Professional Documents
Culture Documents
S S I L I: Eptic Hock After Ntracervical Aminaria Nsertion
S S I L I: Eptic Hock After Ntracervical Aminaria Nsertion
Uploaded by
ari naOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
S S I L I: Eptic Hock After Ntracervical Aminaria Nsertion
S S I L I: Eptic Hock After Ntracervical Aminaria Nsertion
Uploaded by
ari naCopyright:
Available Formats
S.Y.
Lin, et al ■ SHORT COMMUNICATION ■
SEPTIC SHOCK AFTER INTRACERVICAL
LAMINARIA INSERTION
1
Shin-Yu Lin, Wen-Fang Cheng, Yi-Ning Su , Chi-An Chen, Chien-Nan Lee*
Departments of Obstetrics and Gynecology and 1Medical Genetics,
National Taiwan University Hospital, Taipei, Taiwan.
SUMMARY
Objective: Laminaria placement is seldom thought to be associated with postabortal sepsis.
Case Report: A nulliparous woman presented with high fever, low blood pressure, and signs of infection during
artificial legal abortion with laminaria placement for cervical dilatation. Broad-spectrum antibiotics were given.
Cultures of blood, placenta, and arterial line all yielded Enterobacter cloacae. The patient responded to antibiotics
and supportive care.
Conclusion: The use of laminaria still places patients at risk for infection because there is a certain risk of
ascending colonization with potentially pathogenic microorganisms from the vaginal and cervical microflora,
as in our patient. Surgical disinfection, prophylactic antibiotics, and shortened duration of laminaria placement
are helpful to prevent infectious insult. Once signs of infection are noted, physicians should take action as
soon as possible, such as initiating broad-spectrum antibiotics and intensive care. [Taiwanese J Obstet Gynecol
2006;45(1):76–78]
Key Words: laminaria, septic abortion, termination
Introduction the first report of sepsis due to E. cloacae bacteremia
associated with laminaria for elective abortion.
There are many ways to facilitate mid-trimester abor-
tion, including osmotic cervical dilatation with lamina-
ria japonicum tents, prostaglandin E2 vaginal tablets, Case Report
and sulprostone intravenous infusion. Osmotic cervical
dilatation is considered safe and effective. We have A nulliparous 32-year-old woman at 17 weeks’ gesta-
used it uneventfully in more than 800 patients in tion was admitted for elective abortion due to fetal om-
the past 10 years. Despite the inability to sterilize the phalocele. She had four laminaria placed after betadine
laminaria, it is seldom associated with infection [1]. vaginal disinfection. A purulent whitish vaginal dis-
We present the case of a patient who used laminaria for charged was noted. The patient took oral prophylactic
cervical dilatation and suffered sepsis and severe bac- cephalexin one capsule 250 mg every 6 hours. The
teremia. MEDLINE and PUBMED searches using the next morning, sulprostone was given intravenously
words “laminaria”, “sepsis”, and “Enterobacter cloacae” to augment uterine contractions. The laminaria was
from 1966 to December 2004 suggest that this is uneventfully removed 22 hours later. After artificial
rupture of the membranes on the 3rd morning, no
malodor or dirty amniotic fluid was noted. A three-way
*Correspondence to: Dr. Chien-Nan Lee, Department of Obstetrics Foley catheter with 50 mL of distilled water was inserted
and Gynecology, National Taiwan University Hospital, 7 Chung- into the cervix to facilitate cervical dilatation. However,
Shan South Road, Taipei, Taiwan. chills and fever up to 39.9° C developed 2 hours later.
