Professional Documents
Culture Documents
Comparison Between View Summing and Tube Pulsing in Ultra Low Dose CT Acquisitions For PET Attenuation Correction
Uploaded by
Hernan PerezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Comparison Between View Summing and Tube Pulsing in Ultra Low Dose CT Acquisitions For PET Attenuation Correction
Uploaded by
Hernan PerezCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/279999743
Comparison between View Summing and Tube Pulsing in Ultra Low Dose CT
Acquisitions for PET Attenuation Correction
Conference Paper · November 2014
CITATIONS READS
0 880
5 authors, including:
Adam Alessio Paul E Kinahan
Michigan State University University of Washington Seattle
179 PUBLICATIONS 3,395 CITATIONS 475 PUBLICATIONS 19,079 CITATIONS
SEE PROFILE SEE PROFILE
Bruno De Man
GE Global Research
141 PUBLICATIONS 3,411 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
GPU based Fast Projection and Backprojection model development View project
CT research View project
All content following this page was uploaded by Paul E Kinahan on 18 July 2015.
The user has requested enhancement of the downloaded file.
X-ray pulsing methods for reduced-dose computed tomography in
PET/CT attenuation correction
Uwe Wiedmann1, V. Bogdan Neculaes1, Dan Harrison1, Evren Asma1, Paul E Kinahan2 and Bruno
De Man1
1
GE Global Research Center, Niskayuna, NY, USA
2
University of Washington, Seattle, WA, USA
ABSTRACT
The image quality needed for CT-based attenuation correction (CTAC) is significantly lower than what is used currently
for diagnostic CT imaging. Consequently, the X-ray dose required for sufficient image quality with CTAC is relatively
small, potentially smaller than the lowest X-ray dose clinical CT scanners can provide. Operating modes have been
proposed in which the X-rays are periodically turned on and off during the scan in order to reduce X-ray dose. This study
reviews the different methods by which X-rays can be modulated in a CT scanner, and assesses their adequacy for low-
dose acquisitions as required for CTAC. Calculations and experimental data are provided to exemplify selected X-ray
pulsing scenarios. Our analysis shows that low-dose pulsing is possible but challenging with clinically available CT
tubes. Alternative X-ray tube designs would lift this restriction.
Keywords: Pulsing, X-rays, Computed tomography, CT-based attenuation correction, PET/CT, low-dose, sparse
sampling
1. INTRODUCTION AND MOTIVATION
Positron Emission Tomography (PET) combined with X-ray Computed Tomography (CT) has become a primary tool for
oncology diagnosis and staging during the last decade [1]. Quantitative assessment of therapy-induced changes in tumor
18F-FDG uptake may allow for the prediction of tumor response and patient outcome very early in the course of therapy
[2]. The CT component in a PET/CT system provides precise anatomical localization of regions identified on the PET
tracer uptake images. In addition the CT image is used for CT-based attenuation correction of the PET emission data, an
essential step for quantitative PET imaging [3].
Under the constraint of using a standard clinical X-ray CT scanner, there are several potential methods for reducing CT
radiation dose for CT-based attenuation correction (CTAC) and for reducing the bias and noise that are characteristic of
low dose CT images [4]. Potentially the most important of these is the recognition that diagnostic CT images usually
have a higher signal to noise ratio and resolution than is necessary for CTAC, due to the relatively higher noise and
lower resolution imposed by PET imaging physics. This recognition allows for the use of several simple strategies to
enable CT radiation dose reduction while maintaining or improving PET image quality [5], [6].
In this study we evaluate the feasibility of such 'pulsing' methods, where the X-ray tube is switched on and off during
rotation to provide fewer views, but with the same total radiation dose as a typical reduced-dose CT scan. Clinical CT
scanners typically use a continuous high-flux X-ray illumination on a rotating gantry, with approximately 1000 views or
snapshots of X-ray attenuation per gantry revolution [7]. High flux and fine sampling is needed for diagnostic CT image
quality, but not for CTAC where one only needs the line integrals of the 511 keV linear attenuation coefficients.
The noise in energy-integrating CT detectors is well modeled as a compound Poisson process with an additive Gaussian
electronic noise process. At low photon fluxes the electronic noise dominates, introducing non-positive values into the
raw data, confounding the initial log operation and introducing artifacts. By using fewer views, but with the same total
number of photons (i.e. integrated signal) the effect of the electronic noise is reduced with little or no impact on PET
attenuation correction and subsequent PET image quality.
Our approach is based on a comparison of potential methods and modeling the basic X-ray tube physics to predict
expected operational limitations. From these analyses we predict the potential operating requirements for such a system.
Medical Imaging 2014: Physics of Medical Imaging, edited by Bruce R. Whiting, Christoph Hoeschen, Despina Kontos,
Proc. of SPIE Vol. 9033, 90332Z · © 2014 SPIE · CCC code: 1605-7422/14/$18 · doi: 10.1117/12.2043021
Proc. of SPIE Vol. 9033 90332Z-1
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
2. APPROACHES FOR DOSE REDUCTION
We here describe several dose reduction approaches, with their advantages and disadvantages. An overview of these
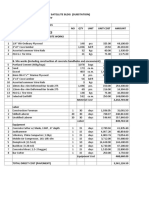
methods is given in Table 1.
One approach to reduce dose in a conventional CT system is by reducing the X-ray tube current and thus reducing the
flux level.
A second method is to increase the gantry rotation speed and thus reduce the exposure duration per rotation. The
sampling rate is increased here correspondingly to maintain a constant number of views per rotation.
A third approach consists of inserting a (static) spectral filter in the X-ray beam before it reaches the patient. Spectral
filtering is particularly effective in reducing skin dose [8]: it removes the lower energy photons, which do not penetrate
through the patient. While typical Radiography/Fluoroscopy (R/F) systems are limited to 0.3 mm maximum copper filter
thickness [8], the more expensive vascular systems have copper thicknesses up to 0.9 mm [9]. In CT systems, the
inherent filtration of the central ray is on the order of 7 mm Aluminum equivalent [10], corresponding to roughly 1 mm
copper filtration.
All three methods will result in a reduced detector signal for each view. The X-ray emission follows a Poisson process.
The X-rays that have penetrated through the patient are typically converted to light in a scintillator, which in turn
generates photo-electric electrons in a photodiode. The charge of those electrons is then read out by a noisy electronic
channel. Each of the detector views has a separate integration period and the electronics adds a relatively constant
variance noise for each view. At moderate and high integrated flux levels, the detected signal fluctuation (noise) is
dominated by the Poisson statistics of the X-rays. At low integrated flux levels, electronic noise is the most significant.
The dominance of electronic noise at low photon fluxes introduces significant errors and drastically reduces the photon
information content. Hence we are interested in reducing the dose while avoiding the regime where electronic noise has a
considerable impact.
