspended with culture medium [DMEM sup-
model, as the predifferentiation procedure may alter plemented with 10% of fetal bovine serum (FBS, Sigma,
the paracrine factors released [16]. USA), 1% of penicillin and streptomycin (Sigma-Aldrich,
In the present study, we injected both autologous USA)] and then plated on 100 mm dishes. The dishes
rabbit SF-MSCs (rbSF-MSCs) and predifferentiated were incubated at 37 °C in a humidified atmosphere con-
rbSF-MSCs to the experimental rabbit articular cav- taining 5% CO2. After 48 h, the non-adherent cells were
ity. We first confirmed the therapeutic effects of removed by changing the media. Then the media was
autologous rbSF-MSCs, and then compared the ther- changed every 3 days. The cells adhered to the bottom of
apeutic effects of rbSF-MSCs and predifferentiated the flask and cell colonies formed (Passage 1).
rbSF-MSCs. We found that predifferentiation weak- After 7–10 days, cells were lifted by 0.05% trypsin (Life
ened the therapeutic effect of the MSCs, which implies Technologies, USA) and seeded to 75 cm2 dishes at a
that the predifferentiation process alters the paracrine density of about 2000 cells/cm2. The media was changed
factors released by the cells. every 3 days (P2) until the cells reached 80% confluency.
The cells were passaged several times until the amount
of cells reached 1 × 108 cells (P5). The cells were used for
Methods flow cytometry, multipotency assay, qRT-PCR, and intra-
Animals articular injection.
Eighteen adult New Zealand white rabbits (6 months
old and weighing 2 ± 0.5 kg) were used in this study.
Immunophenotyping identification of rbSF‑MSCs by flow
To minimize distress, the rabbits were housed singly
cytometry
and allowed to move freely in their cages with unre-
stricted access to water and food. Prior to the animal The rbSF-MSCs were lifted by trypsin and suspended
experiment, rabbits were allowed to acclimate to their in PBS containing 5% bovine serum albumin (Sigma-
cages for at least 7 days. Aldrich, USA) at a concentration of 3 × 105 cells/50 μL.
The animals were randomly assigned to three groups The cells were incubated with mouse anti-rabbit CD44
of six. Synovial fluid was obtained from all animals by (Bio-Rad, MCA806GA), CD73 (eBiosciences, 25073180),
arthrocentesis and then articular cartilage defects were CD90 (BD Sciences, 554895), CD31 (Antibodies online
induced in the femur condyle. After 2 weeks, the rab- inc., ABIN153449), CD34 (Gene Tex, GTX28158), and
bits were intra-articularly injected as follows, group 1 CD45 (Bio-Rad, MCA808GA) monoclonal antibody
(Control group) with saline, group 2 with predifferen- (mAb) (1:100 dilution) at 4 °C for 1 h. Then the cells were
tiated rbSF-MSCs, and group 3 with rbSF-MSCs. The washed with PBS three times and incubated with a FITC-
injections were administrated once a week for 4 weeks. labeled secondary anti-mouse antibody (Alexa Fluor
488-labeled secondary anti-rat antibody for CD34) (1:200
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 3 of 12
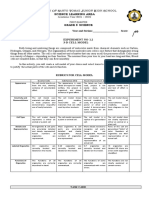
dilution, Invitrogen) at 4 °C for 30 min. The appropriate Table 1 Primers used for real-time PCR
rabbit isotype antibodies were used as controls. Samples Gene name Primer sequence
were processed using a FACS Canto II flow cytometer
(BD Biosciences, USA) and analyzed with FlowJo soft- GAPDH Forward: 5′-GGAGAAAGCTGCTAA-3′
ware (Tree Star). Reverse:5′-ACGACCTGGTCCTCGGTGTA-3′
Runx2 Forward: 5′-TATGAAAAACCAAGTAGCAAGGTTC-3′
Trilineage differentiation of the rbSF‑MSCs Reverse: 5′-GTAATCTGAC TCTGTCCTTGTGGAT-3′
Passage 5 rbSF-MSCs were seeded in a 6-well tissue Osteocalcin Forward: 5′-GTGCAGAGTCCAGCAAAGGT-3′
culture plate with a density of 1 03 cells/cm2. Trilineage Reverse: 5′-CTAGCCAACTCGTCACAGTC-3′
differentiation was induced by the MSC osteogenic dif- Col2A1 Forward: 5′-CAGGCAGAGGCAGGAAACTAAC-3′
ferentiation medium (MODM, ScienCell, USA), MSC Reverse: 5′-CAGAGGTGTT TGACACGGAGTAG-3′
adipogenic differentiation medium (MADM, ScienCell, Sox9 Forward: 5′-GTACCCGCACCTGCACAAC-3′
USA), and MSC chondrogenic differentiation medium Reverse: 5′-TCCGCCTCCTCCACGAAG-3′
without serum (MCDM, ScienCell, USA). For chondro- PPARγ Forward: 5′-GACCACTCCCACTCCT TTGA-3′
genic differentiation, we also used the pellet culture of Reverse: 5′-CGACATTCAATTGCCATGAG-3′
SF-MSCs for the histological staining. 200,000 P5 cells LPL Forward: 5′-TACAGGGCGGCCACAAGTT TT-3′
were pelleted by centrifuge at 400g to the bottom of the Reverse: 5′-ATGGAGAGCAAAGCCC TGC TC-3′
conical tube. Then cell pellets were induced by the MSC
chondrogenic differentiation medium. The induction
medium was changed every 3 days for 3 weeks. After was performed with a 7500 real-time PCR detection
induction, the cells were further processed for histologi- system (ABI, Foster City, CA). The 2−ΔΔCT method was
cal and quantitative real-time PCR (qRT-PCR) analysis. used to analyze the relative gene expression levels using
GAPDH as an endogenous control.
Histological staining after trilineage differentiation
After osteogenic differentiation, the cells were fixed
Establishment of cartilage defects
with 4% formaldehyde for 30 min at room temperature
Rabbits were placed in a dorsal-recumbent position after
and stained with 1% Alizarin Red (Sigma-Aldrich, USA)
general anesthesia induced by injecting 3% pentobarbi-
for 5 min [17]. After adipogenic differentiation, the cells
tal sodium into the marginal ear vein at a dose of 1 mL/
were fixed with 4% formaldehyde for 30 min at room
kg. The knee previously used for synovial fluid collection
temperature and stained with Oil Red O (Sigma-Aldrich,
was used for the operation. The hair on the knee area
USA) for 10 min [18]. After chondrogenic differentiation,
was shaved and the surgical site was disinfected with the
the pellet was fixed with 4% formaldehyde for 30 min
povidone iodine solution and 75% ethanol three times.
at room temperature, sectioned (50 nm thickness) and
The rabbits’ knee joints were operated on using a medial
stained with Toduiline blue (Sigma-Aldrich, USA) for
parapatellar approach. A cylindrical full-thickness car-
30 min at room temperature [19]. After staining, the cells
tilage defect (3.5 mm in diameter and 1.5 mm in depth)
were washed with PBS and images were captured under a
was created on the trochlear groove using a special drill
microscope.