E-mail: leecn@ha.mc.ntu.edu.tw
We stopped sulprostone immediately because it is
Received: October 4, 2005
Revised: October 6, 2005 reported to cause a febrile reaction. We also added
Accepted: October 12, 2005 cefamezine 1.0 g intravenously every 8 hours as
76 Taiwanese J Obstet Gynecol • March 2006 • Vol 45 • No 1
Septic Shock after Laminaria Insertion
prophylaxis. Two sets of blood cultures were performed clinically verified endometritis/salpingitis was registered
immediately. A dead fetus was expulsed 5 hours later. in this study and the authors concluded that presurgi-
Tachycardia (144 bpm) and low blood pressure cal dilatation with laminaria tents involves a negligible
(75/42 mmHg) were noted after abortus delivery. The risk of a pelvic inflammatory disease as long as the
body temperature was up to 38.8° C and oxygen treatment does not exceed 24 hours. In a clinical series
saturation was 96% under room air. The patient’s con- of 1,000 consecutive dilation and evacuation (D&E)
sciousness was clear throughout the whole course. abortions at 17–26 weeks’ gestation using multiple
Leukopenia (from 6,890 to 1,600 × 103/μL) was noted laminaria treatments over 48 hours, Hern reported the
and, under the impression of sepsis, she was transferred following complications possibly attributable in part
to the intensive care unit. Empiric antibiotic treatment to laminaria use: three minor intraoperative cervical
included ampicillin/sulbactam, gentamicin, and met- lacerations and one infection before D&E [4]. Bryman
ronidazole. Ampicillin/sulbactam was replaced with et al compared laminaria tents with Hegar dilators
intravenous ceftazidime to cover pseudomonas and reported a 2% incidence of endometritis in
infection. Thrombocytopenia (from 245 to 91 × 103) the laminaria group versus 13% in the Hegar dilator
and positive disseminated intravascular coagulation group [5]. Similarly, a prospective randomized study
profiles were noted, and packed red blood cells (500 involving 519 women revealed that the rate of post-
mL) and fresh frozen plasma (4 U) were supplied. abortal inflammatory disease was significantly lower
3
Leukocytosis (from 1,600 to 7,220 to 11,680 × 10 /μL) after pretreatment with laminaria tents [6].
and elevating C-reactive protein (from 2.87 to 18.47 Septic abortions are usually polymicrobial, with
mg/dL) developed 1 day later. bacteria derived from the normal flora of the vagina
Two sets of peripheral blood cultures, one set of and endocervix, and the important addition of sexually
arterial line blood cultures, and a placental culture all transmitted pathogens. The Gram-positive aerobic cocci
yielded E. cloacae within 24 hours. From the sensitivity Staphylococcus epidemidis, Streptococcus faecalis, and Strep-
results, we switched ceftazidime to ceftriaxone and tococcus agalactiae as well as Escherichia coli and Klebsiella/
stopped metronidazole. The fever subsided and the Enterobacter are the most frequent microorganisms
patient did well, with blood pressure stabilizing to among aerobic isolates from endocervices and laminaria
90–120/58–70 mmHg. Antibiotics were continued tents [3]. Our patient had bacteremia with E. cloacae
for the full 10-day course at the infection specialist’s following placement of laminaria. E. cloacae is a Gram-
suggestion. The patient was discharged in a stable con- negative bacillus that is more commonly a cause of
dition and no oral antibiotics were prescribed. hospital-acquired infection in immunocompromised
patients and is not susceptible to -lactam antibiotics.
It has been associated with a major epidemic of intraven-
Discussion ous line contamination. However, we followed appro-
priate aseptic technique between patients and there
The hydroscopic property of laminaria enables it to was no horizontal spread in our hospital. Our Infection
expand up to five times in diameter over 12–24 hours, Control Committee failed to find an association between
thereby gradually dilating the cervix. It has been further this patient’s bacteremia and intravenous line contami-
hypothesized that this gradual mechanical stretching nation. It is fortunate that these bacteria responded to
provides a stimulus for the local release of the pro- our empiric ceftazidime and gentamicin. We suggest
staglandin, cytokines, and elastase thought to be im- the use of broad-spectrum antibiotics as soon as possible
portant in cervix ripening [2]. Laminaria tents fell out of in cases of suspected septic abortion.
