Professional Documents
Culture Documents
Helicobacter Pylori
Uploaded by
BnB UsmleCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Helicobacter Pylori
Uploaded by
BnB UsmleCopyright:
Available Formats
Helicobacter Pylori:
- Gram -ve curved rods
- Micro-aerophilic
- Has lophotrichous flagella
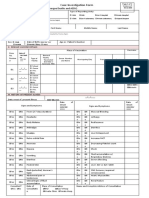
Pathogenesis:
1. Colonization of gastric mucosa
Motility : With help of lophotrichous flagella, it can remain suspended in the viscous mucus
over the mucosa. (if suspended nabhako bhaye Gastric acid le garda degrade huna sakthyo)
Acid resistant: Due to urease enzyme which converts urea into NH3. NH3 buffers the acidic
pH of stomach.
Adhesins: Mostly, H. pylori remains in the mucosa. Some of them express adhesins and gets
attached to the mucous lining. The adhesins are: - Adherence associated lipoprotein, - Blood
group antigen binding protein
2. Pathological changes:
Exotoxins: 1. Vacuolating cytotoxin, 2. Cytotoxin associated gene A (cagA)
The vacuolating cytotoxin forms vacuoles in the cytoplasm of lining epithelial cells. (actual
pathway, Presence of vacuolating cytoplasm expression of anionic channel osmotically
influx of water formation of vacuoles) and they also cause decreased proliferation of T-
cell and inhibits antigen presentation of B-cell. They also inhibit NO release from
macrophages and hence survives
Endotoxin: The LPS of bacteria mimics the antigen expressed on parietal cell of gastric
antrum. (that antigen is H/K ATPase pump)
Factors promoting infection:
- Smoking, eating salty food and canned food. Vitamin C and anti-oxidants have protective effect.
- Inverse relation with : GERD, Barret’s esophagus, adenocarcinoma of esophagus, inflammatory
condition like asthma.
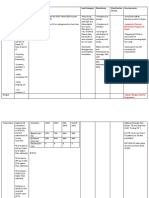
Lab diagnosis:
(A) Invasive test:
Biopsies of gastric mucosa (usually antrum) is collected by endoscopy and subjected to:
- Histopathological staining: by Warthin Starry Silver stain, where bacteria appears black
- Microbiological staining: Gram’s stain: appears pink, rod shaped.
- Culture: Could be done in Campylobacter medium like Skirrow's media or in chocolate medium.
Should be incubated at microaerophilic condition (5-20% CO2). It is highly SPECIFIC but not
sensitive
- Biological test: Catalase, oxidase, urease test +ve
- Biopsy urease test (Rapid urease test): Biopsy is placed in a plate with urea and pH indicator. It is
more SENSITIVE.
(B) Non-invasive test:
Urea breath test: Labeled nonradioactive Urea (with C13) is ingested and if there is bacteria,
urease enzyme cleaves the urea. Labeled CO2 is released in breath. This is highly SENSITIVE
test
Stool examination: Bacterial antigen may be found in stool
Urea breath test and stool examination are done for monitoring treatment
Antibody detection: ELISA could be done to detect IgG in serum.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Injuries Due To Explosive ForcesDocument35 pagesInjuries Due To Explosive ForcesBnB UsmleNo ratings yet
- Injuries StudentsDocument101 pagesInjuries StudentsBnB UsmleNo ratings yet
- FirearmDocument112 pagesFirearmBnB Usmle100% (1)
- Autopsy Report 123nehaDocument29 pagesAutopsy Report 123nehaBnB UsmleNo ratings yet
- Asphyxia KSDocument109 pagesAsphyxia KSBnB Usmle100% (1)
- Death, Time Since Death and Issuanceof DC StudentsDocument101 pagesDeath, Time Since Death and Issuanceof DC StudentsBnB UsmleNo ratings yet
- AUTOPSY ReezuDocument16 pagesAUTOPSY ReezuBnB UsmleNo ratings yet
- Pituitary GlandDocument2 pagesPituitary GlandBnB UsmleNo ratings yet
- DiseaseDocument5 pagesDiseaseBnB UsmleNo ratings yet
- Academic Writing Handbook: Guidance For StudentsDocument34 pagesAcademic Writing Handbook: Guidance For StudentsBnB UsmleNo ratings yet
- Bacterial ConjunctivitisDocument5 pagesBacterial ConjunctivitisBnB UsmleNo ratings yet