(Additional file 1: Figure S1A). Then, the joint capsular
was sutured and closed layer by layer using absorbable
qRT‑PCR analysis after trilineage differentiation surgical sutures (VICRYL Plus). After surgery, the rabbits
Total RNA was extracted by using Trizol (Invitrogen). were allowed free movement in their cages. The surgical
The RNA was then reverse-transcribed into cDNA by site was disinfected with 0.1% povidone iodine twice a
a DNA synthesis kit (TaKaRa, Shiga, Japan). qRT-PCR day for 3 days. Wound healing was monitored for 1 week
was carried out using the SYBR Green PCR Kit (TaKaRa, and no infection was observed.
Shiga, Japan). Rabbit-specific primers were used for ana-
lyzing the transcription level of Osteocalcin and Runx2
Injection of rbSF‑MSCs and predifferentiated rbSF‑MSCs
(runt-related transcription factor 2), collagen type II
The rbSF-MSCs were cultured in culture medium or
alpha 1 (Col2A1) and sex determining region Y-box 9
chondrogenic differentiation medium for 3 weeks. Cells
(Sox9), peroxisome proliferators-activated receptor γ
were lifted by trypsin and resuspended in saline solution.
(PPARγ) and lipoprotein lipase (LPL), for the osteogenic,
500 μL saline solution containing 5 × 106 cells were artic-
chondrogenic and adipogenic samples, respectively. Glyc-
ularly injected in the knee joint of experimental rabbits
eraldehyde-3-phosphate dehydrogenase (GAPDH) was
using large 18G size needles (BD, USA) at 7, 14, 21, and
used as an endogenous reference. The primer sequences
28 days after surgery (Additional file 1: Figure S1B). The
used in this study were listed in Table 1. Real-time PCR
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 4 of 12
control group animals were injected with 500 μL saline passage 2 cells displayed a spindle-like morphology, but
solution only. after further passages the percentage of cells with typical
fibroblastic cell morphology increased (Fig. 1).
Macroscopic score and histological evaluation of cartilage
repair Epitope identification of rbSF‑MSCs
After 8 and 12 weeks of intra-articular injection, all rab- Flow cytometry was used to identify the surface mark-
bits were sacrificed and the operated distal femur con- ers of rbSF-MSCs, according to the MSC identification
dyles were harvested. The specimens were fixed with criteria recommended by the International Society for
10% formalin solution (Sigma-Aldrich, USA) for 24 h and Cellular Therapy [23, 24]. The results showed that the
then decalcified for 24 h with a 10% aqueous solution of rbSF-MSCs we cultured met the identification criteria of
nitric acid for paraffin embedding (Sigma-Aldrich, USA). MSCs, as the cells were negative for CD31, CD34, CD45
All specimens were cut into sections of 4 μm thickness (below 3%) and positive for CD44, CD73 CD90 (above
and stained with hematoxylin–eosin,toluidine blue, Col 95%) (Fig. 2).
I and Col II (Abcam, UK) for morphological analysis.
The gross appearance and histological evaluation of the Trilineage differentiation of rbSF‑MSCs
defect sites were photographed and blindly scored by 3 To further evaluate the stem cell properties of rbSF-
independent observers based on the International Carti- MSCs, we assayed their potential to differentiate to
lage Repair Society (ICRS) macroscopic scoring system osteogenic, adipogenic, and chondrogenic lineages.
(Additional file 2: Table S1) and ICRS Visual Histological After culturing the rbSF-MSCs in osteogenic media for
Assessment Scale (Additional file 3: Table S2) [20–22]. 3 weeks, the formation of calcium mineral deposition
was clearly observed by Alizarin Red staining (Fig. 3a, d).
Also, Osteocalcin and Runx2 were strongly induced when
Statistical analysis
compared to the control cells (Fig. 4a, d). To assess adi-
All data are presented as mean ± standard deviation
pogenesis, cells were induced by adipogenic medium for
(SD). Statistical analysis was performed using the one-
3 weeks. Oil Red O staining indicated the formation of
way ANOVA followed by the Turkey’ post hoc test. All
lipid droplets (Fig. 3b, e). Up-regulation of the adipocyte
experiments were repeated three times. In all groups, P
marker genes, PPARγ and LPL, further confirmed adipo-
values less than 0.05 were considered to indicate a statis-
genic differentiation (Fig. 4b, e). When the rbSF-MSCs
tically significant difference, and P values less than 0.01
were cultured in chondrogenic medium for 3 weeks, they
and 0.001 were considered highly significant differences.
successfully differentiated into chondrocytes, which was
The Graph-Pad Prism version 6.0 was used for statistical
confirmed by both Toduiline blue staining (Fig. 3c, f ) and
analysis.
the up-regulation of Col2A1 and Sox9 (Fig. 4c, f ).
Results Cartilage repair effects of rbSF‑MSCs and predifferentiated
Characterization of rbSF‑MSCs rbSF‑MSCs
Morphology of rbSF‑MSCs Gross observation of repaired cartilage
Multiple cell colonies formed on the plate after culturing Rabbits were sacrificed 8 and 12 weeks after the first
the synovial fluid pellet for several days. The majority of intra-articular injection and the femoral condyles were
Fig. 1 Cell morphology observed by microscope. A Colonies formed on the plate (passage 1), B Passage 2 cells, C Passage 4 cells. Scale
bar = 100 μm
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 5 of 12
Fig. 2 Cell surface marker analysis by flow cytometry. Passage 5 rbSF-MSCs were positive for CD44 (95.4%), CD73 (96.8%), and CD90 (95.4%), and
negative for CD31 (2.8%), CD34 (1.2%), and CD45 (0.16%)
harvested. We first evaluated the performance of car- in cartilage repair, but rbSF-MSCs produced better
tilage repair by gross observation (Fig. 5A–F). The outcomes.
saline-treated control group still had a clear boundary
between the normal tissue and the defect after 8 and Histological analyses of repaired cartilage
12 weeks (Fig. 5A, D). The defects in the predifferenti- Cartilage damage without intervention resulted in obvi-
ated rbSF-MSCs group was covered by a thin layer of ous hollowing and the formation of fibrous tissues after
fibrous tissue at 8 weeks, and was completely covered 8 weeks (Fig. 6A, B). The damaged area decreased after
with white hyper-proliferative fibrous tissue at 12 weeks 12 weeks, and was covered by some inflammatory tis-
(Fig. 5B, E). The regenerated tissue in the rbSF-MSCs sue (Fig. 6C, D). Animals injected with predifferenti-
group covered more than 80% of the defects at 8 weeks ated rbSF-MSCs obtained better repair compared with
and the defect was completely repaired at 12 weeks the control group. However, the regenerated tissue
(Fig. 5C, F). Therefore, rbSF-MSCs exhibited better was fibrous and the gap between newly grown tissue
repair effects than the predifferentiated rbSF-MSCs. and native cartilage was obvious at 8 weeks (Fig. 6E,
We further evaluated repair using the ICRS macro- F). After 12 weeks, the regenerated tissue was primar-
scopic scores. Both the predifferentiated rbSF-MSCs ily hyper-proliferated fibrous tissue, while only a small
and rbSF-MSCs treatments had much higher scores part was cartilage-like tissue as indicated by Collagen I
than the control group at the two time points, indicat- immune-histological staining and Toluidine blue staining
ing that the treatments with both cells were effective (Figs. 6G, H, 7). The rbSF-MSCs group regenerated carti-
(Fig. 5G, H). However, surprisingly the predifferenti- lage better than the predifferentiated rbSF-MSCs group,
ated rbSF-MSCs group had significantly lower scores which was similar to the gross observation (Fig. 6I, J).
than the rbSF-MSCs group. Therefore, based on gross With the injection of rbSF-MSCs, there was newly-
observation, we found that injection of both cells aids formed cartilage tissue in the defect at 8 weeks (Fig. 6I, J).
