Professional Documents
Culture Documents
Pharmacology of Diabetes: Insulin and Oral Agents for Type 1 and Type 2 Diabetes
Uploaded by
mus zaharaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacology of Diabetes: Insulin and Oral Agents for Type 1 and Type 2 Diabetes
Uploaded by
mus zaharaCopyright:
Available Formats
Pharmacology of Diabetes
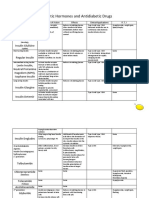
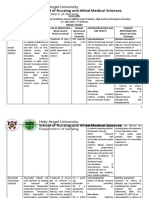
Type 1 DM – Insulin: acts by tyrosine kinase system → increases glucose uptake by muscles and fat, decreases hepatic glucose output, and controls postprandial hyperglycemia. Duration of action of an insulin preparation differed
from other insulin preparations mainly due to change in its rate of absorption from the site of injection.
Onset of Duration
Preparation Peak AE Interactions Uses Other
action of action
Rapid-acting (5-15 minutes before meal) -PK: SC, IM, IV. Site of injection: most rapid
-Hypoglycemia: -Type 1 DM
Insulin lispro --blockers (-1 selective & non-selective): from abdominal wall>arm>buttock>thigh.
palpitations, sweating,
Insulin aspart 10-30 min 30-60 min 3-5 hrs mask symptoms of hypoglycemia
anxiety, nausea, -Diabetic ketoacidosis
Insulin glulisine (palpitations, tremors, anxiety) -Rapid-acting & short-acting insulins used
hunger, headaches, (hyperglycemia, acidosis,
Short-acting (30 minutes before meal) for controlling post-prandial
confusion, dizziness, dehydration)
Regular insulin 30-60 min 1-2 hours 5-7 hrs -Ethanol: blocks gluconeogenesis & hyperglycemia
blurred vision, bizarre
Intermediate-acting behavior, seizures, glycogenolysis → precipitates hypoglycemia -Diabetes in pregnancy (drug of
NPH -Intermediate & long-acting insulins used to
1-2 hrs 6-12 hrs 18-24 hrs coma choice)
(Insulin isophane) provide basal levels in between meals.
-Salicylates
Long-acting Glargine has sustained “peak-less”
-Allergic reactions -Type 2 diabetics: who fail to respond
absorption → associated with less
-Loop diuretics & thiazides: blood glucose to combination therapy with oral
hypoglycemia.
-Lipodystrophy levels & effectiveness of insulin; antidiabetic agents; who have
Insulin glargine 1-2 hrs No Peak 24 hrs (atrophy or concomitant use with insulin → risk of contraindications for using oral
-Regular insulin can be injected IV (used
Insulin detemir 1-2 hrs 3-9 hrs >12 hrs hypertrophy of fat hypokalemia → ventricular arrhythmia, antidiabetic drugs & exenatide; who
in diabetic ketoacidosis & hyperglycemic
tissue at site of respiratory paralysis, & death are under stressful conditions
emergencies)
injection) (surgery, acute illness, accident)
Type 2 DM
• Goal of all MOA’s: sugar levels
• Diet and exercise is important in the initial management of Type 2 DM before starting treatment with oral antidiabetic agents.
Insulin Secretagogues (hypoglycemic effect requires functioning beta-cells in the pancreatic islets of Langerhans)
Half-life Duration of
Class Drug MOA Adverse Effects Interactions Uses
(hrs) action (hrs)
Tolbutamide* 4-5 6-12 Hypoglycemia (very rare); weight gain; safe in elderly
-Potentiation of hypoglycemic effect:
-Block ATP-sensitive K+ Hypoglycemia (more common); Disulfiram-like
reaction with alcohol; potentiate ADH action (water insulin, alcohol, -blockers, salicylates Management of
Chlorpropamide* channels in pancreatic 24-32 ~60 -Diminished hypoglycemic effect: neurogenic diabetes
beta cells → change retention) → dilutional hyponatremia → SIADH;
corticosteroids, thiazides, loop- insipidus
Sulfonylureas resting potential of cells weight gain
diuretics, phenytoin
Glyburide** → opening of voltage- 4-6 18-24 Hypoglycemia; weight gain
-CI: pregnancy. Sulfa allergy,
gated calcium channels Hypoglycemia (less chances); weight gain; preferred in
Glipizide** 2-4 14-16 significant hepatic and renal
→ calcium influx → elderly
insufficiency
Glimepiride** release of preformed 5-7 ~24 Hypoglycemia (less chances); weight gain
insulin. Short-duration
-Sulfonylureas reduce Control postprandial
(fast-acting: taken
Meglitinides Repaglinide glucagon concentrations <1 Hypoglycemia (less chances); weight gain hyperglycemia, allergic to
10-15mins before
sulfonylureas
meal)
** are preferred over * for managing Type 2 DM. 2nd generation agents are more potent, equally efficacious, and their biological actions last longer.
