Professional Documents
Culture Documents
Letter: When Less Is More: Dexamethasone Dosing For Brain Tumors
Uploaded by
Cheflak KitchenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Letter: When Less Is More: Dexamethasone Dosing For Brain Tumors
Uploaded by
Cheflak KitchenCopyright:
Available Formats
CORRESPONDENCE
Letter: When Less is More: Dexamethasone easier for patients and have not been associated with diminished
Dosing for Brain Tumors efficacy.
Dexamethasone has a biological half-life of 36 to 54 h (despite
To the Editor: a plasma half-life of about 4 hs) and can provide a symptomatic
We are writing to highlight the discrepancy in dosing schedules benefit for a prolonged duration.3 A study published in 1990,
for corticosteroids used to treat peritumoral edema between the which utilized autoradiography to monitor capillary permeability
neurosurgical community and the neuro-oncology community to study peritumoral edema in a C6 rat glioma model, revealed
Downloaded from https://academic.oup.com/neurosurgery/article/85/3/E607/5520500 by guest on 26 November 2021
and suggest that it may be time to re-evaluate the dosing of dexam- that a single dose of dexamethasone maintained a reduction
ethasone for brain tumors. in capillary permeability over a 12-h course.4 Another study
Corticosteroids have been ubiquitously used to treat brain corroborated a substantial reduction in vascular permeability and
tumor patients with cerebral edema since the 1950s. In particular, water content of tumor and peritumoral brain tissue in RG2 rat
dexamethasone, due to its low mineralocorticoid potency and glioma following twice daily dexamethasone dosing.5 Although
high glucocorticoid activity, is arguably the most commonly used rigorous patient studies on twice per day dexamethasone dosing
symptomatic agent out of the limited armamentarium available are lacking, a small pilot study of 14 patients with intracranial
to physicians caring for brain tumor patients. This widespread metastases on a twice daily tapering regimen starting at 8 mg twice
practice traces its origin in part to the landmark paper by Dr a day showed similar rates of clinical response and no neurological
Joseph Galicich and colleagues from the University of Minnesota decline when compared to historical cohorts.6
in 1961.1 In this study, 14 patients with brain tumor-related Administering corticosteroids every 6 h frequently can result
cerebral edema were treated with an initial bolus of 10 to 40 mg in poor sleep due to medication-related effects or medication
of dexamethasone, followed by a regimen of 4 mg intramuscularly administration itself, contributing to increased daytime fatigue.
every 6 h. A total of 13 out of the 14 patients experienced a signif- In a population where preserving the quality of life is paramount,
icant improvement in their neurological symptoms, and dexam- and in the absence of evidence to justify more frequent dosing,
ethasone was hence deemed a “safe and highly effective” agent in we hope the neurosurgical community will join the neuro-
the treatment of tumor-related cerebral edema. Since that time, it oncology community and consider changing its practice to
has been standard practice for dexamethasone to be administered once or twice a day dosing of dexamethasone for brain tumor
to patients every 6 h, including, frequently, in the middle of the patients.
night.
While the benefit of dexamethasone can be dramatic both
clinically and radiographically, particularly in patients with Disclosures
brain metastases and lymphoma, balancing the side effects Dr Colman is on the Advisory Board for and is a consultant for Abbvie,
remains a real challenge, and overuse of dexamethasone is Foundation Medicine, Innocrin, Tactical Therapeutics, Deciphera, Newlink
Genetics, Best Doctors, Merck, and Karyopharm Therapeutics, and receives
common. Steroid-related toxicities present a significant concern
research funding (Site PI/Institutional Contract): Newlink Genetics, Plexxikon,
over time and include iatrogenic Cushing’s syndrome, behav- Kadmon, Orbus, Merck, DNATrix, Abbvie, Beigene, and Forma. Dr Lo is on
ioral issues, myopathy, opportunistic infections, and osteo- the Advisory Board for Gilead Sciences and is a consultant for Viiv Healthcare.