One way to achieve this is to turn off the X-ray source during some views and ignore the associated X-ray-Off view data,
as illustrated in Fig. 1 (right-hand side). The integrated flux in each active view remains high and therefore the electronic
noise remains insignificant. This results in sparse view sampling, making the reconstruction more ill-posed (incomplete
data). Recently compressed sensing approaches have been proposed to achieve good image quality from sparse
measurements [11].
Alternatively, we can reduce the tube current and at the same time reduce the angular sampling rate. Again, the
integrated flux in each view remains high and the electronic noise remains insignificant. A possible disadvantage is the
fact that the increased azimuthal blur (rotational blur) makes it harder for reconstruction to recover good spatial
resolution (more ill-posed). In the pulsed approach we still have limited sampling, but techniques such as compressed
sensing have a better chance to still recover high resolution images.
Table 1. Overview of dose reduction approaches along with their relative electronic noise impact and data completeness.
Increase rotation Reduce tube
Reduce tube
speed & increase Spectral filter Pulsing current & reduce
current
sampling rate sampling rate
Tube current = = =
Sampling rate = = =
View duration = = =
mAs per view = = =
E-noise impact High (bad) High (bad) High (bad) Low (good) Low (good)
Data
Good Good Good Bad Bad
completeness
Proc. of SPIE Vol. 9033 90332Z-2
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
X-ray tube motion with gantry rotation
1 2
4
relative
1
0 X-ray
intensity
continuous pulsed
acquisition acquisition
X-ray
fan
beam
Figure 1. Illustration of two methods to reduce the dose. The left side – region 1 – shows a reduction in tube current. The
right side – region 2 – shows a pulsed approach, in which case the same total intensity of photons is divided into a subset of
the views with higher intensity. In this example the tube is off ¾ of the time for a 25% duty cycle, and on at 4x the intensity
of the continuous acquisitions. Thus total radiation dose is the same for both modes.
In this paper we focus on describing various methods for achieving tube current pulsing, and we present calculations and
experimental data for selected approaches.
3. PULSING REQUIREMENTS
In a state-of-the-art CT scanner, the X-ray tube rotates around the patient, at a typical speed of 0.35 s to 2 s per rotation,
and the equipment samples up to 2496 views per rotation [12], i.e. up to one view every 140 µs [12]. This is 2.5 times
more views per rotation [13] than a typical system with 1000 views per rotation [7]. Such a typical system would have a
view duration of 1 ms at a speed of one rotation per second.
In a standard CT system, X-rays are emitted continuously during the exposure, and the fast read-out electronics of the
detector sample the integrated signal at the end of each view duration. In that case, X-rays are turned on and off only
once for each scan, and rise and fall durations are of little importance.
However, for pulsing on a view-by-view basis, we want the on/off transition times to be at least one order of magnitude
shorter than the view duration. This implies that the on/off transition times for each pulse should be 10 µs to 100 µs,
since the view duration is on the order of 100 µs to 1 ms. For CTAC, operation at the slower end of these ranges is
sufficient, due to the relatively low image quality required for this application.
4. X-RAY GENERATION PHYSICS MODEL
In most clinically available X-ray tubes, schematically illustrated in Fig. 2, electrons are emitted into a vacuum by
heating the emitter/cathode, typically a filament similar to the one encountered in the conventional light bulb, by passing
a current through it. Those negatively charged electrons are then accelerated towards the anode, by acceleration voltages
on the order of 100 kV. In some X-ray tubes, the electron beam can be suppressed by applying a much smaller negative
voltage to an additional grid electrode, located in the proximity of the emitter/cathode – shown in Fig. 2. When the
electrons hit the metallic anode, they generate X-rays, which can leave the X-ray tube only through a predefined
relatively small fixed output window. The spectral content of the X-ray beam is adjusted by inserting one of several
spectral filters, and the X-rays are then collimated to the clinically required beam size.
Proc. of SPIE Vol. 9033 90332Z-3
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
1mA…1000mA
Tube Current
X-Ray Tube
Spectral Filter
Output
Window Collimator
Tube =
Voltage Target (Anode)
X-Rays
40kV…150kV Electron Beam
Grid = Emitter
Grid Electrode
Voltage (Cathode)
-1kV…-10kV
2A…10A
Filament Current
Figure 2. Schematic drawing of an X-ray tube. Gridding capability is added here – although currently only available for
interventional tubes.
In the next section we present an overview of tube pulsing and modulation technologies along with their strengths and
weaknesses.
5. OVERVIEW OF THE X-RAY TUBE PULSING METHODS
Pulsing of the X-ray output can be realized by several means, summarized in Table 2, each with its own advantages and
disadvantages:
Mechanical collimation: While CT systems typically have collimators to adjust the coverage, the speed of
these collimators is on the order of 10 mm/s [14]. This results in transition times on the order of 100 ms, which
is about three orders of magnitude slower than what is required for dose modulation on a view-by-view basis.
Emitter temperature: Modulation of the emitter temperature is commonly used for dose reduction features
such as smart mA, where the tube current is modulated as a function of gantry angle and longitudinal patient
position (Z axis) [15]. With the emitter typically being a filament, its temperature can be adjusted by
modulating the heating current that is forced through it. However, just as in a conventional light bulb, the
cooling of the filament in the vacuum takes on the order of 100 ms [15], which is far too slow for current
modulation on a view-by-view basis.
High-voltage switching: This method, also called kVp switching, makes use of the intrinsic capability of any
high-voltage generating device to switch the high voltage on and off. Fig. 3 illustrates the relationship between
tube current and tube voltage at a constant emitter temperature. Tube voltage dynamics will determine the tube
current dynamics. The tube voltage dynamics, in turn, are limited by the time it takes to charge and discharge
the high-voltage capacitance of the X-ray generator and the high-voltage tank. As a result, rise and fall times
may be non-negligible in some applications, as illustrated in Fig. 4. Not only do the rise and fall tails limit the
minimum pulse duration, but they also generate soft X-rays. These soft X-rays are undesirable, as they are
nearly entirely absorbed in the patient, which means that they contribute to patient dose, but only marginally to
the image [16].
Proc. of SPIE Vol. 9033 90332Z-4
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
Gridding: X-ray gridding uses the same principle as the triode, which was the precursor of our modern
transistor. While the emitter remains hot, and the high voltage applied between the cathode and the anode of the
X-ray tube remains constant, an additional much smaller voltage is applied to a third electrode, called the grid
electrode (Fig. 2), which is typically located around the cathode. This smaller voltage, applied between the
cathode and the grid electrode, is sufficient to suppress the electron beam that normally forms between the
cathode and the anode. This pulse generation method is commonly used in interventional imaging [17], and
illustrated in Fig. 5. The high voltage is applied continuously, the high-voltage capacitance of the X-ray
generator and the high-voltage tank does not need to be discharged into the X-ray tube at each pulse end, and
much smaller pulses are achievable compared to high-voltage switching. In vascular applications that use
gridding, the smallest pulse charge typically used is 0.02 mAs, with a tube current of 3 to 4 mA, and a pulse
width of 5 to 6 ms [8]. Some devices allow making even smaller pulses, down to 0.002 mAs at 1 mA [18]. This
makes gridding a promising technology for dose-efficient CTAC. It must be noted that X-ray gridding for
vascular applications is typically limited to a maximum repetition rate of 30 pulses per second [18], which is
significantly slower than what is needed for CTAC.