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 6 of 12
Fig. 3 Trilineage differentiation of rbSF-MSCs characterized by histological staining. a, d Alizarin red staining for osteogenic differentiation; b, e oil
red O staining for adipogenic differentiation; c, f toduiline staining for chondrogenic differentiation. Scale bar = 100 μm
After 12 weeks, the regenerated tissue completely filled injected predifferentiated rbSF-MSCs for cartilage defect
the defect, which had a similar histological staining as repair. However, our results showed that the regener-
the native hyaline cartilage as indicated by Toluidine blue ated tissue after injecting predifferentiated rbSF-MSCs
and Collagen II staining (Figs. 6K, L, 8). was mainly composed of fibrous tissue, which is unfa-
We further evaluated the repair effect based on the vorable for cartilage repair. Therefore, predifferentiation
ICRS Visual Histological Assessment Scale system might hinder the regenerative effects of rbSF-MSCs,
(Fig. 6M, N). Similar with our other observations, treat- which contradicts result reported by others. Several stud-
ment with both cell types resulted in obvious repair com- ies have reported that MSCs function in vivo as seed
pared to the control group. However the rbSF-MSCs cells and in the production of bioactive factors [30–32].
showed a significantly higher repair score than the predif- The predifferentiation process could also weaken the
ferentiated rbSF-MSCs. Overall, the rbSF-MSCs showed stemness of rbSF-MSCs as well as altering the autocrine
the best effect in regenerating cartilage after damage. and paracrine factors [33–35]. Recently, it’s been shown
that exosome released from MSCs can be used to treat
Discussion inflammatory diseases, including osteoarthritis [36, 37].
Articular cartilage tissue repair is challenging because Besides osteoarthritis, Zhu et al. reported that a stem
of the limited self-regenerative potential of native carti- cell-derived exosome-laden hydrogel could regenerate
lage [25, 26]. MSC-based therapy holds great promise cartilage tissue in a rabbit model after 12 weeks, which
for restoring cartilage defects [27]. SF-MSCs are easily confirmed the repair effects of the paracrine factors [38].
obtained and are highly proliferative, making them an Carrying bioactive factors may cause the differences
ideal cell source for cartilage repair [28, 29]. In this study, between our study and others. Researchers often seed
we injected autologous rbSF-MSCs into the experimental the pre-differentiated cells on a scaffold [39–41]. When
rabbit articular cavity. Results of this study showed that implanting the cell-scaffold complex in a defect, they
the cartilage defect was fully repaired with undifferen- implanted the paracrine factors from the cells and the
tiated rbSF-MSCs after 12 weeks. This is the first study extracellular matrix together. However, in this study,
to demonstrate the superiority of autologous rbSF-MSC we digested the cells from the culture flask before injec-
injection for cartilage repair in a rabbit model. tion. Therefore, only the differentiated cells was injected
It has been reported that predifferentiation ben- without the paracrine factors. Junstunlin et al. injected
efits repair because it mimicks ACI [11]. We therefore resuspended cells for cartilage repair as well, but they
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 7 of 12
Fig. 4 Trilineage differentiation of rbSF-MSCs characterized by qRT-PCR analysis. a, d Induced rbSF-MSCs had much higher levels of the osteogenic
marker gene (Runx2 and Osteocalcin) than control cells. b, e Induced rbSF-MSCs had up-regulatd PPARγ and LPL compared with control cells. c,
f Chondrogenic differentiation markers (Col2A1, Sox9) were significantly increased after induction compared to the control. Gene expression was
normalized to GAPDH, and obtained from at least three independent experiments. (****P < 0.0001)
administrated cells together with platelet-rich plasma, functional chondrocytes and secrete a large amount of
which had plentiful bioactive factors [16]. They observed extracellular matrix, making them an excellent alterna-
comparable repair effects for both undifferentiated MSCs tive cell source for cartilage regenerative therapy [42–44].
and predifferentiated MSCs. Without the nutrition of This study also had several limitations. The optimum
the bioactive factors from the platelet-rich plasma, the cell number of rbSF-MSCs for intra-articular injection
predifferentiated MSCs may have less repair activity. We remains unknown. It is also uncertain whether the newly
remain in need of further investigations to clarify the regenerated tissue was completely induced from injected
physiological mechanisms. rbSF-MSCs. Finally, in our animal study, we observed
Thirdly, the inherent advantages of the SF-MSCs could and evaluated results after 8 and 12 weeks. This follow
establish their potential role in cartilage damage treat- up time may be too short to show more significant differ-
ment. Jones et al. reported that the number of SF-MSCs ences of the repair quality.
in knee joints significantly increased sevenfold during the
early stages of osteoarthritis (OA) [8]. The increased SF-
MSCs could contribute to maintaining the physiological Conclusions
homeostasis of joints. In addition, treatment with autol- In summary, we confirmed the repair effects of autolo-
ogous SF-MSCs has no dispute about safety and immu- gous rbSF-MSCs in a rabbit model. We found that a
nogenicity. Furthermore, the SF-MSCs possess highly predifferentiation process was not helpful for cartilage
immunosuppressive properties in vivo [7]. Compared to repair, which could be explained by loss of paracrine func-
the BM-MSCs and synovium-derived mesenchymal stem tion of MSCs by predifferentiation. Intra-articular injec-
cells (SM-MSCs), SF-MSCs prefer differentiation into tion of autologous undifferentiated rbSF-MSC represents
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 8 of 12
Fig. 5 Macroscopic assessment of repaired cartilage. A–F Photographs of rabbit knee articular defects 8 and 12 weeks after cell injection. Black
dotted circles indicate the original defect margin. G, H ICRS macroscopic scores of repaired cartilage at 8 and 12 weeks. Data are presented as
mean ± SD (n = 6, **P < 0.01, ****P < 0.0001)
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 9 of 12
Fig. 6 Histological evaluation of repaired cartilage. A–L Representative H&E and toluidine blue staining of repaired cartilage at 8 and 12 weeks.
