Professional Documents
Culture Documents
Perazella - 2018 - Pharmacology Behind Common Drug Nephrotoxicities-4
Uploaded by
Oneng IfayaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Perazella - 2018 - Pharmacology Behind Common Drug Nephrotoxicities-4
Uploaded by
Oneng IfayaniCopyright:
Available Formats
1900 Clinical Journal of the American Society of Nephrology
Accumulation of high concentrations of the polycationic inhibitors, and aminosalicylates (49–53). Newer agents such
aminoglycosides within intracellular lysosomes causes as the immune checkpoint inhibitors (ipilimumab, nivolumab,
lysosomal injury, which is associated with phospholipid pembrolizumab) cause AIN via activation of T cells and
membrane injury, oxidative stress, and mitochondrial dys- perhaps reducing tolerance to exogenous drugs (54–56). As
function. This promotes proximal tubular cell apoptosis and will be discussed, the patient’s genetic makeup may enhance
necrosis with clinical manifestations such as an isolated immunogenicity to exogenous agents.
proximal tubulopathy or AKI (5–7,40–42).
Amphotericin B, and the lipid/liposomal formulations Drug-Induced Cast Nephropathy
to a lesser degree, cause kidney injury by disrupting tubular Another intriguing drug-related kidney injury is vancomycin-
cell membranes and increasing permeability to cations, related obstructive tubular cast formation. Using immuno-
which result in tubular dysfunction due to cell swelling/ histologic staining techniques to detect vancomycin in kidney
dysfunction (40). In general, the lipid/liposomal formula- tissue, casts composed of noncrystal nanospheric vancomy-
tions are less nephrotoxic. The polymixin antimicrobial cin aggregates entangled with uromodulin have been ob-
agents, colistin and polymyxin B, are highly nephrotoxic served in patients with AKI (57). In these patients, high
with a very narrow therapeutic window. Nephrotoxicity vancomycin trough plasma levels were observed. These
is related to their D-amino content and fatty acid compo- same vancomycin casts were reproduced experimentally in
nent, which increases cellular membrane permeability and mice using in vivo imaging techniques. Thus, the interaction
allows cation influx (41). This effect leads to tubular cell of uromodulin with nanospheric vancomycin aggregates re-
swelling and lysis with AKI development. presents a new mode of tubular injury with development of
The acyclic nucleotide phosphonates (adefovir, cidofovir, vancomycin-associated cast nephropathy (57).
tenofovir) enter the cell via basolateral human organic anion
transporter–1(hOAT-1) and promote cellular injury primarily
through disturbing mitochondrial function. Mitochondrial The Patient
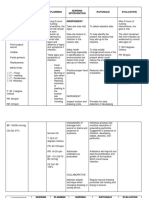
injury is manifested by mitochondrial enlargement, clumped There are a number of patient-specific factors that in-
cristae, and convoluted contours that impair cellular ener- crease risk for medication-induced nephrotoxicity (Figure
getics (8,10,26,43). Tenofovir, which is employed widely to 2, Table 2). Underlying risk factors for nephrotoxicity may
treat hepatitis B virus and HIV infection, is associated with be nonmodifiable, such as older age and female sex, which
proximal tubulopathy and AKI (8,10,26,43). are associated with decreased lean body mass and reduced
Antiangiogenesis therapy with monoclonal antibodies total body water that can lead to excess drug dosing (6–9).
against vascular endothelial growth factor (VEGF), circu- A “normal serum creatinine” in these patients may actually
lating soluble VEGF receptors, and small molecule tyrosine be a lower GFR. Women and the elderly have lower serum
kinase inhibitors that impair intracellular VEGF signaling albumin concentrations—hypoalbuminemia results in re-
pathways are associated with various forms of kidney duced drug binding and increased free drug concentrations
injury (11,44–47). In the kidney, VEGF is produced by that can be nephrotoxic (6–9,35–38). In addition to these
podocytes and binds glomerular and peritubular capillary factors, the elderly have an increased propensity to vaso-
endothelial cell VEGF receptors. Glomerular endothelial constriction from excessive circulating angiotensin II and
VEGF receptor binding maintains normal fenestrated endothelin levels and have higher levels of oxidatively
endothelial health and is important for normal functioning modified biomarkers (58). These factors combine to in-
of the glomerular basement membrane (11,44–47). Reduc- crease patient exposure to excess drug concentrations and
tion in VEGF levels or signaling pathways by antiangio- nephrotoxicity risk.
