Professional Documents
Culture Documents
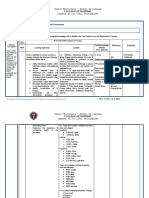
NCM 102 Care of Mother, Child, and Population Group at Risk or With Problems
Uploaded by
Ayman DaudOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCM 102 Care of Mother, Child, and Population Group at Risk or With Problems
Uploaded by
Ayman DaudCopyright:
Available Formats
NCM 102 High Risk Mom
Care of Mother, Child, and Population Group at Risk or
with Problems What is High Risk Pregnancy?
poor maternal or fetal outcome due to :
PRENATAL CARE medical
THE PURPOSE OF PRENATAL CARE IS TO ENSURE AN reproductive
UNCOMPLICATED PREGNANCY AND THE DELIVERY OF A Psychosocial
LIVE AND HEALTHY INFANT. Obstetrical
SCREENING
BALANCE OF FORCES IN PREGNANCY Diagnostic and Laboratory Examinations
FETAL SURVIVAL Complete Blood Count
MATERNAL SURVIVAL Hemoglobin
5 Branches of Maternal Health Hematocrit
• Nutrition Leukocyte
• Prenatal Care Thrombocytes
• Safe Delivery Blood Typing
• Breastfeeding Rhesus Factor
• Family Planning URINALYSIS
Prenatal Care Pus cells
• Regular prenatal care increases the chances of a Bacteria
healthy mother and child after birth. Protein/albumin
• Early detection of congenital & birth defects Sugar
• Prenatal immunizations can prevent mother-to- Squamous epithelial cells
child-transmission and infection. PAP SMEAR
DOH STANDARDS OF PRENATAL CARE ULTRASONOGRAPHY
1. WEIGHT Transabdominal
2. HEIGHT TRANSVAGINAL ULTRASOUND
3. BLOOD PRESSURE BLOOD GLUCOSE TEST
4. FHT FBS
5. FUNDIC HEIGHT HGT/CBG
• 5th month = 20 cm OGTT
• 6th month = 21-24 cm OGCT
• 7th month = 25-28 cm 2 HRS. POST PRANDIAL
• 8th month = 29-30 cm AMNIOCENTESIS
• 9th month = 30-34 cm Maternal Alpha-Feto Protein
6. LEOPOLD’S MANEUVER Fetal neural tube defect:
anencephaly
gastroschisis
spina bifida
DOPPLER VELOCIMETRY
PERCUTANEOUS UMBILICAL BLOOD SAMPLING
BIOPHYSICAL SCORING
30 minutes observation by USD
5 markers:
non stress test
fetal breathing
amniotic fluid
fetal body movement
fetal tone
BPS RESULT INTERPRETATION
8 – 10 - Normal fetus
6 - chronic asphyxia
7. TT IMMUNIZATION - repeat the procedure after 24 hours
TETANUS TOXOID WHEN TO GIVE 4 - abnormal result
TT 1 ANYTIME DURING 2 - ill fetus, terminate pregnancy
PREGNANCY Non Stress Test (NST)
TT 2 4 WEEKS AFTER TT 1 2 - 2 or more FHT acceleration
TT 3 6 MONTHS AFTER TT 2 per movement
TT 4 1 YEAR AFTER TT 3 1 - <2 accelerations
TT 5 1 YEAR AFTER TT 4 per movement
0 - no acceleration
8. DIET Fetal Breathing
9. DANGER SIGNS OF PREGNANCY 2 - 1 episode/30 minutes lasting 30 seconds
10. BREASTFEEDING 0 - no episode
11. FAMILY PLANNING - more than 30 minutes
12. POSTPARTUM CARE - not lasting 30 seconds
AMNIOTIC FLUID INDEX ATRIAL – SEPTAL DEFECT
2 - fluid filled pocket of 1 cm or more asymptomatic
0 - no amniotic fluid or less than 1 cm in every increase pulmonary blood flow
pocket pulmonary hypertension
FETAL BODY MOVEMENT VENTRICULAR SEPTAL DEFECT
2 - 3 or more discrete movement of limbs and left ventricular hypertrophy
body in 30 minutes pulmonary hypertension
1 - less than 3 movements biventricular hypertrophy
0 - no movements PATENT DUCTUS ARTERIOSUS
FETAL TONE rare
2 - 1 or more episodes of active extension with early surgical repair
return to flexion of limbs and trunk similar with VSD
1 - slow extension with return to flexion RHEUMATIC HEART DISEASE
0 - no movements Group A Beta Hemolytic Streptococcus
HEPATITIS B DETERMINATION Inflammatory process
1 Hepatitis B Antigen (HBSAg) Autoimmune disease
