Professional Documents
Culture Documents
Renal Dose Adjustment Guidelines For Antimicrobial
Uploaded by
JAMUNAOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Renal Dose Adjustment Guidelines For Antimicrobial
Uploaded by
JAMUNACopyright:
Available Formats
Renal Dose Adjustment Guidelines for Antimicrobials
CRRT Dosing Recommendations
CRRT Background:
• When a patient is initiated on CRRT, antimicrobial therapy often requires adjustment to
ensure adequate drug concentrations are achieved.
• CVVHD removes solutes (including drugs) via diffusion. An electrolyte solution (dialysate)
runs countercurrent to the patient’s blood flow which creates a concentration gradient,
driving the removal of solutes.
o Drug removal is impacted by protein binding (e.g. highly protein bound drugs will be
minimally removed) and rate of dialysate flow (increased removal with higher flow
rates).
o Drugs that are renally cleared or removed by hemodialysis are likely to be impacted
by CVVHD.
• CVVH removes solutes (including drugs) via convection. Convection is a transport
mechanism that is accomplished by using a high-permeability membrane to generate a
large ultrafiltrate volume. Along with the ultrafiltrate, plasma water and certain solutes are
forced across the membrane.
Important Considerations:
• In patients with renal failure, the time to achievement of steady-state is increased for renally-
eliminated agents. Additionally, patients on CRRT frequently have an increased volume of
distribution. Therefore, a loading dose should be utilized if not initiating therapy at the
full dose.
• Patients undergoing CRRT may be predisposed to changes in pharmaceutical agents’
volume of distributions (Vd). When agents with relatively large therapeutic windows (e.g.
beta-lactams) and low levels of toxicity are utilized in critically ill patients, it may be prudent
to err on the side of more aggressive dosing to account for any increases in (Vd).
• While on CRRT, patients’ residual renal function may continue to change. Improvements or
reductions in residual renal function may warrant a change in dosing strategy. Residual
renal function should be evaluated on a daily basis when making CRRT dosing plans.
• Monitor patients for interruption of CRRT (e.g. clotting) or changing filtration rates. When
CRRT is off, dose as hemodialysis patients or based on any residual renal function.
• The recommendations below should be used as a guide to aid in antibiotic dosing while
on CRRT. Dosing regimens should be tailored based on presumed source of infection, MIC
data (when available), and residual renal function. When a dosing range is indicated in the
tables below (e.g., ampicillin/sulbactam 1.5-3 g q6-8h), a more aggressive dose should be
selected for severe infections.
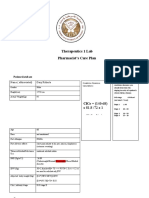
• Pharmacists should document final dosing recommendations and any necessary rationale
using the preformatted note available in One Chart.
The following anti-infectives do NOT require dose adjustment during CRRT:
• Amphotericin • Metronidazole
• Azithromycin • Micafungin
• Ceftriaxone • Oxacillin
• Clindamycin • Rifampin
• Doxycycline • Tigecycline
• Linezolid • Voriconazole
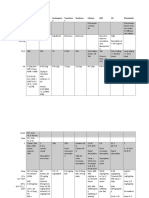
Table 1. CVVHD Dosing Recommendations
Loading Dose Dose by CVVHD Dialysate Flow Rate
Drug Standard Anephric Dose Ref.