genic drugs promotes loss of the healthy fenestrated
endothelial phenotype and promotes microvascular injury Genetic Makeup
and thrombotic microangiopathy, causing proteinuria and Along the lines of nonmodifiable risk factors is the patient’s
AKI. Reduced nephrin expression in the slit diaphragms underlying genetic makeup. In fact, the role of pharmacogenetics
may also contribute to the development of proteinuria. Al- as an explanation for the heterogeneous patient response
though other kidney lesions occur with these drugs, endo- to drugs (underdosing, therapeutic dosing, and overdosing)
thelial injury and thrombotic microangiopathy are most reflects genetic makeup and supports the need for “person-
common (11,44–47). By interfering with local alternative alized” or “precision” medicine. As such, underlying host
complement pathway regulators, these drugs may also genetic makeup can enhance vulnerability of the kidney to
activate complement and increase risk for TMA (48). potential nephrotoxins (59–63). There are data that sug-
gest that metabolic pathways, transport proteins, and drug
Drug-Induced Inflammation transporters vary between patient populations due to the
Another pathway of drug-induced nephrotoxicity is effect of genetic composition. Several enzymes that com-
through induction of an inflammatory response by the prise the hepatic cytochrome P450 (CYP450) enzyme
host, which can target the kidney (49–53). Through multiple system have gene polymorphisms that are associated with
mechanisms (hapten/prohapten, molecular mimicry, immu- reduced drug metabolism and subsequent end organ toxicity.
ne-complex formation), medications can promote the devel- Because the kidney also possesses CYP450 enzymes that
opment of acute interstitial nephritis (AIN) leading to AKI participate in drug metabolism (59–63), it is not surprising
and/or various urinary abnormalities such as tubular that gene polymorphisms favoring reduced drug metabolism
proteinuria, pyuria, and hematuria (49–52). Classic drugs could increase nephrotoxic risk.
associated with AIN include antimicrobial agents (in partic- Polymorphisms of genes encoding proteins involved in
ular B-lactams and sulfonamides), NSAIDs, proton pump the metabolism and subsequent elimination of drugs by the
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Pmed 1002595 s003Document2 pagesPmed 1002595 s003Oneng IfayaniNo ratings yet
- Biostatistics: Descriptive Analysis and Differences Between GroupsDocument17 pagesBiostatistics: Descriptive Analysis and Differences Between GroupsOneng IfayaniNo ratings yet
- Intervention Type Quality AssessmentDocument5 pagesIntervention Type Quality AssessmentOneng IfayaniNo ratings yet
- PRISMA 2009 Checklist: Section/topic # Checklist Item Reported On Page #Document3 pagesPRISMA 2009 Checklist: Section/topic # Checklist Item Reported On Page #Oneng IfayaniNo ratings yet
- Biostatistics 1Document20 pagesBiostatistics 1Oneng IfayaniNo ratings yet
- Sample Size Required Per Group When Using The T Test To Compare Means of Continuous VariablesDocument11 pagesSample Size Required Per Group When Using The T Test To Compare Means of Continuous VariablesOneng IfayaniNo ratings yet
- Chapter 14Document15 pagesChapter 14Oneng IfayaniNo ratings yet
- Adverse Drug Reactions: Type C - Continuous Reactions Due To Long-Term Drug UseDocument9 pagesAdverse Drug Reactions: Type C - Continuous Reactions Due To Long-Term Drug UseOneng IfayaniNo ratings yet
- Chapter 8Document30 pagesChapter 8Oneng IfayaniNo ratings yet
- Chapter 9Document23 pagesChapter 9Oneng IfayaniNo ratings yet
- Chapter 4Document11 pagesChapter 4Oneng IfayaniNo ratings yet
- Conceiving The Research Question and Developing The Study PlanDocument9 pagesConceiving The Research Question and Developing The Study PlanOneng IfayaniNo ratings yet
- Chapter 1Document12 pagesChapter 1Oneng IfayaniNo ratings yet
- Quality of Antimikrobial - En.idDocument4 pagesQuality of Antimikrobial - En.idOneng IfayaniNo ratings yet
- Vandergarde Thorax2006Document5 pagesVandergarde Thorax2006Oneng IfayaniNo ratings yet