favor in the early 20th century because of complications Although the infection rate associated with laminaria
due to infection. The potential for these sea plants to has decreased with improving sterilization techniques,
harbor pathogens led some investigators to speculate the use of laminaria still places patients at some risk
that colonization of laminaria tents may lead to post- for infection. There is a certain risk of ascending coloni-
abortive infection. Recently, with modern sterilization zation with potentially pathogenic microorganisms
techniques using ethylene oxide and -irradiation, la- from the vaginal and cervical microflora, as occurred in
minaria tents are re-emerging as an option for cervical our patient. Therefore, presurgical vaginal preparation,
dilatation. The associated infection rates are similar to aseptic techniques, short duration of laminaria place-
those achieved with standard methods. ment, and prophylactic antibiotics play a role. Once
Evaldson et al sent endocervical specimens for cul- patients present with signs of infection, the clinician
ture preoperatively and laminaria postoperatively in 53 should be alert for septic abortion and use broad-
women who requested first-trimester abortion [3]. No spectrum antibiotics empirically.
Taiwanese J Obstet Gynecol • March 2006 • Vol 45 • No 1 77
S.Y. Lin, et al
References microbiological study. Acta Obstet Gynecol Scand 1986;65:
257–61.
4. Hern WM. Serial multiple laminaria and adjunctive urea in
1. Hern WM. Laminaria versus Dilapan osmotic cervical dilat-
late outpatient dilatation and evacuation abortion. Obstet
ors for outpatient dilation and evacuation abortion: ran-
Gynecol 1984;63:543–9.
domized cohort comparison of 1001 patients. Am J Obstet
5. Bryman I, Granberg S, Norstrom A. Reduced incidence of
Gynecol 1994;171:1324–8.
postoperative endometritis by the use of laminaria tents in
2. El Maradny E, Kanayama N, Halim A, Maehara K, Kobayashi connection with first trimester abortion. Acta Obstet Gynecol
T, Terao T. Biochemical changes in the cervical mucus after Scand 1988;67:323–5.
application of laminaria tent. Acta Obstet Gynecol Scand 1996; 6. Jonasson A, Larsson B, Bygdeman S, Forsum U. The influence
75:203–7. of cervical dilatation by laminaria tent and with Hegar dilat-
3. Evaldson GR, Fianu S, Jonasson A, Larsson B, Nord CE, ors on the intrauterine microflora and the rate of postabortal
Olund AR. Does the hygroscopic property of the laminaria pelvic inflammatory disease. Acta Obstet Gynecol Scand 1989;
tent imply a risk for ascending infection in legal abortions? A 68:405–10.
78 Taiwanese J Obstet Gynecol • March 2006 • Vol 45 • No 1
You might also like
- Curriculum 2a Biology Assignment 2 Final PDFDocument17 pagesCurriculum 2a Biology Assignment 2 Final PDFapi-357661397100% (1)
- Classification of DiseasesDocument51 pagesClassification of Diseasesapi-446296420No ratings yet
- Food SpoilageDocument15 pagesFood Spoilagewahehe102113100% (3)
- Clinical Teaching 4PEUPERAL SEPSISDocument5 pagesClinical Teaching 4PEUPERAL SEPSISAjit M Prasad Prasad100% (1)
- Pharma Prelim and Conceptual ExamsDocument20 pagesPharma Prelim and Conceptual Examsquidditch07No ratings yet
- Ob Management Septic AbortionDocument8 pagesOb Management Septic AbortionspringdingNo ratings yet
- Ollege OF Ducation: Don Honorio Ventura State UniversityDocument9 pagesOllege OF Ducation: Don Honorio Ventura State UniversityIrving Kelly B. PinedaNo ratings yet