for CRRT 1 L/h 2 L/h 3-4 L/h
Aminoglycosides
Amikacin 10 mg/kg Provide loading dose then Provide loading dose then dose per TDM;
1, 2
Gentamicin 3 mg/kg dose per TDM patients may require repeat dosing q24h at flow rates >1 L/h
Tobramycin 3 mg/kg
Acyclovira NA 2.5-5 mg/kg q24h 5-7.5 mg/kg q24h 5-10 mg/kg q24h 5-10 mg/kg q12hb 1, 2
Ampicillin/sulbactam 3g 1.5-3 g q24h 1.5-3g q8h 1.5-3g q6-8hb 1.5-3g q6hb 1, 2
Aztreonam 2g 1-2 g q24h 1 g q8h or 2 g q12h 1g q8h or 2 g q12h 2 g q8hb 1
Cefazolin 2g 1-2 g q24h 1 g q8h or 2 g q12h 1 g q8h or 2 g q12h 2 g q8hb 1
Cefepime (Standard dose) 2g 1 g q24h 1 g q8h 1 g q6h 2 g q8hb
1, 2, 3,
Cefepime (High dose for 4, 18
2g 1 g q24h 2g q12h 2g q8h
neutropenic fever)
Ceftazidime 2g 1 g q24h 1 g q8h or 2 g q12h 1 g q8h or 2 g q12h 2 g q8hb 1, 2
Ceftolozane/tazobactamc 1.5 g 150 mg q8h 375 mg q8h 750 mg q8h 1.5g q8h 16
1, 2,
Colistin NA 50 mg q12h 2.5 mg/kg q24h 2.5 mg/kg q24h 2-3 mg/kg q12h 13, 22,
23
1, 2, 5,
Daptomycin NA 6 mg/kg q48h 4-6 mg/kg q24hr 6 mg/kg q24hr 6-8 mg/kg q24h 6, 19
Ertapenem 1g 500mg IV q24h 1g IV q24h 13
800 mg 400 mg (6 mg/kg) after HD 400 mg q24h
Fluconazoled 800 mg q24h 800 mg q24h 1, 2, 7
(12 mg/kg) three times weekly 800 mg q24h
1.25 mg/kg after HD three 5 mg/kg q24h or
Ganciclovir 5 mg/kg 2.5 mg/kg q24h 5 mg/kg q12h 1, 12
times weekly 2.5 mg/kg q12h
1, 2,
Levofloxacin 500 mg 250-500 mg q48h 250-750 mg q24h 17
Meropenem (Standard dose) 1-2 g 500-1000 mg q24h 500 mg q8h 500 mg q8h 500 mg q6h
Meropenem (High dose for 1, 2, 3,
2g q12h 9
meningitis, cystic fibrosis, or 2g 2g IV q24h 2g q8h
MIC of 4 mcg/mL)
If not undergoing HD – Not
recommended;
Oseltamivir NA 150 mg q12h
If undergoing HD – 30 mg
after every HD cycle
Piperacillin/tazobactamf EI NA 4.5 g EI q12h 4.5 g EI q8h 10, 15
Severe infections/PJP:
Trimethoprim/sulfamethoxazole
10 mg/kg 7.5-10 mg/kg/day (TMP) 10 mg/kg/day (TMP) divided q12h 20, 21
(TMP/SMX)
divided q12-24h
Provide loading dose then
dose accordingly to obtain Provide loading dose then dose patients 10-15 mg/kg q24h and adjust accordingly
Vancomycin 20-25 mg/kg 1, 11
serum concentrations within to obtain serum concentrations within desired range
desired range
Abbreviations: EI, extended infusion (4 hours); HD, hemodialysis; NA, not applicable; PJP, Pneumocystis jiroveci pneumonia; TDM, therapeutic drug monitoring
a
Use lower dose for mucocutaneous HSV and higher dose for HSV encephalitis or VZV
b
Flow rates > 2 L/hr are rarely addressed in literature; decreasing the interval is done empirically to maintain levels above MIC for time-dependent antibiotics, specifically those with limited protein binding
c
Dose adjustments based on data from CVVH since data is lacking for CVVHD
d
Dose assuming invasive candidiasis
e
Decreased interval is based on data from CVVH since data is lacking for CVVHD and some antimicrobials; however, CVVHD solute elimination is in general greater than CVVH
f
Tazobactam can accumulate as it is not removed as readily; caution in decreasing interval beyond every 8 hours (i.e. q6h) in patients with lack of residual renal function
Table 2. CVVH Dosing Recommendations
Loading Dose Dose by CVVH Dialysate Flow Rate
Drug Standard Anephric Dose Ref.