porosis. In addition, early steroid use in primary brain Dr Mellinghoff receives research funding from General Electric, Amgen, and
tumor patients has been associated with increased morbidity Lilly, has advisory roles with Agios, Puma Biotechnology, and Debiopharm
and mortality.2 As newer therapies attempt to augment the Group, and has received honoraria from Roche for a presentation. Dr Mehta is
immune response in the treatment of brain tumors, the use of a consultant for Varian, Abbvie, Celgene, Astra-Zeneca, Tocagen, and Blue Earth
Diagnostics, and is on the Board of Directors for Oncoceutics. Dr Lassman has
steroids for symptomatic relief has become counterproductive
received honoraria/travel/research support (prior 12 mo, all outside the submitted
in many cases. Every attempt should be made to start at the work) from Karyopharm, NW Bio, Agios, AbbVie, Sapience, Oncoceutics,
lowest effective dose and taper as rapidly and as safely as Novocure, Tocagen, Genentech/Roche, Amgen, Millenium, Celldex, Novartis,
possible. Pfizer, Aeterna Zentaris, Pfizer, Kadmon, VBI Vaccines, Beigene, and Bioclinica.
Dosage and tapering of dexamethasone in brain tumor-related Dr Ahluwalia has received grants/research support from Astrazeneca, Abbvie,
cerebral edema are physician, specialty, institution, and patient BMS, Bayer, Incyte, Pharmacyclics, Novocure, and Merck, has received honoraria
dependent. Over time, there has been a growing discrepancy or consultation fees from Elsevier, Wiley, Astrazeneca, Abvvie, VBI Vaccines,
Flatiron, Varian Medical Systems, and Prime Education, and is a stock shareholder
between the dose and schedule of dexamethasone used by the in Doctible and Mimiva.
neurosurgical and the neuro-oncology communities. Most neuro-
surgeons initiate dexamethasone at 4 mg every 6 h, following
Mary Jane Lim-Fat, MD∗
a bolus, and maintain an every 6 h schedule for lower doses.
Wenya Linda Bi, MD, PhD‡
In contrast, most neuro-oncologists administer dexamethasone
Janet Lo, MD§
twice daily or even once daily. These schedules are significantly
NEUROSURGERY VOLUME 85 | NUMBER 3 | SEPTEMBER 2019 | E607
CORRESPONDENCE
Eudocia Quant Lee, MD, MPH∗ ¶ §§
Department of Neurology
Manmeet S. Ahluwalia, MD|| Memorial Sloan Kettering Cancer Center
Tracy T. Batchelor, MD, MPH∗ ¶ New York, New York
Susan M. Chang, MD# ¶¶
Division of Medical Oncology
E. Antonio Chiocca, MD, PhD‡ Mayo Clinic
Ugonma Chukwueke, MD∗ ¶ Rochester, Minnesota
Timothy F. Cloughesy, MD∗∗ ||||
Neuro-Oncology Branch
Howard Colman, MD, PhD‡‡ Center for Cancer Research
Lisa M. Deangelis, MD§§ National Cancer Institute
Evanthia Galanis, MD¶¶ Bethesda, Maryland
Downloaded from https://academic.oup.com/neurosurgery/article/85/3/E607/5520500 by guest on 26 November 2021
Mark R. Gilbert, MD|||| ##
Department of Neuro-Oncology
John F. De Groot, MD## The University of Texas M.D. Anderson Cancer Center
Andrew B. Lassman, MD∗∗∗ Houston, Texas
Linda M. Liau, MD, PhD, MBA‡‡‡ ∗∗∗
Division of Neuro-Oncology
Warren Mason, MD§§§ Department of Neurology, and Herbert Irving Comprehensive
J. Ricardo McFaline-Figueroa, MD, PhD∗ ¶ Cancer Center
Minesh P. Mehta, MD¶¶¶ Columbia University Irving Medical Center
