Professional Documents
Culture Documents
Root Fracture 2
Root Fracture 2
Uploaded by
henariaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Root Fracture 2
Root Fracture 2
Uploaded by
henariaCopyright:
Available Formats
Int J Burn Trauma 2021;11(3):226-233
www.IJBT.org /ISSN:2160-2026/IJBT0115924
Case Report
Minimally invasive approach supported by the use of
mouthguard in the treatment of sport-related
root fracture: a case report
Vania Gomes Moraes1, Ludmila Silva Guimaraes2, Erlange Andrade Borges Silva2, Livia Azeredo Alves
Antunes1,2,3, Romulo Franchini4, Leonardo Santos Antunes1,2,3
1
Postgraduate Program, School of Dentistry, Fluminense Federal University, Nova Friburgo, RJ, Brazil;
2
Postgraduate Program, School of Dentistry, Fluminense Federal University, Niterói, RJ, Brazil; 3Department of
Specific Formation, School of Dentistry, Fluminense Federal University, Nova Friburgo, RJ, Brazil; 4Department of
Basic Science, Fluminense Federal University, Nova Friburgo, RJ, Brazil
Received June 9, 2020; Accepted August 9, 2020; Epub June 15, 2021; Published June 30, 2021
Abstract: All sporting activities have an associated risk of orofacial injuries that can affect the oral health-related
quality of life (OHRQoL). A custom-made mouthguard can be used as an adjuvant treatment for faster recovery
of an athlete to resume sporting activities. This case report described a minimally invasive approach by use of
mouthguard for treating sport-related root fracture and its impact on OHRQoL. In a dental trauma care program, the
patient was treated by repositioning the coronary portion and the confection of a splint. It was opted to not realize
the endodontic treatment and the patient was inserted in a rigorous clinical and radiographic follow-up. A custom-
made mouthguard was made, which allowed for the immediate return of athletes to practicing sports. The athlete’s
OHRQoL was negatively impacted by dental trauma, but the treatment proposed was associated with the use of
custom-made mouthguards. After 2 years, the absence of radiographical lesions and a positive response to sensibil-
ity tests were observed. The success of the minimally invasive approach was attributed to immediate conduct fol-
lowing dental trauma, the implementation of follow-up, and associated with the use of custom-made mouthguard.
Keywords: Dental trauma, contact sports, mouthguard, quality of life
Introduction at the same time. This fracture is uncommon,
with an incidence of 7% of all traumatic dental
Orofacial injuries represent a major public lesions [7]. It is diagnosed mainly by radio-
health problem worldwide [1] due to their high graphic examination, requiring several conven-
prevalence, prolonged management, financial tional two-dimensional imaging projections and
burden associated with these injuries [2], and angulations [8, 9]. This fracture can appear in
psychological impact [3]. With the ever-increas- the cervical, middle, or apical third, although in
ing competitiveness in sports and a more dif- most cases, the middle third is the most affect-
fuse practice in the general population, there is ed region [10].
a natural trend to see an increase in sports
lesions. Studies conducted in different coun- Dental trauma has consequences not only for
tries have reported that sports activities in- the traumatized individual but also for family
crease the risk of these injuries in athletes [4, members and society. Orofacial lesions can be
5]. Most injuries affect the upper jaw, with the agonizing events causing not only physical but
maxillary anterior teeth being the most prone also psychological trauma to the victim [11].
to injury [6]. Therefore, evaluating the oral health-related
quality of life (OHRQoL) is important for assess-
Horizontal radicular fracture, that generally ing an individual’s perception of life, with regard
results from horizontal impact, is a lesion that to culture and the values by which he lives and
affects pulp, ligament, dentin, and cementum his or her life goals, expectations, patterns, and
Sport-related root fracture
Case report/clinical techniques
A 36-year old male athlete was referred to the
Dental Trauma Care Program (DTCP) in a
Brazilian public university due to dental trau-
ma that occurred during a soccer match. The
immediate treatment was performed in a pri-
vate clinic two hours after dental trauma. The
patient presented at the university clinic app-
roximately three days after the dental trauma
(Figures 3 and 4). Ethics approval was obtain-
ed from the local Research Ethics Committee
(No. 1.233.367). A patient informed consent
form was obtained. During anamnesis, the ath-
lete reported that the maxillary left central inci-
sor presented mobility toward the palatal re-
gion (vertical mobility). In the previous appoint-
ment in a particular clinic, the tooth was manu-
ally repositioned, and splinting with light-curing
resin was performed. The patient reported that
the dentist had planned to extract the tooth fol-
lowed by implant placement. The initial radio-
Figure 1. Initial periapical radiograph, showing hori- graph showed an oblique horizontal radicular
zontal radicular fracture in the cervical third. fracture in the cervical third (Figure 1). Pulp
sensibility tests to hot and cold were per-
formed, and it was positive. Based on this posi-
concerns [11]. This is a subjective concept that tive diagnosis, treatment plan was splint main-
complements clinical health and encompasses tenance for three months associated with cus-
a well-rounded physical well-being, including tom-made mouthguards to guarantee the ath-
mental and social health, and not only the lete’s safe return to sports practice.
absence of disease [11].