Scale bar: 100 μm. M, N ICRS Visual Histological Assessment Scale for repaired cartilage at 8 (M) and 12 (N) weeks. Data are presented as mean ± SD
(n = 6; *P < 0.05, **P < 0.01, ***P < 0.001)
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 10 of 12
Fig. 7 Immuno-histological staining of Collagen I. A–C Representative Collagen I staining of repaired cartilage at 12 weeks. a–c Enlarged image of
the dashed box in A–C, respectively. Scale bar: 100 μm
Fig. 8 Immuno-histological staining of Collagen II. A–C Representative Collagen II staining of repaired cartilage at 12 weeks. a–c Enlarged image of
the dashed box in A–C, respectively. Scale bar: 100 μm
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 11 of 12
a better approach for efficient and effective treatment Consent for publication
The details/images of this study will be freely available on the internet and
for articular cartilage lesions. This in vivo research could may be seen by the general public.
contribute to the use of SF-MSC-based therapeutics in
cartilage tissue engineering. Ethics approval and consent to participate
Ethical approval for animal experiments was obtained from the Institutional
Additional files Animal Care and Use Committee of Shenzhen Second People’s Hospital,
Shenzhen University, China.
Additional file 1: Figure S1. Surgical procedures of rabbit articular Funding
cartilage defect introduction and intra-articular injections of rbSF-MSCs. This study was supported financially by the following grants: Natu-
(A) A cylindrical full-thickness cartilage defect (3.5 mm in diameter and 1.5 ral Science Foundation of China (Nos. 81572198; 81772394); Fund for
mm in depth) was created on the trochlear groove using a special drill. (B) High Level Medical Discipline Construction of Shenzhen University (No.
The cells were articularly injected in the knee joint of experimental rabbits 2016031638); The Medical Research Foundation of Guangdong Province,
using using large 18G size needles. China (No. A2016314); Shenzhen Science and Technology Projects (Nos.
JCYJ20170306092215436; JCYJ20170412150609690; JCYJ20170413161800287;
Additional file 2: Table S1. International Cartilage Repair Society macro- SGLH20161209105517753; JCYJ20160301111338144).
scopic evaluation of cartilage repair.
Additional file 3: Table S2. The ICRS Visual Histological Assessment Scale.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in pub-
lished maps and institutional affiliations.
Abbreviations
ACI: autologous chondrocyte implantation; MSC: mesenchymal stem cell; BM- Received: 23 January 2018 Accepted: 17 April 2018
MSCs: bone marrow-derived mesenchymal stem cells; rbSF-MSC: rabbit syno-
vial fluid-derived mesenchymal stem cell; SM-MSCs: synovium-derived mesen-
chymal stem cells; OA: osteoarthritis; PBS: phosphate-buffered saline; DMEM:
Dulbecco’s modified eagle medium; MODM: MSC osteogenic differentiation
medium; MADM: MSC adipogenic differentiation medium; MCDM: MSC chon- References
drogenic differentiation medium; FBS: fetal bovine serum; Runx2: runt-related 1. Messner K, Gillquist J. Cartilage repair: a critical review. Acta Orthop
transcription factor 2; Col2A1: collagen type II alpha 1; Sox9: sex determining Scand. 1996;67:523–9.
region Y-box 9; PPARγ: peroxisome proliferators-activated receptor γ; LPL: 2. Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L. Treat-
lipoprotein lipase; GAPDH: glyceraldehyde-3-phosphate dehydrogenase. ment of deep cartilage defects in the knee with autologous chondrocyte
transplantation. N Engl J Med. 1994;331:889–95.
Authors’ contributions 3. Pareek A, Carey JL, Reardon PJ, Peterson L, Stuart MJ, Krych AJ. Long-term
JZF and LQS designed the protocol and participated in the experiments and outcomes after autologous chondrocyte implantation: a systematic
drafted the manuscript; participated in the design of the draft and revised it review at mean follow-up of 11.4 years. Cartilage. 2016;7:298–308.
critically for important intellectual content; LYJ and LXF performed labora- 4. Shen W, Chen J, Zhu T, Chen L, Zhang W, Fang Z, Heng BC, Yin Z, Chen
tory culture of MSCs and characterization of the cells by microscopy and X, Ji J, Chen W, Ouyang HW. Intra-articular injection of human meniscus
flow cytometry; XX and OYK participated in the animal experiments and stem/progenitor cells promotes meniscus regeneration and ameliorates
interpreted the data obtained; XJY critically revised the draft for important osteoarthritis through stromal cell-derived factor-1/cxcr4-mediated hom-
intellectual content and obtained funding; DL and WDP supervised the study, ing. Stem Cells Transl Med. 2014;3:387–94.
helped to coordinate the study, revised the draft for important intellectual 5. Pelttari K, Pippenger B, Mumme M, Feliciano S, Scotti C, Mainilvarlet P,
content, obtained funding and approval of the final version of the manuscript. Procino A, von Rechenberg B, Schwamborn T, Jakob M, Cillo C, Barbero
All authors read and approved the final manuscript. A, Martin I. Adult human neural crest-derived cells for articular cartilage
repair. Sci Transl Med. 2014;6:251ra119.
Author details 6. Augello A, Tasso R, Negrini SM, Cancedda R, Pennesi G. Cell therapy using
1
Postgraduate Institution, Guangzhou Medical University, Guangzhou 511436, allogeneic bone marrow mesenchymal stem cells prevents tissue dam-
Guangdong Province, China. 2 Shenzhen Key Laboratory of Tissue Engineer- age in collagen-induced arthritis. Arthritis Rheum. 2007;56:1175–86.
ing, Shenzhen Laboratory of Digital Orthopeadic Engineering, Shenzhen 7. Lee WJ, Hah YS, Ock SA, Lee JH, Jeon RH, Park JS, Lee SI, Rho NY, Rho GJ,
Second Peoples Hospital (The First Hospital Affiliated to Shenzhen University), Lee SL. Cell source-dependent in vivo immunosuppressive properties
Shenzhen 518035, Guangdong Province, China. 3 Guangdong Provincial of mesenchymal stem cells derived from the bone marrow and synovial
Research Center for Artificial Intelligence and Digital Orthopedic Technology, fluid of minipigs. Exp Cell Res. 2015;333:273–88.
Shenzhen 518035, People’s Republic of China. 4 Department of Chemistry, The 8. Jones EA, Crawford A, English A, Henshaw K, Mundy J, Corscadden D,
Chinese University of Hong Kong, Shatin, Hong Kong SAR, China. 5 Shenz- Chapman T, Emery P, Hatton P, McGonagle D. Synovial fluid mesenchymal
hen Kangning Hospital, Shenzhen Mental Health Center, Shenzhen 518035, stem cells in health and early osteoarthritis: detection and functional
Guangdong Province, People’s Republic of China. evaluation at the single-cell level. Arthritis Rheum. 2008;58:1731–40.
9. Sakaguchi Y, Sekiya I, Yagishita K, Muneta T. Comparison of human stem
Acknowledgements cells derived from various mesenchymal tissues: superiority of synovium
We thank the members of our research group. All authors have approved the as a cell source. Arthritis Rheum. 2005;52:2521–9.
final version of the manuscript and read the journal’s authorship agreement. 10. Chiang CW, Chen WC, Liu HW, Chen CH. Application of synovial fluid
mesenchymal stem cells: platelet-rich plasma hydrogel for focal cartilage
Competing interests defect. J Exp Clin Med. 2014;6:118–24.