Ingo K. Mellinghoff, MD§§ New York-Presbyterian Hospital
L. Burt Nabors, MD|||||| New York, New York
Lakshmi Nayak, MD∗ ¶ ‡‡‡
Department of Neurosurgery
David A. Reardon, MD∗ ¶ University of California, Los Angeles
Patrick Y. Wen, MD∗ ¶ Los Angeles, California
§§§
∗
Center for Neuro-Oncology Division of Neurology
Dana Farber Cancer Institute Princess Margaret Hospital, Toronto
Boston, Massachusetts Ontario, Canada
¶¶¶
‡
Department of Neurosurgery Department of Radiation Oncology
Brigham and Women’s Hospital Miami Cancer Institute
Boston, Massachusetts Coral Gables, Florida
||||||
§
Neuroendocrine Unit UAB Comprehensive Cancer Center
Massachusetts General Hospital The University of Alabama at Birmingham
Boston, Massachusetts Birmingham, Alabama
¶
Department of Neurology REFERENCES
Brigham and Women’s Hospital
Boston, Massachusetts 1. Galicich JH, French LA, Melby JC. Use of dexamethasone in treatment of cerebral
|| edema associated with brain tumors. J Lancet. 1961;81:46-53.
Burkhardt Brain Tumor and Neuro-Oncology Center 2. Pitter KL, Tamagno I, Alikhanyan K, et al. Corticosteroids compromise survival in
Cleveland Clinic glioblastoma. Brain. 2016;139(5):1458-1471.
Cleveland, Ohio 3. Melby JC. Drug Spotlight Program. Ann Intern Med. 1974;81(4):505.
# 4. Shapiro WR, Hiesiger EM, Cooney GA, Basler GA, Lipschutz LE, Posner JB.
Department of Neurological Surgery Temporal effects of dexamethasone on blood-to-brain and blood-to-tumor transport
University of California, San Francisco of 14C-alpha-aminoisobutyric acid in rat C6 glioma. J Neuro-Oncol. 1990;
San Francisco, California 8(3):197-204.
∗∗ 5. Tjuvajev J, Uehara H, Desai R, et al. Corticotropin-releasing factor decreases
UCLA Neuro-Oncology Program
vasogenic brain edema. Cancer Res. 1996;56(6):1352-1360.
University of California, Los Angeles 6. Weissman DE, Janjan NA, Erickson B, et al. Twice-daily tapering dexamethasone
Los Angeles, California treatment during cranial radiation for newly diagnosed brain metastases. J Neuro-
‡‡
Huntsman Cancer Institute and Department of Neurosurgery Oncol. 1991;11(3):235-239.
University of Utah
Salt Lake City, Utah 10.1093/neuros/nyz186
E608 | VOLUME 85 | NUMBER 3 | SEPTEMBER 2019 www.neurosurgery-online.com
You might also like
- Ischemic Stroke in An Obese Patient Receiving Dabigatran: Elliott Foucar, M.DDocument3 pagesIschemic Stroke in An Obese Patient Receiving Dabigatran: Elliott Foucar, M.DBagus Ngurah MahasenaNo ratings yet
- Brain Metastases: Review ArticleDocument17 pagesBrain Metastases: Review ArticleSebastianNo ratings yet
- Brain Metastasis TreatmentDocument28 pagesBrain Metastasis TreatmentMonica AngNo ratings yet
- 11 PDFDocument9 pages11 PDFirfhanahusaNo ratings yet
- Posology For Regenerative TherapyDocument5 pagesPosology For Regenerative TherapySofia AraujoNo ratings yet
- Jama Andersen 2021 Oi 210108 1632503925.26159Document9 pagesJama Andersen 2021 Oi 210108 1632503925.26159AlizaPinkyNo ratings yet
- Advanced Neuroprotection For Brain Ischemia: An Alternative Approach To Minimize Stroke DamageDocument7 pagesAdvanced Neuroprotection For Brain Ischemia: An Alternative Approach To Minimize Stroke DamageLinda MercadoNo ratings yet