Custom-made mouthguards were fabricated by
The mouthguard is a protective appliance that the authors. Impressions were made by stan-
effectively reduces the frequency and severity dard trays using alginate impression material
of oral facial injuries in sports activities [12]. and were poured with dental stone to obtain
Mouthguards can also help prevent other working models. Before the models were con-
prejudicial consequences of impact, such as fected, the impressions were disinfected using
brain lesions, concussions, bone fractures, 1% sodium hypochlorite. Mouthguard consist-
and lesions in the temporomandibular articula- ed of a double 3-mm and 1-mm lamination of
tion [13, 14]. Even so, many athletes and their ethyl vinyl acetate (EVA) sheet (Ultradent, Salt
trainers do not understand the importance of Lake City, UT, USA). Sheets were placed in a
wearing mouthguards during sports [15, 16]. thermal forming machine (BioSTAR; Scheu-
Dental, Iserlohn, Germany). A pressure-molding
Therefore, this case report described a mini- machine was used for 70 s at 220°C under 5.5
mally invasive approach supported by the use bar pressure of. The cooling phase lasted for
of mouthguard for treating sport-related root 179 sec. The design of the mouthguards fol-
fracture of element 21. A custom-made mouth- lowed the criteria: (i) labially 2 mm short of the
guard was used to recover the athlete earlier to vestibular reflection with rounded borders at
sporting activities and as a preventive measure the buccal peripheries, (ii) approximately 4 mm
for other injuries. Furthermore, the impact of from the cervical margin in the palatal limit,
the proposed treatment was assessed on the tapered at the edges, and (iii) enclosing the
patient’s oral health-related quality of life maxillary teeth to the distal surface of the first
(OHRQoL). molars. Finally, the mouthguard was polished
227 Int J Burn Trauma 2021;11(3):226-233
Sport-related root fracture
Figure 4. Initial athlete occlusion.
Figure 2. One-month follow-up radiograph.
Figure 5. Finalized type IV custom-made mouth-
guard.
post-op complication such as ankylosis or coro-
nary discoloration was observed.
The athlete’s OHRQoL was assessed upon
arrival in DTCP (T1), immediately after placing
the custom-made mouthguard (T2), three-
month (T3), one-year (T4), and two-year (T5)
follow-up. The OHRQoL index involves socio-
dental factors that complement to the clinical
Figure 3. Initial photograph of the palatal region. indicators of the oral condition, detecting psy-
chosocial aspects along with the disease sta-
tus. This allows a more holistic view of how the
and the margin adaptation, stability, and reten- patient is affected.
tion were checked, while delivering.
For the evaluation of OHRQoL, the Brazilian
Regular follow-up was performed at intervals of version of the Oral Health Impact Profile
one-month (Figure 2), three months (Figure 6), (OHIP), measured by the 14-question instru-
one-year (Figure 7), and two years (Figure 8). ment (OHIP-14), was applied in the form of
Clinically, normal and healthy appearance of interviews. The response categories of OHIP-
the left central incisor was observed. The tooth 14 were based on a 5-point Likert scale (0 =
showed no sensitivity to percussion and no ten- never, 1 = rarely, 2 = sometimes, 3 = often,
derness of the surrounding tissues on palpa- and 4 = always), and the participants can se-
tion. Pulp sensibility was assessed with a cold lect one of the five options [17]. These scores
pulp test, and the tooth had a very slight reac- were calculated by the addition of the athletes’
tion. The radiographic examination revealed a responses. The OHIP-14 value for each of its
radiopaque area in the cervical fractured root, seven domains was also analyzed separately.
suggesting bone neoformation along with the This assessment method ranged from 0 to 56.
results of minimally invasive treatment. No High scores revealed poor OHRQoL.
228 Int J Burn Trauma 2021;11(3):226-233
Sport-related root fracture
Figure 6. Three-month radiographic follow-up show-
ing the beginning of tissue regeneration and newly Figure 8. Two-year radiographic follow-up, where
formed bone. pulp tissue regeneration is observed as well as newly
formed stabilized bone.
guards (Figure 5), OHRQoL was reapplied and
showed a positive influence on the athlete’s
quality of life, as it reduced the psychosocial
impact according to the scores. The differences
observed between pre- and post-treatment
scores confirmed the treatment’s success.
Even though, due to trauma, the athlete dem-
onstrated a negative impact on the emotional
well-being domain, the points were different
post-treatment (T2). Therefore, this case report
highlights that dental trauma can compromise
the athlete’s psychosocial well-being.
Furthermore, the traumatized tooth showed
improvement with minimally invasive treat-
ment. Another success factor in this case was
the implementation of a custom-made mouth-
guard as a co-adjuvant in treatment, guaran-
teeing more safety in sports and reducing
recovery time.
Discussion
Figure 7. One-year radiographic follow-up with bone
and tissue regeneration in progress.