Extraction grid: X-ray sources used in multi-source CT use extraction mesh grids on top of the cathode that
are designed for ultra-fast modulation, in the µs range, and they have successfully been demonstrated on a
research CT prototype [19]. The multi-source technology is intrinsically capable of generating pulses at lower
repetition rates for dose reduction. However, this technology is not used in clinically available CT systems.
Table 2. Overview of X-ray pulsing approaches along with their relative speed and availability.
Emitter High-voltage
Collimation Gridding Extraction grid
temperature switching
Speed Slow Slow Intermediate Fast Fast
Additional
None None None Grid & Supply Grid & Supply
Hardware
Hardware Available Research &
Availability Available Available
ready (vascular only) Development
Tube Current
Tube Voltage
Figure 3. Schematic drawing of tube current as a function of tube voltage, for an X-ray tube with a thermal emitter at a given
temperature. This type of dependency can be applied to high-voltage switching. Tube voltage here goes up to roughly
100 kV, while tube current is on the order of 100 mA.
Proc. of SPIE Vol. 9033 90332Z-5
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
Tube Voltage
Tube Current
Time
Figure 4. Schematic drawing of tube voltage and tube current waveforms of a high-voltage switched pulse. Note that the
tube current is a function of tube voltage, as illustrated in Fig. 3.
Tube Voltage
Tube Current
Time
Figure 5. Schematic drawing of tube voltage and tube current waveforms of a gridded pulse. Note that the tube voltage is
stable during the entire pulse duration.
In the next sections we provide a more detailed description of two pulsing technologies at opposite ends of the spectrum
in terms of maturity in clinical systems: high-voltage switching (that is available for implementation in CT systems
today, without hardware changes), and extraction grid as used in multi-source technologies (an elegant, hardware based
approach, demonstrated on research CT prototypes, but not available on clinical systems).
6. X-RAY TUBE PULSING THROUGH HIGH-VOLTAGE SWITCHING
6.1 High-voltage switching overview
In a typical high-voltage generator, an incoming alternating current (AC) is fed into a high-voltage transformer (Fig. 6).
The output of the transformer is then rectified with diodes, and filtered with a capacitor [20], [21]. The high-voltage
cable capacitance provides additional filtering.
Proc. of SPIE Vol. 9033 90332Z-6
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
High-Voltage Rectifier High-Voltage X-Ray
Transformer & Filter Cable Tube
Anode
AC Power
Supply
Cathode
Figure 6: High-voltage circuit equivalent schematics.
The AC Power Supply is typically regulated to achieve a constant X-ray tube voltage during the exposure, and the supply
is switched off at the end of the exposure. At this point, the energy stored in the rectifying and filtering capacitors will
discharge into the X-ray tube – this energy cannot go back to the power supply due to the diodes in the rectifying stage.
This leads to a tube voltage tail (Fig. 7), and an associated tube current tail. The smallest exposure possible is limited by
the size of this tail.
90
80
70
>
Y
60
50
cq) 40
> 30
á 20
~ 10
0
10
-0.2 0.0 0.2 0.4 0.6 0.8 1.0 12
Time (ms)
Figure 7: Measured data for a high-voltage switched tube pulse, nominally operating at 80kVp and 400mA [22].
In high-voltage switched pulsing, each pulse is a separate exposure with its own tail. During the tailing time, the tube
voltage decreases, and softer X-rays are created. These softer X-rays are more strongly absorbed by the patient, which
means that they contribute to patient dose, but only marginally to the image [16]. Softer X-rays are also created during
the voltage rise interval, but since the rise time is typically a lot shorter, we ignore that part in the following discussion.
The finite duration of the tail has two implications. First, there is a minimum amount of dose associated with each pulse,
hence a constraint on the number of pulses to remain below a maximum dose level. Second, there is a finite time
associated with each pulse and hence, for a given rotation time, a limit on the number of pulses that can be fired.
The charge and the size of the tail will be quantified in subsection 6.2. The dose constraints are studied in subsection 6.3
and the timing constraints in subsection 6.4.
6.2 Minimum pulse charge and tail size
The high-voltage capacitance of a medical X-ray system is typically on the order of 1 nF [17], with its main contributors
being the high-voltage generator and the high-voltage cable. While a portion of this overall capacitance is due to discrete
capacitors in the high-voltage tank, parasitic capacitances are a significant contributor, such as the high-voltage cable
with typically 100-200 pF/m [23]. The charge Q stored in the high-voltage capacitance C at a voltage V is given by
Q C V (1)
Typical values of high-voltage capacitance C=1nF and tube voltage V=100kV result in a minimum charge per pulse of
Q=0.1mAs. As a sanity check, we compare the minimum pulse charge of Q=0.1mAs to the minimum pulse of a recent
vascular system, which in high-voltage switching mode is 0.2 mAs [18]. A vascular system typically has longer high-
voltage cables than a CT system, and therefore larger high-voltage capacitance, which leads to larger minimum pulses
and confirms the estimate.
Proc. of SPIE Vol. 9033 90332Z-7
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
Each time the high voltage is increased, this capacitance needs to be charged. The higher the target voltage V, the higher
the charge Q, and the longer it takes to charge this capacitance with a generator having a finite output power capability.
The tube voltage rise duration may be either
Limited by control performance: Rise duration is independent of tube current, or
Limited by AC supply power (Fig. 6): Rise duration increases with increasing tube current.
Fig. 7 illustrates a case where rise duration is approximately equal to decay duration, implying that pulse charge during
tube voltage rise is approximately equal to pulse charge during tube voltage decay.
On the other hand, each time the high voltage needs to be decreased, this high-voltage capacitance needs to be
discharged. As simple power supplies, including high-voltage generators, typically comprise a rectifier that only allows
an output current in one direction, this charge Q cannot go back to the power supply at the end of the pulse, but instead it
needs to be dissipated into the X-ray tube. This is done through the tube current I, with
t2
Q1 Q2 I t dt (2)
t1
where t1 and t2 denote the start and end of the voltage decay, respectively, and Q Q1 Q2 is the amount of charge
that needs to be discharged. Assuming constant tube current during the discharge, we get a lower bound of the discharge
time from
Q
tdischarge (3)
I
So for a charge of 0.1mAs and a tube current of 100mA, the discharge time is approximately 1ms.