The authors declare that they have no competing interests. 11. Zscharnack M, Hepp P, Richter R, Aigner T, Schulz R, Somerson J, Josten
C, Bader A, Marquass B. Repair of chronic osteochondral defects using
Availability of data and materials predifferentiated mesenchymal stem cells in an ovine model. Am J Sports
The datasets during and/or analysed during the current study available from Med. 2010;38:1857–69.
the corresponding authors on reasonable request. 12. Ollitrault D Jr, Legendre F Jr, Gomez-Leduc T Jr, Hervieu M Jr, Bouyoucef
M Jr, Drougard C Sr, Mallein-Gerin F Sr, Leclercq S Sr, Boumediene K Sr,
Demoor M Sr, Galera P Sr. Differentiation of human adult mesenchymal
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Jia et al. J Transl Med (2018) 16:123 Page 12 of 12
stem cells in chondrocytes for cartilage engineering. Osteoarthr Cartil. 31. Ha HJ, Shin SS, Sun SO, Young LH, Kyu WS, Hui KB, Ryong SH, Kwan LJ,
2012;20:S278. Kyun PY. Comparison of cytokine expression in mesenchymal stem cells
13. Nakanishi C, Yamagishi M, Yamahara K, Hagino I, Mori H, Sawa Y, Yagihara from human placenta, cord blood, and bone marrow. J Korean Med Sci.
T, Kitamura S, Nagaya N. Activation of cardiac progenitor cells through 2009;24:547–54.
paracrine effects of mesenchymal stem cells. Biochem Biophys Res Com- 32. Horwitz EM, Prather WR. Cytokines as the major mechanism of mesen-
mun. 2008;374:11–6. chymal stem cell clinical activity: expanding the spectrum of cell therapy.
14. Zhang S, Chen L, Liu T, Zhang B, Xiang D, Wang Z, Wang Y. Human umbili- Isr Med Assoc J. 2009;11:209–11.
cal cord matrix stem cells efficiently rescue acute liver failure through 33. Abumaree MH, Al Jumah MA, Kalionis B, Jawdat D, Al Khaldi A, Abomaray
paracrine effects rather than hepatic differentiation. Tissue Eng Part A. FM, Fatani AS, Chamley LW, Knawy BA. Human placental mesenchymal
2012;18:1352–64. stem cells (pMSCs) play a role as immune suppressive cells by shifting
15. Chen L, Tredget EE, Wu PY, Wu Y. Paracrine factors of mesenchymal stem macrophage differentiation from inflammatory M1 to anti-inflammatory
cells recruit macrophages and endothelial lineage cells and enhance M2 macrophages. Stem Cell Rev. 2013;9:620–41.
wound healing. PLoS ONE. 2008;3:e1886. 34. Bernardo ME, Pagliara D, Locatelli F. Mesenchymal stromal cell therapy:
16. Hermeto LC, DeRossi R, Oliveira RJ, Pesarini JR, Antoniolli-Silva AC, Jardim a revolution in regenerative medicine? Bone Marrow Transplant.
PH, Santana AE, Deffune E, Rinaldi JC, Justulin LA. Effects of intra-articular 2012;47:164–71.
injection of mesenchymal stem cells associated with platelet-rich plasma 35. Lozito TP, Tuan RS. Mesenchymal stemcells inhibit both endogenous and
in a rabbit model of osteoarthritis. Genet Mol Res. 2016. https://doi. exogenous MMPs via secreted TIMPs. J Cell Physiol. 2011;226:385–96.
org/10.4238/gmr.15038569. 36. Toh WS, Lai RC, Hui JHP, Lim SK. MSC exosome as a cell-free MSC therapy
17. Koyama N, Okubo Y, Nakao K, Osawa K, Fujimura K, Bessho K. Pluripo- for cartilage regeneration: implications for osteoarthritis treatment.
tency of mesenchymal cells derived from synovial fluid in patients with Semin Cell Dev Biol. 2017;67:56–64.
temporomandibular joint disorder. Life Sci. 2011;89:741–7. 37. Wang Y, Yu D, Liu Z, Fang Z, Dai J, Wu B, Zhou J, Heng BC, Zou XH, Ouyang
18. Kim YS, Lee HJ, Yeo JE, Kim YI, Choi YJ, Koh YG. Isolation and characteri- H, Liu H. Exosomes from embryonic mesenchymal stem cells alleviate
zation of human mesenchymal stem cells derived from synovial fluid osteoarthritis through balancing synthesis and degradation of cartilage
in patients with osteochondral lesion of the talus. Am J Sports Med. extracellular matrix. Stem Cell Res Ther. 2017;8:189.
2015;43:399–406. 38. Liu X, Yang Y, Li Y, Niu X, Zhao B, Wang Y, Bao C, Xie Z, Lin Q, Zhu L.
19. Vereb Z, Vancsa A, Pilling M, Rajnavolgyi E, Petrovski G, Szekanecz Z. Integration of stem cell-derived exosomes with in situ hydrogel glue as
Immunological properties of synovial fluid-derived mesenchymal stem a promising tissue patch for articular cartilage regeneration. Nanoscale.
cell-like cells in rheumatoid arthritis. Ann Rheum Dis. 2015;74:A64–5. 2017;9:4430–8.
20. van den Borne MP, Raijmakers NJ, Vanlauwe J, Victor J, de Jong SN, 39. Grigolo B, Lisignoli G, Desando G, Cavallo C, Marconi E, Tschon M,
Bellemans J, Saris DB. International Cartilage Repair Society (ICRS) and Giavaresi G, Fini M, Giardino R, Facchini A. Osteoarthritis treated with
Oswestry macroscopic cartilage evaluation scores validated for use in mesenchymal stem cells on hyaluronan-based scaffold in rabbit. Tissue
Autologous Chondrocyte Implantation (ACI) and microfracture. Osteoar- Eng Part C Methods. 2009;15:647–58.
thritis Cartilage. 2007;15:1397–402. 40. Liu PF, Guo L, Zhao DW, Zhang ZJ, Kang K, Zhu RP, Yuan XL. Study of
21. Mainil-Varlet P, Aigner T, Brittberg M, Bullough P, Hollander A, Hunziker human acellular amniotic membrane loading bone marrow mesenchy-
E, Kandel R, Nehrer S, Pritzker K, Roberts S, Stauffer E. Histological assess- mal stem cells in repair of articular cartilage defect in rabbits. Genet Mol
ment of cartilage repair: a report by the Histology Endpoint Committee Res. 2014;13:7992–8001.
of the International Cartilage Repair Society (ICRS). J Bone Joint Surg Am. 41. Pham PV, Bui HT, Ngo DQ, Vu NB, Truong NH, Phan LC, Le DM, Duong
2003;85(A Suppl 2):45–57. TD, Nguyen TD, Le VT, Phan NK. Activated platelet-rich plasma improves
22. Hoemann C, Kandel R, Roberts S, Saris DB, Creemers L, Mainil-Varlet P, adipose-derived stem cell transplantation efficiency in injured articular
Méthot S, Hollander AP, Buschmann MD. International Cartilage Repair cartilage. Stem Cell Res Ther. 2013;4:91.
Society (ICRS) recommended guidelines for histological endpoints for 42. Lee WJ, Maeng GH, Jeon RH, Rho GJ, Lee SL. 210 comparative characteri-
cartilage repair studies in animal models and clinical trials. Cartilage. zation of mesenchymal stem cells derived from miniature pig synovium,
2011;2:153–72. synovial fluid and bone marrow. Reprod Fert Dev. 2011;24:217.
23. Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, 43. Prado AAF, Favaron PO, Baccarin RYA, Miglino MA, Maria DA. Characteriza-
Deans R, Keating A, Prockop DJ, Horwitz E. Minimal criteria for defining tion of mesenchymal stem cells derived from the equine synovial fluid
multipotent mesenchymal stromal cells. The international society for and membrane. BMC Vet Res. 2015;11:281.
cellular therapy position statement. Cytotherapy. 2006;8:315–7. 44. Zayed M, Caniglia C, Misk N, Dhar MS. Donor-matched comparison
24. Lv FJ, Tuan RS, Cheung KM, Leung VY. Concise review: the surface of chondrogenic potential of equine bone marrow- and synovial
markers and identity of human mesenchymal stem cells. Stem Cells. fluid-derived mesenchymal stem cells: implications for cartilage tissue
2014;32:1408–19. regeneration. Front Vet Sci. 2016;3:121.
25. Hunziker EB. Articular cartilage repair: basic science and clinical pro-
gress. A review of the current status and prospects. Osteoarthr Cartil.
2002;10:432–63.
26. Bekkers J, Creemers L, Tsuchida A, van Rijen M, Custers R, Dhert W, Saris
D. One-stage focal cartilage defect treatment with bone marrow mono-
nuclear cells and chondrocytes leads to better macroscopic cartilage
regeneration compared to microfracture in goats. Osteoarthr Cartil.
Ready to submit your research ? Choose BMC and benefit from:
2013;21:950–6.
27. Caplan AI. Review: mesenchymal stem cells: cell-based reconstructive
• fast, convenient online submission
therapy in orthopedics. Tissue Eng. 2005;11:1198–211.
28. Sekiya I, Ojima M, Suzuki S, Yamaga M, Horie M, Koga H, Tsuji K, Miyaguchi • thorough peer review by experienced researchers in your field
K, Ogishima S, Tanaka H, Muneta T. Human mesenchymal stem cells in • rapid publication on acceptance
synovial fluid increase in the knee with degenerated cartilage and osteo-
• support for research data, including large and complex data types
arthritis. J Orthop Res. 2012;30:943–9.
29. Jones EA, English A, Henshaw K, Kinsey SE, Markham AF, Emery P, • gold Open Access which fosters wider collaboration and increased citations
McGonagle D. Enumeration and phenotypic characterization of synovial • maximum visibility for your research: over 100M website views per year
fluid multipotentialmesenchymal progenitor cells in inflammatory and
degenerative arthritis. Arthritis Rheum. 2004;50:817–27. At BMC, research is always in progress.
30. Weiss ML, Anderson C, Medicetty S, Seshareddy KB, Weiss RJ, VanderWerff
I, Troyer D, McIntosh KR. Immune properties of human umbilical cord Learn more biomedcentral.com/submissions
Wharton’s jelly-derived cells. Stem Cells. 2008;26:2865–74.
Content courtesy of Springer Nature, terms of use apply. Rights reserved.
Terms and Conditions
Springer Nature journal content, brought to you courtesy of Springer Nature Customer Service Center GmbH (“Springer Nature”).
Springer Nature supports a reasonable amount of sharing of research papers by authors, subscribers and authorised users (“Users”), for small-
scale personal, non-commercial use provided that all copyright, trade and service marks and other proprietary notices are maintained. By
accessing, sharing, receiving or otherwise using the Springer Nature journal content you agree to these terms of use (“Terms”). For these
purposes, Springer Nature considers academic use (by researchers and students) to be non-commercial.
These Terms are supplementary and will apply in addition to any applicable website terms and conditions, a relevant site licence or a personal
subscription. These Terms will prevail over any conflict or ambiguity with regards to the relevant terms, a site licence or a personal subscription
(to the extent of the conflict or ambiguity only). For Creative Commons-licensed articles, the terms of the Creative Commons license used will
apply.
We collect and use personal data to provide access to the Springer Nature journal content. We may also use these personal data internally within
ResearchGate and Springer Nature and as agreed share it, in an anonymised way, for purposes of tracking, analysis and reporting. We will not
otherwise disclose your personal data outside the ResearchGate or the Springer Nature group of companies unless we have your permission as
detailed in the Privacy Policy.
While Users may use the Springer Nature journal content for small scale, personal non-commercial use, it is important to note that Users may
not:
1. use such content for the purpose of providing other users with access on a regular or large scale basis or as a means to circumvent access
control;
2. use such content where to do so would be considered a criminal or statutory offence in any jurisdiction, or gives rise to civil liability, or is
otherwise unlawful;
3. falsely or misleadingly imply or suggest endorsement, approval , sponsorship, or association unless explicitly agreed to by Springer Nature in
writing;
4. use bots or other automated methods to access the content or redirect messages
5. override any security feature or exclusionary protocol; or
6. share the content in order to create substitute for Springer Nature products or services or a systematic database of Springer Nature journal
content.
In line with the restriction against commercial use, Springer Nature does not permit the creation of a product or service that creates revenue,
royalties, rent or income from our content or its inclusion as part of a paid for service or for other commercial gain. Springer Nature journal
content cannot be used for inter-library loans and librarians may not upload Springer Nature journal content on a large scale into their, or any
other, institutional repository.
These terms of use are reviewed regularly and may be amended at any time. Springer Nature is not obligated to publish any information or
content on this website and may remove it or features or functionality at our sole discretion, at any time with or without notice. Springer Nature
may revoke this licence to you at any time and remove access to any copies of the Springer Nature journal content which have been saved.
To the fullest extent permitted by law, Springer Nature makes no warranties, representations or guarantees to Users, either express or implied
with respect to the Springer nature journal content and all parties disclaim and waive any implied warranties or warranties imposed by law,
including merchantability or fitness for any particular purpose.
Please note that these rights do not automatically extend to content, data or other material published by Springer Nature that may be licensed
from third parties.