Health is a concept that takes a multidimen-
sional holistic view of an individual. This eva-
Table 1 shows an impact of OHRQoL in athlete. luation is important for athletes. Several case
In T1, the athlete’s quality of life was negatively reports about horizontal root fracture [18-24]
impacted. With the use of custom-made mouth- (Table 2); however, to the best of our knowl-
229 Int J Burn Trauma 2021;11(3):226-233
Sport-related root fracture
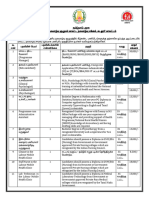
Table 1. Oral health-related quality of life questionnaire-OHIP-14
Post Just after Three-month One-year Two-year
Domain trauma mouthguard follow-up follow-up follow-up
(T1) placement (T2) (T3) (T4) (T5)
1-Did you have trouble saying any words? Oral symptom 0 0 0 0 0
2-Did the taste of your food get worse? Oral symptom 0 0 0 0 0
3-Did you feel mouth or tooth ache? Oral symptom 2 0 0 0 0
4-Did you feel uncomfortable eating any foods? Oral symptom 3 0 0 0 0
5-Were you concerned? Emotional well-being 4 0 0 0 0
6-Were you stressed? Emotional well-being 2 0 0 0 0
7-Was your eating impaired? Functional limitation 0 0 0 0 0
8-Did you have to stop eating your meals? Functional limitation 3 0 0 0 0
9-Did you find it hard to relax? Emotional well-being 0 0 0 0 0
10-Have you ever felt embarrassed? Emotional well-being 0 0 0 0 0
11-Were you irritable towards other people? Emotional well-being 1 0 0 0 0
12-Did you have difficulty performing daily activities? Functional limitation 0 0 0 0 0
13-Did you feel life in general got worse? Emotional well-being 0 0 0 0 0
14-Were you totally unable to perform your daily activities? Functional limitation 0 0 0 0 0
A) Comparing yourself to people your age, how do you see your oral health? Social well-being 1 1 1 0 0
B) Comparing yourself to people your age, how do you see your general health? Social well-being 1 1 1 0 0
C) In the last 3 months, due to problems with your teeth, mouth, bones in your mouth or treatments, how much Social well-being 3 1 1 0 0
was your well-being (life) affected by these events?
Footnote: T1: post trauma; T2: just after mouthguard placement; T3: three-month follow-up; T4: one-year follow-up; T5: two-year follow-up.
Table 2. Characteristics of the clinical cases inserted in the main text
Authors Tooth Fracture location Splint Splint time Type healing Follow up
Poi et al. [18] Upper left-central incisor Between the middle- and apical-third 0.7-mm stainless steel wire and 3 months Fibrous connective tissue 3 years
of a followed-up for over photopolymerized composite
Artvinli and Dural [19] Maxillary right central incisor Coronal third of the root Spontaneously healed - Separated by bone with normal trabecular 6 years
pattern
Cobankara and Ungör [20] Maxillary first premolar Middle-third of the root Spontaneously healed - Fibrous tissue develops between the 14 years
fractured segments
Cantore et al. [21] Upper left-central incisors Middle- and apical-third of the root Orthodontic stainless steel 1 year - Over 4 years
Davis [22] Maxillary right central incisor - Spontaneously healed - Bone repair 8 years
Soares Ditzel et al. [23] Left maxillary lateral incisor Middle third of the root Rigid splint 3 months Mineralized tissue between the fragments 8 years
Tobiska and Krastl [24] Both maxillary central incisors Cervical root Titanium ring split 3 ½ months Interposition of calcified tissue, not ocurr 12 years
230 Int J Burn Trauma 2021;11(3):226-233
Sport-related root fracture
edge, there are no studies reporting a minimal- munication of the fracture line with the oral
ly invasive approach by the use of mouthguard environment. If the fracture line is in communi-
for treating sport-related root fracture and its cation with the oral cavity, immobilization is dif-
influence on OHRQoL. Therefore, this clinical ficult and microbial contamination of the pulp
case report revealed that a custom-made with subsequent pulpal necrosis is inevitable
mouthguard can be used as the treatment for [26]. In this case, the fracture occurred below
sport-related root fracture decreasing the ath- the alveolar crest. Thus, there was no commu-
lete’s recovery time and can be a preventive nication between the sulcular bacteria and the
measure for other injuries. oral environment. In our clinical case, healing
was due to the interposition of hard tissue
The prognosis of root fractures depends on between the fragments (fragments are little
the extent of the fracture line, the pulp tissue separated by the growth of hard tissue).
involvement, occlusion, dislocation of frag-
ments, and the general health of the patient. Long-term follow-up of patients with injuries is
The mobility of the coronary segment can oc- important, as pathological changes can occur
cur to a greater or lesser extent according to several years after injury. A retrospective study
the extent of line of fracture. In this clinical of 400 root-fractured permanent incisors de-
case, there was severe mobility and coronal veloped by Andreasen et al. [25] observed that
segment displacement, due to the severe the follow-up period for healed fractures rang-
impact leading to the cervical third fracture. ed from 1 to 13 years (3.6 years ± 3.0). Long-
The immediate treatment consisted of reposi- term success will be identified by positive
tioning the coronary portion and splinting. In responses to sensitivity tests in cases where
DTCP, the authors chose to maintain this type there is pulp vitality and absence of radio-
of splint for a three-month period, due to the graphic pathological peri-radicular alterations
athlete’s aesthetic needs and the possibility of [18-22]. Once evidence of pulp necrosis is
making a custom-made mouthguard without observed through the fistula, bone resorption
the interference of an apparatus by the vesti- in the fracture line or negative pulp sensibility
bular teeth (orthodontic wire or nylon). Im- test, endodontic treatment must be imple-
mobilization for at least three months is impor- mented.