The minimum dose in each pulse is the sum of the rise time dose and the discharge time dose. The charge delivered to
the X-ray tube during the rise time can be approximated as tube current multiplied by rise time. The charge delivered to
the X-ray tube during high-voltage discharge was derived above. Based on this minimum overall pulse charge we can
compute a maximum number of pulses, i.e. where the dose would reach parity with the continuous low mA scan. This is
represented by the solid blue curve in Fig. 8.
Proc. of SPIE Vol. 9033 90332Z-8
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
Maximum Number of Pulses per Rotation
1000
Max. Number of Pulses
100
10 Time Limit
Dose Limit
Dose Limit with Additional Filtering
Max. # of Pulses
Max. # of Pulses with Add. Filtering
1
1 10 100 1000
Tube Current (mA)
Figure 8: Maximum number of pulses per rotation, with respect to the time limit (red line) and dose limit (blue lines). Time
limit is calculated for the case where the pulses follow each other without off-time. Dose limit is for same dose as a
continuous exposure at 10mA, 0.5s/rot. Other parameters used are tube voltage 100kV, cable capacitance 1nF, and pulse rise
time 0.2ms. The dashed blue line illustrates a case where spectral filtering reduces patient dose in the pulsed mode by a
factor of 10. The green circles correspond to the maximum number of pulses that satisfy both the time limit and the dose
limit, in the case without and with additional filtering.
In the next two subsections we are going to assess the performance of high-voltage switching with respect to two criteria:
reduction of patient dose, and shortest achievable pulse duration.
6.3 Maximum number of pulses for same dose as standard CT (assuming same spectral filtering)
Let us now compare high-voltage switching to an acquisition in standard CT mode, where X-rays are not pulsed, but
applied continuously. In such a continuous mode, the charge Q applied to the tube during a time t with a tube current I is
Q I t (4)
At a typical minimum tube current of 10 mA [10], and a typical fastest rotation speed of 0.35 s per rotation [10], the
charge per full rotation in continuous mode is 3.5 mAs. For Radiography/Fluoroscopy (R/F) systems, X-ray generators
with significantly lower minimum tube current are used, down to 0.2 mA [24]. If such generators were used in CT
systems, the minimum charge per full rotation would be even lower than 3.5 mAs.
We now want to use compressed sensing to lower detector noise while maintaining patient dose, in a scheme as shown in
Fig. 1. The baseline minimum charge per rotation without pulsing is 3.5 mAs. This means that in pulsed mode with a
minimum pulse charge of 0.1mAs, we can have a maximum of 35 pulses (solid blue line in Fig. 8). This may result in
severe under-sampling artifacts in the reconstruction, for which with a continuous exposure about 1000 views are
available.
It would therefore be desirable to lower the minimum charge per pulse by an order of magnitude, so that we can have up
to a few hundred pulses per rotation, while reducing or at least maintaining the overall charge of 3.5 mAs per rotation.
While the minimum pulse charge of 0.1 mAs may be too high for efficient dose reduction with compressed sensing with
today’s scanners, the addition of strong spectral filtering could significantly lower the patient dose at same minimum
pulse charge. An additional benefit of strong spectral filtering would be that the lower-energy X-rays during high-voltage
switching transitions would be filtered out even more efficiently, thereby increasing the dose-efficiency of high-voltage
switched pulses. The new dose limit with an assumed dose reduction by a factor of 10 through spectral filtering is shown
as blue dashed line in Fig. 8.
Existing CT systems already have a number of different spectral filters, and adding or replacing one of them with a
stronger filter is technically feasible. This relatively small hardware modification would make high-voltage switching a
good option for pulsing at low additional cost.
Proc. of SPIE Vol. 9033 90332Z-9
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
6.4 Maximum number of pulses with respect to charge and discharge time
In case of strong additional spectral filtering, the pulse charge may not any longer be the limiting factor, but we still need
to pay attention to the pulse charge and discharge times. Table 3 shows the upper bound of the number of pulses during a
0.5 s, 1 s and 2 s rotation, for typical values of high-voltage capacitance C=1nF and tube voltage V=100kV. In the
extreme case calculated here, the pulses would follow each other without any X-ray-Off time. For pulsing to be an
effective dose-reduction scheme, the actual number of pulses per rotation needs to be significantly lower than the
maximum numbers shown in Table 3 – last three columns on the right hand side.
Table 3. Maximum number of pulses with respect to discharge time, in the extreme case where the pulses follow each other
without any X-ray-Off time. Assuming high-voltage capacitance C=1nF and tube voltage V=100kV.
Pulse Charge Tube Discharge Max. Number of Max. Number of Max. Number of
(1 nF, 100 kV) Current Time Pulses During 0.5 s Pulses During 1 s Pulses During 2 s
0.1 mAs 1000 mA 0.1 ms 5000 10000 20000
0.1 mAs 500 mA 0.2 ms 2500 5000 10000
0.1 mAs 200 mA 0.5 ms 1000 2000 4000
0.1 mAs 100 mA 1 ms 500 1000 2000
0.1 mAs 10 mA 10 ms 50 100 200
Only the first row in Table 3 satisfies our initial goal of a discharge duration of 100 µs, which had been set to make sure
that transition on/off times are short with respect to pulse durations for a one second gantry rotation speed. The high tube
current of 1000 mA associated with this short transition time shows us once more that strong spectral filtering will
generally be a prerequisite for making high-voltage switching a viable option for dose reduction.
Taking into account the additional time required for the tube voltage rise duration of approximately 0.2 ms (Fig. 7), a
reasonable trade-off may be found at an intermediate tube current of about a hundred mA (Fig. 8).
7. X-RAY TUBE PULSING THROUGH EXTRACTION GRID MODULATION
One example of an electron gun for CT applications with outstanding pulsing capabilities was demonstrated at GE
Global Research for Inverse Geometry CT [19] – multi-source electron gun with an extraction grid. While typical
electron guns in clinical CT systems tend to have temperature limited electron emission with the tube current controlled
by the filament current, as depicted in Fig. 2, this novel electron gun – see Figures 8 and 9 – has been designed for the
space charge limited regime. In the space charge regime, the tube current is solely controlled by the voltage locally
applied on the cathode using an extraction electrode/extraction grid, completely decoupled from the filament current and
the target acceleration voltage. This means that the electron beam reaching the target – and consequently the X-ray
emission – can be modulated very fast by changing the extraction voltage of a mesh grid located at few hundreds of
microns from the electron emitting surface (a dispenser cathode in this case). The emitter/cathode temperature remains
constant. For the multi-source gun presented here, the focusing voltages and the target voltage are kept constant during
operation; the extraction voltage is used to pulse the electron beam and therefore the X-ray output of the source.