- Introduction To History TakingDocument88 pagesIntroduction To History TakingBnB UsmleNo ratings yet
- Base of BrainDocument19 pagesBase of BrainBnB UsmleNo ratings yet
- Introduction To Clinical ExaminationDocument153 pagesIntroduction To Clinical ExaminationBnB UsmleNo ratings yet
- Lymphoid OrganDocument23 pagesLymphoid OrganSwetha RameshNo ratings yet
- EPI Schedule Malawi COM 2017Document2 pagesEPI Schedule Malawi COM 2017INNOCENT KHULIWANo ratings yet
- 2 MM10 CellulitisDocument3 pages2 MM10 CellulitisSelva VelanNo ratings yet
- Hematology Unit: Complete Blood Count (CBC)Document2 pagesHematology Unit: Complete Blood Count (CBC)Rasha ElbannaNo ratings yet
- Vaccination in SwineDocument6 pagesVaccination in SwineAljolynParungaoNo ratings yet
- Take Illness SeriouslyDocument3 pagesTake Illness SeriouslyMD Jakir Hossain RanaNo ratings yet
- Acinetobacter Baumannii Infections UpdateDocument68 pagesAcinetobacter Baumannii Infections Updatetummalapalli venkateswara rao100% (2)
- Vaccination in Calves: Presented By: Divya TrivediDocument12 pagesVaccination in Calves: Presented By: Divya Trivedirajkumar871992No ratings yet
- Drug Study: NCM 106 PharmacologyDocument2 pagesDrug Study: NCM 106 Pharmacologypoleene de leon100% (1)
- Hepatita B ProiectDocument3 pagesHepatita B ProiectaleecssandraaNo ratings yet
- Diagnosis Hfis DPP KlinikDocument8 pagesDiagnosis Hfis DPP KlinikFrans Aditiya TamaNo ratings yet
- Dengue Death Case Investigation Form (CIF)Document3 pagesDengue Death Case Investigation Form (CIF)Chamee Mallillin100% (1)
- White Blood CellsDocument4 pagesWhite Blood Cells9786541238No ratings yet
- Clinical Review October 20 2017 - SHINGRIXDocument158 pagesClinical Review October 20 2017 - SHINGRIXPayneMaxNo ratings yet
- PCP Glossary of Diseases 1Document1 pagePCP Glossary of Diseases 1Aria Jean MostajoNo ratings yet
- Prevalence of Human Immunodeficiency Virus Infection Among Tuberculosis Patients at Infectious Disease Hospital, Kano State, NigeriaDocument8 pagesPrevalence of Human Immunodeficiency Virus Infection Among Tuberculosis Patients at Infectious Disease Hospital, Kano State, NigeriaUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Anaphy Lec Sas-17Document4 pagesAnaphy Lec Sas-17Francis Steve RipdosNo ratings yet
- A02 419Document36 pagesA02 419jaimeNo ratings yet
- TonsilitisDocument9 pagesTonsilitisDeepak patelNo ratings yet
- Basic Facts On Hiv AidsDocument20 pagesBasic Facts On Hiv AidsKenneth Miles100% (2)
- The Statistics of Lyme in The State From Louisiana From The DHHDocument5 pagesThe Statistics of Lyme in The State From Louisiana From The DHHSam WinstromNo ratings yet
- Viral Hepatitis Types Symptoms TreatmentDocument9 pagesViral Hepatitis Types Symptoms TreatmentTAMBI TANYINo ratings yet
- ATLS-9e Tetanus PDFDocument2 pagesATLS-9e Tetanus PDFAroell KriboNo ratings yet
- Heamtopoises ReviewerDocument17 pagesHeamtopoises ReviewerClyde BaltazarNo ratings yet
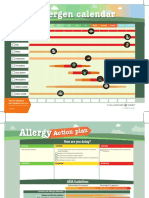
- Allergen Calendar - EnglishDocument2 pagesAllergen Calendar - Englishpkgill15No ratings yet
- Virapid Mono M&G - VR001 - enDocument4 pagesVirapid Mono M&G - VR001 - enCristinaNo ratings yet
- Hospital Infection ControlDocument31 pagesHospital Infection ControlIndian Railways Knowledge PortalNo ratings yet
- PTS - Soal Bahasa Inggris Kelas IXDocument6 pagesPTS - Soal Bahasa Inggris Kelas IXRini YusmayantiNo ratings yet
- Fine-Needle Aspiration Cytology in The Diagnosis of Tuberculous LesionsDocument9 pagesFine-Needle Aspiration Cytology in The Diagnosis of Tuberculous Lesionsmohamaed abbasNo ratings yet
- Nobel Prize Laurates in Immunology Presentation List FINALDocument3 pagesNobel Prize Laurates in Immunology Presentation List FINALzeyneptoros13No ratings yet