tant to stabilize the newly formed calcified
material [25]. There is consensus in the literature that the
use of OHRQoL instruments to measure the
Follow-ups are fundamental after traumatic impact of dental trauma is paramount impor-
injuries. Each follow-up should include, eva- tant since these instruments help us evaluate
luation of any signs or symptoms, clinical and prevention and therapeutic options and aim to
radiographic examinations, pulp sensibility improve an individual’s [27] health. This ques-
testing, and photographic documentation [9]. tionnaire was used to complement clinical indi-
Immediately after dental trauma, diagnostic of cators, detailing functional disadvantages and
pulp necrosis (coronal discoloration, loss of psychosocial aspects of these lesions, provid-
pulpal sensibility, and periapical radiolucency) ing a more complete image of the individual’s
could not to discriminate between infected health status [28]. In this case report, all these
pulp and pulp where healing might occur (isch- principles were observed and there was a neg-
emic pulps under revascularization) [8]. A pre- ative impact on the athlete’s concern, which
cipitated untimely endodontic intervention can impacted his psychosocial well-being. Throu-
be one of the factors associated with unsuc- ghout treatment, this was reversed, improving
cessful repair in radicular fractures. In the the OHRQoL of the athlete. The differences in
case of pulp vitality post-lesion, healing pat- scores pre- and post-treatment confirmed
terns can be observed by hard tissue union of treatment success. The immediate association
fragments, connective tissue union of frag- with custom-made mouthguards allowed the
ments, or nonunion due to the interposition of athlete to safely return to sports. Therefore,
granulation tissue between fragments result- indicators of OHRQoL should be implemented
ing from pulp necrosis of the coronal fragment in the dentist’s clinical routine to promote
[8]. A factor that significantly influences the health strategies encompassing psychosocial
healing process in cases of horizontal frac- well-being and not just clinical treatment, with
tures is the presence or absence of a com- a broader holistic view of the patient [27].
231 Int J Burn Trauma 2021;11(3):226-233
Sport-related root fracture
The practice of sports activities soon after oro- Superior, PROEX/UFF - Pro-Reitoria de Exten-
facial injury can represent a risk for the treat- são Universidade Federal Fluminense and
ment proposed and can slow down the player’s CNPQ - Conselho Nacional de Desenvolvimento
performance, causing fear for the athlete and Científico e Tecnológico).
even for his or her opponents [29, 30]. The use
of protective equipment as a coadjuvant treat- Disclosure of conflict of interest
ment provides the athlete with the possibility
None.
of getting back to sports activities faster after
orofacial injuries [31]. In this case report, the Address correspondence to: Dr. Leonardo Santos
use of a custom-made mouthguard allowed Antunes, Department of Specific Formation, School
the athlete to return to sports activities offer- of Dentistry, Fluminense Federal University, Rua
ing more safety against possible new facial Doutor Silvio Henrique Braune, 22 Centro, Nova
injuries and to allow the root fracture to heal Friburgo, RJ 28625-650, Brazil. Fax: +55 22
during sports activities. 25287168; E-mail: leonardoantunes@id.uff.br
Regarding the use of custom-made mouth- References
guards, athletes and their coaches have misin-
formation regarding their relevance in sports [1] Petersen PE. The World Oral Health Report
[17, 18]. Despite its clear role in lesion preven- 2003: continuous improvement of oral health
in the 21st century--the approach of the WHO
tion, many athletes believe that mouthguards
Global Oral Health Programme. Community
are uncomfortable and cause speech and Dent Oral Epidemiol 2003; 31 Suppl 1: 3-23.
breathing problems, which can, in turn, com- [2] Andersson L. Epidemiology of traumatic dental
promise their performance [32-34]. A system- injuries. J Endod 2013; 39: S2-5.
atic review developed by Ferreira et al. [35] [3] Covassin T, Beidler E, Ostrowski J and Wallace
showed that custom-made mouthguards do J. Psychosocial aspects of rehabilitation in
not cause changes in athletes performance in sports. Clin Sports Med 2015; 34: 199-212.
contrast to other kinds of mouthguards. [4] Vidovic D, Bursac D, Skrinjaric T, Glavina D and
Gorseta K. Prevalence and prevention of den-
Therefore, the use of the correct mouthguard
tal injuries in young taekwondo athletes in
should be reinforced, with increased athlete Croatia. Eur J Paediatr Dent 2015; 16: 107-
and sports team awareness [15]. 110.
[5] Bergman L, Milardović Ortolan S, Žarković D,
Conclusions Viskić J, Jokić D and Mehulić K. Prevalence of
dental trauma and use of mouthguards in pro-
Dental trauma negatively affects the psy-
fessional handball players. Dent Traumatol
chosocial aspects of the patient’s OHRQoL. 2017; 33: 199-204.
Conservative treatment of root fracture asso- [6] Bücher K, Neumann C, Hickel R and Kühnisch
ciated with the use of a custom-made mouth- J. Traumatic dental injuries at a German uni-
guard provided a favorable prognosis. The ath- versity clinic 2004-2008. Dent Traumatol
lete could return rapidly to sports and prevent 2013; 29: 127-133.
future trauma, thus increasing OHRQoL. The [7] Andreasen JO. Etiology and pathogenesis of
traumatic dental injuries. A clinical study of
use of a custom-made mouthguard is an effi-
1,298 cases. Scand J Dent Res 1970; 78:
cient co-adjuvant treatment method for ath- 329-342.
letes who suffer root fractures because it [8] Andreasen FM. Pulpal healing after luxation
reduces the period of convalescence, allowing injuries and root fracture in the permanent
the athlete to resume practice after a short dentition. Endod Dent Traumatol 1989; 5:
duration, assuring comfort, safety, and pro- 111-131.
tection. [9] Bourguignon C, Cohenca N, Lauridsen E,
Flores MT, O’Connell AC, Day PF, Tsilingaridis
Acknowledgements G, Abbott PV, Fouad AF, Hicks L, Andreasen JO,
Cehreli ZC, Harlamb S, Kahler B, Oginni A,
The authors would like to thank the participant Semper M and Levin L. International Associa-
of this report. The work was supported by indi- tion of Dental Traumatology guidelines for the
vidual scholarships (FAPERJ - Fundação de Am- management of traumatic dental injuries: 1.