Experimental data in Fig. 11 shows current pulses on the order of 3 µs width and about 950 mA amplitude. Rise time for
the extractor voltage is on the order of 200 ns; data in Fig. 11 open the possibility of pulse widths of even 1 µs, using the
multi-source space charge limited electron gun. This type of electron gun enables a very elegant and ultra-flexible way of
accomplishing tube pulsing. In the end, it is much faster to turn on/off the extraction voltage of few hundreds of volts, as
opposed to pulsing the X-ray tube by turning on/off the high voltage between the emitter and the target, on the order of
100 kV.
Proc. of SPIE Vol. 9033 90332Z-10
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
Extraction grid
Extraction grid Target
Target
Focusing plate Target
Focusing plate
FE
E
Emitter
ECE
Figure 9: Electron gun structure designed at GE Global Research for Inverse Geometry CT [19]. Emitter = emitter/cathode,
Extraction grid = mesh grid, ECE = emittance compensating electrode (focusing electrode 1), Focusing plate = focusing
electrode 2. Simulation of the electron beam optics/focusing is illustrated here.
Focusing plate
ECE Extraction Emitter
grid
Figure 10: Electron gun built at GE Global Research for Inverse Geometry CT – the structure of the gun is similar with
Fig. 8. Emitter here is a dispenser cathode. Each electron gun has four different emitters (see the left hand side image). Each
individual beam line has the extraction and focusing scheme illustrated in Fig. 8.
Proc. of SPIE Vol. 9033 90332Z-11
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
1kV
ECE voltage for focusing
DCE emitted Grid voltage outside the
current pulse: Grid voltage pulse pulse : -557 V to turn off
953 mA (3us) : +266 V DCE emission
500V
200mA
ti
1µs
Figure 11: Example of tube pulsing using one cathode of the multi-source space charge limited electron gun demonstrated
for Inverse Geometry CT at GE Global Research. Green line is the ECE voltage (constant 6 kV, used for focusing). Blue
line is the pulsed extraction grid voltage: +266 V for extraction during a 3 µs pulse width, and -557 V outside the pulse to
suppress the DCE emission. Magenta trace is the current emitted by the dispenser cathode emitter (DCE): 953 mA during
the pulse.9
8. CONCLUSIONS
Clinically available CT systems deliver a minimum charge per pulse on the order of 0.1 mAs, which may be too high to
be useful in low-dose pulsing schemes when high-voltage switching is used. In vascular systems, much smaller pulses of
0.002 mAs are currently available, with added grid and corresponding power supply hardware. While this additional
gridding hardware could technically be implemented in a CT scanner, it is not included in clinically available CT scanner
models, as up to now there has been no clinical demand for such small pulses.
Alternative options for low-dose CT acquisitions with little or no hardware modifications of clinically available CT
systems include the addition of strong spectral filtering in order to lower patient dose at the minimum pulse charge
available, and continuous non-pulsed acquisitions at significantly reduced tube current.
In the absence of novel CT tube architectures that include gridding or space charge electron guns with extraction grids, a
high-voltage switching approach may be employed, with a combination of gantry speed optimization, spectral filtration
and faster pulsing at medium tube current. For example, a protocol with 1 s gantry rotation, 1 kHz sampling rate,
200 mA (discharge time of 0.5 ms), 100 active views and 900 inactive views may be used (Table 3). This paper focused
on the feasibility of tube pulsing technologies, and not the determination of the appropriate or optimal imaging protocol.
Such an analysis is the subject of future research.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by Grant Number 1R01CA160253 from the National Cancer
Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of
the National Cancer Institute or the National Institutes of Health.
Proc. of SPIE Vol. 9033 90332Z-12
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
REFERENCES.
[1] Weber, W. A., “Assessing tumor response to therapy,” Journal of Nuclear Medicine 50, Suppl 1, 1S-10S (2009).
[2] Weber, W. A., “Positron emission tomography as an imaging biomarker,” Journal of Clinical Oncology 24, 3282-92
(2006).
[3] Kinahan, P. E., Townsend, D. W., Beyer, T. and Sashin, D., “Attenuation correction for a combined 3D PET/CT
scanner,” Medical Physics 25, 2046-53 (1998).
[4] Xia, T., Alessio, A. M., De Man, B., Manjeshwar, R., Asma, E., Kinahan, P. E., “Ultra-Low Dose CT Attenuation
Correction for PET/CT,” Physics in Medicine and Biology 57, 309-328 (2012).
[5] Colsher, J. G., Jiang, H., Thibault, J.-B., Lonn, A., Pan, T., Lokitz, S. J. and Turkington, T. G., “Ultra low dose CT
for attenuation correction in PET/CT,” Nuclear Science Symposium Conference Record, NSS '08, IEEE, 5506-5011
(2008). http://ieeexplore.ieee.org/stamp/stamp.jsp?arnumber=04774499
[6] Xia, T., Alessio, A. and Kinahan, P. E., “Spectral shaping for ultra-low dose CT attenuation correction in PET/CT,”
The First International Meeting on Image Formation in X-Ray Computed Tomography, Salt Lake City, Utah, 105-
108 (2010).
[7] Ulzheimer, S.. et al., “Multislice CT: Current Technology and Future Developments”, Springer, ISBN 978-3-540-
33124-7 (2009). http://www.springer.com/978-3-540-33124-7
[8] American Association of Physicists in Medicine, “Functionality and Operation of Fluoroscopic Automatic
Brightness Control/Automatic Dose Rate Control Logic in Modern Cardiovascular and Interventional Angiography
Systems”, AAPM Report No. 125 (2012). http://149.28.118.16/pubs/reports/RPT_125.pdf
[9] Belanger, B., Boudry, J., “Management of pediatric radiation dose using GE fluoroscopic equipment,” Pediatric
Radiology 36, Suppl 2, 204–211 (2006).
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2663641/pdf/247_2006_Article_228.pdf
[10] NHS Purchasing and Supply Agency, “Comparative specifications, 64 slice CT scanners”, CEP08027 (2009).
http://nhscep.useconnect.co.uk/ShowDocument.ashx?id=146&i=true
[11] Jørgensen J. S., Sidky, E. Y., Pan, X, “Quantifying admissible undersampling for sparsity-exploiting iterative image
reconstruction in X-ray CT,” IEEE Transactions on Medical Imaging 32(2), 460-73 (2013).
[12] Chandra, N., “CT Sampling Technology. Discovery CT750HD,” A GE Healthcare CT publication, Spring 2009,
http://www.gehealthcare.com/usen/ct/products/docs/ct_sampling_technology09.pdf (2009).
[13] GE Healthcare Website, “Discovery CT750 HD FREEdom Edition,”
http://www3.gehealthcare.com/en/Products/Categories/Computed_Tomography/Discovery_CT750_HD#tabs/tab95
D7BCF2EB2F481F9748C1B0B247AC92 (16 December 2013).
