Professional Documents
Culture Documents
Contribution of Haptic Simulation To Analogic Training Environment in Restorative Dentistry
Uploaded by
pradnja surya paramithaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Contribution of Haptic Simulation To Analogic Training Environment in Restorative Dentistry
Uploaded by
pradnja surya paramithaCopyright:
Available Formats
Use of Technology in Dental Education
Contribution of Haptic Simulation
to Analogic Training Environment in
Restorative Dentistry
Marin Vincent, David Joseph, Christophe Amory, Nathalie Paoli, Pascal Ambrosini,
Éric Mortier, Nguyen Tran
Abstract: The aim of this study was to evaluate the contribution of virtual reality to the conventional analogic training environ-
ment and show the complementarity of conventional techniques and virtual reality in the learning of dental students. All 88 first-
year dental students at a dental school in France in early 2019 were randomly assigned to one of two groups: group 1 (n=45) was
assigned to cavity preparations on a haptic simulator (Virteasy) and group 2 (n=43) was assigned to conventional practical work
on plastic analogue teeth (Kavo). Following three training sessions, the students in group 1 took a final exam on the same plastic
analogue teeth exercise. The results showed improvement in the drilling skill of both groups. The simulator-trained group (group
1) had similar results to the plastic analogue-trained group (group 2) in the final test on a plastic analogue tooth. In this study,
virtual reality allowed an assessment based on objective criteria and reduced the subjectivity of evaluations conducted on plastic
analogue teeth. Considering the saving of supervision and teaching time as well as the material gain offered by virtual reality, the
learning methods of haptic simulators are educational options that should be considered by dental educators.
Marin Vincent, DDS, PhD, is Associate Professor, Department of Restorative Dentistry and Endodontics, Faculty of Odontology
of Nancy, France; David Joseph, DDS, PhD, is Associate Professor, Department of Periodontology, Faculty of Odontology of
Nancy, France; Christophe Amory, DDS, PhD, is Associate Professor, Department of Restorative Dentistry and Endodontics,
Faculty of Odontology of Nancy, France; Nathalie Paoli, DDS, is Assistant Professor, Department of Periodontology, Faculty of
Odontology of Nancy, France; Pascal Ambrosini, DDS, PhD, is Professor, Department of Periodontology, Faculty of Odontology
of Nancy, France; Éric Mortier, DDS, PhD, is Professor, Department of Restorative Dentistry and Endodontics, Faculty of
Odontology of Nancy, France; and Nguyen Tran, PhD, is Associate Professor, Operational Director, School of Surgery of Nancy-
Lorraine, France. Dr. Joseph is co-first author of this article, and Dr. Mortier is co-last author. Direct correspondence to Dr. Marin
Vincent, University of Lorraine, Campus Brabois Santé, Faculté d’Odontologie de Lorraine, 7 avenue de la Forêt de Haye, BP
20199, 54505 Vandœuvre-lès-Nancy, France; 0688605764; marin.vincent@univ-lorraine.fr.
Keywords: dental education, restorative dentistry, preclinical skills, educational technology, simulation, haptics
Submitted for publication 3/1/19; accepted 9/20/19; first published online 12/9/19
doi: 10.21815/JDE.019.187
R
estoring damage to mineralized tooth tissues the literature by Towers et al. in 2019 found that
resulting from caries is a prerequisite stan- numerous questions remain concerning the use of
dard of all dentists. Mastering cavity prepara- haptic simulation in dentistry, particularly to deter-
tion is taught in every dental school, through various mine the roles and place it should be given in dental
training strategies that try to address an appropriate education programs.6 According to Al-Saud et al.,
synergy between the theoretical knowledge necessary virtual reality combined with instructor feedback
for fully understanding clinical procedures and best helps optimize the acquisition and retention of certain
manual practices. However, for many reasons, there basic conservative dentistry skills.7 The use of haptic
are still gaps in the number and the efficacy of re- simulators coupled with virtual reality, for which the
sources, training, and acquisition,1 and there are also realism is constantly improving, enables students to
calls for medico-surgical institutions to go beyond repeat procedures an unlimited number of times. The
the minimum standard and adopt new approaches cost benefits of this absence of repetition limit were
that will meaningfully address modern and objective described by Suebnukarn et al..8 Furthermore, haptic
certification of proficiency.2-5 simulation may represent an ecological advance since
Virtual simulation or computer-assisted virtual it limits the waste produced by the use of plastic
assistance may be an efficient educational pathway teeth in traditional simulation methods. Virtual real-
to achieving a high level of practice. A review of ity could be eventually used to certify the clinical
Published online ahead of print 9 Dec. 2019 ■ Journal of Dental Education e1
skills of practitioners as part of continuing profes-
sional development.9,10 Since its inception, simula- Materials and Methods
tion in dental education has shown better efficacy in
In accordance with the University Hospital of
teaching than traditional techniques through more
Nancy procedures, this research was submitted to the
effective learning and systematic feedback.9 The
Research and Innovation Department and the Ethics
results are particularly encouraging as they concern
Committee of the University Hospital of Nancy. No
fields as varied as implantology,10,11 oral surgery,12
reservations to the publication of this work were is-
prosthetics,13 pediatrics,14 radiology,15 conservation
sued. The study was conducted at the School of Sur-
dentistry,16 and endodontics.8
gery of Nancy-Lorraine (Lorraine University, France)
In restorative dentistry, cavity preparation
and the Faculty of Dentistry of Nancy (University of
concepts have evolved towards a tissue-sparing
Lorraine, France) in early 2019.
approach, requiring a high level of skill and preci-
All first-year dental students (n=88) of the
sion when preparing cavities. As in other dental
Faculty of Dentistry of Nancy were enrolled and
disciplines, restorative dentistry can cause iatrogenic
randomly defined. All the students signed an agree-
damage, such as breaching of the pulp chamber, loss
ment validated by the school board of the University
of substance on the proximal surfaces of adjacent
of Lorraine. Group 1 (n=45) was assigned to cavity
teeth, or excessive deterioration of the dental struc-
preparations on a haptic simulator (Virteasy; HRV
ture, ultimately resulting in mutilation due to a lack
Simulation, Changé, France), and group 2 (n=43)
of control of the surgical procedure. In addition,
was assigned to conventional practical work on
understanding, adhering to, and mastering some
plastic analogue teeth (Kavo; Kavo Dental, Brea,
of the geometric preparation concepts used for the
CA, USA). Following three training sessions, the
preparation of bonded indirect restorations are some
students in group 1 took a final exam on the same
of the psychomotor skills that need to be acquired
plastic analogue teeth exercise. For both groups,
during dental education.17 In 2013, Yamaguchi et al.
the maximum time for each cavity preparation was
reported the utility of haptic simulation for perform-
restricted to ten minutes. There was an interval of
ing cavity preparation on molars in seven students.18
one week between each session.
