Professional Documents
Culture Documents
Hypocalcemia
Uploaded by
Jezreel Bona0 ratings0% found this document useful (0 votes)
4 views4 pagesCopyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views4 pagesHypocalcemia
Uploaded by
Jezreel BonaCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 4
CALCIUM (Ca) - Most active form is called calcitriol.
Minimum daily requirement 800 mg/day Increases calcium absorption from intestine and
Higher among adolescents and young adults acids PTH in mobilizing bone calcium.
because they are still growing. Enhances calcium and phosphorus availability
Pregnant, lactating women, post-menopausal for new bone formation.
women and adults older than age 65, have low
calcium levels.
Distribution of calcium in the body
99% of calcium found in bones and teeth.
(Calcium makes bones and teeth durable)
1% of calcium in Extra Cellular Fluid
o Normal serum calcium (total serum
calcium) level 4.5-5.5 mEq/L (9-11
mg/dl)
53% of calcium in ECF is bound to protein,
mainly albumin. (It cannot cause capillary
membranes to leave the vascular system.)
Ionized calcium (iCa) accounts for 47% serum
This illustration of maintaining calcium balance
calcium. (Calcium dissolved in plasma is
considered physiologically active because it
Extracellular calcium levels are normally kept
crosses cell membranes)
constant by several interrelated processes that move
o Normal value of iCa: 2.2-2.5 mEq/L
calcium ions into and out of ECF. Calcium enters the
(4.5-5.0mg/dl)
extracellular space through resorption of calcium ions
from bone through the absorption of dietary calcium in
Calcium deposited in bones in teeth
the GI tract and through reabsorption of calcium from
Maintenance of skeletal elements.
the kidneys. Calcium leaves ECF as it is excreted in stool
and urine, and deposited in bone tissues.
Ionized calcium
Regulation of neuromuscular activity
HYPOCALCEMIA (Calcium Deficit)
Regulates cell membrane permeability.
- Characterized by serum calcium less than 4.5
Regulates transmission of nerve impulse.
mEq/L.
Regulates muscle contraction and relaxation.
Influences enzyme activity. (Activates enzymes)
Medical Definition
Other roles: functions in blood coagulation by
HYPO: Low
converting prothrombin to thrombin; a
CALC: Calcium
necessary part of material that holds cell
together. EMIA: In the blood
o Calcium less than 9.0 mg/dl
Normal Regulation of Calcium Levels
Bone resorption CALCIUM
Renal absorption
Regulated by 3 main hormones:
Intestinal absorption.
1. Parathyroid hormone
Parathyroid hormone (PTH)
- Increases calcium concentration in the blood.
- When serum calcium level is low in the blood.
2. Calcitonin hormone
Promotes transfer of Ca from bone to plasma.
- Decreases blood calcium.
Promotes absorption of Ca from small intestine.
- Puts a ton of calcium into the bones.
Enhances renal absorption of Ca.
Secreted in response to low serum Ca levels.
3. Calcitriol
- Controls blood calcium by stopping or inhibiting
Calcitonin (thyrocalcitonin)
the release of calcitonin.
- Hormone produced by thyroid gland.
- Reverses the ton of calcium in the bone so
calcium gets released into the blood stream.
Promotes transfer of calcium from plasma to
bone.
Best friend = Magnesium
Secreted in response to high serum calcium
levels. Calcium helps build job functions for
magnesium often when magnesium is low.
Vitamin D
- Ingested in food or synthesized in the body. Worst Enemy = Phosphate
When phosphate is low, calcium is high and vice o Magnesium sulfate, Propylthiouracil
versa. (PTU - for hypothyroidism), Colchicine
(Antigout), Plicamycin, Neomycin,
The function of Calcium is to keep the 3 B’s strong: excessive sodium citrate.
These agents inhibit
1. Bones parathyroid hormone secretion
2. Blood – The clotting factors will be strong. and decrease serum calcium
3. Beats – Heartbeats level.
o Acetazolamide (for acute altitude
Pathophysiology & Etiology sickness), Aspirin (Anticoagulant),
Dietary Factors Anticonvulsants, Estrogens,
- Sources of calcium. Aminoglycosides, Gentamycin, Amikacin
- Inadequate intake of food rich in calcium. These agents can alter the
o Inadequate calcium in food vitamin D metabolism that is
o Lack of vitamin D needed for calcium absorption.
o Inadequate protein in diet o Phosphate preparations (Sodium
phosphate, Potassium phosphate)
GI Factors Can increase the serum
- May interfere with the absorption of calcium phosphorus level and decrease
from the gut. the serum calcium level.
o Decreased absorption due to o Corticosteroids
pancreatitis May also decrease calcium
o Crohn’s disease mobilization and inhibit the
chronic inflammatory bowel absorption of calcium.
disease (IBD) of unknown origin o Loop diuretics (furosemide, Lasix)
which usually affects the ilium Reduce calcium absorption
and colon. from the renal tubules.