[14] Pemler, P. et al., “Influence of respiration-induced organ motion on dose distributions in treatments using enhanced
dynamic wedges,” Med. Phys. 28, 2234 (2001). http://dx.doi.org/10.1118/1.1410121
[15] General Electric Company, “AutomA / SmartmA Theory, TiP Training in Partnership,” "08-10495 01-08",
http://www3.gehealthcare.co.uk/en-GB/Education/Offering_by_Product/~/media/Downloads/us/Education/Product-
Education-Clinical/TiP-App-Library/GEHealthcare-Education-TiP-App-Library_CT-AutomA-SmartmA-Theory.pdf
(16 December 2013).
[16] Beland, R., “Discharge module for X-ray cable,” Patent, US 5056125 A (1991).
[17] Lu, Z., Nickoloff, E., Ruzal-Shapiro, C., So, J. and Dutta, A., “New automated fluoroscopic systems for pediatric
applications,” Journal of Applied Clinical Medical Physics 6(4), 88–105 (2005).
[18] GE Healthcare, “InnovaTM 2100-IQ, 3100-IQ, 4100-IQ Cardiovascular Imaging System Operator Manual,”
Direction 5391979-5-399 (EN), Revision 1 (2011).
[19] Uribe, J. et al., “Multisource inverse-geometry CT — Prototype system integration,” Nuclear Science Symposium
Conference Record (NSS/MIC), 2578 – 2581 (2010).
[20] McClelland, I., “X-ray equipment maintenance and repairs workbook for radiographers & radiological
technologists,” Appendix E: X-ray equipment operation, “Fig. E-21b”, World Health Organization (2004).
http://libdoc.who.int/publications/2004/9241591633_part5.pdf
[21] Maher, K.., “Basic Physics of Digital Radiography/The Source,” Fig. 2.16, Wikibook,
http://en.wikibooks.org/wiki/Basic_Physics_of_Digital_Radiography/The_Source#Automatic_Exposure_Control
(16 December 2013).
[22] Kinahan, P., “Enabling Ultra Low Dose PET/CT Imaging,” Grant application for FOA PAR-10-169 "Academic-
Industrial Partnerships for Translation of in vivo Imaging Systems for Cancer Investigations (R01)", University of
Washington (2010).
Proc. of SPIE Vol. 9033 90332Z-13
Downloaded From: http://spiedigitallibrary.org/ on 07/18/2015 Terms of Use: http://spiedl.org/terms
[23] Claymount, “N3-type 160 kVDC rated High Voltage Cable,” http://www.claymount.com/l/library/download/998.
Claymount, “J3-type 160 kVDC rated High Voltage Cable,” http://www.claymount.com/l/library/download/1150
(16 December 2013).
[24] NHS Purchasing and Supply Agency, “Radiography/Fluoroscopy (R/F) imaging systems,” Buyers’ guide,
CEP08032 (2008). http://nhscep.useconnect.co.uk
[25] Kinahan, P. E., Hasegawa, B. H. and Beyer, T. “X-ray-based attenuation correction for positron emission
tomography/computed tomography scanners,” Seminars in Nuclear Medicine 33, 166-79 (2003).
[26] Beyer, T., Townsend, D. W., Brun, T., Kinahan, P. E., Charron, M., Roddy, R., Jerin, J., Young, J., Byars, L. and
Nutt, R. “A combined PET/CT scanner for clinical oncology,” Journal of Nuclear Medicine 41, 1369-79 (2000).
Proc. of SPIE Vol. 9033 90332Z-14
DownloadedViewFrom:
publicationhttp://spiedigitallibrary.org/
stats on 07/18/2015 Terms of Use: http://spiedl.org/terms
You might also like
- DepEd CI GuidebookDocument244 pagesDepEd CI Guidebookasdfg100% (4)
- Practice Exercise For Final Assessment 2221Document3 pagesPractice Exercise For Final Assessment 2221Guneet Singh ChawlaNo ratings yet
- Unit 3 Digital Documentation: Multiple Choice QuestionsDocument7 pagesUnit 3 Digital Documentation: Multiple Choice Questions07tp27652% (21)
- Supply Chain Management 5th Edition Chopra Solutions ManualDocument3 pagesSupply Chain Management 5th Edition Chopra Solutions Manualdammar.jealousgvg6100% (18)
- Guideline MD Listing and Authorization MDS-G5 PDFDocument153 pagesGuideline MD Listing and Authorization MDS-G5 PDFSyed SalmanNo ratings yet
- DLL in Science 5 Q1 W1Document3 pagesDLL in Science 5 Q1 W1Rhinalyn Andaya Barberan100% (2)
- X-Ray Pulsing Methods For Reduced-Dose Computed Tomography in PET/CT Attenuation CorrectionDocument15 pagesX-Ray Pulsing Methods For Reduced-Dose Computed Tomography in PET/CT Attenuation CorrectionsunlianzhuNo ratings yet
- Chapter 1: Introduction: 1.1 Background and MotivationDocument5 pagesChapter 1: Introduction: 1.1 Background and Motivationnirav34No ratings yet
- Radiol 2018172656Document20 pagesRadiol 2018172656rnjNo ratings yet
- Physics and Imaging in Radiation OncologyDocument6 pagesPhysics and Imaging in Radiation Oncologydarr artNo ratings yet
- CT Sim ParametersDocument11 pagesCT Sim ParametersEskadmas BelayNo ratings yet
- Photon Counting Spectral CT Versus Conventional CT: Comparative Evaluation For Breast Imaging ApplicationDocument27 pagesPhoton Counting Spectral CT Versus Conventional CT: Comparative Evaluation For Breast Imaging Applicationcarlos56dbNo ratings yet
- Strategies For Radiation Dose OptimizationDocument10 pagesStrategies For Radiation Dose OptimizationthutaNo ratings yet
- Computed TomographyDocument4 pagesComputed TomographyemilyNo ratings yet
- Characterization of A Novel Photon Counting DetectDocument10 pagesCharacterization of A Novel Photon Counting DetectMax dos santos ramosNo ratings yet
- Development and Validation of A Low Dose Simulation Algorithm For Computed TomographyDocument9 pagesDevelopment and Validation of A Low Dose Simulation Algorithm For Computed TomographyBrankica MitrovicNo ratings yet
- Treatment Planning in Proton TherapyDocument20 pagesTreatment Planning in Proton Therapyokolinta godwin100% (1)
- Medical Physics - 2018 - Ommen - Image Quality of Conventional Images of Dual Layer SPECTRAL CT A Phantom StudyDocument13 pagesMedical Physics - 2018 - Ommen - Image Quality of Conventional Images of Dual Layer SPECTRAL CT A Phantom StudyAmril MukminNo ratings yet