for CRRT 1 L/h 2 L/h 3 L/h 4 L/h
Aminoglycosides
Amikacin 10 mg/kg Provide loading dose then Provide loading dose then dose per TDM;
1
Gentamicin 3 mg/kg dose per TDM patients may require repeat dosing q24h at flow rates >1 L/h
Tobramycin 3 mg/kg
Acyclovira NA 2.5-5 mg/kg q24h 5-7.5 mg/kg q24h 5-10 mg/kg q24h 1
Ampicillin/sulbactam 1.5-3 g 1.5-3 g q24h 1.5-3 g q8-12h 1
Aztreonam 2g 1-2 g q24h 1 g q8h 2g q12h 2 g q8h 2 g q6h 2
Cefazolin 2g 1-2 g q24h 1 g q12h 1 g q12h 1 g q8h 1 g q8h 2
Cefepime (Standard dose) 2g 1 g q24h 1 g q8h 1 g q6h 2g q8h 2g q8h
Cefepime (High dose for 1, 3
2g 1 g q24h 2g q12h 2g q8h
neutropenic fever)
Ceftazidime 2g 1 g q24h 1 g q12h 2g q12h 2 g q8h 2 g q8h 2
Ceftolozane/tazobactamb 1.5 g 150 mg q8h 375 mg q8h 750 mg q8h 1.5g q8h 4
Colistin 50 mg q12h 2.5 mg/kg q48h 1, 8
Daptomycin NA 6 mg/kg q48h No adjustment necessary; dose as anephric 1
800 mg 400 mg (6 mg/kg) after HD
Fluconazolec 200 mg q24h 400 mg q24h 400 mg q12h 400 mg q12h 1, 5
(12 mg/kg) three times weekly
Levofloxacin 500-750 mg 250-500 mg q48h 250 mg q24h 1
Meropenem (Standard dose) 1-2 g 500-1000 mg q24h 500 mg q12h 500 mg q8h 500 mg q6h 500 mg q6h
Meropenem (High dose for
1, 6
meningitis, cystic fibrosis, or 2g 2g q24h 2g q12h 2g q8h
MIC of 4 mcg/mL)
Piperacillin/tazobactam EI NA 4.5 g EI q12h 4.5 g EI q8h 7
Severe infections/PJP:
Trimethoprim/sulfamethoxazole
NA 7.5-10 mg/kg/day (TMP) 2.5-7.5mg/kg (TMP) q12h 1
(TMP/SMX)
divided q12-24h
Provide loading dose then
Provide loading dose then dose patients approximately 500 mg q12h when dialysate
dose accordingly to obtain
Vancomycin 20-25 mg/kg flow rates >1 L/h and adjust accordingly to obtain serum concentrations within 6
serum concentrations within
desired range
desired range
Abbreviations: EI, extended infusion (4 hours); HD, hemodialysis; NA, not applicable; PJP, Pneumocystis jiroveci pneumonia; TDM, therapeutic drug monitoring
a
Use lower dose for mucocutaneous HSV and higher dose for HSV encephalitis or VZV
b
Data limited to dialysate flow rates of 2 L/hr
c
Dose assuming invasive candidiasis
CVVHD References:
1. Heintz BH, Matzke GR, Dager WE. Antimicrobial dosing concepts and recommendations for
critically ill adult patients receiving continuous renal replacement therapy or intermittent
hemodialysis. Pharmacotherapy. 2009;29(5):562-77.
2. Trotman RL, Williamson JC, Shoemaker DM, Salzer WL. Antibiotic dosing in critically ill
adult patients receiving continuous renal replacement therapy. Clin Infect Dis.
2005;41(8):1159-66.
3. Choi G, Gomersall CD, Tian Q, Joynt GM, Freebairn R, Lipman J. Principles of antibacterial
dosing in continuous renal replacement therapy. Crit Care Med. 2009;37(7):2268-82.
4. Wilson FP, Bachhuber MA, Caroff D, Adler R, Fish D, Berns J. Low cefepime concentrations
during high blood and dialysate flow continuous venovenous hemodialysis. Antimicrob
Agents Chemother. 2012 Apr;56(4):2178-80.
5. Vilay AM, Grio M, Depestel DD, Sowinski KM, Gao L, Heung M, et al. Daptomycin
pharmacokinetics in critically ill patients receiving continuous venovenous hemodialysis. Crit
Care Med. 2011;39(1):19-25.
6. Khadzhynov D, Slowinski T, Lieker I, Spies C, Puhlmann B, Konig T, et al. Plasma
pharmacokinetics of daptomycin in critically ill patients with renal failure and undergoing
CVVHD. Int J Clin Pharmacol Ther. 2011;49(11):656-65.