Wang et al. also found that this type of tool was useful
in restorative dentistry.19 However, they identified
several different research topics to be developed, Simulator and Exercises
including, in particular, increasing the task difficulty. The haptic simulator Virteasy consists of a PC-
In this context, we opted to use the proximal type computer running Windows 7, a touch-screen
cavity in our study (G.V. Black’s Class II cavity), control for interacting with simulator software, a pair
conventionally used to evaluate the skill level of of 3D screen stereoscopic glasses (Estar America
students in cavity preparation due to its relative ESG6100; BienestarAmerica, Hillstar, OR, USA)
complexity in terms of both depth and form. This for viewing the 3D scene, a plastic contra-angled
type of procedure demands an understanding of the handpiece connected to force feedback arm device
task to be performed, mastery of the tool via good (Geomagic Touch X Haptic Device, Geomagic Inc.,
hand-eye coordination in order not to damage ad- Morrisville, NC, USA) to transcribe the tactile sen-
jacent teeth, and the need to comply with different sations of drill in the bone, and a foot pedal to start
preparation heights. Preparation of a Class II cavity the virtual handpiece in the simulator. No student
is a more complete and more complex exercise than had experienced virtual simulators before this study.
conventional Class I cavity preparation. However, Before the exercise, each student in both groups
two studies found that students had low proficiency experienced a short demonstration on how to use the
on these preparations.15,20 simulator, including use of the virtual handpiece,
The aim of our study was to evaluate the contri- ergonomic positions, and feedback force provided by
bution of virtual reality to the conventional analogic the machine. The exercise on the haptic simulator was
training environment and show the complementarity a Black’s Class II cavity on a first right mandibular
of conventional techniques and virtual reality in the molar (#46) consisting of a principal cavity with a
learning of dental students. Analysis was performed mesial opening and a depth of 4 mm and in a second-
from comparative data extracted from simulators and ary cavity (prophylactic extension) with a depth of 2
from the traditional method via cavity preparation on mm. The second right mandibular premolar was left
plastic analogue teeth. in place throughout the cavity preparation.
e2 Journal of Dental Education ■ Published online ahead of print 9 Dec. 2019
Before the first simulator exercise, all students software; percentage of tissue removed outside the
in group 1 received a briefing with a PowerPoint requested target, noted “outside” in the Virteasy
presentation concerning the shape imperatives for software; formula calculated as “100 – (inside +
a perfect cavity. The three first sessions (G1 E1, G1 outside)”; and drilling time (time in seconds during
E2, and G1 E3) were performed without assistance which the drill bit is rotated during the exercise).
provided by the simulators (but with photographs of Subjective parameters recorded from both
the ideal cavity as a model). All cavity preparation groups. For each test and in both groups, different
was achieved by means of an identical dental drill subjective parameters were evaluated in a double-
(Ref 830009, diameter: 0.9 mm). After each exercise blind manner by odontology teachers. The evalua-
on the haptic simulator, each student underwent a tors were the two supervisors who established the
ten-minute debriefing period with the same teacher, evaluation grid and followed all the students during
and areas of improvement were clearly explained the sessions. Then, all the data were recorded in an
before new sessions. The students had to judge for Excel spreadsheet: a) outline shape of the cavity:
themselves the quality of their preparations. Then, -2=very bad (no outline shape), -1=bad (outline
the teacher explained how to improve the prepara- shape slightly pronounced), 0=passable (visible
tion scores. but irregular outline shape), 1=good (outline shape
globally respected), and 2=very good (outline shape
Plastic Analogue Teeth and perfectly respected); b) respect of depth (2 mm)
within the principal and secondary cavities: -1=no
Exercises difference (depth=0), 0=depth partially respected
The students knew the instrumentation (contra- (depth <2 mm), and 1=perfect depth difference
angle and burrs as well as the material used for the (depth=2 mm); c) regularity of the cavity floor:
teeth). However, the exercise (Black’s Class II cavity) -2=over 3 irregularities or presence of a perforation,
was not known, and the students did not know the -1=3 irregularities <1 mm or presence of 1 irregular-
rules of preparation before this date. They did not ity >1 mm, 0=2 irregularities, 1=1 irregularity, and
acquire the skills before carrying out the training. 2=0 irregularity; d) iatrogenic milling on the molar
The exercise on plastic analogue teeth was the same (#46): -1=iatrogenic milling on 46, and 1=no iatro-
as that on the haptic simulator. All students benefitted genic milling on 46; and 3) distal iatrogenic milling
from the same briefing procedure with a PowerPoint on the premolar (#45): -1=iatrogenic cavity on 45,
presentation displaying required operations and 0=iatrogenic damage on 45 without cavity, and 1=no
expected results. iatrogenic damage on 45.
The three sessions (G2 E1, G2 E2, and G2
E3) were performed on plastic analogue teeth. Dur- Statistical Analysis
ing these sessions, students had a photograph of
the master preparation as a model. The dental drills The results were expressed as mean±standard
were references 830008 and 830010 (diameter 0.8 deviation. Data were analyzed using non-parametric
and 1 mm). After each exercise, each student had an Friedman statistical tests with Dunn’s correction at
individual ten-minute debriefing session, and areas α=0.05 for multiple paired comparison and non-
of improvement were clearly explained before new parametric Kruskal-Wallis statistical tests with
sessions. In the last (fourth) session, for the final Dunn’s correction at α=0.05 for multiple unpaired
exam of group 1 on a plastic analogue tooth, a cavity comparison. A probability p<0.05 was considered
preparation following the same described protocol significant. Analyses were made possible through
was performed (noted G1 analogue). the GraphPad Prism software (GraphPad Software,
San Diego, CA, USA).