o Resection of small bowel
o Chronic diarrhea Other Causes
o Alcoholism
Hormonal Factors o Medullary thyroid carcinoma
- Regulate calcium levels Alter the functions of thyroid
o PTH deficiency (usually the main cause and parathyroid glands.
often secondary to sepsis, burns, and o Rapid infusion of banked blood during
surgery like parathyroidectomy, transfusion
thyroidectomy, radical neck dissection.) Because of increased number of
o Vitamin D deficiency (may be r/t renal sodium citrate.
failure)
Causes
Other electrolyte imbalances L – ow Parathyroidism
o Magnesium deficiency o PTH increased blood calcium
less than 1 mg/dl History of Thyroidectomy (check the
When magnesium goes down calcium levels)
so does calcium. o Pancreatitis
o Increased serum phosphorus O – ral meds
often due to renal failure o PTH increased blood calcium
As serum phosphorus increase, o Laxatives, Loop Diuretics (furosemide)
serum calcium decreases. o Corticosteroids
o Alkalosis o Antiseizure meds (Dilantin (Generic =
resulting in increased protein Phenytoin), Phenobarbital)
bound calcium with less than o Phosphate enemas
ionized calcium available even o Citrate
when total serum calcium is W – ound drainage
normal. o GI Wounds
o Increased serum albumin o Higher risk for low calcium
may result in increase in bound C – hronic diseases
calcium. Thus, serum calcium o Celiac & Crohn’s disease
decreases. o Chronic kidney issues (excessive
o Rapid dilution of plasma with calcium excretion of calcium)
free solution. o Diuretics & Corticosteroids
A – ntibiotics
Drugs predisposing to hypocalcemia L – ow Vitamin D & Low Magnesium
I – ncreased Phosphate levels in the blood
Chronic Hypocalcemia
Signs and Symptoms -exist for more than six (6) months.
Vary widely from client to client based on Osteoporosis (loss of bone mass)
severity, duration, and rapidity of onset. o Due to prolonged low calcium intake.
When hypokalemia is present, symptoms are o Serum calcium levels are normal, but
potentiated. total body calcium is decreased.
o Increased incidence of skeletal
Neuromuscular signs fractures.
o Tetany, including neural excitability
o Tingling and muscle spasms of mouth, hands, Treatment & Management
and feet, and larynx in severe hypocalcemia. Emergency measures: administration of
o Trousseau’s sign parenteral calcium salts such as:
o Chvostek’s sign o Calcium gluconate
o Calcium chloride
Classic Physical Examination Findings o Calcium gluceptate diluted with 5%
o Chvostek’s sign dextrose in water.
Twitching of facial muscles in Mild or chronic hypocalcemia:
response to tapping over the o Foods high in calcium
facial nerve area. o Oral calcium supplements
This test is neither sensitive or o Vitamin D supplements
specific. o Increased protein in diet
Absent in about 30% of patients
with hypocalcemia. Nursing Process/Nursing Assessment
Present in 10% of patients with Obtain client history relative to potential causes
normal levels of calcium. of hypocalcemia.
o Trousseau’s sign Obtain client history relative to drugs
Development of carpopedal predisposing to hypocalcemia.
spasm that results from Assess for signs of hypocalcemia.
ischemia. One way to induce Obtain baseline values for serum calcium,
the ischemia is the application ionized calcium, serum albumin, and acid-base
of a blood pressure cuff that status.
gets inflated over the arm and Obtain baseline ECG, noting abnormalities in S-T
gradual flexion of the fingers segment and Q-T interval.
and thumb, and the wrist, and Take safety precautions if client is confused or
some degree of pronation hallucinating.
occurs. Prepare to adopt seizure precautions if
This test is more sensitive and hypocalcemia is severe.
specific.
Present in 94% of the patients Nursing Diagnoses
with hypocalcemia. Altered nutrition related to inadequate intake
Only occurs in about 1% of of calcium, vitamin D, or protein
patients with normal calcium.
Altered nutrition relative to inadequate calcium
absorption
CNS Changes
High risk for injury, bleeding, related to
o Irritability
interference with coagulation secondary to
o Anxiety calcium loss.
o Delusions
o Hallucinations Nursing Interventions
o Memory impairment Monitor laboratory test results, with emphasis
o Depression on serum and ionized calcium.
o Convulsions Monitor ECG for changes in pattern.
When calcium is given parentally, monitor for
Cardiovascular Changes irritation of subcutaneous tissue and tissue
o Gross changes: weak contractions, potential for sloughing.
CHF Teaching client to eat high-calcium foods;
o ECG abnormalities: S-T segment lengthened, Q- educate client concerning prevention of
T interval prolonged osteoporosis.
Educate client concerning proper, moderate
Changes in Laboratory Test Values use of laxatives and antacids.
o Serum calcium is decreased Monitor for signs of cardiac arrythmia in clients
o Ionized calcium decreased receiving digitalis and calcium supplements
o Blood-clotting time is increased (either oral or I.V.)