2 reactive - positive Scarring of the valves
3 non-reactive – negative SIGNS AND SYMTOMS OF CARDIAC DISEASES
4 Hepatitis B Antibiodies (HBSAb) Shortness of breath
qualitative Palpitations
quantitative Orthopnea
CONTRACTION STRESS TEST (CST) Expectoration of blood
done after 32 weeks AOG Cyanosis
Negative - normal; no fetal heart
Murmur
deceleration
Heart enlargement
Positive - abnormal; with deceleration
FUNCTIONAL CLASSIFICATIONS OF CARDIAC
FETOSCOPY
- Direct visualization of the fetus through a scope DISEASES
- Obtain sample tissues or blood
CLASS 1 - asymptomatic
- May perform intrauterine fetal surgery
FETAL MOVEMENT COUNTING CLASS II - symptomatic but with
- Done after 27 weeks AOG normal activities
- Twice daily for 20-30 minutes CLASS III - symptomatic and with less
- Normal – 5-6movements in 20-30 minutes than normal activities
- Abnormal – less done 3 movements in 1 hour CLASS IV - symptomatic and at rest
Judgment of safety of pregnancy
• Conception should be prevented if:
1. Severe heart disease
MEDICAL COMPLICATIONS DURING PREGNANCY
2. Functional classification: class III-IV
CARDIOVASCULAR DISORDERS
3. History of heart failure
PREGNANCY
4. Pulmonary hypertension
Increase blood volume 40 – 50%
5. Right to left shunting
Increase cardiac output
6. Severe arrhythmia
Decrease B during first trimester
7. rheumatic fever
Increase size of ventricular chamber
8. Combined valve disease
LEFT TO RIGHT SHUNTING
9. Acute myocarditis
MANAGEMENT OF CARDIAC DISEASES
o termination of pregnancy by CS
Weight reduction
Rest
prevent infection
Digoxin
Diuretics
NURSING CARE OF CARDIAC DISEASES
Vital signs
Provide rest
Emotional support
I & O monitoring
Proper nutrition
Carry out medical orders
GESTATIONALDIABETES MELLITUS Respiratory Depressant
RISK FACTORS CAUSING GDM ALCOHOL EFFECTS ON FETUS
Obesity Fetal Alcohol Syndrome (FAS)
Family history
Personal history Intrauterine Growth Restriction
Sedentary lifestyle Preterm Delivery
Improper diet
(PATHOPHYSIOLOGY NOT INCLUDED) CNS Depressants:
Morphine,
FETAL/NEONA TAL COMPLICATIONS OF GDM Heroin,
Fetal hyperglycemia
Fetal Hyperinsulinemia
Macrosomia
Prematurity
Respiratory Distress
Neonatal Hypoglycemia
MATERNAL COMPLICATIONS OF GDM
Preeclampsia
Polyhydramnious
Infection
Dystocia
Postpartum Bleeding
Birth canal trauma
Caesarean delivery
Fasting & 2 hours postprandial venous plasma sugar Methadone
during pregnancy. Analgesics
STIMULANTS
FASTING 2HRS POST RESULT Cocaine
PRANDIAL Amphetamine
<100 mg/dl < 145mg/ dl. Not diabetic Ecstacy
Caffeine
>125 mg/ dl >200 mg/ dl. Diabetic EFFECTS OF STIMULANTS
Increase Concentration
ORAL GLUCOSE CHALLENGE TEST Alertness
fasting post midnight Paranoia
blood and urine specimen are obtained Hypertension
50 grams glucose intake Psychosis
after 1 hour, blood and urine specimen is STIMULANTS’ EFFECTS ON FETUS
Preterm labor
obtained
Spontaneous abortion
A value above 130 – 140 gms/l one hour after
Placental abruption
is used as threshold for performing a 3-hour Fetal hypertension
OGTT. PREGNANCY SMOKING
Prerequisites of OGTT: Higher rates of spontaneous abortion, placenta
Normal diet for 3 days before the test. previa,
No diuretics 10 days before. Preterm labor
At least 10 hours fast. Low birth weight infant
Test is done in the morning at rest. Fetal hypertension
CRITERIA FOR OGTT MARIJUANA
The maximum blood glucose values during pregnancy: Relaxant
• fasting 90 mg/dl Hallucination
• one hour 165 mg/dl Short term Memory loss
• 2 hours 145 mg/dl Low birth weight Infant
