Professional Documents
Culture Documents
Bronchiectasis Causes, Types, and Pathology
Uploaded by
Dawn MarcoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bronchiectasis Causes, Types, and Pathology
Uploaded by
Dawn MarcoCopyright:
Available Formats
BRONCHIECTASIS & LUNG ABSCESS 2014 -2015
Dr. constantino
Pulmonology
Bronchiectasis B. Vascular
Irregular or beaded pattern
Irreversible airway dilatation, focal or diffuse Similar to varicose veins
Affects older individual, 2/3 women
Focal C. Saccular (cystic)
- Localized, extrinsic/intrinsic obstruction Ballooned, end in blind sac
Localized depends on one segmental of
the lung or one lobe and secondary to In xray, it is very difficult to see the cylindrical or
extrinsic or intrinsic obstruction tubular pattern, what would be very visible are
Intrinsic – obstruction by an enlarged “tram tracts” appearance bronchiectatic
lymph node or parenchymal masses structures of the lung which are closed together
Extrinsic – foreign body, bronchial because of the atelectasis, they are parallel to each
tumor or tuberculosis and bronchitis other similar to “train” tracts
Diffused
- Widespread, systemic infectious process III. Etiogenesis
Consequence of inflammation and destruction of
I. Pathology structural components of bronchial wall
Destructive inflammatory changes in medium sized airway Infection is the usual cause – offending agents:
walls (segmental/subsegmental) pigments, protease and toxins injure epithelium
Mediated by neutrophils, elastase and MMO and impair mucociliary clearance
Inflammatory changes mediated by neutrophils Inflammatory response induces epithelial injury due
and the inflammatory changes they produced like to mediators
elastase and matrix metalloproteinase Allow colonization of the mucosa by bacteria and
Structural components destroyed, fibrosis subsequently produces another bout or infection
Structural components include cartilage, muscle The inflammatory produces epithelial injury
and elastic tissue and they undergo fibrosis because of the elucidation of the mediators
Dilated airways with thick purulent material Compromised protection susceptible to
Peripheral airways occluded by secretion or obliterated colonization by microorganism and bacterial growth
Traction bronchiectasis Cycle: Inflammation airway damage impaired
Dilated airways caused by parenchymal distortion clearance INFECTION
due to fibrosis so the airways are pulled apart “VICIOUS CYCLE HYPOTHESIS
because of the fibrosis Infection inflammation subsequent
airway damage with empiric clearance of
II. Histology secretions susceptible again to infection
Bronchial and peribronchial inflammation and fibrosis which develops another bout of infection
ulceration of bronchial wall This is a cycle that goes on and on, and that
squamous metaplasia is the reason why there is CHRONIC
Mucous gland hyperplasia INFLAMMATION IN BRONCHIECTASIS
You have a lot of changes in the wall with variant As time goes on, it progresses involving
degrees of injury more areas of the lung which subsequent
Involved area: combination of fibrosis, emphysema, changes also in pulmonary function
bronchopneumonia, atelectasis resulting to symptoms
Involved area supplied by the affected bronchus
Increased vascularity, enlargement of bronchial artery and IV. Etiology
anastomosis of the bronchial and pulmonary circulation A. Infectious
Reason why bleeding is the common problem in
bronchiectasis Primary
Most important – VIRUSES AND BACTERIA
Viruses – adenoviruses and inflammatory virus
Adenoviruses and influenza virus were the
Patterns: most implicated in the development of
A. Cylindrical or tubular pattern bronchial inflammation and destruction and
Uniform dilatation and ends disruption subsequent bronchiectasis formation
Bacteria
Magno Opere Somnia Dura Page 1 of 6 MAYI
BRONCHIECTASIS & LUNG ABSCESS 2014 -2015
Dr. constantino
Pulmonology
Especially with necrotizing organism like Kartganer’s Syndrome Triad:
staph and klebsiella would lead to bronchiectasis, situs inversus, sinusitis
bronchiectasis especially is treatment is not Ciliary movement is also needed for
given or delayed proper location of the viscera during
Staph embryonic development, so if you have