Class Drug MOA Adverse effects Uses
-GI disturbances: nausea, diarrhea -“Anti-hyperglycemic”
- Glucose production by the liver (acts mainly in the liver)
-Lactic acidosis: chances in predisposing conditions – renal -For obese type 2 DM patients
-Activation of AMP-stimulated protein kinase → gluconeogenesis, insulin
Biguanides Metformin impairment, hepatic disease, alcoholism, cardiac failure, MI, & (reduce plasma triglycerides by
resistance, glucose absorption from GI, plasma glucagon 15-20%)
chronic hypoxic lung disease
-Half-life = 1.5-3hrs -Polycystic ovary syndrome
-Does not cause hypoglycemia or weight gain
- Uptake of sugar by muscle & fat cells
Rosiglitazone
-Selective agonist of nuclear PPAR - activation of insulin-responsive genes that -Fluid retention, edema, angina, MI, heptatoxicity
Thiazolidinediones regulate carbohydrate & lipid metabolism → insulin resistance / insulin -Do not cause hypoglycemia “Insulin sensitizers”
Pioglitazone sensitivity (activation of adiponectin) -CI: congestive heart failure (BBW) & liver disease
-Max effects after 6-12wks
-Slow sugar absorption in the gut
Acarbose -Flatulence, diarrhea, abdominal pain
-Glucosidase -Inhibit breakdown of starch & oligosaccharides to monosaccharaides by
-Hypoglycemia when used with other secretagogues (Tx: glucose)
inhibitors inhibiting -glucosidases → slows absorption of carbohydrates & blunts
Miglitol -CI: inflammatory bowel disease, renal & hepatic dysfunction
postprandial rise in plasma glucose
-“Glucose-dependent” insulin secretion ( insulin secretion when glucose levels
GLP-1 receptor are elevated)
-Nausea, vomiting, diarrhea
agonist (incretin Exenatide -Suppresses glucagon secretion
-Rare & fatal: necrotizing & hemorrhagic pancreatitis -SC
mimetic) -Slows gastric emptying ( rate of glucose entering circulation)
- Appetite
- Degradation of endogenous incretins → GLP-1 & GIP
DPP-4 inhibitor Sitagliptin Nasopharyngitis, upper respiratory infections, headache
- Glucose mediated insulin secretion & glucagon levels
You might also like
- DM TreatmentDocument9 pagesDM TreatmentAshraf AbdullahNo ratings yet
- Pancreatic Hormones and Diabetes: Bantilan Borden EstreraDocument12 pagesPancreatic Hormones and Diabetes: Bantilan Borden EstreraKiarra Angelu Martinez EstreraNo ratings yet
- ApidraDocument4 pagesApidraRobert Ivan AgujarNo ratings yet
- Endocrine Chart - DM MedsDocument7 pagesEndocrine Chart - DM MedsrhondaNo ratings yet
- Med BundleDocument36 pagesMed Bundlejamie sealNo ratings yet
- Diabetes Drug Chart: Drug Action Use Side Effects Nursing ImplicationsDocument2 pagesDiabetes Drug Chart: Drug Action Use Side Effects Nursing ImplicationspulmonologistNo ratings yet
- Diabetes MellitusDocument9 pagesDiabetes Mellitusapi-708254576No ratings yet
- Insulin HandbookDocument67 pagesInsulin HandbookThits SarNo ratings yet
- Pharmacology Pre-Finals Antidiabetics InsulinDocument4 pagesPharmacology Pre-Finals Antidiabetics InsulinMaderazo, Rowan XinNo ratings yet
- Novolin and HumulinDocument3 pagesNovolin and HumulinChynnaNo ratings yet
- Pancreatic Hormones and Antidiabetic DrugsDocument6 pagesPancreatic Hormones and Antidiabetic DrugsCas BuNo ratings yet
- Manage Insulin Therapy SafelyDocument3 pagesManage Insulin Therapy SafelyTri Purma SariNo ratings yet