If you would like to use or distribute our Springer Nature journal content to a wider audience or on a regular basis or in any other manner not
expressly permitted by these Terms, please contact Springer Nature at
onlineservice@springernature.com
You might also like
- Transfusion MedicineDocument396 pagesTransfusion Medicinemjtjdomingo85% (26)
- IDEA GEN BIO 1 First WeekDocument4 pagesIDEA GEN BIO 1 First WeekCherrina AguilaNo ratings yet
- Review On Animal and Plant CellDocument3 pagesReview On Animal and Plant CellLadymae GalolaNo ratings yet
- Performance Task 1.2 - 3D-Cell ModelDocument2 pagesPerformance Task 1.2 - 3D-Cell ModelRy Choco100% (1)
- 10 1177@0363546519859855Document10 pages10 1177@0363546519859855a vNo ratings yet
- Fekrazad 2016Document7 pagesFekrazad 2016Basith HalimNo ratings yet
- TherapyDocument7 pagesTherapySam Bradley DavidsonNo ratings yet
- Sauer Bier 2010Document10 pagesSauer Bier 2010abdelrahman s.hassopaNo ratings yet
- Ajtr0009 3200Document13 pagesAjtr0009 3200iam_ca2No ratings yet
- Original Article: Bhaskar Vyas, Atul Shah, Anant Marathe, Ansarullah, Rajni Vyas, Ramesh BhondeDocument5 pagesOriginal Article: Bhaskar Vyas, Atul Shah, Anant Marathe, Ansarullah, Rajni Vyas, Ramesh BhondeAtul ShahNo ratings yet
- Ha Et Al. - 2021 - Human Dental Pulp-Derived Mesenchymal Stem Cell PoDocument13 pagesHa Et Al. - 2021 - Human Dental Pulp-Derived Mesenchymal Stem Cell PoEbaycustomer number01No ratings yet
- Human Adipose-Derived Stem Cells Inhibit Bioactivity of Keloid FibroblastsDocument8 pagesHuman Adipose-Derived Stem Cells Inhibit Bioactivity of Keloid FibroblastssesiaNo ratings yet
- MIEPEI 2021 2022 Artigo 1Document7 pagesMIEPEI 2021 2022 Artigo 1Eliana CorreiaNo ratings yet
- 53 1361582419reportDocument17 pages53 1361582419reportfanioNo ratings yet
- Kamei 2013Document11 pagesKamei 2013ferd dinanNo ratings yet
- Knee Stem CellsDocument25 pagesKnee Stem CellsKN TMNo ratings yet
- Assessment of Ionic and Anionic Surfactants Effect On Demineralized Osteochondral TissueDocument10 pagesAssessment of Ionic and Anionic Surfactants Effect On Demineralized Osteochondral TissueVitalie CobzacNo ratings yet
- Wu Et Al-2007-Stem CellsDocument12 pagesWu Et Al-2007-Stem CellsNinanu Nida-nnNo ratings yet
- Long-Term Effects of Fibrin Conduit With Human Mesenchymal Stem Cells and Immunosuppression After Peripheral Nerve Repair in A Xenogenic ModelDocument14 pagesLong-Term Effects of Fibrin Conduit With Human Mesenchymal Stem Cells and Immunosuppression After Peripheral Nerve Repair in A Xenogenic ModelYashar Mehrbani AzarNo ratings yet
- S - DMSO - and - Serum - Free - Cryopreservation - ofDocument16 pagesS - DMSO - and - Serum - Free - Cryopreservation - ofayisha.maharramovaNo ratings yet
- Wang 2020Document10 pagesWang 2020Norman Enrique Brenes CorderoNo ratings yet
- Fu 2013Document11 pagesFu 2013Erwin CandraNo ratings yet
- Ingeniería de TejidosDocument8 pagesIngeniería de TejidosAlo CedilloNo ratings yet
- Osteoartritis EquinaDocument4 pagesOsteoartritis EquinaparamyNo ratings yet
- Optimal In-Vitro Expansion of Chondroprogenitor Cells in Monolayer CultureDocument15 pagesOptimal In-Vitro Expansion of Chondroprogenitor Cells in Monolayer CultureKumar SingarapuNo ratings yet
- Article For DiscussionDocument9 pagesArticle For DiscussionAnthony DavisNo ratings yet
- E Ect FF of Intra-Articular Injection of Mesenchymal Stem Cells in Cartilage Repair in Experimental AnimalsDocument9 pagesE Ect FF of Intra-Articular Injection of Mesenchymal Stem Cells in Cartilage Repair in Experimental AnimalsPKNo ratings yet
- 2012 Article 9528Document9 pages2012 Article 9528Lê Thùy NgânNo ratings yet
- Mesenchymal Stem Cells Derived From Rat Bone Marrow: Techniques For Isolation, Expansion and DifferentiationDocument9 pagesMesenchymal Stem Cells Derived From Rat Bone Marrow: Techniques For Isolation, Expansion and DifferentiationMona ChasdianaNo ratings yet
- Rank - BPsDocument8 pagesRank - BPsIsteicy CortezNo ratings yet
- 2022 Article 3076Document14 pages2022 Article 3076shimos AlshareefNo ratings yet
- s12014 020 09279 6Document18 pagess12014 020 09279 6laryss.csantosNo ratings yet
- Assessing The Potential Regeneration Ability of CorpusDocument8 pagesAssessing The Potential Regeneration Ability of Corpusxhliu1992No ratings yet
- PeriodontitisDocument13 pagesPeriodontitisAida DanielaNo ratings yet
- Tissue EngineeringDocument8 pagesTissue EngineeringJimsNo ratings yet
- Implant For Autologous Soft Tissue Reconstructio - 2018 - Journal of Plastic ReDocument11 pagesImplant For Autologous Soft Tissue Reconstructio - 2018 - Journal of Plastic RePandhu HarlanNo ratings yet
- OsteoclasDocument8 pagesOsteoclasTlalli ZambraNo ratings yet
- LNC NTF3 5 Promotes Osteogenic Differentiation of Maxillary Sinus Membrane Stem Cells Via Sponging Mir 93 3pDocument12 pagesLNC NTF3 5 Promotes Osteogenic Differentiation of Maxillary Sinus Membrane Stem Cells Via Sponging Mir 93 3pBagis Emre GulNo ratings yet
- Gholobova Et Al. - Biofabrication - 2020 - Functional Evaluation of Prevascularization in One-Stage Versus Two-Stage Tissue EngineeriDocument19 pagesGholobova Et Al. - Biofabrication - 2020 - Functional Evaluation of Prevascularization in One-Stage Versus Two-Stage Tissue EngineeriLievenNo ratings yet
- Xin 2013Document5 pagesXin 2013Maximiliano PfannlNo ratings yet
- 9747010Document13 pages9747010fabio classdNo ratings yet
- Pi Is 1010518211000424Document6 pagesPi Is 1010518211000424Muthia FadhilaNo ratings yet
- MSC DIFFERENTIATIONDocument10 pagesMSC DIFFERENTIATIONBastion ReinhartNo ratings yet
- 2018 - Layer-By-Layer Cell Coating Technique Using Extracellular Matrixfacilitates Rapid Fabrication and Function of Pancreaticb-Cell SpheroidsDocument10 pages2018 - Layer-By-Layer Cell Coating Technique Using Extracellular Matrixfacilitates Rapid Fabrication and Function of Pancreaticb-Cell SpheroidsAndrés MenesesNo ratings yet
- Stem CellDocument11 pagesStem CellRush32No ratings yet
- Jurnal KJH-Derivation of Mesenchymal Stem Cells from HumanDocument9 pagesJurnal KJH-Derivation of Mesenchymal Stem Cells from HumanClarion 642No ratings yet