Klebsiella delayed treatment impaired ciliary movement abnormal
Bordetella childhood location SITUS INVERSUS in
Common bronchiectasis in childhood Kartagener’s syndrome
TB direct/indirect CF (Cystic Fibrosis) : thick tenacious secretions
Common cause of bronchiectasis in the impair mucocilary clearance subsequent
Philippines bacterial colonization chronic infection
Direct: due to parenchymal destruction due
to the TB infection B. Non Infectious
Indirect: either by extrinsic compression of Toxic exposure
the bronchus by enlarged lymph nodes or More common
endobronchial obstruction because of Leads to a severe inflammatory response that
bronchostenosis would subsequently injured the bronchial
MOTT: 1 or 2 infection mucosa
HIV recurrent bacterial infection Gas inhalation (ammonia), acid aspiration
Due to immunodeficient status of In gastric acid aspiration – lungs don not only
the patient exposed to gastric acid but also the bacteria
secondary bacterial infection
Secondary Immune response trigger inflammation and
Localized impairment of host defenses subsequent destruction of tissue
Endobrochial obstruction chronic Example: allergic bronchopulmonary
infection aspergillosis (ABPA)
Most common Syndrome wherein there is aspergillosis in the
Endobronchial obstruction – cannot clear lungs and asthma like manifestations
organism or secretions involved in lung α -1 antitrypsin deficiency – occ. Bronchiectasis
segments bacterial colonization Yellow nail syndrome – hypoplastic lymphatics
CHRONIC INFECTION bronchial mucosal Pleural effusion and yellowish discoloration of
injury the nails
Generalized impairment of pulmonary defense
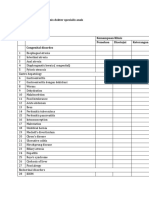
Immunoglobulin deficiency state Table 258-1 Major etiologies of Bronchiectasis and
IgG (IgG2) Proposed work up
Panhypogammaglobulinemia: skin/sinus Focal : Obstruction Bronchoscopy – if suspecting
infection obstruction in bronchiectasis
These two are the most common Diffused:
PCD: 5-10% causes recurrent upper/lower RT, Infection
abnormal radial spokes, dysnein arms, Gram’s stain/culture
microtubules If difficult to identify Bronhoscopy
PCD – primary ciliary dyskinesia with bronchoalveolar lavage
Recurrent upper/lower RT – remember Immunodeficency syndromes
cilia is needed in the mucociliary Immunoglobulin methods to test for HIV
movement so if you have dyskinetic Genetic causes
cilia, you will have impaired mucociliary CF measurement of swear chloride
clearance levels
Abnormal radial spokes, dynein arms Kartagener’s syndrome biopsy of th
and microtubules – part of the ciliary bronchial and submucosal and look at
apparatus the cilia if it’s abnormal
Autoimmune causes
Males – infertile Workup for connective tissue diseases
Because ciliary movement is also Recurrent aspiration
needed for sperm motility Test for swallowing if there is impaired
50% kartagener’s syndrome swallowing
Magno Opere Somnia Dura Page 2 of 6 MAYI
BRONCHIECTASIS & LUNG ABSCESS 2014 -2015
Dr. constantino
Pulmonology
CXR (tubular): behind the cardiac shadow,
you will see the prominent bronchial
V. Clinical Manifestation: markings close to each other due to
Persistent productive cough, thick, tenacious sputum atelectasis
and history of purulent respiratory cough infection Chest CT Scan
Reason why patient come back a lot of Modality of choice
times because of chronic productive Especially the high resolution CT Scan
cough In ordinary CT scan, you cannot see the
Different from chronic bronchitis, in the tubular pattern of BE but with HRCT you
sense of usually a patient has a lot of can see all types of BE
sputum upon waking up in the morning. “tram tracks”
Reason is that when they sleep the Signet ring sign
secretion pooled in the lungs so when Due to the enlarged bronchus which is
they wake up they cough out and about 1.5 times bigger than the
produce copious amount of sputum In adjacent vessel, parang may maliit tapos
the morning malaki
Dry type bronchiectasis – upper lobes Tree in bud appearance
Usually involves upper lobes especially in synonymous to secretions which filled
tuberculosis up the bronchiectatic segment
Dry – cough is non-productive Cystic infiltrate
Hemoptysis – 50-70% due to friable mucosa,