Parameters Studied
Objective parameters recorded from the Results
simulator. For each test, different objective param-
eters provided by the simulator were recorded and The objective outcomes of group 1 are shown in
displayed in an Excel spreadsheet: percentage of Figure 1. The analysis of the objective data collected
tissue removed corresponding to the required target revealed progressive improvement in students’ drill-
(between 0 and 100%), noted “inside” in the Virteasy ing skill, especially concerning the crucial formula
Published online ahead of print 9 Dec. 2019 ■ Journal of Dental Education e3
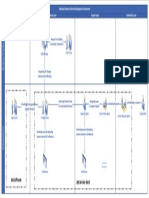
Figure 1. Evolution of objective parameters: % inside of group 1 on haptic simulation (panel a); % outside of group 1
on haptic simulation (panel b); formula (100 – inside + outside) of group 1 on haptic simulation (panel c); drilling time
of group 1 on haptic simulation (panel d); total time of group 1 on haptic simulation (panel e); total time of group 2 on
plastic analogue tooth (panel f)
*Significant at p<0.05; **p<0.01; ***p<0.0001
e4 Journal of Dental Education ■ Published online ahead of print 9 Dec. 2019
of “inside/outside” parameters (p<0.01) (panel c).
The time spent by group 1 to perform virtual drill- Discussion
ing was 216±107 seconds during the first exercise
The current paradigm of surgical training in
decreasing significantly to 150±60 seconds (p<0.01)
general and particularly in dentistry continues to
during phase 3 of training. In parallel, we noted an
raise concerns about the appropriate evaluation of
improvement in the total exercise time (527±102 to
a student’s proficiency since subjective criteria still
425±112; p<0.0001). When considering the novices
play a fundamental role in judgment. Virtual reality in
using the plastic analogue tooth (group 2), we also
the field of medico-surgical training has been shown
observed an improvement in the sole objective pa-
to be an efficient pedagogical adjunct to better shape
rameter available: the total exercise time (543±73 to
the learning process and learning outcomes: simula-
424±105; p<0.0001). Their learning curve is shown
tors with haptic arms have been successfully tested
in panel f.
in many dental and medical fields.21-29 In comparing
Figure 2 shows the gain in experience stem-
this innovative learning method of cavity preparation
ming from subjective outcomes of novices working
with the traditional technique on plastic analogue
with the virtual and analogic cavity models. For the
teeth, several key messages might be extracted
“outline shape of the cavity” and “respect of the
from our study. First, the haptic simulator allowed
depths” parameters, a clear progressive improvement
us, according to available objective parameters, to
over time was observed (p<0.01 for both groups be-
monitor the progression of novices concerning cav-
tween E1 and E3) on virtual training period (group
ity preparation on a Black’s Class II cavity. Second,
1). We also noted a non-significant improvement of
there was no significant difference between the two
the “iatrogenic milling on 46,” “iatrogenic milling on
methods of learning according to the subjective and
45,” and “regularity of the cavity floor” parameters
objective indicators used.
highlighted by a decrease in median and/or SD.
We conducted this study with first-year dental
In comparison, students in group 2, who
students in order to limit potential bias related to
worked with the plastic analogue preparation in the
previous experience. According to Wang et al., it
three training sessions, also had gains in all skills.
would be necessary to increase the difficulty of the
The results were mostly higher with better median
task presented during the research carried out on
and/or SD but non-significant (Figure 3). After the
these simulators.19 For this reason, we used a Black’s
three sessions of both groups, group 1 conducted
Class II cavity to test the progression in dexterity of
the same plastic analogue tooth exercise. When we
first-year students in cavity preparation. This model
tried to compare the two groups on plastic analogue
provides a good base for the development of fine
preparations, the outcomes of all subjective param-
motor skills such as the respect of shape and depth
eters were reported, and no significant difference was
of the cavity, the regularity of the cavity floor, and
found between the two groups. However, only based
the absence of iatrogenic milling. Likewise, without
on median and/or SD, we can note that the results of
well-integrated psychomotor skills such as timing,
group 1 were equivalent to or better than the second
sequencing, speed and precision of hand-eye coordi-
exercise of group 2. However, the analysis of the
nation, and mechanical ability, proficiency in cavity
“iatrogenic milling on 45” parameter on the plastic
preparation becomes quite challenging, and some
analogue tooth showed lower results for group 1 than
authors have called for a better certification of this
for the three exercises of group 2.
procedure.7,30
Regarding the sole comparable objective
A major factor driving an efficient learning
parameter—the total exercise time—we found a
curve is likely to be the reliance on correlation in du-
significant difference between the plastic analogue
ration of procedure and in performance of dexterity,
exercise of group 1 and the second and third exercises
which is a fundamental component of efficiency.10,31-36
of group 2 (p<0.01 and p<0.001, respectively). Even
Our findings clearly showed that the two methods
if the exercise was the same on the plastic analogue
of cavity preparation (virtual or physical) led to
tooth and virtual reality, the transition from a virtual
improvement in dexterity with similar beneficial
to an analog environment for the students of group
impact on the learning curves. Indeed, the time spent
1 would explain this no significant difference in
performing the exercises diminished significantly
total time between the two first analogue exercises
with training in both groups. Regarding group 1,
of both groups.
the time for exercise completion was significantly
Published online ahead of print 9 Dec. 2019 ■ Journal of Dental Education e5
Figure 2. Evolution of subjective parameters and total exercise time with group 1 on haptic simulator (left) and group 2
on plastic analogue tooth (right): outline shape of the cavity (panel a); respect of the depths (panel b); regulatory of the
cavity floor (panel c); iatrogenic milling on 45 (panel d); iatrogenic milling on 46 (panel e); total time (panel f)
*Significant at p<0.05; **p<0.01; ***p<0.0001
e6 Journal of Dental Education ■ Published online ahead of print 9 Dec. 2019
Figure 3. Comparison between groups 1 and 2 on plastic analogue tooth: outline shape of the cavity (panel a); respect
of the depths (panel b); regularity of the cavity floor (panel c); iatrogenic milling on 45 (panel d); iatrogenic milling on
46, no SD for G1 analogue, all students had the note 1 (panel e); and total time (panel f)
*Significant at p<0.01; **p<0.001
Published online ahead of print 9 Dec. 2019 ■ Journal of Dental Education e7
reduced, going from an average of 216 seconds in supervision time, the material gains, and the repeat-
the first exercise to 150 seconds in the third one—an ability of the acts, virtual reality could be a real asset
improvement of about 30%. To further evaluate their for the education of dental students.