- Ppa 7 027 PDFDocument9 pagesPpa 7 027 PDFbellaNo ratings yet
- Molecular stratification shifts medulloblastoma treatmentDocument7 pagesMolecular stratification shifts medulloblastoma treatmentHeru WahyudiNo ratings yet
- Anticoagulacion Temprana Vs Tardia en ACV Con FADocument11 pagesAnticoagulacion Temprana Vs Tardia en ACV Con FACesar Mauricio Daza CajasNo ratings yet
- Tomography 09 00090Document16 pagesTomography 09 00090PPDS Rehab Medik UnhasNo ratings yet
- Effects of Dexamethasone PDFDocument9 pagesEffects of Dexamethasone PDFAndreea Livia DumitrescuNo ratings yet
- NIH Public Access: Author ManuscriptDocument17 pagesNIH Public Access: Author ManuscriptCheflak KitchenNo ratings yet
- Crameretal 2017 Recoveryrehab IssuesDocument8 pagesCrameretal 2017 Recoveryrehab IssuesNovia RambakNo ratings yet
- Application of Manual Therapy For Dysphagia in Head and Neck Cancer PatientDocument8 pagesApplication of Manual Therapy For Dysphagia in Head and Neck Cancer PatientpoppyNo ratings yet
- 1510493354article pdf1389454199Document6 pages1510493354article pdf1389454199Yolanda FitrianiNo ratings yet
- 2009 Article 57Document12 pages2009 Article 57khalila humairaNo ratings yet
- Cancer Medicine - 2019 - Sankey - Operative and Peri Operative Considerations in The Management of Brain MetastasisDocument23 pagesCancer Medicine - 2019 - Sankey - Operative and Peri Operative Considerations in The Management of Brain Metastasista alNo ratings yet
- Medulloblastoma: Nathan E. Millard, MD and Kevin C. de Braganca, MDDocument13 pagesMedulloblastoma: Nathan E. Millard, MD and Kevin C. de Braganca, MDPediatria HCNo ratings yet
- Eliminating Neurologic Complications of ExtracorpoDocument2 pagesEliminating Neurologic Complications of Extracorpofabiola shoshajNo ratings yet
- Neurocognitive Function and Progression in Patients With Brain Metastases Treated With Whole-Brain Radiation and Motexafin Gadolinium Results of A Randomized Phase III TrialDocument10 pagesNeurocognitive Function and Progression in Patients With Brain Metastases Treated With Whole-Brain Radiation and Motexafin Gadolinium Results of A Randomized Phase III TrialManuel Guerrero GómezNo ratings yet
- Xia 2008Document9 pagesXia 2008Danuza Gandra RossiNo ratings yet
- Cerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDocument11 pagesCerebral Oximetry Monitoring To Maintain Normal Cerebral ExplainDaniel EllerNo ratings yet
- s1042368008000053 PDFDocument14 pagess1042368008000053 PDFKevin EdroNo ratings yet
- Nonmalignant Brain TumorsDocument28 pagesNonmalignant Brain TumorsHenrique OliveiraNo ratings yet
- Mitochondrial Disease and Anesthesia: Vincent C. Hsieh, MD, Elliot J. Krane, MD, and Philip G. Morgan, MDDocument5 pagesMitochondrial Disease and Anesthesia: Vincent C. Hsieh, MD, Elliot J. Krane, MD, and Philip G. Morgan, MDJZNo ratings yet
- Multicenter, Prospective, Single Arm, Open Label, Observational Study of STMS For Migraine Prevention (ESPOUSE Study Starling2018Document11 pagesMulticenter, Prospective, Single Arm, Open Label, Observational Study of STMS For Migraine Prevention (ESPOUSE Study Starling2018CESAR AUGUSTO CARVAJAL RENDONNo ratings yet