- MScThesis KareliotisDocument116 pagesMScThesis KareliotisAndrés ValdezNo ratings yet
- Geometrik Kedokteran2Document5 pagesGeometrik Kedokteran2tasyaNo ratings yet
- Sarti 2012Document12 pagesSarti 2012mariaNo ratings yet
- Wavelet Based Noise Reduction in CT-Images Using Correlation AnalysisDocument20 pagesWavelet Based Noise Reduction in CT-Images Using Correlation Analysisprashant jadhavNo ratings yet
- SPECT/CT Radiation DosimetryDocument13 pagesSPECT/CT Radiation DosimetryMohamed Abd ElazizNo ratings yet
- Improving Radiotherapy Planning in Patients With MDocument14 pagesImproving Radiotherapy Planning in Patients With MTaro TenriNo ratings yet
- Medical ImagingDocument9 pagesMedical ImagingRajes WariNo ratings yet
- CT Angiography: Current Technology and Clinical Use: Go ToDocument46 pagesCT Angiography: Current Technology and Clinical Use: Go ToEuis NurvikaNo ratings yet
- Dose Reduction With Iterative Reconstruction For Coronary CT Angiography: A Systematic Review and Meta-AnalysisDocument9 pagesDose Reduction With Iterative Reconstruction For Coronary CT Angiography: A Systematic Review and Meta-AnalysisHenry MruizNo ratings yet
- Medical Imaging Systems Example QuestionsDocument2 pagesMedical Imaging Systems Example QuestionsPika17No ratings yet
- Kim 2010Document13 pagesKim 2010face bookNo ratings yet
- Radiation Dose Modulation Techniques MDCTDocument10 pagesRadiation Dose Modulation Techniques MDCTFelipe Gustavo Tercero Vega AbantoNo ratings yet
- Gislason-Lee Et Al 2014 ADRC ECR EposterDocument12 pagesGislason-Lee Et Al 2014 ADRC ECR EposterAnders ErikssonNo ratings yet
- Principles of CT and CT Technology : P CT CTT - Goldman 115Document14 pagesPrinciples of CT and CT Technology : P CT CTT - Goldman 115Madalina ConstantinNo ratings yet
- Analysis of CT and MRI Image Fusion Using Wavelet TransformDocument5 pagesAnalysis of CT and MRI Image Fusion Using Wavelet Transform18onaldo20orresNo ratings yet
- Impact of Focal Spot Size On Radiologic Image Quality - A Visual Grading AnalysisDocument10 pagesImpact of Focal Spot Size On Radiologic Image Quality - A Visual Grading AnalysisNurulazirah SalihNo ratings yet
- BulganDocument10 pagesBulganIkh nahia Ikh Nakhia PharmNo ratings yet
- Utilization Patterns of Multidetector Computed Tomography in Elective and Emergency Conditions: Indications, Exposure Risk, and Diagnostic GainDocument4 pagesUtilization Patterns of Multidetector Computed Tomography in Elective and Emergency Conditions: Indications, Exposure Risk, and Diagnostic GainJorge RodriguezNo ratings yet
- Medical Physics - 2021 - Lee - Medical X Band Linear Accelerator For High Precision RadiotherapyDocument16 pagesMedical Physics - 2021 - Lee - Medical X Band Linear Accelerator For High Precision RadiotherapyNima SalianiNo ratings yet
- T/CT Physical Principles and Attenuation Correction Prepared By: Hala Rabee/ID: s1811023 Supervisor: Dr-Mohammed Al-HjoujDocument25 pagesT/CT Physical Principles and Attenuation Correction Prepared By: Hala Rabee/ID: s1811023 Supervisor: Dr-Mohammed Al-HjoujHala YousefNo ratings yet
- Optical Coherence TomographyDocument2,567 pagesOptical Coherence Tomographyप्रताप जय हिन्द100% (1)
- CancerDocument9 pagesCancerMARIA JOSE RIVERA AVILANo ratings yet
- SPECT Imaging TechniqueDocument15 pagesSPECT Imaging TechniqueChris HartoyoNo ratings yet
- Implications of CBCT in Pediatric Dentistry-A ReviewDocument8 pagesImplications of CBCT in Pediatric Dentistry-A ReviewIJAR JOURNALNo ratings yet
- Al-Sharify 2020 IOP Conf. Ser. Mater. Sci. Eng. 870 0120431Document11 pagesAl-Sharify 2020 IOP Conf. Ser. Mater. Sci. Eng. 870 0120431Hua Hidari YangNo ratings yet
- CT Physics for Quality and Dose OptimizationDocument75 pagesCT Physics for Quality and Dose OptimizationdanaNo ratings yet
- J. Nucl. Med. Technol. 2007 Goldman 115 28Document15 pagesJ. Nucl. Med. Technol. 2007 Goldman 115 28Ruxandra LúthienNo ratings yet
- The CT Handbook Optimizing Protocols For Today's Feature Rich Scanners Chapter 1Document35 pagesThe CT Handbook Optimizing Protocols For Today's Feature Rich Scanners Chapter 1Abdullah AliNo ratings yet
- Quantitative Cone-Beam CT Imaging in Radiotherapy Parallel Computation and Comprehensive Evaluation On The TrueBeam SystemDocument8 pagesQuantitative Cone-Beam CT Imaging in Radiotherapy Parallel Computation and Comprehensive Evaluation On The TrueBeam SystemKe LuNo ratings yet
- CT Radiation ProtectionDocument8 pagesCT Radiation ProtectionKhush JainNo ratings yet
- Principles of CT and CT TechnologyDocument15 pagesPrinciples of CT and CT TechnologyLida Velasquez SierraNo ratings yet
- Qims 12 01 766Document15 pagesQims 12 01 766Hamza ArjahNo ratings yet
- Computed TomographyDocument31 pagesComputed TomographyAvik Mukherjee100% (3)
- Contrast MediaDocument11 pagesContrast MediaDEVI ANDRIANINo ratings yet
- IW Yu Leng Image Reconstruction TechniquesDocument6 pagesIW Yu Leng Image Reconstruction TechniquesNurul Hazi putriNo ratings yet
- A Fast Iterative Reconstruction Algorithm For Sparse Angle CT Based On Compressed SensingDocument6 pagesA Fast Iterative Reconstruction Algorithm For Sparse Angle CT Based On Compressed Sensingfrima kurniawanNo ratings yet
- TM 10. CT CARDIAC Artikel 2 PCD-CTDocument13 pagesTM 10. CT CARDIAC Artikel 2 PCD-CTrellvandraaaNo ratings yet
- A Dose-Neutral Image Quality Comparison of Different CBCT and CT Systems Using Paranasal Sinus Imaging Protocols and PhantomsDocument8 pagesA Dose-Neutral Image Quality Comparison of Different CBCT and CT Systems Using Paranasal Sinus Imaging Protocols and Phantomsmarito’No ratings yet