- 10 1016@j Biomaterials 2016 09 007Document11 pages10 1016@j Biomaterials 2016 09 007Jorge Aguirre GonzalezNo ratings yet
- ArthritsDocument27 pagesArthritsLakshmipriya GopinathNo ratings yet
- Research Article in Vitro and in VivoDocument14 pagesResearch Article in Vitro and in VivoVILEOLAGOLDNo ratings yet
- Fitzpatrick 2016Document13 pagesFitzpatrick 2016smansa123No ratings yet
- Tissue-Engineered Bone RegenerationDocument5 pagesTissue-Engineered Bone RegenerationElsa GonçalvesNo ratings yet
- Biazzo Systematic Review of RCTDocument21 pagesBiazzo Systematic Review of RCTAhmed Khaled AwadNo ratings yet
- Materials Science & Engineering C: SciencedirectDocument12 pagesMaterials Science & Engineering C: Sciencedirectmadhu kammarNo ratings yet
- A - Adipose MSC Source 1Document6 pagesA - Adipose MSC Source 1desy amediayu wardhaniNo ratings yet
- ღეროვანი უჯრედებიDocument10 pagesღეროვანი უჯრედებიIrakli GhlontiNo ratings yet
- Preparing For Cell Culture Scale-Out: Establishing Parity of Bioreactor-And Flask-Expanded Mesenchymal Stromal Cell CulturesDocument13 pagesPreparing For Cell Culture Scale-Out: Establishing Parity of Bioreactor-And Flask-Expanded Mesenchymal Stromal Cell Culturesdevin alexanderNo ratings yet
- Mesenchymal Stem Cell Isolation from Umbilical Cord TissueDocument8 pagesMesenchymal Stem Cell Isolation from Umbilical Cord TissueQuỳnh NhưNo ratings yet
- 2017년 Biomaterials xEntrDocument14 pages2017년 Biomaterials xEntrjonghyeokshin7No ratings yet
- Biomaterials That Promote Cell-Cell Interactions Enhance The Paracrine Function of MSCsDocument12 pagesBiomaterials That Promote Cell-Cell Interactions Enhance The Paracrine Function of MSCsSadie LaniganNo ratings yet
- Strategies To Capitalize On Cell Spheroid Therapeutic Potential For Tissue Repair and Disease ModelingDocument13 pagesStrategies To Capitalize On Cell Spheroid Therapeutic Potential For Tissue Repair and Disease ModelingShai FuchsNo ratings yet
- Fetal Mesenchymal Stromal Cells Secretome Regenerate Skin Wounds Via Collagen SynthesisDocument3 pagesFetal Mesenchymal Stromal Cells Secretome Regenerate Skin Wounds Via Collagen SynthesisIOSR Journal of PharmacyNo ratings yet
- Medical Engineering and PhysicsDocument11 pagesMedical Engineering and PhysicsTserendagva NyamdavaaNo ratings yet
- Braid Et Al 2018Document13 pagesBraid Et Al 2018Cahaya Carla BangsawanNo ratings yet
- Tissue Engineering and Regeneration in Dentistry: Current StrategiesFrom EverandTissue Engineering and Regeneration in Dentistry: Current StrategiesRachel J. WaddingtonNo ratings yet
- Pipino Article JCOT-10-2019Document9 pagesPipino Article JCOT-10-2019hashim_716108627No ratings yet
- Powerpick InstrumentsDocument4 pagesPowerpick Instrumentshashim_716108627No ratings yet
- Clinical Monograph: NanofractureDocument2 pagesClinical Monograph: Nanofracturehashim_716108627No ratings yet
- Marketing Operation Budget BreakdownDocument4 pagesMarketing Operation Budget Breakdownhashim_716108627No ratings yet
- Business PlanDocument42 pagesBusiness Planhashim_716108627No ratings yet
- Strategy Marketing Sales RRDocument39 pagesStrategy Marketing Sales RRhashim_716108627No ratings yet
- Marketing Operation Budget BreakdownDocument4 pagesMarketing Operation Budget Breakdownhashim_716108627No ratings yet
- Business PlanDocument42 pagesBusiness Planhashim_716108627No ratings yet
- VENDOR's REGISTRATION FORM New ExcelDocument2 pagesVENDOR's REGISTRATION FORM New Excelhashim_716108627No ratings yet
- Lesson17 Epithelial CellsDocument22 pagesLesson17 Epithelial CellsGemma WrigleyNo ratings yet
- BIOCHEM 1 Cell Biomolecules PDFDocument3 pagesBIOCHEM 1 Cell Biomolecules PDFHarold James AlcantaraNo ratings yet
- Introduction to BiochemistryDocument3 pagesIntroduction to BiochemistryJustineNo ratings yet
- Exercise-6.1: NCERT Solution For Class 9 Science - Chapter 6 TissuesDocument9 pagesExercise-6.1: NCERT Solution For Class 9 Science - Chapter 6 TissuesShah RukhNo ratings yet
- Bio 100 NotesDocument2 pagesBio 100 Notesapi-269828776No ratings yet
- FCPS Part 1 SyllabusDocument37 pagesFCPS Part 1 SyllabusMd Hasan Imam100% (2)
- Lab ReviewerDocument3 pagesLab Reviewerryana cabreraNo ratings yet
- Circulatory SystemDocument14 pagesCirculatory Systemsmbdy tbhhhNo ratings yet
- Chapter 5Document50 pagesChapter 5kebNo ratings yet
- Plant and Animal Tissue TestDocument5 pagesPlant and Animal Tissue TestSri Suhartini100% (1)
- Connective TissueDocument4 pagesConnective TissueLANGWAEMILLNo ratings yet
- Opertaor Manual GXDocument266 pagesOpertaor Manual GXGamal Abdel MoityNo ratings yet
- Cells: Structures, Functions and ComparisonDocument17 pagesCells: Structures, Functions and ComparisonDewi SallehNo ratings yet
- Exfoliative CytologyDocument1 pageExfoliative CytologyNathaniel SimNo ratings yet
- Biology LS 1001 GramStainDocument20 pagesBiology LS 1001 GramStainAshok KumarNo ratings yet
- Module 1 BiochemDocument40 pagesModule 1 BiochemAlyssa PachecoNo ratings yet
- Cell BiologyDocument60 pagesCell BiologyBhargavi SaravananNo ratings yet
- PDQ HistoDocument225 pagesPDQ HistoHtike Myat PhyuNo ratings yet
- MISCELLANEOUS BLOOD GROUP ANTIGENSDocument4 pagesMISCELLANEOUS BLOOD GROUP ANTIGENSIan Leo SantosNo ratings yet
- IFS Lecture 3 BloodDocument73 pagesIFS Lecture 3 BloodRodrigo RuizNo ratings yet
- Cabrera-Guiding Endosomal Maturation - 2010-CellDocument3 pagesCabrera-Guiding Endosomal Maturation - 2010-CellMargarita CabreraNo ratings yet
- Tarea 2 Teoríacelular López Marmolejo Clere MishellDocument3 pagesTarea 2 Teoríacelular López Marmolejo Clere Mishellclere02marmolejoNo ratings yet
- Cell Structure and FunctionDocument30 pagesCell Structure and FunctionSalman KhanNo ratings yet
- Week 6-Histopath Lab Impregnation and Embedding Impregnation Paraffin Wax ImpregnationDocument6 pagesWeek 6-Histopath Lab Impregnation and Embedding Impregnation Paraffin Wax ImpregnationAgatha A.No ratings yet
- 4-Hematology Analyzer - Detecting Erroneous Blood CountsDocument23 pages4-Hematology Analyzer - Detecting Erroneous Blood CountsRajeshNo ratings yet
- Affirmagen Affirmagen 4: OrthoDocument6 pagesAffirmagen Affirmagen 4: OrthoDominic EmerencianaNo ratings yet