- Early Versus Later Anticoagulation For Stroke With Atrial FibrillationDocument11 pagesEarly Versus Later Anticoagulation For Stroke With Atrial Fibrillationguille.1492No ratings yet
- Ketorolac As An Analgesic Agent For Infants and Children After Cardiac SurgeryDocument8 pagesKetorolac As An Analgesic Agent For Infants and Children After Cardiac Surgerydiogofc123No ratings yet
- Artigo InglesDocument11 pagesArtigo InglesEllen AndradeNo ratings yet
- Epilepsia y VIH 4, NoDocument14 pagesEpilepsia y VIH 4, NoDra Carolina Escalante Neurologa de AdultosNo ratings yet
- Serarslan 2017Document5 pagesSerarslan 2017vistamaniacNo ratings yet
- Darzalex PBS Media ReleaseDocument4 pagesDarzalex PBS Media ReleaseJonathonNo ratings yet
- A Randomized, Placebo-Controlled Trial of Natalizumab For Relapsing Multiple SclerosisDocument12 pagesA Randomized, Placebo-Controlled Trial of Natalizumab For Relapsing Multiple Sclerosisarnoldo VazquezNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofNatalia ArizaNo ratings yet
- LancetDocument9 pagesLancetRenju KuriakoseNo ratings yet
- Comparison of Low-Dose Dienogest With Low-Dose Danazol For Long-Term Treatment of AdenomyosisDocument2 pagesComparison of Low-Dose Dienogest With Low-Dose Danazol For Long-Term Treatment of AdenomyosisMohamed ElhelalyNo ratings yet
- P64728A - IAL - Biology - WBI15 - 01 - Jun-2020 Scientific Article 4TH ProofDocument8 pagesP64728A - IAL - Biology - WBI15 - 01 - Jun-2020 Scientific Article 4TH Proofcrocusozan100% (3)
- Brain Tumor Thesis StatementDocument8 pagesBrain Tumor Thesis Statementchristinamartinspringfield100% (2)
- heart failure articleDocument7 pagesheart failure articlefaraz.mirza1No ratings yet
- Dalteparin Versus Unfractionated Heparin in Critically Ill PDocument10 pagesDalteparin Versus Unfractionated Heparin in Critically Ill PPedro BurgosNo ratings yet
- Choosing The Best Operation For Chronic Subdural Hematoma - A Decision Analysis (Journal of Neurosurgery)Document7 pagesChoosing The Best Operation For Chronic Subdural Hematoma - A Decision Analysis (Journal of Neurosurgery)Mon ChávezNo ratings yet
- Manajemen EpistaksisDocument2 pagesManajemen EpistaksistiaraaaindahNo ratings yet
- Current and emerging treatment strategies for Duchenne muscular dystrophyDocument14 pagesCurrent and emerging treatment strategies for Duchenne muscular dystrophyANAMIKA ANANDINo ratings yet
- Cross 2023 PediatricepilepsysurgeryDocument11 pagesCross 2023 PediatricepilepsysurgeryGala GonzalezNo ratings yet
- NDT 12 1795 PDFDocument13 pagesNDT 12 1795 PDFAdrian KhomanNo ratings yet
- Jurnal 1Document9 pagesJurnal 1AnnisNo ratings yet
- Cancer Stem Cells: To The EditorDocument4 pagesCancer Stem Cells: To The Editormira ariantiNo ratings yet
- Mills & Tamnes, 2014.methods and Considerations For Longitudinal Structural Brain Imaging Analysis Across DevelopmentDocument10 pagesMills & Tamnes, 2014.methods and Considerations For Longitudinal Structural Brain Imaging Analysis Across DevelopmentSu AjaNo ratings yet
- Central Nervous System MetastasesFrom EverandCentral Nervous System MetastasesManmeet AhluwaliaNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundDita Putri DamayantiNo ratings yet