7. Pittrow L, Penk A. Dosage adjustment of fluconazole during continuous renal replacement
therapy (CAVH, CVVH, CAVHD, CVVHD). Mycoses. 1999;42(1-2):17-9.
8. Meyer B, Kornek GV, Nikfardjam M, Karth GD, Heinz G, Locker GJ, Jaeger W, Thalhammer
F. Multiple-dose pharmacokinetics of linezolid during continuous venovenous
haemofiltration. J Antimicrob Chemother. 2005;56(1):172-9.
9. Pea F, Viale P, Pavan F, Furlanut M. Pharmacokinetic considerations for antimicrobial
therapy in patients receiving renal replacement therapy. Clin Pharmacokinet.
2007;46(12):997-1038.
10. Valtonen M, Tiula E, Takkunen O, Backman JT, Neuvonen PJ. Elimination of the
piperacillin/tazobactam combination during continuous venovenous haemofiltration and
haemodiafiltration in patients with acute renal failure. J Antimicrob Chemother.
2001;48(6):881-5.
11. Wilson FP, Berns JS. Vancomycin levels are frequently subtherapeutic during continuous
venovenous hemodialysis (CVVHD). Clin Nephrol. 2012;77(4):329-31.
12. Horvatis T, Kitzberger R, Frolz A, Zauner C, Jager W, Bohmdorder M, et al.
Pharmacokinetics of ganciclovir during continuous venovenous hemodiafiltration in critically
ill patients. Antimicrob Agents Chemother. 2014;58:94-101.
13. Li J, Rayner CR, Nation RL, et al. Pharmacokinetics of colistin methanesulfonate and colistin
in a critically ill patient receiving continuous venovenous hemodiafiltration. Antimicrob
Agents Chemother. 2005;49:4814-4815.
14. Eyler RF, Vilay AM, AN, Heung M, Pleva M, Sowkinski KM, et al. Pharmacokinetics of
ertapenem in critically ill patients receiving continuous venovenous hemodialysis or
hemodiafiltration. Antimicrob Agents Chemother. 2014;58:1320-1326.
15. Awissi d, Beauchamp A, Hebert E, Lavigne V, Munoz DL, Lebrun G, Savoie M, et al.
Pharmacokinetics of an extended 4-hour infusion of piperacillin-tazobactam in critically ill
patients undergoing continuous renal replacement therapy. Pharmacotherapy. 2015;35:600-
607.
16. Oliver WD, Heil EL, Gonzales JP, Mehrotra S, Robinett K, Saleeb P, Nicolau DP.
Ceftolozane-tazobactam pharmacokinetics in a critically Ill patient on continuous
venovenous hemofiltration. Antimicrob Agents Chemother. 2016;60:1899-1901.
17. Hanson E, Bucher M, Jakob W, et al. Pharmacokinetics of levofloxacin during continuous
veno-venous hemofiltration. Intensive Care Med. 2001;27:371-375.
18. Carlier M, Taccone FS, Beumier M, et al. Population pharmacokinetics and dosing
simulations of cefepime in septic shock patients receiving continuous renal replacement
therapy. Int J Antimicrob Agents. 2015;45(4):413-9.
19. Preiswerk B, Rudiger A, Fehr J, et al. Experience with daptomycin daily dosing in ICU
patients undergoing continuous renal replacement therapy. Infection. 2013;41(2):533-7.
20. Curkovic I, Luthi B, Franzen D, et al. Trimethoprim/Sulfamethoxazole pharmacokinetics in
two patients undergoing continuous venovenous hemodiafiltration. Ann Pharmcother.
2010;44(10):1669-1672.
21. Kesner JM, Yardman-Frank JM, Mercier RC, et al. Trimethoprim and sulfamethoxazole
transmembrane clearance during modeled continuous renal replacement therapy. Blood
Purif. 2014;38:195-202.
22. Markou N, Fousteri M, Markantonis SL, et al. Colistin pharmacokinetics in intensive care unit
patients on continuous venovenous haemodiafiltration: an observational study. J Antimicrob
Chemother. 2012; 67:2459-2462.
23. Honore PM, Jacobs R, Joannes-Boyaud O, et al. Continuous renal replacement therapy-
related strategies to avoid colistin toxicity: a clinically oriented review. Blood Purif.