- Applied Statistics Survival AnalysisDocument23 pagesApplied Statistics Survival AnalysisOneng IfayaniNo ratings yet
- Statistik Deskriptif - SDA 2Document30 pagesStatistik Deskriptif - SDA 2Oneng IfayaniNo ratings yet
- Biochemistry and Cell Biology of Dopaminergic NeurotransmissionDocument18 pagesBiochemistry and Cell Biology of Dopaminergic NeurotransmissionOneng IfayaniNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Subjective Well-Being - WikipediaDocument13 pagesSubjective Well-Being - WikipediaDiana GhiusNo ratings yet
- Mercy KillingDocument37 pagesMercy KillingRamesh Babu Tatapudi100% (1)
- Government of Nunavut EHB Policy GuidelinesDocument5 pagesGovernment of Nunavut EHB Policy GuidelinesNunatsiaqNewsNo ratings yet
- Gastrointestinal System: Git Brief Introduction: Dr. S. M. A. WaseemDocument20 pagesGastrointestinal System: Git Brief Introduction: Dr. S. M. A. WaseemHoping HeartsNo ratings yet
- Usmle QDocument46 pagesUsmle QRoh Jiten100% (1)
- Case Study Genome Edited Human EmbryosDocument2 pagesCase Study Genome Edited Human EmbryosDivya Dharshini RNo ratings yet
- Appointments Boards and Commissions 09-01-15Document23 pagesAppointments Boards and Commissions 09-01-15L. A. PatersonNo ratings yet
- Natural History of HIV Infection by DR A K Gupta, Addl. Project Director, DSACSDocument29 pagesNatural History of HIV Infection by DR A K Gupta, Addl. Project Director, DSACSdr.a.k.gupta6924100% (3)
- Owen A O'Connor, Stephen M Ansell, John F Seymo 230518 053705Document514 pagesOwen A O'Connor, Stephen M Ansell, John F Seymo 230518 053705Juan RivasNo ratings yet
- Msds HCL 0,1 NDocument6 pagesMsds HCL 0,1 NRinie Aeryn Nayndine'netzzNo ratings yet
- ProteusDocument20 pagesProteusMonishaNo ratings yet
- Biomedical Engineering Presentation With VideoDocument13 pagesBiomedical Engineering Presentation With VideoJi Hun YangNo ratings yet
- Are Viruses Alive The Replicator Paradigm Sheds Decisive Light On Anold But Misguided Question PDFDocument10 pagesAre Viruses Alive The Replicator Paradigm Sheds Decisive Light On Anold But Misguided Question PDFAdriana MontañaNo ratings yet
- Acute Kidney Injury in Patients With CancerDocument13 pagesAcute Kidney Injury in Patients With CancerzikryauliaNo ratings yet
- General Biology Modules 1 3Document36 pagesGeneral Biology Modules 1 3Glen MillarNo ratings yet
- Campylobacter Spp. and Related Organisms in PoultryDocument212 pagesCampylobacter Spp. and Related Organisms in PoultryNicku MalanceaNo ratings yet
- General Biology Last Set of ActivitiesDocument2 pagesGeneral Biology Last Set of ActivitiesAubrey GuilaranNo ratings yet
- GCE Biology Marking Scheme (January 2007)Document21 pagesGCE Biology Marking Scheme (January 2007)potterhead1DNo ratings yet
- SCHWANNOMADocument4 pagesSCHWANNOMAAshwani Kumar Pati TripathiNo ratings yet
- Mgs Syllabus ZOOLOGY PDFDocument32 pagesMgs Syllabus ZOOLOGY PDFhsjsjNo ratings yet
- Patel Hospital: Molecular PathologyDocument1 pagePatel Hospital: Molecular PathologyFarrukh NaveedNo ratings yet
- Fallout TTRPG v2.0 PDFDocument179 pagesFallout TTRPG v2.0 PDFJavontay PeoplesNo ratings yet
- NCP - JaundiceDocument5 pagesNCP - JaundiceQueen Shine0% (1)
- Cell and Organs of The Immune SystemDocument43 pagesCell and Organs of The Immune Systemcyrhenmie100% (1)
- Biochemistry of AgingDocument2 pagesBiochemistry of AgingKaedehara KazuhaNo ratings yet
- Biochemistry: Pharmaglimps-A Glimpse of PharmacyDocument38 pagesBiochemistry: Pharmaglimps-A Glimpse of PharmacySHRIKANTNo ratings yet
- In-Depth: How Does A Child Get A Pectus Excavatum?Document12 pagesIn-Depth: How Does A Child Get A Pectus Excavatum?Gino VillanuevaNo ratings yet
- Joseph MerrickDocument12 pagesJoseph Merrickyairherrera100% (1)
- Autism Spectrum Disorder (ASD) in Girls. Co-Occurring Psychopathology. Sex Differences in Clinical ManifestationDocument11 pagesAutism Spectrum Disorder (ASD) in Girls. Co-Occurring Psychopathology. Sex Differences in Clinical ManifestationRania shafiraNo ratings yet
- GE IV TH SemDocument185 pagesGE IV TH Semrahul vivekNo ratings yet