precision in achieving a virtual cavity, we used the Interestingly, new findings emerged when stu-
additional parameter “formula 100 – (% inside + % dents in group 1 performed their first plastic analogue
outside)” to better define the student’s improvement tooth exercise after their virtual training period on
than the “% inside” and “% outside” criteria alone. haptic simulators. When we compared their final ana-
Indeed, a student with a “% inside” of 95% could be logue cavity preparation with the three exercises of
considered as good while outcome of “% outside” group 2, there was no significant difference, suggest-
was over 10%. This formula allowed us to eliminate ing that earlier training on a virtual cavity was effec-
this statistical bias by considering the complete per- tive at improving their dexterity when experiencing
formance of each student. Taken together, we found a physical model for the first time. Our data from the
a concomitant improvement in ability as witnessed final plastic analogue test pointed to the usefulness
by the result obtained from the ratio between the of the simulator in the acquisition of surgical skills.
percentages of “inside” and “outside” of students Piromchai et al. found that virtual reality-based train-
in this group displaying a significant learning curve ing significantly improved the surgical ability and psy-
during the training phase. chometric skills of learners.41 Simulators with haptic
As with group 1, reduction in timing was also arms have been successfully tested in many dental and
seen in the group of students undergoing learning on medical fields.21-28 Our results were in agreement with
the plastic analogue materials (group 2)—improve- these studies and showed that these new virtual real-
ment being 22% after three sessions going from ity training technologies could be used in preclinical
543±73 to 424±105 seconds. This improvement training for dental students, allowing them to enhance
was also associated with a significant improvement their learning curve, as found by Buchanan.42
in “outline shape of the cavity” and “respect of the Similar to Fanning and Gaba,43 we outlined the
principal and secondary cavity depths.” Thus, it could importance of mentoring through correct briefing/
be argued that the combination of repetition and de- debriefing procedure. In the contemporary context
briefings during the phase of acquisition was crucial where our educational mission may be hampered by
to reach the expected pedagogical endpoint. It should low teacher-student ratios, it becomes more and more
be noted that the timing to prepare a virtual cavity difficult to maintain an appropriate level of interac-
was very similar to the time spent for plastic analogue tion between learners and tutors. The objective of
achievement (Figure 2). However, the simulator-based the implementation of this new technology would be
students performed cavity preparation with less iatro- therefore to complete the training of dental preclinical
genic damage. We theorize that this outcome might be students.1 Prior studies have found a real benefit in
attributable to the enhanced computerized visual sys- terms of time, individualized training, and material
tem favoring the hand-eye coordination of the novice. and human resources.44-46 In these ways, students can
We and others have previously examined the feasibil- be trained more quickly with systematic feedback,
ity and benefits of 3D simulators on task-oriented and their progress curves are accelerated. In addition,
approaches in new surgical techniques such as robotic self-service concepts could allow students to be able
surgery37,38 and implantology.10,11 Magnification of to train outside of their preclinical hours, without the
details helps strengthen the cognitive acquisition of mandatory presence of teachers. In this framework,
the task and improves the confidence of the novice. and for all the reasons outlined in this study, we agree
Prior studies found that young residents with former with McGaghie et al. that the learning methods of
experience in microsurgery (3D visualization and haptic simulators are educational options that should
coordination) significantly improved their abilities be fully considered.47
and their performance in robotic training.39,40 We This study had several limitations. Since it
suggest the use of a dedicated microscope in cavity took place in only one academic dental institution,
preparation training might be an effective tool to its results may not be generalizable to students in
contribute to enhancing the outcome. other programs. Also, the study may have had human
In our study, the virtual reality and conventional factor bias, and it used only one type of simulator
learning curves were extremely similar. However, and took place in only one area of dentistry. Future
the results obtained on simulators were slightly studies should repeat the research with other groups
better. Associated with the saving of teaching and of students in order to check its reproducibility, to
e8 Journal of Dental Education ■ Published online ahead of print 9 Dec. 2019
increase sampling to reduce human factor bias, to 9. Perry S, Bridges SM, Burrow MF. A review of the
validate our results with other types of simulators, use of simulation in dental education. Simul Healthc
2015;10(1):31-7.
and to expand this educational method to other areas
10. Joseph D, Jehl JP, Maureira P, et al. Relative contribu-
of dentistry (implantology, prosthodontics, etc.). tion of haptic technology to assessment and training in
These studies are already under way. implantology. BioMed Res Int 2014;14:e413951.
11. Kinoshita H, Nagahata M, Takano N, et al. Development
of a drilling simulator for dental implant surgery. J Dent
Conclusion Educ 2016;80(1):83-90.
12. Pohlenz P, Gröbe A, Petersik A, et al. Virtual dental
Our study highlighted the complementarity of surgery as a new educational tool in dental school. J
Craniomaxillofac Surg 2010;38(8):560-4.
the traditional and virtual method in the training of 13. Kikuchi H, Ikeda M, Araki K. Evaluation of a virtual real-
dental students and showed that virtual reality pre- ity simulation system for porcelain fused to metal crown
pared students for the analog environment. In learn- preparation at Tokyo Medical and Dental University. J
ing phasing, haptic simulation can serve to improve Dent Educ 2013;77(6):782-92.
these aspects of this particular preparation prior to 14. Papadopoulos L, Pentzou AE, Louloudiadis K, Tsiatsos
TK. Design and evaluation of a simulation for pedi-
transitioning to the analog training. Objective certi- atric dentistry in virtual worlds. J Med Internet Res
fication of basic dexterity in odontology thanks to 2013;15(10).
these new devices should gradually become essential 15. Nilsson TA, Hedman LR, Ahlqvist JB. A randomized
in initial training and continuing education. In order trial of simulation-based versus conventional training of
to be fully usable, the development and implementa- dental student skill at interpreting spatial information in
radiographs. Simul Healthc 2007;2(3):164-9.
tion of new objective evaluation criteria could be a
16. Eve EJ, Koo S, Alshihri AA, et al. Performance of dental
solution to improve student self-assessment. students versus prosthodontics residents on a 3D immer-
sive haptic simulator. J Dent Educ 2014;78(4):630-7.