Fractures and luxations. Dent Traumatol 2020;
paro à Pesquisa do Estado do Rio de Janeiro 36: 314-330.
#E-26/010.002195/2019), CAPES - Coordena- [10] Cvek M, Tsilingaridis G and Andreasen JO. Sur-
ção de Aperfeiçoamento de Pessoal de Nível vival of 534 incisors after intra-alveolar root
232 Int J Burn Trauma 2021;11(3):226-233
Sport-related root fracture
fracture in patients aged 7-17 years. Dent [24] Tobiska S and Krastl G. 12 years’ preservation
Traumatol 2008; 24: 379-387. of maxillary permanent incisors with cervical
[11] The World Health Organization Quality of Life root fractures adjacent to aggressive periodon-
assessment (WHOQOL): position paper from titis: report of a case. Quintessence Int 2018;
the World Health Organization. Soc Sci Med 49: 543-548.
1995; 41: 1403-1409. [25] Andreasen JO, Andreasen FM, Mejàre I and
[12] Knapik JJ, Marshall SW, Lee RB, Darakjy SS, Cvek M. Healing of 400 intra-alveolar root frac-
Jones SB, Mitchener TA, delaCruz GG and tures. 2. Effect of treatment factors such as
Jones BH. Mouthguards in sport activities: his- treatment delay, repositioning, splinting type
tory, physical properties and injury prevention and period and antibiotics. Dent Traumatol
effectiveness. Sports Med 2007; 37: 117-144. 2004; 20: 203-211.
[13] Patrick DG, van Noort R and Found MS. Scale [26] Hovland EJ. Horizontal root fractures. Treat-
of protection and the various types of sports ment and repair. Dent Clin North Am 1992; 36:
mouthguard. Br J Sports Med 2005; 39: 278- 509-525.
281. [27] Antunes LA, Leão AT and Maia LC. The impact
[14] Verissimo C, Costa PV, Santos-Filho PC, Tantbi- of dental trauma on quality of life of children
rojn D, Versluis A and Soares CJ. Custom-fitted
and adolescents: a critical review and mea-
EVA mouthguards: what is the ideal thickness?
surement instruments. Cien Saude Colet
A dynamic finite element impact study. Dent
2012; 17: 3417-3424.
Traumatol 2016; 32: 95-102.
[28] Piassi E, Antunes LS and Antunes LA. Orth-
[15] Berg R, Berkey DB, Tang JM, Altman DS and
odontic treatment reduces the impact on chil-
Londeree KA. Knowledge and attitudes of Ari-
zona high-school coaches regarding oral-facial dren and adolescents’ oral health-related
injuries and mouthguard use among athletes. quality of life. Indian J Dent Res 2016; 27: 213-
J Am Dent Assoc 1998; 129: 1425-1432. 219.
[16] Fernandes LM, Neto JCL, Lima TFR, Magno [29] Morita R, Shimada K and Kawakami S. Facial
MB, Santiago BM, Cavalcanti YW and de Al- protection masks after fracture treatment of
meida LFD. The use of mouthguards and prev- the nasal bone to prevent re-injury in contact
alence of dento-alveolar trauma among ath- sports. J Craniofac Surg 2007; 18: 143-145.
letes: a systematic review and meta-analysis. [30] Procacci P, Ferrari F, Bettini G, Bissolotti G,
Dent Traumatol 2019; 35: 54-72. Trevisiol L and Nocini PF. Soccer-related facial
[17] Oliveira BH and Nadanovsky P. Psychometric fractures: postoperative management with fa-
properties of the Brazilian version of the Oral cial protective shields. J Craniofac Surg 2009;
Health Impact Profile-short form. Community 20: 15-20.
Dent Oral Epidemiol 2005; 33: 307-314. [31] Antunes LS, Torres AFC, Ferreira G, Prado R,
[18] Poi WR, Manfrin TM, Holland R and Sonoda Coto NP and Antunes LAA. Custom-made face-
CK. Repair characteristics of horizontal root mask as a coadjuvant in the postoperative
fracture: a case report. Dent Traumatol 2002; treatment of sport-related facial trauma: case
18: 98-102. report. Dent Traumatol 2018; 34: 378-381.
[19] Artvinli LB and Dural S. Spontaneously healed [32] Gardiner DM and Ranalli DN. Attitudinal fac-
root fracture: report of a case. Dent Traumatol tors influencing mouthguard utilization. Dent
2003; 19: 64-66. Clin North Am 2000; 44: 53-65.
[20] Cobankara FK and Ungör M. Spontaneously [33] Collares K, Correa MB, Mohnsam da Silva IC,
healed horizontal root fracture in maxillary first Hallal PC and Demarco FF. Effect of wearing
premolar: report of a case. Dent Traumatol mouthguards on the physical performance of
2007; 23: 120-122. soccer and futsal players: a randomized cross-
[21] Cantore S, Ballini A, Crincoli V and Grassi FR. over study. Dent Traumatol 2014; 30: 55-59.