2014;37:291-295.
CVVH References:
1. Heintz BH, Matzke GR, Dager WE. Antimicrobial dosing concepts and recommendations for
critically ill adult patients receiving continuous renal replacement therapy or intermittent
hemodialysis. Pharmacotherapy. 2009;29(5):562-77.
2. Scheetz MH, Scarsi KK, Ghossein C, Hurt KM, Zembower TR, Postelnick MJ. Adjustment of
antimicrobial dosages for continuous venovenous hemofiltration based on patient-specific
information. Clin Infect Dis. 2006;42(3):436-7.
3. Carlier M, Taccone FS, Beumier M, et al. Population pharmacokinetics and dosing
simulations of cefepime in septic shock patients receiving continuous renal replacement
therapy. Int J Antimicrob Agents. 2015;45(4):413-9.
4. Oliver WD, Heil EL, Gonzales JP, Mehrotra S, Robinett K, Saleeb P, Nicolau DP.
Ceftolozane-tazobactam pharmacokinetics in a critically Ill patient on continuous
venovenous hemofiltration. Antimicrob Agents Chemother. 2016;60:1899-1901.
5. Bergner R, Hoffmann M, Riedel KD, Mikus G, Henrich DM, Haefeli WE, Uppenkamp M,
Walter-Sack I. Fluconazole dosing in continuous veno-venous haemofiltration (CVVHF):
need for a high daily dose of 800 mg. Nephrol Dial Transplant. 2006;21(4):1019-23.
6. Pea F, Viale P, Pavan F, Furlanut M. Pharmacokinetic considerations for antimicrobial
therapy in patients receiving renal replacement therapy. Clin Pharmacokinet.
2007;46(12):997-1038.
7. Awissi d, Beauchamp A, Hebert E, Lavigne V, Munoz DL, Lebrun G, Savoie M, et al.
Pharmacokinetics of an extended 4-hour infusion of piperacillin-tazobactam in critically ill
patients undergoing continuous renal replacement therapy. Pharmacotherapy. 2015;35:600-
607.
8. Honore PM, Jacobs R, Joannes-Boyaud O, et al. Continuous renal replacement therapy-
related strategies to avoid colistin toxicity: a clinically oriented review. Blood Purif.
2014;37:291-295.
Prepared By: Greg Peitz, PharmD, BCCCP; Kiri Rolek, PharmD, BCPS; Trevor Van Schooneveld, MD
Approved by Antimicrobial Stewardship Program: June 2016
You might also like
- Pharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamFrom EverandPharmacy Calculation Workbook: 250 Questions to Prepare for the NAPLEX and PTCB ExamRating: 5 out of 5 stars5/5 (1)
- Vancomycin Dosing RecommendationsDocument2 pagesVancomycin Dosing RecommendationsStacey WoodsNo ratings yet
- Antimicrobial Renal DosingDocument5 pagesAntimicrobial Renal DosingdamondouglasNo ratings yet
- Stanford Health Care Antimicrobial Dosing Reference GuideDocument7 pagesStanford Health Care Antimicrobial Dosing Reference GuideKarl Martin PinedaNo ratings yet
- Picu NotesDocument65 pagesPicu NotesAhmed Mohammed100% (2)
- Drugrenaladjustment 12052565Document18 pagesDrugrenaladjustment 12052565jirat iyarapongNo ratings yet
- SHC ABX Dosing GuideDocument7 pagesSHC ABX Dosing GuideDanielVillaNo ratings yet
- SHC ABX Dosing GuideDocument7 pagesSHC ABX Dosing GuideDeena AlJawamisNo ratings yet
- Am Iog Lyco SidesDocument2 pagesAm Iog Lyco Sidesthemega1111No ratings yet
- Stanford Dosing AntibioticsDocument6 pagesStanford Dosing AntibioticsSayeerah MamaNo ratings yet