- Brain Cancer in CanadaDocument4 pagesBrain Cancer in CanadaRileyNo ratings yet
- Develop Med Child Neuro - 2018 - Chambers - Selective Percutaneous Muscle Lengthening in Cerebral Palsy When There IsDocument1 pageDevelop Med Child Neuro - 2018 - Chambers - Selective Percutaneous Muscle Lengthening in Cerebral Palsy When There IsPrem AnandNo ratings yet
- Strokeaha 107 485649Document8 pagesStrokeaha 107 485649Linh Nguyen DuyNo ratings yet
- Ultrafiltration in Decompensated Heart Failure With Cardiorenal SyndromeDocument9 pagesUltrafiltration in Decompensated Heart Failure With Cardiorenal SyndromeThales YulianusNo ratings yet
- Maris 2007Document15 pagesMaris 2007asialoren74No ratings yet
- New England Journal Medicine: The ofDocument12 pagesNew England Journal Medicine: The ofAna Laura AntunezNo ratings yet
- Trial of Decompressive Craniectomy For Traumatic Intracranial HypertensionDocument12 pagesTrial of Decompressive Craniectomy For Traumatic Intracranial HypertensionV ANo ratings yet
- Target Volume Delineation for Pediatric CancersFrom EverandTarget Volume Delineation for Pediatric CancersStephanie A. TerezakisNo ratings yet
- Radiotherapy in Managing Brain Metastases: A Case-Based ApproachFrom EverandRadiotherapy in Managing Brain Metastases: A Case-Based ApproachYoshiya YamadaNo ratings yet
- Pedoman Diagnosis Dan Penatalaksanaan Hiperglikemia Dalam KehamilanDocument51 pagesPedoman Diagnosis Dan Penatalaksanaan Hiperglikemia Dalam KehamilanCheflak KitchenNo ratings yet
- Disordered Eating Behavior in Individuals With Diabetes: Importance of Context, Evaluation, and ClassificationDocument7 pagesDisordered Eating Behavior in Individuals With Diabetes: Importance of Context, Evaluation, and ClassificationCheflak KitchenNo ratings yet
- NIH Public Access: Author ManuscriptDocument17 pagesNIH Public Access: Author ManuscriptCheflak KitchenNo ratings yet
- Evidence-Based Dexamethasone Dosing in Malignant BDocument17 pagesEvidence-Based Dexamethasone Dosing in Malignant BCheflak KitchenNo ratings yet
- Ge-NOSE - Electronic Nose For Sniffing Food-Borne Bacteria (#668970) - 914547Document4 pagesGe-NOSE - Electronic Nose For Sniffing Food-Borne Bacteria (#668970) - 914547Dadang SaparudinNo ratings yet
- Ramadhan 1442 ScheduleDocument2 pagesRamadhan 1442 ScheduleCheflak KitchenNo ratings yet
- Ramadhan 1442 ScheduleDocument2 pagesRamadhan 1442 ScheduleCheflak KitchenNo ratings yet
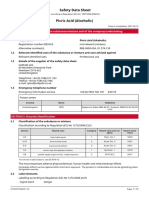
- Safety Data Sheet Picric Acid (Alcoholic)Document14 pagesSafety Data Sheet Picric Acid (Alcoholic)tarek aneesNo ratings yet
- CBT therapy overview: strengths, sessions, evidenceDocument1 pageCBT therapy overview: strengths, sessions, evidencezulkaberNo ratings yet
- SGL 7 (Nutrition Basics 1)Document21 pagesSGL 7 (Nutrition Basics 1)Joo Se HyukNo ratings yet
- Oum Business School: Matriculation No: Identity Card No.: Telephone No.: E-Mail: Learning CentreDocument6 pagesOum Business School: Matriculation No: Identity Card No.: Telephone No.: E-Mail: Learning CentreInspire28No ratings yet
- Tests of Hypothesis Single MeanDocument5 pagesTests of Hypothesis Single MeanMhar G-i SalalilaNo ratings yet