hypertrophied bronchial artery VII. Approach
Remember in BE, you have Clinical history
hypervascularization and enlargement of Approach is more of clinical history
the bronchial arteries with anastomosis to Get the history of recurrent infection –
the bronchial and pulmonary aterial skin or sinus infection especially if there
circulation is immunoglobulin deficiency
Bleeding may be arterial – massive History of chronic productive cough
hemoptysis >200ml of blood with copious amount of sputum
PE: crackles, rhonchi, wheezing, clubbing production because during
Clubbing because of the presence of chronic exacerbation of chronic BE, wherein
inflammation in the lungs they have infection, there is increase
PFT: mild to moderate airway obstruction volume of secretion with increase
Pulmonary function testing like spirometry purulence
Mild to moderate obstruction – means that Chest imaging
BE is an obstructive disease CXR is very important
One clue that there is BE in CXR
VI. Diagnosis persistence of pulmonic infiltrates even
CXR: “tram tracks” indicate dilated airways and after treatment
sometime cystic lucencies Pneumonia is resolved with treatment after
One feature would be the prominent 3 weeks, so if CXR is repeated and there is
bronchial markings because of the still presence of pneumonia in the same
peripheral inflammation and they would place, then after 2 or 3 months if CXR is
reach up to periphery of the lungs repeated still present Possible BE
Normally, there is tapering of the Differentiated from obstructive pneumonia
pulmonary marking, but once they reach pneumonia will present even with
the 2/3 of the lng zone, it is not seen treatment
anymore Work up for etiology including diffuse bronchiectasis
“tram tracks appearance – 2 enlarged Diffuse BE – more of systemic disease
bronchi parallel to each other involved, so a lot of examinations is needed
Typical appearance: combination of tubular Bronchoscopy to rule out obstruction
and cystic BE Obstruction – may be a tumor or foreign
CXR (varicose type of BE): irregular beaded body
pattern, parang beads Example: story about a patient, young male
who present with history of recurrent
Magno Opere Somnia Dura Page 3 of 6 MAYI
BRONCHIECTASIS & LUNG ABSCESS 2014 -2015
Dr. constantino
Pulmonology
cough, bronchoscopy was done earring with α-1 antitypsin deficiency, if they
of his girlfriend was found (pano nangyari do have BE, most of the time they
yun? Di ko maimagine. Hehe. Medyo develop emphysema
hardcore ) After removal, condition Aspergillus serum testing – especially
resolves but has some degree of permanent if the patient has symptoms of
damage because of the chronic infection asthma
PFT for functional assessment Rheumatic disease serology –
Because BE is an obstructive lung disease because the rheumatoid arthritis is
bronchial obstruction reversible with related to BE also
bronchodilator HIV screening
IX. Treatment
VIII. Algorithm Control of active infection
They often have repeated bouts of bacterial
infection increased sputum production,
increased purulence of sputum, may or may
not have fever so treat the infection with
antibiotics
Improvement in secretion, clearance and bronchial
hygiene
Done by doing Chest physiotherapy and
mucolytics to improve secretions
Chest physiotherapy would consists of chest
tapping or percussion and postural drainage
Decrease microbial load and minimize recurrent
infection
By giving cyclic antibiotics for severe cases
A. Antibiotic treatment
For causative and presumptive pathogen
Antibiotic course would depend on the type
of BE
Evaluation of GERD/aspiration – because One antibiotic to be used should cover
these are some of the common cause of Pseudomonas common pathogen in BE
chronic cough 7-10 days
If CT scan is abnormal, in focal BE – consider Consider treating NTB (MAC)
bronchoscopy because obstruction may be Can cause primary or secondary
due to a tumor or a foreign body. And do infection in cases of BE
induced sputum for acid fast bacilli –
because one cause of obstruction is B. Bronchial hygiene
endotracheal tuberculosis Hydration
If diffuse BE: Mucolytics
Quantitative immunoglobulin analysis Bronchodilator aerosolzation