- Insulin Detemir Overview and Nursing ConsiderationsDocument2 pagesInsulin Detemir Overview and Nursing ConsiderationsFeliciaDorghamNo ratings yet
- Skills LabDocument107 pagesSkills LabskybluealiNo ratings yet
- Drug Study On Agents Used Thyroid and Glucose Metabolism - ClementeDocument18 pagesDrug Study On Agents Used Thyroid and Glucose Metabolism - ClementeJames Emman ClementeNo ratings yet
- Insulin Treatment in DiabetesDocument86 pagesInsulin Treatment in DiabetesAhsan Rauf100% (1)
- Anti Diabetic DrugsDocument2 pagesAnti Diabetic DrugsChenai04No ratings yet
- Pomr Mik SK 4 NeewwDocument4 pagesPomr Mik SK 4 NeewwDewi Ayu CahyaningrumNo ratings yet
- Diabetes & ArthritisDocument4 pagesDiabetes & ArthritisGeoffrey KernsNo ratings yet
- INSULINDocument6 pagesINSULINmilaNo ratings yet
- Drug Study (3rd Rot.) (GMC) - JSGSDocument6 pagesDrug Study (3rd Rot.) (GMC) - JSGSJohannes SantosNo ratings yet
- Drugs For Diabetes PDFDocument4 pagesDrugs For Diabetes PDFDylan RastoNo ratings yet
- Jyane ReubenDocument35 pagesJyane ReubenAmr El-RefaeyNo ratings yet
- Drugs For The Treatment of Diabetes MellitusDocument54 pagesDrugs For The Treatment of Diabetes MellitusAndreas AndreouNo ratings yet
- Insulin Glulisine (rDNA Origin) : (In-Su-Lin Gloo-Lye-Seen)Document3 pagesInsulin Glulisine (rDNA Origin) : (In-Su-Lin Gloo-Lye-Seen)FeliciaDorghamNo ratings yet
- Insulinas de OsmosisDocument3 pagesInsulinas de OsmosisDennise A. Hernández JuárezNo ratings yet
- Type 2 Diabetes Treatment Options ExplainedDocument2 pagesType 2 Diabetes Treatment Options ExplainedSafiya JamesNo ratings yet
- Drugs For The Treatment of Diabetes MellitusDocument55 pagesDrugs For The Treatment of Diabetes MellitusAparna DheerajNo ratings yet
- Yr5 InsulinTherapyDocument61 pagesYr5 InsulinTherapyCrystel Tze JingNo ratings yet
- Drugs For Diabetes MellitusDocument3 pagesDrugs For Diabetes MellitusGerardLum100% (1)
- Insulin IssuesDocument6 pagesInsulin Issuesdoctorzo0% (1)
- Insulin History & Modality For Diabetic Patient: A. Makbul M. AmanDocument69 pagesInsulin History & Modality For Diabetic Patient: A. Makbul M. AmanRey Alwiwikh100% (1)
- Insulin As PartDocument3 pagesInsulin As PartRezaNo ratings yet
- Diabetes DrugsDocument1 pageDiabetes DrugsFlowerNo ratings yet
- Insulin, Oral Hypoglycaemic Agents, GlucagonDocument63 pagesInsulin, Oral Hypoglycaemic Agents, GlucagonBhavesh kunvarNo ratings yet
- The Essential Role of Insulin in Diabetes ManagementDocument9 pagesThe Essential Role of Insulin in Diabetes ManagementAbdul SamadNo ratings yet
- Rapid-Acting Insulin (Onset: 15-30 MinsDocument5 pagesRapid-Acting Insulin (Onset: 15-30 MinsBea TanNo ratings yet
- Drug Study Insulin LisproDocument2 pagesDrug Study Insulin LisproEzron Kendrick Duran100% (1)
- Pharmacology of Diabetes Mellitus: Glucose RegulationDocument33 pagesPharmacology of Diabetes Mellitus: Glucose RegulationAbdullah RawashdehNo ratings yet
- Endocrine CologyDocument124 pagesEndocrine CologyBehailu TejeNo ratings yet
- Case Clue - 1 LinersDocument753 pagesCase Clue - 1 LinersOnly MrcpNo ratings yet
- Nursing - CS - Comparison Chart of Different Insulins - 04Document1 pageNursing - CS - Comparison Chart of Different Insulins - 04Jazzmine GuraNo ratings yet