- Stanford Health Care Antimicrobial Dosing Reference GuideDocument6 pagesStanford Health Care Antimicrobial Dosing Reference GuidePaan SuthahathaiNo ratings yet
- 38054 台北市聯合醫院抗生素商品名對照表 PDFDocument99 pages38054 台北市聯合醫院抗生素商品名對照表 PDFka timNo ratings yet
- Aminoglycoside Guideline For Children-2Document7 pagesAminoglycoside Guideline For Children-2Alina CaraciobanuNo ratings yet
- GentamiciniDocument11 pagesGentamiciniBenjie SisonNo ratings yet
- 107.11.1 GlycopeptidePK - 20181101 - GIOCP - Case - Part2Document4 pages107.11.1 GlycopeptidePK - 20181101 - GIOCP - Case - Part2ft84nzzc92No ratings yet
- Tablas de Dosificacion Kirk 9na EdDocument68 pagesTablas de Dosificacion Kirk 9na EdMarlieth Rosales HernandezNo ratings yet
- TCHP-Docetaxel Carboplatin Trastuzumab Pertuzumab Neoadjuvant Adjuvant Protocol V2.2Document21 pagesTCHP-Docetaxel Carboplatin Trastuzumab Pertuzumab Neoadjuvant Adjuvant Protocol V2.2smokkerNo ratings yet
- Doses Commonly Prescribed Antibiotics PDFDocument13 pagesDoses Commonly Prescribed Antibiotics PDFAhmed SobhNo ratings yet
- New Zealand Data Sheet: 1. Product NameDocument15 pagesNew Zealand Data Sheet: 1. Product NameMhd IjlalNo ratings yet
- Drug Dose Pediatrics NephrologyDocument16 pagesDrug Dose Pediatrics NephrologyNujhat TabassumNo ratings yet
- Tabla AINE PDFDocument1 pageTabla AINE PDFÁmbar GonzálezNo ratings yet
- JMHPCardAntiretrovirals15 PDFDocument2 pagesJMHPCardAntiretrovirals15 PDFindahfitria87No ratings yet
- Antiepileptic Doses: Medication FDA Approval Maintenance Oral DoseDocument1 pageAntiepileptic Doses: Medication FDA Approval Maintenance Oral DoseLolo GhostNo ratings yet
- Guidelines For Intravenous Albumin Administration PDFDocument4 pagesGuidelines For Intravenous Albumin Administration PDFKunni MardhiyahNo ratings yet
- Digoxin Phenytoin Cyclosporin e Tacrolimu S Sirolimus Lithium CBZ VA PhenobarbDocument5 pagesDigoxin Phenytoin Cyclosporin e Tacrolimu S Sirolimus Lithium CBZ VA PhenobarbDana MradNo ratings yet
- 2014 SHC ABX Dosing GuideDocument4 pages2014 SHC ABX Dosing GuideisnaeniNo ratings yet
- SHC Antimicrobial Dosing GuideDocument7 pagesSHC Antimicrobial Dosing GuideHelder LopesNo ratings yet
- AST and Dosing Info Card - FINALDocument2 pagesAST and Dosing Info Card - FINALGAYATHIRINo ratings yet
- Docetaxel Carboplatin Trastuzumab T Carbo H Breast Cancer Adjuvant ProtocolDocument14 pagesDocetaxel Carboplatin Trastuzumab T Carbo H Breast Cancer Adjuvant ProtocolsmokkerNo ratings yet
- Enoxaparin Info SheetDocument7 pagesEnoxaparin Info SheetjafarkassimNo ratings yet
- Cefepime Kabi DatasheetDocument16 pagesCefepime Kabi Datasheetتوفيق باعبادNo ratings yet
- Ozempic Dispensing Quick Reference Guide 2023-06-07Document2 pagesOzempic Dispensing Quick Reference Guide 2023-06-07Graham Thomas GipsonNo ratings yet
- qt753782f6 NosplashDocument4 pagesqt753782f6 NosplashGeorge E. FergusonNo ratings yet
- Stanford Hospital & Clinics Antimicrobial Dosing Reference Guide 2013Document3 pagesStanford Hospital & Clinics Antimicrobial Dosing Reference Guide 2013SANCHOSKYNo ratings yet
- Cushing's Syndrome: Oleh: Kelompok VDocument15 pagesCushing's Syndrome: Oleh: Kelompok VMakmunNawilNo ratings yet