Treatment of horizontal root fracture: a case [34] Delaney JS and Montgomery DL. Effect of non-
report. Cases J 2009; 2: 8101. custom bimolar mouthguards on peak ventila-
[22] Davis TB. Horizontal root fracture in a maxillary tion in ice hockey players. Clin J Sport Med
central incisor: a case report. Gen Dent 2019; 2005; 15: 154-157.
67: 47-50. [35] Ferreira GB, Guimarães LS, Fernandes CP,
[23] Soares Ditzel A, Tulio Manfron AP, Westphalen
Dias RB, Coto NP, Antunes LAA and Antunes
FH, da Silva Neto UX, Kowalczuck A, Carneiro E
LS. Is there enough evidence that mouth-
and Ditzel Westphalen VP. Management of
guards do not affect athletic performance? A
multiple dental trauma: case report with eight-
systematic literature review. Int Dent J 2019;
year follow-up. Iran Endod J 2018; 13: 410-
69: 25-34.
412.
233 Int J Burn Trauma 2021;11(3):226-233
You might also like
- Concept MapDocument1 pageConcept MapAngela SumiranNo ratings yet
- Clinical Outcomes of Vertical Bone Augmentation To Enable Dental Implant Placement: A Systematic ReviewDocument13 pagesClinical Outcomes of Vertical Bone Augmentation To Enable Dental Implant Placement: A Systematic Reviewvanessa_werbickyNo ratings yet
- Rife FrequenciesDocument12 pagesRife Frequenciesdllabarre100% (1)
- Historical Evolution of NursingDocument33 pagesHistorical Evolution of NursingAnuchithra Radhakrishnan100% (1)
- Nursing in The Prison ServiceDocument148 pagesNursing in The Prison ServiceptsievccdNo ratings yet
- Spots and DentistDocument8 pagesSpots and Dentistlina sonaNo ratings yet
- Jaw Fractures Managing The Whole PatientDocument2 pagesJaw Fractures Managing The Whole PatientElisa BaronNo ratings yet
- 2023 Article 3644Document7 pages2023 Article 3644voni.zlatarNo ratings yet
- Alsaadi2007 Factores SistemicosDocument8 pagesAlsaadi2007 Factores SistemicosTorres MauricioNo ratings yet
- JR Ibm YuanaDocument7 pagesJR Ibm Yuanayuana dnsNo ratings yet
- Post-Extraction Pain in The Adjacent Tooth After Surgical Extraction of The Mandibular Third MolarDocument8 pagesPost-Extraction Pain in The Adjacent Tooth After Surgical Extraction of The Mandibular Third MolarFahmi UtomoNo ratings yet
- Immediate Dentoalveolar RestorationDocument8 pagesImmediate Dentoalveolar RestorationДмитрий ЦененкоNo ratings yet
- Orthodontic Button - National Journal of Orthodontic SocietyDocument5 pagesOrthodontic Button - National Journal of Orthodontic SocietyShruti Maroo - RathiNo ratings yet
- Management of Severe Dento-Alveolar Traumatic Injuries in A 9-YeaDocument7 pagesManagement of Severe Dento-Alveolar Traumatic Injuries in A 9-YeasintaznNo ratings yet
- Witek 2019Document7 pagesWitek 2019Alejandro FereñoNo ratings yet
- 97 105 Badel Jerolimov PanduricDocument9 pages97 105 Badel Jerolimov PanduricMaqbul AlamNo ratings yet
- Badel 2007Document10 pagesBadel 2007MICHAEL ERNESTO QUINCHE RODRIGUEZNo ratings yet
- 2021 Incidence and Pattern of Mandible Fractures An Urban Tertiary Care Centre ExperienceDocument5 pages2021 Incidence and Pattern of Mandible Fractures An Urban Tertiary Care Centre ExperienceSatisha TSNo ratings yet
- Case Report Multidisciplinary Oral Rehabilitation of A Severely Compromised DentitionDocument7 pagesCase Report Multidisciplinary Oral Rehabilitation of A Severely Compromised DentitionAgum Nila Sari IINo ratings yet
- Ankle Arthrodesis For Pilon FractureDocument12 pagesAnkle Arthrodesis For Pilon FracturestudmmaNo ratings yet
- ArtigoDocument5 pagesArtigoCarolina DezanNo ratings yet
- Risk Factors Associated With Early Implant Failure: A 5-Year Retrospective Clinical StudyDocument6 pagesRisk Factors Associated With Early Implant Failure: A 5-Year Retrospective Clinical StudystortoNo ratings yet
- Australian Dental Journal - 2015 - Badenoch Jones - Consent For Third Molar Tooth Extractions in Australia and New ZealandDocument5 pagesAustralian Dental Journal - 2015 - Badenoch Jones - Consent For Third Molar Tooth Extractions in Australia and New ZealandKrishna KadamNo ratings yet
- BLL 2020 05 352Document6 pagesBLL 2020 05 352Benjamin O. ZuñigaNo ratings yet
- Segmental Alveolar Process FractureDocument4 pagesSegmental Alveolar Process FracturegiselaNo ratings yet
- A Clinical Approach To Management of TMJ Disorder With Direct Bonding CompositeDocument5 pagesA Clinical Approach To Management of TMJ Disorder With Direct Bonding Compositewanda oktariaNo ratings yet