Acknowledgments 17. Roy E, Bakr MM, George R. The need for virtual reality
simulators in dental education: a review. Saudi Dent J
This work was carried out thanks to the support 2017;29(2):41-7.
of the European Fund for Regional Development 18. Yamaguchi S, Yoshida Y, Noborio H, et al. The usefulness
(Fonds Européens de Développement Régional, of a haptic virtual reality simulator with repetitive training
FEDER) within the framework of the project Virtual to teach caries removal and periodontal pocket probing
Hospital of Lorraine. skills. Dent Mater J 2013;32(5):847-52.
19. Wang D, Zhao S, Li T, et al. Preliminary evaluation of a
virtual reality dental simulation system on drilling opera-
REFERENCES tion. Biomed Mater Eng 2015;26(Suppl 1):S747-56.
1. LeBlanc VR, Urbankova A, Hadavi F, Lichtenthal RM. 20. Zou H, Jin S, Sun J, Dai Y. Cavity preparation skill evalu-
A preliminary study in using virtual reality to train dental ation system for assessing junior dental students. Med
students. J Dent Educ 2004;68(3):378-83. Educ 2016;50(5):586-7.
2. Kaufmann CR. Computers in surgical education and the 21. Gallagher AG, Lederman AB, McGlade K, et al. Discrimi-
operating room. Ann Chir Gynaecol 2001;90(2):141-6. native validity of the minimally invasive surgical trainer
3. Wanzel KR, Ward M, Reznick RK. Teaching the surgi- in virtual reality (MIST-VR) using criteria levels based
cal craft: from selection to certification. Curr Probl Surg on expert performance. Surg Endosc 2004;18(4):660-5.
2002;39(6):573-659. 22. Gallagher AG, Richie K, McClure N, McGuigan J. Objec-
4. Okuda Y, Bryson EO, DeMaria S Jr, et al. The utility of tive psychomotor skills assessment of experienced, junior,
simulation in medical education: what is the evidence? and novice laparoscopists with virtual reality. World J Surg
Mt Sinai J Med 2009;76(4):330-43. 2001;25(11):1478-83.
5. Bilotta FF, Werner SM, Bergese SD, Rosa G. Impact and 23. Gallagher K, Stephenson J, Brown R, et al. Exploiting 3D
implementation of simulation-based training for safety. spatial sampling in inverse modeling of thermochronologi-
Sci World J 2013;13:652956. cal data. Rev Mineral Geochem 2005;58(1):375-87.
6. Towers A, Field J, Stokes C, et al. A scoping review of the 24. Wierinck ER, Puttemans V, Swinnen SP, van Steenberghe
use and application of virtual reality in preclinical dental D. Expert performance on a virtual reality simulation
education. Br Dent J 2019;226(5):358. system. J Dent Educ 2007;71(6):759-66.
7. Al-Saud LM, Mushtaq F, Allsop MJ, et al. Feedback and 25. Wierinck E, Puttemans V, Swinnen S, van Steenberghe
motor skill acquisition using a haptic dental simulator. D. Effect of augmented visual feedback from a virtual
Eur J Dent Educ, June 1, 2016. reality simulation system on manual dexterity training.
8. Suebnukarn S, Hataidechadusadee R, Suwannasri N, et Eur J Dent Educ 2005;9(1):10-6.
al. Access cavity preparation training using haptic virtual 26. van der Meijden OAJ, Schijven MP. The value of haptic
reality and microcomputed tomography tooth models. Int feedback in conventional and robot-assisted minimal
Endod J 2011;44(11):983-9. invasive surgery and virtual reality training: a current
review. Surg Endosc 2009;23(6):1180-90.
Published online ahead of print 9 Dec. 2019 ■ Journal of Dental Education e9
27. Quinn F, Keogh P, McDonald A, Hussey D. A study 37. Perez M, Perrenot C, Tran N, et al. Prior experience in
comparing the effectiveness of conventional training and micro-surgery may improve the surgeon’s performance in
virtual reality simulation in the skills acquisition of junior robotic surgical training. Int J Med Robot 2013;9(3):351-8.
dental students. Eur J Dent Educ 2003;7(4):164-9. 38. Perrenot C, Perez M, Tran N, et al. The virtual reality
28. Moorthy K, Munz Y, Sarker SK, Darzi A. Objec- simulator dV-Trainer is a valid assessment tool for robotic
tive assessment of technical skills in surgery. BMJ surgical skills. Surg Endosc 2012;26(9):2587-93.
2003;327(7422):1032-7. 39. Bhayani SB, Andriole GL. Three-dimensional (3D) vi-
29. de Boer IR, Lagerweij MD, de Vries MW, et al. The effect sion: does it improve laparoscopic skills? An assessment
of force feedback in a virtual learning environment on the of a 3D head-mounted visualization system. Rev Urol
performance and satisfaction of dental students. Simul 2005;7(4):211-4.
Healthc 2017;12(2):83-90. 40. Tanagho YS, Andriole GL, Paradis AG, et al. 2D versus
30. Mirghani I, Mushtaq F, Allsop MJ, et al. Capturing differ- 3D visualization: impact on laparoscopic proficiency us-
ences in dental training using a virtual reality simulator. ing the fundamentals of laparoscopic surgery skill set. J
Eur J Dent Educ, Nov. 1, 2016. Laparoendosc Adv Surg Tech A 2012;22(9):865-70.
31. Ioannou I, Kazmierczak E, Stern L, et al. Towards defining 41. Piromchai P, Avery A, Laopaiboon M, et al. Virtual reality
dental drilling competence, part 1: a study of bone drilling training for improving the skills needed for performing
technique. J Dent Educ 2010;74(9):931-40. surgery of the ear, nose, or throat. Cochrane Database Syst
32. Mohtashami F, von Dadelszen P, Allaire C. A surgical Rev 2015;9:CD010198.
virtual reality simulator distinguishes between expert 42. Buchanan JA. Use of simulation technology in dental
gynecologic laparoscopic surgeons and perinatologists. education. J Dent Educ 2001;65(11):1225-31.