- 12 Merritt Lecture 2 Lead ToxicityDocument85 pages12 Merritt Lecture 2 Lead ToxicityЩербакова ЛенаNo ratings yet
- VBMC Heparin Protocol FINAL May2004Document3 pagesVBMC Heparin Protocol FINAL May2004Pharmacy OneSource100% (1)
- NSAID藥物整理Document2 pagesNSAID藥物整理kennyNo ratings yet
- Antimicrobial Dosing GuideDocument7 pagesAntimicrobial Dosing GuideMuhammad RawasNo ratings yet
- Dosis PCT 10mg/kg/× Ibuprofen 5-10mg/kg/xDocument3 pagesDosis PCT 10mg/kg/× Ibuprofen 5-10mg/kg/xdeaaannnnnnNo ratings yet
- 1.13 Hyper-CVAD-MA Version 2.1Document5 pages1.13 Hyper-CVAD-MA Version 2.1Alina CrissNo ratings yet
- Icu Adult and PaedsDocument2 pagesIcu Adult and PaedsPrashin RocharamNo ratings yet
- Antibiotic Dosing Guidelines For Renal ImpairmentDocument6 pagesAntibiotic Dosing Guidelines For Renal ImpairmentvitauxianaNo ratings yet
- Renal PharmacologyDocument52 pagesRenal PharmacologyashrafNo ratings yet
- CC2-LABDocument4 pagesCC2-LABCOC UNIVERSALNo ratings yet
- ICU Rabu 29.01.2020: Nama Umur Diagnosa Diet Gcs + TTV Resp Terapi Plan BalanceDocument3 pagesICU Rabu 29.01.2020: Nama Umur Diagnosa Diet Gcs + TTV Resp Terapi Plan BalanceAndre AzharNo ratings yet
- Noradrenaline Infusion Rate BSUH Critical CareDocument4 pagesNoradrenaline Infusion Rate BSUH Critical CareAndreiCostei100% (1)
- Antibiotic - Bactrim Dosage GuideDocument3 pagesAntibiotic - Bactrim Dosage GuidejustanothergunnutNo ratings yet
- Aminoglycosides:: Setting Initial DoseDocument4 pagesAminoglycosides:: Setting Initial DoseArham AhmedNo ratings yet
- RANITIDINE - Ranitidine Hydrochloride Injection, Solution: Page 1 of 9Document9 pagesRANITIDINE - Ranitidine Hydrochloride Injection, Solution: Page 1 of 9Nur Syamsiah LaisaNo ratings yet
- AntimicrobialDocument3 pagesAntimicrobiallamavakum 30No ratings yet
- Acute Coronary ReportDocument15 pagesAcute Coronary ReportNormana ZureikatNo ratings yet
- 21 - 246berita Terkini-Guideline IDSA-ATS 2016 Untuk HAP Dan VAP PDFDocument1 page21 - 246berita Terkini-Guideline IDSA-ATS 2016 Untuk HAP Dan VAP PDFMariana MarpaungNo ratings yet
- Renal PharmacologyDocument52 pagesRenal Pharmacologyashraf0% (1)
- Renal Dosing2Document3 pagesRenal Dosing2Mohammed IbrahimNo ratings yet
- Dosing Protocol RPeducationDocument28 pagesDosing Protocol RPeducationbala muruganNo ratings yet
- Jurnal EndokarditisDocument2 pagesJurnal EndokarditisAwang WibisonoNo ratings yet
- NFCC. Chapter 8. ElectrolytesDocument13 pagesNFCC. Chapter 8. ElectrolytesOsman fadilNo ratings yet
- Answers To Practice Problem Set #10Document3 pagesAnswers To Practice Problem Set #10Raju NiraulaNo ratings yet
- MID 3 PHARMA Chemotherapeutic AgentsDocument85 pagesMID 3 PHARMA Chemotherapeutic AgentsMariah Angela PinedaNo ratings yet
- Stockverfication NewDocument184 pagesStockverfication NewbhadushaNo ratings yet
- Pt. Rania Jaya Farmarindo Daftar Harga Jual PersediaanDocument22 pagesPt. Rania Jaya Farmarindo Daftar Harga Jual PersediaanWulan FitriNo ratings yet
- Aminoglycosides STUDY GUIDEDocument3 pagesAminoglycosides STUDY GUIDEBen Thomas MooreNo ratings yet
- Psychotropic Drugs: Bryan Mae H. DegorioDocument65 pagesPsychotropic Drugs: Bryan Mae H. DegorioBryan Mae H. Degorio100% (2)