– to determine if it’s due to Not only improve airway
immunodeficiency obstruction but also improves
Sputum examination for tuberculosis mucociliary clearance
– because disseminated TB can lead Chest physiotherapy (postural
to BE drainage/pneumonia)
Studies of ciliary morphology and Proteolytic damage (Dnase) – CF related BE
function – by doing biopsies of the
nasal and bronchial cilia C. Anti-inflammatory treatment
Semen analysis – because it is The control of inflammation in BE may be
involved in primary ciliary dyskinesia beneficial
α-1 antitypsin level – especially if Inhaled GC: decreased dyspnea, dec. β
pateients are young, remember, BE agonist, dec. sputum production
affects older individuals but in patient
Magno Opere Somnia Dura Page 4 of 6 MAYI
BRONCHIECTASIS & LUNG ABSCESS 2014 -2015
Dr. constantino
Pulmonology
Ex: Bumesonide, meticazone ? But in diffused BE, better option would
(sound like) be bronchial artery embolization
No significant difference in lung function on
exacerbation whether GC is use or not Prognosis:
Risk of immunosuprresive adrenal Vary with underlying etiology, frequency of
suppression exacerbation and --- pathology
Oral/systemic GC may be important in If etiology is more serious, more
ABPA, AI chronic or untreatable POOR
Autoimmune disease like PROGNOSIS because BE will progress
Sjogren’s syndrome or as time goes on and since it is
rheumatoid arthritis progressive, lung function is
compromised which is also
D. Refractory cases/complication progressive, patient may become
Surgery of focal disease dependent to oxygen and then
Surgery may be done for focal develop COR PULMONALE death
disease especially if you have from respiratory failure
bothersome symptoms like If etiology is treatable like
chronic productive cough that immunoglobulin defiency,
may interfere In the work (e.g. immunoglobulin is given GOOD
patient is a “GRO” nakakandong PROGNOSIS
sa client ubo ubo Kat GRO
ngaaa ) Prevention:
Surgery will just involved the Dec. risk of recurrent infection
affected lobe Reversal immunodeficient state
Transplant for advanced cases Risk of infection can be decreased by vaccination
For very severe advanced cases of BE, lung Smoking cessation
transplant is an option smoking contributes to the decrease
Criteria for lung transplant donors is very mucociliary clearance Infection
strict – no systemic diseases, no lung
disease E. Suppresive antibiotics
Oral antibiotics given for 1-2 months
Complication: Antibiotics should be rotated – give
Repeated antibiotic resistance different antibiotics not the same
Go back to the more primitive antibiotics for several months to minimize
antibiotics antibiotic resistance
rd
Instead of using 3 generation Marcolides may be added for 3 times a
cephalosporins or new generation week for acute inflammation
quinolone COTRIMOXAZOLE, Aerosolized antibiotics to reduce side effect
FLUOROQUINOLONES (?) earlier Reduces S/E since these are not absorbed
antibiotics because they have not been clinically
use for a long time there is no Intermittent IV antibiotics for severe infection or
resistance from these drugs resistance pathogens
Toxicity from antibiotic combination
Because of the multiple antibiotics LUNG ABSCESS
used renal or hepatotoxicity
Hemoptysis may require bronchial arterial Microbial lung infection that result in
embolization or surgery parenchymal necrosis
Usually managed by providing an Usually 3 diameter or 2 cm
adequate airway Multiple abscesses <2cm NECROTIZING
Bronchoscopy is done to know the PNEUMONIA
source of the bleeding Classifications:
Balloon catheter is used to stop the Acute
bleeding Chronic 4-6 weeks
But in focal BE wherein the bleeding is Cut off point for chronicity: 4 weeks
massive surgery (lobectomy)
Magno Opere Somnia Dura Page 5 of 6 MAYI
BRONCHIECTASIS & LUNG ABSCESS 2014 -2015
Dr. constantino
Pulmonology
Presence of underlying lesions: Problem is the presence of anaerobic
a. Primary – no underlying lesion bacteria and the possibility of rupturing
b. Secondary the abscess
There is an underlying lesion like
tumor obstructing the bronchus or IV. Treatment
systemic condition that could lead to Depends on pressumed or established etiologies