JSLS 2011;15(3):365-72. 43. Fanning RM, Gaba DM. The role of debriefing in simu-
33. Mandava SH, Liu J, Maddox MM, et al. Stratification of lation-based learning. Simul Healthc 2007;2(2):115-25.
expert vs. novice laparoscopists using the basic laparo- 44. Miller MD. Office procedures: education, train-
scopic urologic surgery (BLUS) curriculum at a single ing, and proficiency of procedural skills. Prim Care
institution. J Surg Educ 2015;72(5):964-8. 1997;24(2):231-40.
34. Kenney PA, Wszolek MF, Gould JJ, et al. Face, content, 45. Derossis AM, Fried GM, Abrahamowicz M, et al. De-
and construct validity of dV-Trainer, a novel virtual reality velopment of a model for training and evaluation of
simulator for robotic surgery. Urology 2009;73(6):1288-92. laparoscopic skills. Am J Surg 1998;175(6):482-7.
35. Ioannou I, Stern L, Kazmierczak E, et al. Towards defin- 46. Kalsi AS, Higham H, McKnight M, Dhariwal DK. Simula-
ing dental drilling competence, part 2: a study of cues and tion training for dental foundation in oral and maxillofacial
factors in bone drilling. J Dent Educ 2010;74(9):941-50. surgery: a new benchmark. Br Dent J 2013;215(11):571-6.
36. Morton J, Cumming A, Cameron H. Performance-based 47. McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ.
assessment in undergraduate medical education. Clin A critical review of simulation-based medical education
Teacher 2007;4(1):36-41. research: 2003-09. Med Educ 2010;44(1):50-63.
e10 Journal of Dental Education ■ Published online ahead of print 9 Dec. 2019
You might also like
- Contemporary Undergraduate Implant Dentistry Education A Systematic ReviewDocument13 pagesContemporary Undergraduate Implant Dentistry Education A Systematic ReviewfloraNo ratings yet
- Sarkis-Onofre2015 (Poste Fibra)Document6 pagesSarkis-Onofre2015 (Poste Fibra)Carmen AdamesNo ratings yet
- Indirect Pulp Capping Versus Pulpotomy For Treating Deep Carious Lesions Approaching The Pulp in Primary Teeth: A Systematic ReviewDocument6 pagesIndirect Pulp Capping Versus Pulpotomy For Treating Deep Carious Lesions Approaching The Pulp in Primary Teeth: A Systematic ReviewKingkan HongyonNo ratings yet
- Jurnal Internasional 1Document8 pagesJurnal Internasional 1Shafira SaragihNo ratings yet
- Using Simulation To Learn Surgical Skills in Oral Surgery: What Do Students Think?Document7 pagesUsing Simulation To Learn Surgical Skills in Oral Surgery: What Do Students Think?Brent FabialaNo ratings yet
- Effectiveness of Blended Teaching Method in Tooth Carving Applied in Preclinical Course of Dental Education During The Covid-19 PandemicDocument9 pagesEffectiveness of Blended Teaching Method in Tooth Carving Applied in Preclinical Course of Dental Education During The Covid-19 PandemicIJAR JOURNALNo ratings yet
- Eficacia Del Paso A Paso en TalladoDocument5 pagesEficacia Del Paso A Paso en TalladoHugo MoralesNo ratings yet
- 10 1111@ger 12411Document9 pages10 1111@ger 12411AlexandraNo ratings yet
- Analysis of The Need For, and Scope of Training In, Maxillo-Facial Prosthodontics in The South African Dental Technology ProgrammeDocument6 pagesAnalysis of The Need For, and Scope of Training In, Maxillo-Facial Prosthodontics in The South African Dental Technology ProgrammemohammadNo ratings yet
- Evaluation of New Injection and Cavity Preparation Model in Local Anesthesia TeachingDocument8 pagesEvaluation of New Injection and Cavity Preparation Model in Local Anesthesia TeachingBagis Emre GulNo ratings yet
- Ergonomics in Dentistry: Experiences of The Practice by Dental StudentsDocument5 pagesErgonomics in Dentistry: Experiences of The Practice by Dental Studentsbr grNo ratings yet
- Dentistry Journal: Flipping The Dental Anatomy ClassroomDocument7 pagesDentistry Journal: Flipping The Dental Anatomy Classroomdea lifhaNo ratings yet
- Knowledge, Awareness and Practice On Application of Presurgical Nasoalveolar Moulding For Cleft Lip and Palate PatientsDocument8 pagesKnowledge, Awareness and Practice On Application of Presurgical Nasoalveolar Moulding For Cleft Lip and Palate PatientsArshid KhandayNo ratings yet
- Contemporary Management of Deep Caries in Primary Teeth: A Systematic Review and Meta AnalysisDocument31 pagesContemporary Management of Deep Caries in Primary Teeth: A Systematic Review and Meta AnalysisPatrícia BittencourtNo ratings yet
- Knowledge of Yemeni Dental Practitioners Towards Resin Bonded ProsthesisDocument7 pagesKnowledge of Yemeni Dental Practitioners Towards Resin Bonded ProsthesisAhmed MadfaNo ratings yet
- Al Musawi Et Al 2017 Dental TraumatologyDocument6 pagesAl Musawi Et Al 2017 Dental TraumatologySebastián CárdenasNo ratings yet
- Implant Positioning Errors in Freehand and Computeraided Placement Methods A Singleblind Clinical Comparative StudyDocument15 pagesImplant Positioning Errors in Freehand and Computeraided Placement Methods A Singleblind Clinical Comparative StudyDenisa CorneaNo ratings yet
- Sry Devi 2016 JURNAL READING 3 (PROSTO) PDFDocument5 pagesSry Devi 2016 JURNAL READING 3 (PROSTO) PDFBersama BisaNo ratings yet