- Case Study - Septic AbortionDocument4 pagesCase Study - Septic AbortionHoneylyn100% (1)
- Policies and Prosedures On Infection Control 2nd EditionDocument226 pagesPolicies and Prosedures On Infection Control 2nd EditionAbah Harris HafizhNo ratings yet
- Wendy Silvers Master Series Interview - Dr. Judy MikovitsDocument92 pagesWendy Silvers Master Series Interview - Dr. Judy MikovitsDaniela30No ratings yet
- Epidemiology and Control of Malaria (With A Focus On Sub-Saharan Africa)Document30 pagesEpidemiology and Control of Malaria (With A Focus On Sub-Saharan Africa)Suchie ILyasNo ratings yet
- Government College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-IDocument4 pagesGovernment College of Nursing Jodhpur: Procedure On-Cordocentesis Subject-Obstetrics & Gynecology Specialty-Ipriyanka100% (2)
- Chapter 4 PRINCIPLES OF INFECTION, PREVENTION AND CONTROLDocument11 pagesChapter 4 PRINCIPLES OF INFECTION, PREVENTION AND CONTROLShanin SalapuddinNo ratings yet
- Immunology Core NotesDocument230 pagesImmunology Core NotesSabinaHorvat100% (1)
- Salmonella Tuboovarian AbscessDocument3 pagesSalmonella Tuboovarian AbscessPaul HartingNo ratings yet
- HK MJ 208944Document3 pagesHK MJ 208944Bianca CaterinalisendraNo ratings yet
- Jurnal - Tuba Ovarii Abses - Anisa Ryani MafitriDocument7 pagesJurnal - Tuba Ovarii Abses - Anisa Ryani MafitriBagus Indra KusumaNo ratings yet
- Pi Is 1701216315302577Document4 pagesPi Is 1701216315302577rio rumaropenNo ratings yet
- Conservative Management of Placenta Accreta in A Multiparous WomanDocument10 pagesConservative Management of Placenta Accreta in A Multiparous WomanRobel Mae Lagos MontañoNo ratings yet
- Vaginal Extrusion of A Ventriculoperitoneal Shunt A Case Report and Review ofDocument10 pagesVaginal Extrusion of A Ventriculoperitoneal Shunt A Case Report and Review ofDian AdiNo ratings yet
- Placenta Increta Causing Um in The 26th Week of Pregnancy 2Document3 pagesPlacenta Increta Causing Um in The 26th Week of Pregnancy 2Kester ApostolNo ratings yet
- F (SHU) CE (Ra1) KM PF1 (AJ KM) PN (SL)Document2 pagesF (SHU) CE (Ra1) KM PF1 (AJ KM) PN (SL)Fariza Nur AiniNo ratings yet
- Post Partum HaemorrhageDocument6 pagesPost Partum Haemorrhagenancy jeyakumarNo ratings yet
- Using Recombinant Activated Factor VII BDocument5 pagesUsing Recombinant Activated Factor VII BBagusHibridaNo ratings yet
- 17 The Puerperium Noted PDFDocument39 pages17 The Puerperium Noted PDFmohammed farajiNo ratings yet
- Daptomycin 5Document2 pagesDaptomycin 5SachithNo ratings yet
- 1-3-JMCRCS2024040906 Revised - Galley - Proof - 1715425008Document2 pages1-3-JMCRCS2024040906 Revised - Galley - Proof - 1715425008ILBS M.Sc. NursingNo ratings yet
- Compliationof PuerperimDocument27 pagesCompliationof PuerperimSuman GuptaNo ratings yet
- Journal of Pediatric Surgery CASE REPORTSDocument4 pagesJournal of Pediatric Surgery CASE REPORTSwidyaNo ratings yet
- Infections of The Female Pelvis: Intrapartum, Postpartum, and Postabortal InfectionsDocument9 pagesInfections of The Female Pelvis: Intrapartum, Postpartum, and Postabortal Infectionsalepedro1234No ratings yet
- Tubo-Ovarian Abscess in A Virgin Girl: Case ReportDocument4 pagesTubo-Ovarian Abscess in A Virgin Girl: Case ReportMaria MiripNo ratings yet
- General Gynaecology:, Leo Francis AquilizanDocument15 pagesGeneral Gynaecology:, Leo Francis AquilizanesjayemNo ratings yet