necrotizing pneumonia Before, Pen G was the DOC for Lung
Non-specific lung abscess abscess but because of the freuquency of
unrecovered pathogen bacteria which produce beta-lactamase,
Usually secondary to anaerobic Pen G was not used anymore
organism
Putrid lung abscess anaerobic Clindamycin 600 mg IV QID 300 PO QID (once
bacteria symptoms subside, become afebrile )
Putrid lung abscess have foul smelling Duration depends on the condition of the
sputum patient, sometimes it is given for 4-6
I. Etiology weeks
Anaerobes – most non-specific lung abscess β-lactam/ β-lactamase inhibitors
Major contributor to lung abscesses Beta-lactam combination like amoxicillin +
Pathogens are not recovered because clavilanate (?) commonly known as CO-
of the use of anaerobic culture AMOXICLAV
Mycobacteria Carbapenem
Important cause of lung abscess, especially Used because of the anti-pseudomonal
in the Phils. Where TB is a common activity but the problem is the anaerobic
problem activity may not be so good
Staph aureus – acute LA, post influenza Metronidazole
Highly necrotizing Good drug for anaerobic bacteria but it
Implicated in acute LA especially after a has no effect on aerobic bacteria which is
bout of influenza a common organism in lung abscess so it is
Fungi/parasites not a DOC
Vancomycin
Table 258-2 Microbial Patthogens causing cavitary lung Used if S. aureus is considered as the
infection cause of Lung abscess
Aspiration-prone host – those who have an S. aureus abscess multiple lung
impaired cough reflex abscesses due to the spread of s. aureus
due to bacteremic effect that’s why it is
II. Clinical features multiple abscesses
Indolent infection, chronic infection which may have
a duration from days to weeks in a host predisposed V. Failure of treatment
to aspiration Fever – 5-7 days after treatment
Fatigue, cough, sputum production and fever Progression of infiltrate
Weight loss, anemia and leukocytosis Consider obstruction, complications like empyema, and
possibility of drug resistance
III. Diagnosis Surgery – for treatment failure, especially if due to
CXR neoplasm or hemorrhage
Very important diagnostic tool Percutaneous drainage
Air-fluid level By doing CT scan guided
Very large abscess Lobectomy
Microbiologic studies: gram stains, cultures including For cases of neoplasm and hemorrhage
fungi and mycobacteria
To identify pathogen for appropriate treatment
Fungi and bacteria study especially for patient who
have immunodeficient state
Pleural fluid
If pleural effusions is present
BAL (bronchoalveolar lavage)
Magno Opere Somnia Dura Page 6 of 6 MAYI
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- ReflectionDocument1 pageReflectionDawn MarcoNo ratings yet
- Zoom Basic GuideDocument26 pagesZoom Basic GuideDawn MarcoNo ratings yet
- Anatomy Is LoveDocument21 pagesAnatomy Is LoveDawn MarcoNo ratings yet
- AssignmentDocument5 pagesAssignmentDawn MarcoNo ratings yet
- NCM BioethicsDocument1 pageNCM BioethicsDawn MarcoNo ratings yet
- Macatangay, Ruth D.: 103 Love of Wisdom ApplicationDocument2 pagesMacatangay, Ruth D.: 103 Love of Wisdom ApplicationDawn MarcoNo ratings yet
- Measure Area Volume Mass ConversionDocument1 pageMeasure Area Volume Mass ConversionDawn MarcoNo ratings yet
- Activity #1 Livelihood A Cheese Stick MakingDocument7 pagesActivity #1 Livelihood A Cheese Stick MakingDawn MarcoNo ratings yet
- UntitledDocument1 pageUntitledDawn MarcoNo ratings yet
- List of Emergencies 2017Document1 pageList of Emergencies 2017Dawn MarcoNo ratings yet
- CHNDocument3 pagesCHNDawn MarcoNo ratings yet
- Macatangay, Ruth D.: 103 Love of Wisdom ApplicationDocument2 pagesMacatangay, Ruth D.: 103 Love of Wisdom ApplicationDawn MarcoNo ratings yet
- Management of Septic ShockDocument31 pagesManagement of Septic ShockDawn MarcoNo ratings yet
- Dave's ProposalDocument1 pageDave's ProposalDawn MarcoNo ratings yet
- POTT's DiseaseDocument18 pagesPOTT's DiseaseDawn MarcoNo ratings yet
- Drug StudyDocument10 pagesDrug Studyjho_No ratings yet
- NURS 451 Critical Care Case Study PaperDocument20 pagesNURS 451 Critical Care Case Study PaperDawn Marco100% (1)
- UntitledDocument1 pageUntitledDawn MarcoNo ratings yet
- UntitledDocument1 pageUntitledDawn MarcoNo ratings yet