- Students Perception and Satisfactory Level in Preclinical Fixed Prosthodontic Teaching: Post and CoreDocument8 pagesStudents Perception and Satisfactory Level in Preclinical Fixed Prosthodontic Teaching: Post and CoreVICTOR FERNANDO LAMAS LARANo ratings yet
- Students' Perceptions of Pre-Clinical Endodontic Training With Artificial Teeth Compared To Extracted Human Teeth PDFDocument4 pagesStudents' Perceptions of Pre-Clinical Endodontic Training With Artificial Teeth Compared To Extracted Human Teeth PDFKemal Selman AltunNo ratings yet
- Critical Analysis of Artificial Teeth For Endodontic Teaching PDFDocument7 pagesCritical Analysis of Artificial Teeth For Endodontic Teaching PDFKemal Selman AltunNo ratings yet
- Bone Augmentation of The Edentulous Maxilla For Implant Placement: A Systematic ReviewDocument12 pagesBone Augmentation of The Edentulous Maxilla For Implant Placement: A Systematic ReviewJarvin Miguel Buitrago GalindezNo ratings yet
- Muneeb ArticleDocument7 pagesMuneeb ArticleFaisal Ali BalochNo ratings yet
- Nano 1Document8 pagesNano 1jennifertaniaNo ratings yet
- Ipic 2018Document4 pagesIpic 2018Afwin ZamronyNo ratings yet
- IJCPD-transpapillary InjectionDocument4 pagesIJCPD-transpapillary InjectionShameena KnNo ratings yet
- When To Intervene in The Caries Process? An Expert Delphi Consensus StatementDocument13 pagesWhen To Intervene in The Caries Process? An Expert Delphi Consensus StatementPablo BenitezNo ratings yet
- Children 09 01176 v2Document19 pagesChildren 09 01176 v2aritradentorthohaldarNo ratings yet
- Full-Mouth Rehabilitation of A Severe Tooth Wear Case: A Digital, Esthetic and Functional ApproachDocument22 pagesFull-Mouth Rehabilitation of A Severe Tooth Wear Case: A Digital, Esthetic and Functional Approachjose figueroaNo ratings yet
- Bmjopen 2016 015542Document6 pagesBmjopen 2016 015542Angie Natalia Arias AponteNo ratings yet
- A 48-Month Clinical Evaluation of Fissure Sealants Placed With Different Adhesive SystemsDocument7 pagesA 48-Month Clinical Evaluation of Fissure Sealants Placed With Different Adhesive SystemsMaria Ximena Torres PovedaNo ratings yet
- Prosthodontic Treatment Planning Current Practice Principles and TechniquesDocument4 pagesProsthodontic Treatment Planning Current Practice Principles and TechniquesZiad RabieNo ratings yet
- The Efficacy of Dental Sealant Used With Bonding Agent On Occlusal CariesDocument14 pagesThe Efficacy of Dental Sealant Used With Bonding Agent On Occlusal CariesJeanpareNo ratings yet
- 1 s2.0 S1991790222000307 MainDocument2 pages1 s2.0 S1991790222000307 Maingfdsa jklNo ratings yet
- Copia de Haptics - The Science of Touch in Periodontics 2Document5 pagesCopia de Haptics - The Science of Touch in Periodontics 2Cristian PeñaNo ratings yet
- Resin Cad CamDocument16 pagesResin Cad CamLeidyNo ratings yet
- Knowledge and Awareness Among Dental Students About Choice of Complete Denture Occlusion in Edentulous PatientDocument7 pagesKnowledge and Awareness Among Dental Students About Choice of Complete Denture Occlusion in Edentulous PatientInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Removable Prosthodontics: Denture AdhesivesDocument2 pagesRemovable Prosthodontics: Denture AdhesivespaulinaNo ratings yet
- Indicações Radiograficas OdontopedDocument34 pagesIndicações Radiograficas OdontopedRobertaSoaresNo ratings yet
- Efficacy Brushing - Power Toohbrush.2017Document10 pagesEfficacy Brushing - Power Toohbrush.2017Carlos GalvezNo ratings yet
- Knowledge and Attitudes of Dental Interns in Karnataka State, India, Regarding ImplantsDocument6 pagesKnowledge and Attitudes of Dental Interns in Karnataka State, India, Regarding ImplantsTarek RabiNo ratings yet
- Use of Dental Radiography Among Lithuanian General Dentists: Scientific ArticlesDocument6 pagesUse of Dental Radiography Among Lithuanian General Dentists: Scientific ArticlesfghdhmdkhNo ratings yet
- Muller Bolla2020Document9 pagesMuller Bolla2020Tiara HapkaNo ratings yet
- Clinical Evaluation and Comparison of Quality of Obturation and Instrumentation Time For Pulpectomy in Primary Molars With or Without A Magnifying Loupe An Invivo StudyDocument9 pagesClinical Evaluation and Comparison of Quality of Obturation and Instrumentation Time For Pulpectomy in Primary Molars With or Without A Magnifying Loupe An Invivo StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 10 1111@eje 12221Document8 pages10 1111@eje 12221Bernard HerreraNo ratings yet
- Dinh 2021Document6 pagesDinh 2021Mai ThúyNo ratings yet
- Direct Pulp Capping in Priamry Teeth A Systematic ReviewDocument11 pagesDirect Pulp Capping in Priamry Teeth A Systematic ReviewDaniel Pierre DyotteNo ratings yet
- Mechanical Plaque Removal of Periodontal Maintenance 2020 RezDocument18 pagesMechanical Plaque Removal of Periodontal Maintenance 2020 RezRazvan SalageanNo ratings yet
- Impression MaterialsDocument19 pagesImpression MaterialsLilly PaulNo ratings yet
- A Retrospective Study On The Long Term Outcomes of Pulpe - 2022 - Journal of DenDocument9 pagesA Retrospective Study On The Long Term Outcomes of Pulpe - 2022 - Journal of DenDavid ABCNo ratings yet
- Burbridge2007 NoDocument6 pagesBurbridge2007 NoKatherine VilchezNo ratings yet