- CORDOCENTESISDocument4 pagesCORDOCENTESISDaily DoseNo ratings yet
- Postpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiDocument4 pagesPostpartum Hemorrhage Post Placenta Previa Centralis-Conservative Management. Astrit M. GashiAstrit GashiNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleHazbullah AisyNo ratings yet
- Tetanus After Induced Abortion A Case ReportDocument4 pagesTetanus After Induced Abortion A Case ReportShrutiNo ratings yet
- Cervical Ectopy 2017Document3 pagesCervical Ectopy 2017Marta GasparNo ratings yet
- Jurnal - Andi Nabila A. Rusli - Infeksi Streptokokus PDFDocument6 pagesJurnal - Andi Nabila A. Rusli - Infeksi Streptokokus PDFoke boskuNo ratings yet
- Abnormal PueperiumDocument24 pagesAbnormal Pueperiumvvmounika reddy907No ratings yet
- Chemical Pleurodesis For Malignant Pleural EffusionDocument6 pagesChemical Pleurodesis For Malignant Pleural EffusiondarmariantoNo ratings yet
- Acute Cholangitis in A Patient With Kluyvera Cryocrescens Bacteremia: A Case Report and Literature ReviewDocument4 pagesAcute Cholangitis in A Patient With Kluyvera Cryocrescens Bacteremia: A Case Report and Literature ReviewDhen Mas PrimanaNo ratings yet
- Sub Diaphragmatic Abscess Leading To Empyema Thoracis in A Case of Perforated Appendix A Rare Case ReportDocument4 pagesSub Diaphragmatic Abscess Leading To Empyema Thoracis in A Case of Perforated Appendix A Rare Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Journal Malaria VivaxDocument3 pagesJournal Malaria VivaxPutri PertiwiNo ratings yet
- 2023.07.13 - Obstetrics S2. 02 - Puerperal InfectionDocument52 pages2023.07.13 - Obstetrics S2. 02 - Puerperal InfectionVignesh ThangavelNo ratings yet
- Uterine Rupture in A Primigravid Patient and Anesthetic Implications: A Case ReportDocument4 pagesUterine Rupture in A Primigravid Patient and Anesthetic Implications: A Case ReportYahia AhmadNo ratings yet
- Toxic Shock Syndrome - PPTX 1-1Document49 pagesToxic Shock Syndrome - PPTX 1-1Mohammed Khedr100% (1)
- Post Partum Infections Obstet MedDocument5 pagesPost Partum Infections Obstet MedMutiaIlyasNo ratings yet
- Empyema Guidelines: DR - Preetham Kumar Reddy Consultant Pediatrician & Intensivist Rainbow Children'S HospitalDocument30 pagesEmpyema Guidelines: DR - Preetham Kumar Reddy Consultant Pediatrician & Intensivist Rainbow Children'S HospitalMahmoud Abdel MoneimNo ratings yet
- Cesarean Hysterectomy With Cystotomy in Parturient Having Placenta Percreta, Gestational Thrombocytopenia, and Portal Hypertension - A Case ReportDocument4 pagesCesarean Hysterectomy With Cystotomy in Parturient Having Placenta Percreta, Gestational Thrombocytopenia, and Portal Hypertension - A Case ReportasclepiuspdfsNo ratings yet
- Stepwise Devascularization Versus B-LyncDocument57 pagesStepwise Devascularization Versus B-LyncBagusHibridaNo ratings yet
- Early-Onset Listeriosis in Prematurity: A Case ReportDocument3 pagesEarly-Onset Listeriosis in Prematurity: A Case ReportAzizan HakimNo ratings yet
- 1 s2.0 S2214751921001584 MainDocument7 pages1 s2.0 S2214751921001584 MainfitriNo ratings yet
- Puerperial PyrexiaDocument4 pagesPuerperial PyrexiaSyaira TanjidNo ratings yet
- TugasDocument3 pagesTugasKirana KlarismaNo ratings yet