- Cosyn Et Al-2011-Journal of Clinical PeriodontologyDocument8 pagesCosyn Et Al-2011-Journal of Clinical PeriodontologyNucleo AlgodonesNo ratings yet
- Clinical Implications of Impingement of The Anterior Femoral Cortex After Cephalomedullary NailingDocument7 pagesClinical Implications of Impingement of The Anterior Femoral Cortex After Cephalomedullary NailingKristianesgaNo ratings yet
- Maturogenesis of A Complicated Crown Fracture: A Case Report With 8 Years Follow-UpDocument4 pagesMaturogenesis of A Complicated Crown Fracture: A Case Report With 8 Years Follow-UpKIH 20162017No ratings yet
- International Journal Of: Dentistry and Oral HealthDocument7 pagesInternational Journal Of: Dentistry and Oral HealthWayan Sutresna YasaNo ratings yet
- Augmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudyDocument7 pagesAugmentation Plating Leaving The Nail in Situ Is An Excellent Option For Treating Femoral Shaft Nonunion After IM Nailing: A Multicentre StudytomimacagnoNo ratings yet
- PRP An Mandibular FractureDocument6 pagesPRP An Mandibular Fracture6hd6mnrzw2No ratings yet
- Etiology, Distribution, Treatment Modalities and Complications of Maxillofacial FracturesDocument9 pagesEtiology, Distribution, Treatment Modalities and Complications of Maxillofacial FracturesPinguin SatuNo ratings yet
- Accuracy and Outcome of Mandibular Fracture Reduction Without and With An Aid of A Repositioning ForcepsDocument8 pagesAccuracy and Outcome of Mandibular Fracture Reduction Without and With An Aid of A Repositioning ForcepsmustafasacarNo ratings yet
- Tecnica de ChampyDocument7 pagesTecnica de Champyboye022694No ratings yet
- Iwanaga 2017Document5 pagesIwanaga 2017zj7n2rhtb4No ratings yet
- Management of Facial Fractures, Its Demography and Clinical OutcomeDocument12 pagesManagement of Facial Fractures, Its Demography and Clinical OutcomeIJAR JOURNALNo ratings yet
- Rehabilitation of Severely Resorbed Edentulous Mandible Using The Modified Visor Osteotomy TechniqueDocument5 pagesRehabilitation of Severely Resorbed Edentulous Mandible Using The Modified Visor Osteotomy TechniqueSaurabh SatheNo ratings yet
- Effect of Occlusal SplintDocument6 pagesEffect of Occlusal SplintDr. Zardasht N. BradostyNo ratings yet
- Implante InmediatoDocument3 pagesImplante InmediatoAlexa LoyaNo ratings yet
- ARTICAL1Document7 pagesARTICAL1Aseel AnesNo ratings yet
- Cureus 0015 00000038746Document10 pagesCureus 0015 00000038746Devid ZilleNo ratings yet
- Miyahira2008 - Miniplates As Skeletal Anchorage For Treating Mandibular Second Molar ImpactionsDocument4 pagesMiyahira2008 - Miniplates As Skeletal Anchorage For Treating Mandibular Second Molar ImpactionsNathália LopesNo ratings yet
- Treatment of Perforating Internal Root Resorption With MTA: A Case ReportDocument5 pagesTreatment of Perforating Internal Root Resorption With MTA: A Case ReportvishalbalpandeNo ratings yet
- Braunstein2020 PDFDocument7 pagesBraunstein2020 PDFZaira ReinaldoNo ratings yet
- Unusual Mandible Fracture Caused by Metallic Spear: Case Report and Literature ReviewDocument8 pagesUnusual Mandible Fracture Caused by Metallic Spear: Case Report and Literature ReviewlindaNo ratings yet
- Bun PIIS174391911400973XDocument5 pagesBun PIIS174391911400973XNorin FornaNo ratings yet
- Deporte e Inflamacio OralDocument11 pagesDeporte e Inflamacio OralJohnny CHNo ratings yet
- Splint Ont MuscleDocument6 pagesSplint Ont MuscleHồ TiênNo ratings yet
- 4 03000605221103974Document13 pages4 03000605221103974Teuku FadhliNo ratings yet
- Long-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior TeethDocument9 pagesLong-Term Stability of Anterior Open-Bite Treatment by Intrusion of Maxillary Posterior TeethNg Chun HownNo ratings yet
- Goyal 2012Document9 pagesGoyal 2012rahulNo ratings yet
- Journal Endang - Ijsr Juli 2020, Fracture MandibleDocument5 pagesJournal Endang - Ijsr Juli 2020, Fracture MandibleEndang Samsudin FKGNo ratings yet
- Is There An Association Between The Use of Antidepressants and Complications Involving Dental Implantes - A Systematic Review and Meta-AnalysisDocument8 pagesIs There An Association Between The Use of Antidepressants and Complications Involving Dental Implantes - A Systematic Review and Meta-AnalysisCaio GonçalvesNo ratings yet
- PEMF - IMF Mand. FractureDocument10 pagesPEMF - IMF Mand. FractureMáté TóthNo ratings yet
- Heel Pain Plantar Fascitis Hard Vs Sorft Orthotics and Heels PadDocument11 pagesHeel Pain Plantar Fascitis Hard Vs Sorft Orthotics and Heels PadDik 40No ratings yet