- Medical-Surgical Nursing Final Flashcards - QuizletDocument22 pagesMedical-Surgical Nursing Final Flashcards - QuizletNursyNurseNo ratings yet
- 4DM PresentationDocument57 pages4DM Presentationamal nassarNo ratings yet
- Drugs For Diabetes MellitusDocument50 pagesDrugs For Diabetes MellitusCherenet TomaNo ratings yet
- Insulin dose and administration guidelinesDocument8 pagesInsulin dose and administration guidelinesMichael Jay MelindoNo ratings yet
- Pancreatic Hormones and DM DrugsDocument55 pagesPancreatic Hormones and DM DrugsDann San AntonioNo ratings yet
- Insulin and Its Preparation: DR C.Sadhana Final Year MD Pharmacology Department of Pharmacology SBMCHDocument62 pagesInsulin and Its Preparation: DR C.Sadhana Final Year MD Pharmacology Department of Pharmacology SBMCHP Vinod KumarNo ratings yet
- Oral Antidiabetes MedicationsDocument4 pagesOral Antidiabetes MedicationsAshwinNo ratings yet
- Pharma Medications and TreatmentsDocument3 pagesPharma Medications and TreatmentsMary Joy Morales BuquiranNo ratings yet
- GUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامDocument1 pageGUIDELINES FOR INPATIENT DIABETES MANAGEMENT هااامAbu HuzaifaNo ratings yet
- Pharmacotherapy of Diabetes Mellitus: Dr. Ave Olivia Rahman, Msc. Bagian Farmakologi Fkik UnjaDocument42 pagesPharmacotherapy of Diabetes Mellitus: Dr. Ave Olivia Rahman, Msc. Bagian Farmakologi Fkik UnjaGita Tanbao SuselinNo ratings yet
- PANCREATIC HORMONES AND ANTIDIABETIC DRUGS: INSULIN AND SULFONYLUREASDocument5 pagesPANCREATIC HORMONES AND ANTIDIABETIC DRUGS: INSULIN AND SULFONYLUREASEric James ManuelNo ratings yet
- Chapter No 8 & 9Document10 pagesChapter No 8 & 9Anuj panditNo ratings yet
- InsulinDocument2 pagesInsulinKristine YoungNo ratings yet
- Diabetes Mellitus (D.M) : Type IDocument2 pagesDiabetes Mellitus (D.M) : Type IAnas SeghayerNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Insulin Handbook: Understanding the Role and Effects of Insulin in Your BodyFrom EverandInsulin Handbook: Understanding the Role and Effects of Insulin in Your BodyNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Genitourinary Tract Tumors Including Renal Tumors: Pre-ReadingDocument31 pagesGenitourinary Tract Tumors Including Renal Tumors: Pre-Readingmus zaharaNo ratings yet
- 5 Pericarditis and Its Complications ICMPDDocument22 pages5 Pericarditis and Its Complications ICMPDmus zaharaNo ratings yet
- Angina Pectoris: Arun Dubey M.D. 2019Document18 pagesAngina Pectoris: Arun Dubey M.D. 2019mus zaharaNo ratings yet
- Arteriosclerosis With Special Emphasis On Atherosclerosis: Pre-Reading: Robbins Basic Pathology 9th Ed: Pages 335-343Document49 pagesArteriosclerosis With Special Emphasis On Atherosclerosis: Pre-Reading: Robbins Basic Pathology 9th Ed: Pages 335-343mus zaharaNo ratings yet
- Somatic Symptom and Related Disorders: Dr. Michelle MaceraDocument24 pagesSomatic Symptom and Related Disorders: Dr. Michelle Maceramus zaharaNo ratings yet
- Renal System Embryology Development StagesDocument52 pagesRenal System Embryology Development Stagesmus zaharaNo ratings yet
- Outbreaks: DR HL HarveyDocument12 pagesOutbreaks: DR HL Harveymus zaharaNo ratings yet