Monitor for hypocalcemia in clients receiving
massive transfusions of citrated blood.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Or 1Document4 pagesOr 1Jezreel BonaNo ratings yet
- Group 10 NCM 112 - (Osteonecrosis)Document8 pagesGroup 10 NCM 112 - (Osteonecrosis)Jezreel BonaNo ratings yet
- Osteonecrosis: Avascular NecrosisDocument8 pagesOsteonecrosis: Avascular NecrosisJezreel BonaNo ratings yet
- HypocalcemiaDocument4 pagesHypocalcemiaJezreel BonaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Practical Cookery 14th Edition SAMPLEDocument16 pagesPractical Cookery 14th Edition SAMPLETendaiNo ratings yet
- Ifm Product Innovations PDFDocument109 pagesIfm Product Innovations PDFJC InquillayNo ratings yet
- Signage Method of Statement and Risk AssessmentDocument3 pagesSignage Method of Statement and Risk AssessmentNajmal AmanNo ratings yet
- 2023 VGP Checklist Rev 0 - 23 - 1 - 2023 - 9 - 36 - 20Document10 pages2023 VGP Checklist Rev 0 - 23 - 1 - 2023 - 9 - 36 - 20mgalphamrn100% (1)
- Distribución Del Mercurio Total en Pescados y Mariscos Del Mar ArgentinoDocument15 pagesDistribución Del Mercurio Total en Pescados y Mariscos Del Mar ArgentinoaldiNo ratings yet
- Grounds of Divorce Under Hindu Religion or Hindu Law Unit-A: Chapter-IiDocument42 pagesGrounds of Divorce Under Hindu Religion or Hindu Law Unit-A: Chapter-IiSatyam PathakNo ratings yet
- Equine Anesthesia Course NotesDocument15 pagesEquine Anesthesia Course NotesSam Bot100% (1)
- Annex 9: Guide To Good Storage Practices For PharmaceuticalsDocument12 pagesAnnex 9: Guide To Good Storage Practices For PharmaceuticalsRyan Noel Perez de TagleNo ratings yet
- Depression List of Pleasant ActivitiesDocument3 pagesDepression List of Pleasant ActivitiesShivani SinghNo ratings yet
- Corn Fact Book 2010Document28 pagesCorn Fact Book 2010National Corn Growers AssociationNo ratings yet
- BARCODESDocument7 pagesBARCODESChitPerRhosNo ratings yet
- February 2019Document4 pagesFebruary 2019sagar manghwaniNo ratings yet
- Week 1 Seismic WavesDocument30 pagesWeek 1 Seismic WavesvriannaNo ratings yet
- Pet 402Document1 pagePet 402quoctuanNo ratings yet
- Medical Representative Healthcare Sales in Fort Myers FL Resume Greg HejlikDocument2 pagesMedical Representative Healthcare Sales in Fort Myers FL Resume Greg HejlikGregHejlikNo ratings yet
- Espiritualidad AFPP - 2018 PDFDocument5 pagesEspiritualidad AFPP - 2018 PDFEsteban OrellanaNo ratings yet
- Api 579-2 - 4.4Document22 pagesApi 579-2 - 4.4Robiansah Tri AchbarNo ratings yet
- Assignment Nutrition and HydrationDocument17 pagesAssignment Nutrition and Hydrationmelencio olivasNo ratings yet
- 2017 LT4 Wiring DiagramDocument10 pages2017 LT4 Wiring DiagramThomasNo ratings yet
- 感應馬達安裝、保養使用說明書31057H402E (英)Document17 pages感應馬達安裝、保養使用說明書31057H402E (英)Rosyad Broe CaporegimeNo ratings yet
- 2017 THE BLUE WAY Visual PDFDocument54 pages2017 THE BLUE WAY Visual PDFAlex KappelNo ratings yet
- Certification "Products Made of Compostable Materials" Procedure No. 3355757Document3 pagesCertification "Products Made of Compostable Materials" Procedure No. 3355757Rei BymsNo ratings yet
- Capacitor BanksDocument49 pagesCapacitor BanksAmal P RaviNo ratings yet
- C 1 WorkbookDocument101 pagesC 1 WorkbookGeraldineNo ratings yet
- HumareaderDocument37 pagesHumareaderStefan JovanovicNo ratings yet
- RestraintsDocument48 pagesRestraintsLeena Pravil100% (1)
- BS7-Touch Screen PanelDocument96 pagesBS7-Touch Screen PanelEduardo Diaz Pichardo100% (1)
- Analyzing Activity and Injury: Lessons Learned From The Acute:Chronic Workload RatioDocument12 pagesAnalyzing Activity and Injury: Lessons Learned From The Acute:Chronic Workload RatioLukas ArenasNo ratings yet
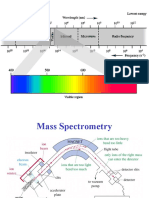
- Mass SpectrometryDocument49 pagesMass SpectrometryUbaid ShabirNo ratings yet
- Complete Renold CatalogueDocument92 pagesComplete Renold CatalogueblpNo ratings yet