- Drugs For Anxiety P Colg RP 3Document48 pagesDrugs For Anxiety P Colg RP 3Theola FrancescaNo ratings yet
- Characteristics of MetamizoleDocument9 pagesCharacteristics of MetamizoleLisa NPNo ratings yet
- 5 Materi DR Ida PainDocument24 pages5 Materi DR Ida PainIkaVeristianaSantiNo ratings yet
- BTK AGUSTUS MutasiObatDocument48 pagesBTK AGUSTUS MutasiObatwulanwidya06No ratings yet
- Introduction To Toxicology 2017 by Dr. PerezDocument15 pagesIntroduction To Toxicology 2017 by Dr. PerezJohn Christopher LucesNo ratings yet
- Stok PH 16 Feb 22Document30 pagesStok PH 16 Feb 22Fahry Shamad TumoroNo ratings yet
- Omega Division Price List: NO Produk Komposisi Kemasan Hna / Box Hna + PPN Branded ProductDocument1 pageOmega Division Price List: NO Produk Komposisi Kemasan Hna / Box Hna + PPN Branded ProductSony Zailer'sNo ratings yet
- List of 24/7 Pharmacies: Firm No. Firm Name Firm Address MobileDocument14 pagesList of 24/7 Pharmacies: Firm No. Firm Name Firm Address Mobilegaurav jainNo ratings yet
- (E) Diagnostic and Therapeutic Modern PharmacologyDocument62 pages(E) Diagnostic and Therapeutic Modern PharmacologyPreeti PatelNo ratings yet
- Injectable Drugs Monographs v2Document201 pagesInjectable Drugs Monographs v2Ihab Moustafa100% (2)
- SO lt.2Document180 pagesSO lt.2Armyta AgustinaNo ratings yet
- Vitamin: NO Nama Obat Stok Fisik ED Komp Keterangan/SelisihDocument4 pagesVitamin: NO Nama Obat Stok Fisik ED Komp Keterangan/SelisihHalimatun SyadyahNo ratings yet
- NCM 206 - PharmacologyDocument17 pagesNCM 206 - PharmacologyJonathan RanocoNo ratings yet
- Regulatory Alert Unbranded Enforcement - Digitas Health - May 2010Document2 pagesRegulatory Alert Unbranded Enforcement - Digitas Health - May 2010Dale CookeNo ratings yet
- Hindawi Publishing Corporation Journal of Pharmaceutics Volume 2014, Article ID 808167, 8 PagesDocument14 pagesHindawi Publishing Corporation Journal of Pharmaceutics Volume 2014, Article ID 808167, 8 PagesnanangNo ratings yet
- 100 Psychotropic Medications - Generic NamesDocument2 pages100 Psychotropic Medications - Generic NamesJerry Don Smith, Jr.100% (4)
- Learning Module 5 - Forensic ChemDocument22 pagesLearning Module 5 - Forensic ChemjohnNo ratings yet
- Ward Class IV and Meds ComputationDocument3 pagesWard Class IV and Meds ComputationyasiraNo ratings yet
- Drug Receptor InteractionDocument29 pagesDrug Receptor InteractionFaisal RahmanNo ratings yet
- Guideline For Intravenous Aminophylline in AdultsDocument4 pagesGuideline For Intravenous Aminophylline in AdultsjesusNo ratings yet
- 04 - Extravascular Administration (Oral)Document41 pages04 - Extravascular Administration (Oral)Prasanna PappuNo ratings yet
- DR James Duke Benefits of MangosteenDocument6 pagesDR James Duke Benefits of Mangosteenrjuicebiz100% (1)
- M2 - Lesson 1 - Preparation of Standard Patient ScriptingDocument22 pagesM2 - Lesson 1 - Preparation of Standard Patient ScriptingElleason Joshua G. FranciscoNo ratings yet
- Obat UperioDocument5 pagesObat UperioAnonymous Aa6VAStNo ratings yet
- Cognitive MedsDocument2 pagesCognitive MedsRNStudent1100% (1)