- Campaign For Best Practice in Intravenous TherapyDocument2 pagesCampaign For Best Practice in Intravenous TherapyDawn MarcoNo ratings yet
- UntitledDocument1 pageUntitledDawn MarcoNo ratings yet
- Drug StudyDocument10 pagesDrug Studyjho_No ratings yet
- UntitledDocument1 pageUntitledDawn MarcoNo ratings yet
- DrugsDocument3 pagesDrugsDawn MarcoNo ratings yet
- UntitledDocument1 pageUntitledDawn MarcoNo ratings yet
- Laws Affecting The Practice of Midwifery and NursingDocument4 pagesLaws Affecting The Practice of Midwifery and NursingDavid RobertNo ratings yet
- Laws Affecting The Practice of Midwifery and NursingDocument4 pagesLaws Affecting The Practice of Midwifery and NursingDavid RobertNo ratings yet
- Campaign For Best Practice in Intravenous TherapyDocument2 pagesCampaign For Best Practice in Intravenous TherapyDawn MarcoNo ratings yet
- UntitledDocument1 pageUntitledDawn MarcoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Bronchiectasis: PathophysiologyDocument3 pagesBronchiectasis: PathophysiologyBharat Singh BanshiwalNo ratings yet
- CF Lecture 2Document8 pagesCF Lecture 2Maha KhanNo ratings yet
- BronchiectasisDocument61 pagesBronchiectasisRapid MedicineNo ratings yet
- BronchiectasisDocument16 pagesBronchiectasisRaras RavenclawwNo ratings yet
- Internal Medicine 2015 Cardiology Part ReviewDocument24 pagesInternal Medicine 2015 Cardiology Part ReviewMargaret ThatcherNo ratings yet
- Pulmonary Disease Study Guide For Exam IDocument2 pagesPulmonary Disease Study Guide For Exam Iulka07No ratings yet
- Toxicology Reports: Brent D. Kerger, M. Joseph FedorukDocument10 pagesToxicology Reports: Brent D. Kerger, M. Joseph FedorukPetrescu MihaiNo ratings yet
- Krok 2 Medicine (EN) Attempt review 1Document52 pagesKrok 2 Medicine (EN) Attempt review 1IS ZDNo ratings yet
- Asthma: Differential Diagnosis and ComorbiditiesDocument9 pagesAsthma: Differential Diagnosis and ComorbiditiesQuel PaivaNo ratings yet
- Cystic Fibrosis Late Diagnosis A Case ReportDocument3 pagesCystic Fibrosis Late Diagnosis A Case ReportVivi DeviyanaNo ratings yet
- Rempe 2007Document5 pagesRempe 2007aristyadewi414No ratings yet
- FinalProgram PDFDocument452 pagesFinalProgram PDFGurzu IrinaNo ratings yet
- Tropics - Infectious DiseasesDocument1,194 pagesTropics - Infectious DiseasesSabera KapasiNo ratings yet
- Chapter 4 BronchiectasisDocument10 pagesChapter 4 BronchiectasisAlmira SiamNo ratings yet
- CopdDocument89 pagesCopdVijayalaxmi KathareNo ratings yet
- Bronchiectasis Physiotherapy Assessment Form 2Document4 pagesBronchiectasis Physiotherapy Assessment Form 2jefferyNo ratings yet
- Cytokine Levels Correlate With A Radiologic ScoreDocument6 pagesCytokine Levels Correlate With A Radiologic ScoresuryoNo ratings yet
- Case Studies GeneticsDocument139 pagesCase Studies GeneticsShammah Cecilia NassaliNo ratings yet
- Lateral thinking in MRCP PACES examDocument73 pagesLateral thinking in MRCP PACES examSagit Nauman81100% (1)
- Non-Cystic Fibrosis Bronchiectasis: Diagnosis and Management in 21st CenturyDocument10 pagesNon-Cystic Fibrosis Bronchiectasis: Diagnosis and Management in 21st CenturyIvan VeriswanNo ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument16 pagesChronic Obstructive Pulmonary DiseaseAlberto MedinaNo ratings yet
- Evaluation Checklist Case 7 Bronchial AsthmaDocument7 pagesEvaluation Checklist Case 7 Bronchial AsthmaChristian MendiolaNo ratings yet
- GMO Amendment 2008Document91 pagesGMO Amendment 2008Anil N AnilNo ratings yet
- AFP Hemoptysis - 2022Document9 pagesAFP Hemoptysis - 2022Joshua DiaoNo ratings yet
- Rincian Kewenangan Klinis Dokter Spesialis AnakDocument6 pagesRincian Kewenangan Klinis Dokter Spesialis AnakHikmah AmaliaNo ratings yet
- Nursing Care Plan (Bronchiectasis)Document4 pagesNursing Care Plan (Bronchiectasis)Leah QuiñanolaNo ratings yet
- ECOLOGIC MODEL ANALYZES BRONCHIECTASISDocument4 pagesECOLOGIC MODEL ANALYZES BRONCHIECTASISrodolfo opidoNo ratings yet
- Copd Case StudyDocument6 pagesCopd Case StudyDivine ParagasNo ratings yet
- Respiratory QuestionDocument79 pagesRespiratory QuestionTofik Mohammed100% (2)
- Focused Exam For CoughDocument3 pagesFocused Exam For CoughBrandon Georges (Scribblemeascript)No ratings yet