- Echinococcosis of The Spleen During Pregnancy: The Israel Medical Association Journal: IMAJ May 2001Document3 pagesEchinococcosis of The Spleen During Pregnancy: The Israel Medical Association Journal: IMAJ May 2001Ibtissam BelehssenNo ratings yet
- Puerpral SepsisDocument5 pagesPuerpral SepsisPriscilla Sarah PayneNo ratings yet
- Pregnancy Complication: Department of Gynaecology and ObstetricsDocument40 pagesPregnancy Complication: Department of Gynaecology and ObstetricssanjivdasNo ratings yet
- Sepsisin ObstetricsDocument9 pagesSepsisin ObstetricsrakulsundaramNo ratings yet
- Day Case Vaginal Pomeroy Tubectomy A Simplified TechniqueDocument11 pagesDay Case Vaginal Pomeroy Tubectomy A Simplified TechniqueedelinNo ratings yet
- Case Report Proteus Species Infection: A Diagnostic DilemmaDocument5 pagesCase Report Proteus Species Infection: A Diagnostic DilemmaTengku AdriansyahNo ratings yet
- A Reading On HEMATOMA: Delivery Room Nursing RotationDocument7 pagesA Reading On HEMATOMA: Delivery Room Nursing RotationJulianeNo ratings yet
- Amnioreduction in Emergency Rescue Cervical Cerclage With Bulging MembranesDocument2 pagesAmnioreduction in Emergency Rescue Cervical Cerclage With Bulging MembranesAmelia FebrinaNo ratings yet
- Ectopic PregnancyDocument7 pagesEctopic PregnancyDeepshikha MahapatraNo ratings yet
- What Is Causing This Girl S Abdominal Pain .10Document2 pagesWhat Is Causing This Girl S Abdominal Pain .10LuisNo ratings yet
- International Journal of Scientific Research: AnesthesiologyDocument2 pagesInternational Journal of Scientific Research: AnesthesiologyALfuNo ratings yet
- BY:-Shalini Joshi M.SC NURSING Ist Year S.C.O.N. DehradunDocument52 pagesBY:-Shalini Joshi M.SC NURSING Ist Year S.C.O.N. DehradunshravaniNo ratings yet
- Elterman 2014Document3 pagesElterman 2014Ana Luisa DantasNo ratings yet
- Abstract. Septic AbortionDocument1 pageAbstract. Septic AbortionIrina LavricNo ratings yet
- Journal of Clinical and Translational Endocrinology: Case ReportsDocument5 pagesJournal of Clinical and Translational Endocrinology: Case ReportsKartikaa YantiiNo ratings yet
- 10 1016@j Ijscr 2020 01 020Document4 pages10 1016@j Ijscr 2020 01 020ari naNo ratings yet
- Primary Umbilical Endometriosis. Case Report and Discussion On Management OptionsDocument7 pagesPrimary Umbilical Endometriosis. Case Report and Discussion On Management Optionsari naNo ratings yet
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument13 pagesBest Practice & Research Clinical Obstetrics and Gynaecologyari naNo ratings yet
- Omphalocele and Gastroschisis: Wendy Nguyen and Kumar BelaniDocument8 pagesOmphalocele and Gastroschisis: Wendy Nguyen and Kumar Belaniari naNo ratings yet
- The Efficacy of Crown Rump Length Measurement by Ultrasound in Estimating The Gestational AgeDocument7 pagesThe Efficacy of Crown Rump Length Measurement by Ultrasound in Estimating The Gestational Ageari naNo ratings yet
- 1 s2.0 S0959804911009336 MainDocument11 pages1 s2.0 S0959804911009336 Mainari naNo ratings yet
- Keterangan Hamil: 0 Post Sc:5 Post Pv:0 Post Vakum ILO:0 Post Manual Plasenta:0 Pasien Ginekologi:0 Post Kuretase: 1Document3 pagesKeterangan Hamil: 0 Post Sc:5 Post Pv:0 Post Vakum ILO:0 Post Manual Plasenta:0 Pasien Ginekologi:0 Post Kuretase: 1ari naNo ratings yet
- MATERNAL DISEASE-PEB-EclampsiaDocument10 pagesMATERNAL DISEASE-PEB-Eclampsiaari naNo ratings yet