- Nano Platform For Positron Emission TomographyDocument4 pagesNano Platform For Positron Emission Tomographygopikrrishna.jNo ratings yet
- Resume C-ArmDocument4 pagesResume C-Armp27838121011No ratings yet
- Matsumoto 2016Document7 pagesMatsumoto 2016A DNo ratings yet
- Dual Energy CTDocument11 pagesDual Energy CTdeadcorpsesNo ratings yet
- 2017 - Dictionary Learning Based Low Dose Helical CT Reconstruction With Longitudinal TV ConstraintDocument1 page2017 - Dictionary Learning Based Low Dose Helical CT Reconstruction With Longitudinal TV ConstraintL AndyNo ratings yet
- JXST 26 1 2018Document29 pagesJXST 26 1 2018nasywa rahmatullailyNo ratings yet
- 3D Dose Computation AlgorithmsDocument10 pages3D Dose Computation AlgorithmsHashir SaeedNo ratings yet
- Ciocca Et Al. - 2019 - Design and Commissioning of The Nondedicated Scanning Proton Beamline For Ocular Treatment at The SynchrotronDocument12 pagesCiocca Et Al. - 2019 - Design and Commissioning of The Nondedicated Scanning Proton Beamline For Ocular Treatment at The SynchrotronKanit TanthanawigraiNo ratings yet
- Iray Technoloty Detector (NDT0505J) - 20190422Document12 pagesIray Technoloty Detector (NDT0505J) - 20190422Hernan PerezNo ratings yet
- Drtech EVS 2430W / EVS 2430GW: Safety and Regulatory Information With User 'S ManualDocument102 pagesDrtech EVS 2430W / EVS 2430GW: Safety and Regulatory Information With User 'S ManualHernan PerezNo ratings yet
- Dpx-Iq: Operator's ManualDocument166 pagesDpx-Iq: Operator's ManualZak zsNo ratings yet
- Quality Control Manual MAMMOMAT Inspiration VA10. MAMMOMAT InspirationDocument56 pagesQuality Control Manual MAMMOMAT Inspiration VA10. MAMMOMAT InspirationHernan PerezNo ratings yet
- Somatom: Hiq/ Plus/ ArDocument18 pagesSomatom: Hiq/ Plus/ ArHernan PerezNo ratings yet
- AN1131 Application Note: MIGRATING APPLICATIONS FROM ST72511/311/314/124 TO ST72521/321/324Document17 pagesAN1131 Application Note: MIGRATING APPLICATIONS FROM ST72511/311/314/124 TO ST72521/321/324Hernan PerezNo ratings yet
- Upgrade Ar - HP To HP Spiral 0.4 SegDocument42 pagesUpgrade Ar - HP To HP Spiral 0.4 SegHernan PerezNo ratings yet
- Operator GuideDocument36 pagesOperator GuideHernan PerezNo ratings yet
- AN1131 Application Note: MIGRATING APPLICATIONS FROM ST72511/311/314/124 TO ST72521/321/324Document17 pagesAN1131 Application Note: MIGRATING APPLICATIONS FROM ST72511/311/314/124 TO ST72521/321/324Hernan PerezNo ratings yet
- ChelarDocument35 pagesChelarkhawar mukhtarNo ratings yet
- Iq-Ris 3.1.0 User Manual Int en - 004rDocument75 pagesIq-Ris 3.1.0 User Manual Int en - 004rHernan PerezNo ratings yet
- Operator's ManualDocument226 pagesOperator's ManualHernan PerezNo ratings yet
- AR Ageing FinalDocument13 pagesAR Ageing FinalHAbbunoNo ratings yet
- GCSE Combined Science PDFDocument198 pagesGCSE Combined Science PDFMpumelelo Langalethu MoyoNo ratings yet
- AN2061 Application Note: EEPROM Emulation With ST10F2xxDocument15 pagesAN2061 Application Note: EEPROM Emulation With ST10F2xxleuchimed mouhNo ratings yet
- KireraDocument3 pagesKireramurithiian6588No ratings yet
- Pragmatics: The Study of Its Historical Overview, Meanings, Scope and The Context in Language UseDocument7 pagesPragmatics: The Study of Its Historical Overview, Meanings, Scope and The Context in Language UseIHINOSEN IYOHANo ratings yet
- Galvanic CorrosionDocument5 pagesGalvanic Corrosionsatheez3251No ratings yet
- Module 1 Power PlantDocument158 pagesModule 1 Power PlantEzhilarasi NagarjanNo ratings yet
- Simha Lagna: First House Ruled by The Planet Sun (LEO) : The 1st House Known As The Ascendant orDocument3 pagesSimha Lagna: First House Ruled by The Planet Sun (LEO) : The 1st House Known As The Ascendant orRahulshah1984No ratings yet
- University of Delhi Third Admission List - Bachelor of Education (B.Ed.)-2021Document8 pagesUniversity of Delhi Third Admission List - Bachelor of Education (B.Ed.)-2021FERA Future electronics and research administrationNo ratings yet
- Physice 2013 Unsolved Paper Outside Delhi PDFDocument7 pagesPhysice 2013 Unsolved Paper Outside Delhi PDFAbhilashaNo ratings yet
- PROPOSED ARFF BUILDINGDocument27 pagesPROPOSED ARFF BUILDINGDale Bryan S DalmacioNo ratings yet
- Speed, Velocity and FrictionDocument10 pagesSpeed, Velocity and FrictionCristie Ann GuiamNo ratings yet
- Is BN 9789526041957Document72 pagesIs BN 9789526041957supriya rakshitNo ratings yet
- PR1 Module 2Document12 pagesPR1 Module 2Ervin GonzalesNo ratings yet
- Dcs Ict2113 (Apr22) - LabDocument6 pagesDcs Ict2113 (Apr22) - LabMarwa NajemNo ratings yet
- Pressure Variation in Tunnels Sealed Trains PDFDocument258 pagesPressure Variation in Tunnels Sealed Trains PDFsivasankarNo ratings yet
- Module 5 Greek ArchDocument22 pagesModule 5 Greek ArchKyla A. EstoestaNo ratings yet
- BG BG 202102080912862 User Manual - File (Long) BG BG-8Document1 pageBG BG 202102080912862 User Manual - File (Long) BG BG-8hofolo39No ratings yet
- Jallikattu: Are Caste and Gender the Real Bulls to TameDocument67 pagesJallikattu: Are Caste and Gender the Real Bulls to TameMALLIKA NAGLENo ratings yet
- Short Time Fourier TransformDocument37 pagesShort Time Fourier TransformGopikaPrasadNo ratings yet
- Facts About SaturnDocument7 pagesFacts About SaturnGwyn CervantesNo ratings yet
- Questions Related To Open Channel Flow.Document3 pagesQuestions Related To Open Channel Flow.Mohd AmirNo ratings yet
- Ch1 - A Perspective On TestingDocument41 pagesCh1 - A Perspective On TestingcnshariffNo ratings yet
- 10.6 Heat Conduction Through Composite WallsDocument35 pages10.6 Heat Conduction Through Composite WallsEngr Muhammad AqibNo ratings yet