- Body Fluids: DR Sheetal C NDocument34 pagesBody Fluids: DR Sheetal C Nmus zaharaNo ratings yet
- 4 Valvular Heart Disease ICMPD (Autosaved)Document30 pages4 Valvular Heart Disease ICMPD (Autosaved)mus zaharaNo ratings yet
- Diuretics part-1: Types, mechanisms, uses, interactions and adverse effectsDocument19 pagesDiuretics part-1: Types, mechanisms, uses, interactions and adverse effectsmus zaharaNo ratings yet
- Population Genetics: DR Malpe Surekha BhatDocument18 pagesPopulation Genetics: DR Malpe Surekha Bhatmus zaharaNo ratings yet
- Embryology and Congenital Anomalies of The Renal SystemDocument45 pagesEmbryology and Congenital Anomalies of The Renal Systemmus zaharaNo ratings yet
- Genetic Engineering Applications and EthicsDocument18 pagesGenetic Engineering Applications and Ethicsmus zaharaNo ratings yet
- Regulation of Gene Expression-1Document30 pagesRegulation of Gene Expression-1mus zaharaNo ratings yet
- Genetic Codon: 3 NucleotidesDocument25 pagesGenetic Codon: 3 Nucleotidesmus zaharaNo ratings yet
- Transcription: Process of Copying of DNA Strand To Produce RNADocument39 pagesTranscription: Process of Copying of DNA Strand To Produce RNAmus zaharaNo ratings yet
- Assignment 1: CASL Subject: Epidemiology Instructor: Dr. Harvey MD: 2Document4 pagesAssignment 1: CASL Subject: Epidemiology Instructor: Dr. Harvey MD: 2mus zaharaNo ratings yet
- Genetic Engineering TechniquesDocument14 pagesGenetic Engineering Techniquesmus zaharaNo ratings yet
- Mutations-2: DR Surekha Bhat Professor in BiochemistryDocument11 pagesMutations-2: DR Surekha Bhat Professor in Biochemistrymus zaharaNo ratings yet
- Anatomy of A Chromosome: - During Cell Division, Each HumanDocument12 pagesAnatomy of A Chromosome: - During Cell Division, Each Humanmus zaharaNo ratings yet
- Patterns of Inheritance and PedigreeDocument58 pagesPatterns of Inheritance and Pedigreemus zaharaNo ratings yet
- Trachea, Bronchi and LungsDocument29 pagesTrachea, Bronchi and Lungsmus zaharaNo ratings yet
- Pharmacodynamics-2: Dr. PrasadDocument20 pagesPharmacodynamics-2: Dr. Prasadmus zaharaNo ratings yet
- 6-MONTH USMLE STEP 1 SCHEDULE SAMPLEDocument4 pages6-MONTH USMLE STEP 1 SCHEDULE SAMPLEmus zaharaNo ratings yet
- Biochem NotesDocument2 pagesBiochem Notesmus zaharaNo ratings yet
- Pictures For PathDocument23 pagesPictures For Pathmus zaharaNo ratings yet
- Arteriosclerosis With Special Emphasis On Atherosclerosis: Pre-Reading: Robbins Basic Pathology 9th Ed: Pages 335-343Document49 pagesArteriosclerosis With Special Emphasis On Atherosclerosis: Pre-Reading: Robbins Basic Pathology 9th Ed: Pages 335-343mus zaharaNo ratings yet
- Bleeding Disorders: Dr. Vishal Saxena MBBS, MD (Path), FicmrDocument59 pagesBleeding Disorders: Dr. Vishal Saxena MBBS, MD (Path), Ficmrmus zaharaNo ratings yet
- Stableangina 140720111702 Phpapp01Document66 pagesStableangina 140720111702 Phpapp01mus zaharaNo ratings yet
- Porphyrins: Heme DegradationDocument2 pagesPorphyrins: Heme Degradationmus zaharaNo ratings yet
- 17-Year-Old Man With Sudden Left Testicular PainDocument20 pages17-Year-Old Man With Sudden Left Testicular PainnurisumirizqiNo ratings yet
- World Congress of Internal Medicine (WCIM) 2014 Poster PresentationDocument34 pagesWorld Congress of Internal Medicine (WCIM) 2014 Poster PresentationTenri AshariNo ratings yet