- Keterangan Hamil: 0 Post Sc:5 Post Pv:0 Post Vakum ILO:0 Post Manual Plasenta:0 Pasien Ginekologi:0 Post Kuretase: 1Document3 pagesKeterangan Hamil: 0 Post Sc:5 Post Pv:0 Post Vakum ILO:0 Post Manual Plasenta:0 Pasien Ginekologi:0 Post Kuretase: 1ari naNo ratings yet
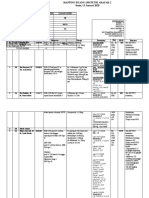
- Mapping Ruang Obstetri Arafah 2 Sabtu, 11 Januari 2020Document5 pagesMapping Ruang Obstetri Arafah 2 Sabtu, 11 Januari 2020ari naNo ratings yet
- Preeklampsia NEJMDocument10 pagesPreeklampsia NEJMari naNo ratings yet
- Slide Obgyn Jurnal ReadingDocument18 pagesSlide Obgyn Jurnal Readingari naNo ratings yet
- Obstetric William Prenatal DiganosisDocument7 pagesObstetric William Prenatal Diganosisari naNo ratings yet
- Options For Questions 1-4Document6 pagesOptions For Questions 1-4ari naNo ratings yet
- Gestational Diabetes: By: Fatima ChoudaryDocument26 pagesGestational Diabetes: By: Fatima Choudaryari naNo ratings yet
- Case Report AIMS IMAMDocument2 pagesCase Report AIMS IMAMari naNo ratings yet
- Agnes Lee Thrombosis PresentationDocument37 pagesAgnes Lee Thrombosis Presentationari naNo ratings yet
- Wound Healing Mila-YesyDocument18 pagesWound Healing Mila-Yesyari naNo ratings yet
- Microbiology Parasitology NotesDocument60 pagesMicrobiology Parasitology Notesaramargareth31No ratings yet
- Blotter Test MethodDocument3 pagesBlotter Test MethodHil MaNo ratings yet
- Salon Safety OERDocument83 pagesSalon Safety OERRosMa WaEi100% (1)
- Helicobacter Pylori, Diagnosis and TreatmentDocument7 pagesHelicobacter Pylori, Diagnosis and TreatmentTrifan_DumitruNo ratings yet
- Please Scroll Down To 3rd PAGEDocument5 pagesPlease Scroll Down To 3rd PAGEnguyennhu1603No ratings yet
- Immunity and Vaccines As Biology Answers AQA OCR EdexcelDocument3 pagesImmunity and Vaccines As Biology Answers AQA OCR EdexcelShela HuangNo ratings yet
- Gender As A Determinant of HealthDocument5 pagesGender As A Determinant of HealthAbdur RahmanNo ratings yet
- Article-2021-COVID-19-Neutralizing Antibodies Predict Disease Severity and SurvivalDocument25 pagesArticle-2021-COVID-19-Neutralizing Antibodies Predict Disease Severity and Survivalcarlos ArozamenaNo ratings yet
- Package Insert - 08052 - H - en - 10100Document7 pagesPackage Insert - 08052 - H - en - 10100Đoàn HạnhNo ratings yet
- Planning and Designing An Isolation Facility in Hospitals Need of The HourDocument9 pagesPlanning and Designing An Isolation Facility in Hospitals Need of The HourdzakyzahidNo ratings yet
- US Army Medical Course MD0722-100 - Microbiology For The Veterinary SpecialistDocument114 pagesUS Army Medical Course MD0722-100 - Microbiology For The Veterinary SpecialistGeorges100% (2)
- Base TestDocument28 pagesBase Testomarelbihi8No ratings yet
- 01.introduction To Microbiology 14Document14 pages01.introduction To Microbiology 14Hosam GomaaNo ratings yet
- Close Reading BittenDocument5 pagesClose Reading Bittenapi-405140390No ratings yet
- Zombie: Survival GuideDocument25 pagesZombie: Survival Guideapi-462582713No ratings yet
- Infection ControlDocument2 pagesInfection Controlapi-500949236No ratings yet
- Marasmus and KwashiorkorDocument11 pagesMarasmus and KwashiorkorSonnia RiveraNo ratings yet
- Abdominal Infections and Puerpural SepsisDocument31 pagesAbdominal Infections and Puerpural SepsisEl Defensor Teas: 100 NaturalNo ratings yet
- PP 1000mcqsDocument65 pagesPP 1000mcqsMUn EEb100% (1)
- Faith Leader Letter To Governor WolfDocument4 pagesFaith Leader Letter To Governor WolfSean DamonNo ratings yet