- Sanskrit EssaysDocument4 pagesSanskrit Essaysafibzfwdkaesyf100% (2)
- The Tiger King PDFDocument52 pagesThe Tiger King PDFAnonymous OITciJmAJ4100% (2)
- (Claim#) (Surname) (Firstname) : C1147 Psychology Services Counselling Extension ReportDocument4 pages(Claim#) (Surname) (Firstname) : C1147 Psychology Services Counselling Extension ReportDawn CasuncadNo ratings yet
- 22-23 Pan Sloan Canyon Student Parent HandbookDocument81 pages22-23 Pan Sloan Canyon Student Parent Handbookapi-470026636No ratings yet
- Craftsman Compressor User ManualDocument60 pagesCraftsman Compressor User ManualMichael ShafferNo ratings yet
- Bm101: Biology For Engineers: Instructor: Yashveer Singh, PHDDocument23 pagesBm101: Biology For Engineers: Instructor: Yashveer Singh, PHDhimanshu singhNo ratings yet
- Allen Wheelis 1956, Will On PsychoanalysisDocument19 pagesAllen Wheelis 1956, Will On Psychoanalysisjk2001No ratings yet
- Colonic Irrigation: Holistic Cleansing and DetoxificationDocument5 pagesColonic Irrigation: Holistic Cleansing and DetoxificationVijaya RaniNo ratings yet
- FLACC ScaleDocument2 pagesFLACC ScaleN Novi Kemala SariNo ratings yet
- Infant Formula and Early Childhood CariesDocument5 pagesInfant Formula and Early Childhood Cariesmutiara hapkaNo ratings yet
- Introduction To Consumer Behaviour: Oxford University Press Sample ChapterDocument51 pagesIntroduction To Consumer Behaviour: Oxford University Press Sample ChapterMuhammad Imran AwanNo ratings yet
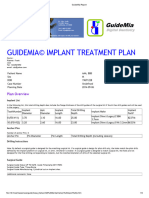
- GuideMia Sample Report - EnglishDocument9 pagesGuideMia Sample Report - Englishzhiao liuNo ratings yet
- Test Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleDocument13 pagesTest Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleAnthonyRiveraqion100% (32)
- Instructions: Answer What Are Being Asked ForDocument23 pagesInstructions: Answer What Are Being Asked ForCatlyn Tagala CalzadoNo ratings yet
- The Hospital Noise Project: Lessons On Addressing Noise From 241 U.S. HospitalsDocument50 pagesThe Hospital Noise Project: Lessons On Addressing Noise From 241 U.S. HospitalsmanishNo ratings yet
- Prelim ncm105Document4 pagesPrelim ncm105klirt carayoNo ratings yet
- Nutrient Solutions: For Controlled Environment AgricultureDocument13 pagesNutrient Solutions: For Controlled Environment AgriculturefozihpaNo ratings yet
- Rusty Moore Visual Impact For WomenDocument34 pagesRusty Moore Visual Impact For Womenchrisie00757% (7)
- FdarDocument4 pagesFdarCecile DavantesNo ratings yet
- Resume: Reasons To Choose This BookDocument5 pagesResume: Reasons To Choose This BookAbu Yazid BusthamiNo ratings yet
- Baby Friendly Hospital Initiative (Bfhi)Document9 pagesBaby Friendly Hospital Initiative (Bfhi)Ankita BramheNo ratings yet
- Dorothy JohnsonDocument9 pagesDorothy JohnsonMarianne Collantes BuendiaNo ratings yet
- Dip Slides For Surfaces and in Liquids, Envirocheck®: MicrobiologyDocument1 pageDip Slides For Surfaces and in Liquids, Envirocheck®: MicrobiologyHaad AhmedNo ratings yet
- FCPS 1 Radiology + AnswersDocument25 pagesFCPS 1 Radiology + AnswersZahid Qamar100% (2)
- JMP 2023 Wash HouseholdsDocument172 pagesJMP 2023 Wash Householdsmadiha.arch24No ratings yet