- Falah 2016 Graftless Sinus AugmentationDocument7 pagesFalah 2016 Graftless Sinus AugmentationLamis MagdyNo ratings yet
- Esthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsFrom EverandEsthetic Oral Rehabilitation with Veneers: A Guide to Treatment Preparation and Clinical ConceptsRichard D. TrushkowskyNo ratings yet
- Article7 13 4 PDFDocument6 pagesArticle7 13 4 PDFbadar_aqNo ratings yet
- Cementation in Dental Implantology: An Evidence-Based GuideFrom EverandCementation in Dental Implantology: An Evidence-Based GuideChandur P.K. WadhwaniNo ratings yet
- Comparison Between Flipped Classroom and Lecture-Based Classroom in Ophthalmology ClerkshipDocument9 pagesComparison Between Flipped Classroom and Lecture-Based Classroom in Ophthalmology ClerkshipSunajNo ratings yet
- Qoa05016 342 348Document7 pagesQoa05016 342 348Humberto CanoNo ratings yet
- Evaluation of Gingival Fiber Retention Technique oDocument7 pagesEvaluation of Gingival Fiber Retention Technique oAbdur RehmanNo ratings yet
- University of Medical Sciences & Technology, Faculty of Dentistry, Department of Fixed ProsthodonticsDocument2 pagesUniversity of Medical Sciences & Technology, Faculty of Dentistry, Department of Fixed ProsthodonticsSida HussainNo ratings yet
- Eastman Kodak Case StudyDocument6 pagesEastman Kodak Case StudyPetter Smith67% (6)
- Database System Concepts and Architecture: Slide 2-1Document52 pagesDatabase System Concepts and Architecture: Slide 2-1problem solverNo ratings yet
- Bank Loan Case StudyDocument7 pagesBank Loan Case StudyRahul ShirudeNo ratings yet
- Lecture 02 - Foundation Problem Building A NetworkDocument165 pagesLecture 02 - Foundation Problem Building A NetworkTanveer Ahmed HakroNo ratings yet
- Poly-Fine II Series Filter Cartridges: Prefilter For Final Membrane ApplicationsDocument3 pagesPoly-Fine II Series Filter Cartridges: Prefilter For Final Membrane ApplicationsMarcelo García FacalNo ratings yet
- Meucci ReDefining and Managing Diversification PDFDocument44 pagesMeucci ReDefining and Managing Diversification PDFcastjamNo ratings yet
- Network and Telecom Engineer Stage Pré-EmbaucheDocument2 pagesNetwork and Telecom Engineer Stage Pré-EmbaucheElmoctar yarguettNo ratings yet
- Web1201 Lab2 CssDocument36 pagesWeb1201 Lab2 Css阿符的故事No ratings yet
- 22 AutoflightDocument2 pages22 AutoflightMONEY ENDLESSLYNo ratings yet
- Strand Century Lighting Saf-T-Patch Patch Panel Free-Standing Desk Spec Sheet 6-77Document2 pagesStrand Century Lighting Saf-T-Patch Patch Panel Free-Standing Desk Spec Sheet 6-77Alan MastersNo ratings yet
- Unveiling - Namecheap Web Hosting and Greengeeks Web HostingDocument3 pagesUnveiling - Namecheap Web Hosting and Greengeeks Web HostingWebsite Hosting DealsNo ratings yet
- Atlassian Software & Service ManagementDocument1 pageAtlassian Software & Service ManagementEnterprise Agile CoachingNo ratings yet
- It-Bpm Engagements: Fundamentals of Business Process Outsourcing 101Document43 pagesIt-Bpm Engagements: Fundamentals of Business Process Outsourcing 101John Dave GentuyaNo ratings yet
- Chap 3 Hash FunctionsDocument26 pagesChap 3 Hash FunctionsRukhsana KousarNo ratings yet
- Md. Iftekharul Islam Sakib: Lecturer Cse, BuetDocument38 pagesMd. Iftekharul Islam Sakib: Lecturer Cse, BuetMd. MoniruzzamanNo ratings yet
- DC DC Converter For PV Application - VethushanDocument8 pagesDC DC Converter For PV Application - Vethushan2k18-EE-243 Vethushan VinnayagamoorththiNo ratings yet
- School Memo FGD On Preparation of LCOPDocument8 pagesSchool Memo FGD On Preparation of LCOPShara Jane Sayco SamonteNo ratings yet
- DV TOOL HalliburtonDocument15 pagesDV TOOL HalliburtonLarryLevine100% (4)
- Pull Out Testing Methodology Ultimate Load Tests For Rebar DowelsDocument3 pagesPull Out Testing Methodology Ultimate Load Tests For Rebar DowelsHenry FlorendoNo ratings yet
- PASPORT A Secure and Private Location Proof Generation and Verification FrameworkDocument7 pagesPASPORT A Secure and Private Location Proof Generation and Verification FrameworkIJRASETPublicationsNo ratings yet
- Price List: Small Pump Business Industry SectorDocument23 pagesPrice List: Small Pump Business Industry Sectorasdjhfkadhf100% (1)
- BSBSTR801 Student Assessment TasksDocument16 pagesBSBSTR801 Student Assessment Tasksravi100% (1)
- MATH 1342 Elementary Statistics Prerequisite ReviewDocument8 pagesMATH 1342 Elementary Statistics Prerequisite ReviewAnaNo ratings yet
- Multiarea OspfDocument13 pagesMultiarea OspfNavneetNo ratings yet
- SLR4 (AS & A) - Operating Systems - Systems SoftwareDocument2 pagesSLR4 (AS & A) - Operating Systems - Systems SoftwareZakNo ratings yet
- Sony XAV-63 - ManualDocument64 pagesSony XAV-63 - ManualVinay Patel100% (1)
- Scientific Method PPTDocument35 pagesScientific Method PPTGaukhar IlashevaNo ratings yet
- Parts Catalog: 2008/7 (Jul.) PublishedDocument36 pagesParts Catalog: 2008/7 (Jul.) PublishedCelebes Diesel100% (1)
- What Is Blockchain Technology The Ultimate Guide Binance AcademyDocument1 pageWhat Is Blockchain Technology The Ultimate Guide Binance AcademyIbinabo JoyNo ratings yet
- Deffect List Rawat Inap Lantai 4 (5lift)Document2 pagesDeffect List Rawat Inap Lantai 4 (5lift)it oetomohospitalNo ratings yet