- Anterior Open Bite Correction Using Bite Block ACase ReportDocument6 pagesAnterior Open Bite Correction Using Bite Block ACase ReportRommy MelgarejoNo ratings yet
- Ortodontia e Lesões Não CariosasDocument7 pagesOrtodontia e Lesões Não CariosasEliane dos santos rodriguesNo ratings yet
- Medicina 59 00355Document12 pagesMedicina 59 00355Anuj BhardwajNo ratings yet
- Root Resorption A 6-Year Follow-Up Case ReportDocument3 pagesRoot Resorption A 6-Year Follow-Up Case Reportpaola lopezNo ratings yet
- Long Term Clinical Result of Implant Induced Injury On The Adjacent ToothDocument9 pagesLong Term Clinical Result of Implant Induced Injury On The Adjacent Toothjdp68svdzwNo ratings yet
- Ams 5 198Document5 pagesAms 5 198dayanaNo ratings yet
- Young KyunDocument6 pagesYoung Kyunodontologia uvNo ratings yet
- Peri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentFrom EverandPeri-Implant Complications: A Clinical Guide to Diagnosis and TreatmentNo ratings yet
- Eczm Policies and Procedures Part 2 - HerpetologyDocument19 pagesEczm Policies and Procedures Part 2 - HerpetologyLauraMercadoIzquierdoNo ratings yet
- Access CavityDocument35 pagesAccess CavitySaca AnastasiaNo ratings yet
- DR Stuart McPherson - Management of Decompensated CirrhosisDocument33 pagesDR Stuart McPherson - Management of Decompensated Cirrhosisana_miulescuNo ratings yet
- CDC Surveilance 2018Document321 pagesCDC Surveilance 2018spiderNo ratings yet
- Gallego, Geraldo, Javellana - Group A3 - BSN 1 Kuan ADocument2 pagesGallego, Geraldo, Javellana - Group A3 - BSN 1 Kuan AChristine Joy JavellanaNo ratings yet
- Brotzman S. - Rehabilitacja Ortopedyczna Tom 1Document199 pagesBrotzman S. - Rehabilitacja Ortopedyczna Tom 1GromisekNo ratings yet
- IPSG May28Document62 pagesIPSG May28S. Pichammal - Quality ManagerNo ratings yet
- Jurnal Kennel CoughDocument12 pagesJurnal Kennel Coughtrisnaput3No ratings yet
- Occupational Therapy's Role in Adult Cognitive DisordersDocument2 pagesOccupational Therapy's Role in Adult Cognitive DisordersThe American Occupational Therapy AssociationNo ratings yet
- TORONTO NOTES 2022 - Cardiologie Et Chirurgie Cardiaque 4Document1 pageTORONTO NOTES 2022 - Cardiologie Et Chirurgie Cardiaque 4mlmbow81No ratings yet
- Njáa Eythœî FGK KHT L Eythœî R F, Flÿ® KHT L : E.F.V©.4609 /M8/2023Document4 pagesNjáa Eythœî FGK KHT L Eythœî R F, Flÿ® KHT L : E.F.V©.4609 /M8/2023SUDHARSAN PERUMALNo ratings yet
- Bonuan Buquig National High SchoolDocument6 pagesBonuan Buquig National High SchoolIra Jane CaballeroNo ratings yet
- Is Davao City, Philippines Ready For E-Health? Dennis John F. Sumaylo UP MindanaoDocument16 pagesIs Davao City, Philippines Ready For E-Health? Dennis John F. Sumaylo UP MindanaoMeredith GreyNo ratings yet
- Newer Classification of Endodontic Fiaps: November 2005Document7 pagesNewer Classification of Endodontic Fiaps: November 2005DrdrNo ratings yet
- English Presentation!Document13 pagesEnglish Presentation!German AcostaNo ratings yet
- Fever in Children With ChemoteraphyDocument23 pagesFever in Children With ChemoteraphyImanuel Far-FarNo ratings yet
- Nutritional AssessmentDocument7 pagesNutritional AssessmentCm MacaliaNo ratings yet
- Med, Supp, Adv Script Live TransferDocument2 pagesMed, Supp, Adv Script Live Transfereraj khan100% (1)
- K Park - Park's Textbook of Preventive and Social Medicine-M - S BANARASIDAS BHANOT Publishers (2019)Document1,008 pagesK Park - Park's Textbook of Preventive and Social Medicine-M - S BANARASIDAS BHANOT Publishers (2019)Labib Orcko100% (2)
- FITT & Training PrinciplesDocument33 pagesFITT & Training Principlescsarimah csarimahNo ratings yet
- GuidelinesDocument26 pagesGuidelinesmsc3nNo ratings yet
- Cancer Lesson Plan - Tutor1Document7 pagesCancer Lesson Plan - Tutor1ta CNo ratings yet
- 1.1, 1.2, 1.3, 1.5 Paediatric Nursing Presentation - 1-1Document54 pages1.1, 1.2, 1.3, 1.5 Paediatric Nursing Presentation - 1-1Christina YounasNo ratings yet
- Explained: What Is 'Eat Right Campus' Tag Given by FSSAI: Updated On Feb 22, 2022, 14:50 ISTDocument3 pagesExplained: What Is 'Eat Right Campus' Tag Given by FSSAI: Updated On Feb 22, 2022, 14:50 ISTVaibhav SatkarNo ratings yet
- Updated Health Assessment Form With Scores 22-1-2023Document9 pagesUpdated Health Assessment Form With Scores 22-1-2023علي الخضيرNo ratings yet
- Laboratory Biosafety Manual-WHODocument109 pagesLaboratory Biosafety Manual-WHORogerio CansiNo ratings yet