- Republic of The Philippines City of Taguig Taguig City University Gen. Santos Avenue, Central Bicutan, Taguig CityDocument2 pagesRepublic of The Philippines City of Taguig Taguig City University Gen. Santos Avenue, Central Bicutan, Taguig CityAldrich ColladoNo ratings yet
- Diabetes Melittus 12Document19 pagesDiabetes Melittus 12mnmrznNo ratings yet
- Narayani Excel Sheet Remedies GuideDocument50 pagesNarayani Excel Sheet Remedies GuideNicky Chhajwani100% (1)
- Schilling Test: DR - CSBR.Prasad, M.D.Document26 pagesSchilling Test: DR - CSBR.Prasad, M.D.muhammad100% (1)
- Orion Anterior STDocument28 pagesOrion Anterior STmatameaNo ratings yet
- Care of Patient On VentilatorDocument18 pagesCare of Patient On VentilatorJose Paul Rader100% (1)
- Uro-Final MCQDocument45 pagesUro-Final MCQع كيف كيفك Dhaif-saeedNo ratings yet
- Counseling People With Early-Stage Alzheimer's Disease: A Powerful Process of Transformation (Yale Counseling People Excerpt)Document6 pagesCounseling People With Early-Stage Alzheimer's Disease: A Powerful Process of Transformation (Yale Counseling People Excerpt)Health Professions Press, an imprint of Paul H. Brookes Publishing Co., Inc.No ratings yet
- Psyche SupplementDocument51 pagesPsyche SupplementAchilles YbarraNo ratings yet
- Diabetic MellitusDocument26 pagesDiabetic Mellitusabdallaah adenNo ratings yet
- Mock Exam 2Document18 pagesMock Exam 2Anna StacyNo ratings yet
- Healthy Habits Summative TestDocument1 pageHealthy Habits Summative Testliz100% (1)
- DNA Fingerprinting in Human Health and SocietyDocument3 pagesDNA Fingerprinting in Human Health and SocietyGursharan Singh AnamikaNo ratings yet
- DNB Emergency Medicine Paper3Document5 pagesDNB Emergency Medicine Paper3Vaishnavi AgrawalNo ratings yet
- Daftar Pustaka Marwah NH 1210312044Document4 pagesDaftar Pustaka Marwah NH 1210312044Linda WijayantiNo ratings yet
- Atenolol Drug StudyDocument2 pagesAtenolol Drug StudyFranz.thenurse6888100% (2)
- SIP On Essential OilsDocument17 pagesSIP On Essential OilsJessa Marie SuarezNo ratings yet
- Pedia Ward Drug Study...Document12 pagesPedia Ward Drug Study...Sheena Arnoco ToraynoNo ratings yet
- NBME Form 1 Step 2 ReviewDocument77 pagesNBME Form 1 Step 2 Reviewalex karevNo ratings yet
- Skoring Osas AmirahDocument11 pagesSkoring Osas AmirahthtklNo ratings yet
- Diet PregnancyDocument62 pagesDiet Pregnancyvaibhav.manchester9372No ratings yet
- Case Group 1Document10 pagesCase Group 1JASMEEN RAVALNo ratings yet
- 82-Year-Old Male With Left HemiparesisDocument12 pages82-Year-Old Male With Left HemiparesisAulia Silkapianis100% (1)
- Arthritis Guide: Classification, Causes, Symptoms & TreatmentsDocument3 pagesArthritis Guide: Classification, Causes, Symptoms & TreatmentsMiguel Cuevas DolotNo ratings yet
- Nursing Care Plan for Fluid Volume DeficitDocument3 pagesNursing Care Plan for Fluid Volume Deficitnj_pink08179456% (9)
- HLTH 501 Final Exam SolutionsDocument13 pagesHLTH 501 Final Exam SolutionsCarl0% (8)
- Anaplasmosis - The Cattle SiteDocument2 pagesAnaplasmosis - The Cattle SiteLopesNo ratings yet
- Quick Number Codes List for Healing ApplicationsDocument18 pagesQuick Number Codes List for Healing ApplicationsHenrii Arias0% (1)