• 3 hours 125 mg/dl Lifetime Effects of Substance Abuse
MANAGEMENT OF GDM Physical deformities
Insulin Mental Retardation
Diet Developmental Problem
Exercise
(END OF FIRST PRESENTATION)
Substance Abuse During Pregnancy
TERATOGEN
Any agents that interferes with normal
embryonic development
ALCOHOL
CNS Depressant
Reduce Anxiety
Sedation
6. AIDS
CD4 counts
Number of CD4 cells in blood provides a
measure of immune system damage
CD4 count reflects phase of disease
CD4 count:
500 – 1200: Normal
200 – 500: Beginning of HIV illness
< 200: AIDS
Window period
Time between infection & enough antibodies
Duration: approximately 3 months
No symptoms or signs of illness
HIV test is negative
Virus is multiplying rapidly - viral load is high
ACQUIRED IMMUNODEFFICIENCY SYNDROME Person is very infectious
Caused by HIV Seroconversion
Transmitted through blood, blood products, Point at which HIV test becomes positive
semen, vaginal fluid, breast milk Body starts making antibodies to HIV a few
Diagnosed by enzyme-linked immunosorbent weeks after infection
assay (ELISA) HIV test becomes positive
Confirmed by western blot test Person may have a mild flu-like illness, lasting a
week or two
SYMPTOMS OF AIDS Afterwards, the person is well again
Extreme weakness and fatigue Asymptomatic period
Rapid weight loss Time period between seroconversion and onset
Frequent fevers with no explanation of HIV/AIDS-related illness
Heavy sweating at night Duration variable: < 1 year to > 15 years
Swollen lymph glands Most people remain healthy (asymptomatic) for
Minor infections that cause skin rashes and about three years
mouth, genital, and anal sores. Duration may depend on socio-economic
White spots in the mouth or throat factors
Chronic diarrhea The CD4 count is above 500 cells/ml
A cough that won’t go away HIV/AIDS-Related Illness
Short-term memory loss Time period between onset of illness &
Fact or Fiction? diagnosis of AIDS
You can get AIDS from a mosquito bite Duration is variable: average about 5 years
Fact or Fiction? Illnesses initially mild, with gradual increase in
You can get AIDS by having oral sex with an infected frequency and severity
person CD4 count is between 500 & 200 cells/ml
Fact or Fiction? AIDS
HIV survives well in the environment, so you can get it Final phase of HIV/AIDS
from toilet seats and door knobs Duration: without antiretroviral drugs, less than
Fact or Fiction? 2 years with antiretrovirals, potentially many
You can get AIDS by hugging a person with HIV who is years
sweating CD4 count is below 200 cells/ml
Fact or Fiction? Viral loads are high & the person is very
You can get AIDS by kissing someone who is HIV infectious
infected Important Facts
Fact or Fiction? Duration of different phases of HIV/AIDS will
Condoms aren't really effective in preventing HIV vary in different people
transmission Factors affecting the course of HIV/AIDS include
Fact or Fiction? nutrition, emotional stress, and access to health
There is a connection between other STDS and HIV care
infection People infected with HIV can infect others at
any phase of the disease
How A Healthy Immune System Works Mother-to-Child Transmission
Physical Barriers: 25–35% of HIV positive pregnant mothers will
Innate Immune System: pass HIV to their newborns
Acquired Immune System: 30% of transmission in utero
How does HIV interrupt the Normal Functioning of the 70% of transmission during the delivery
Immune System? 14% transmission with breastfeeding
HIV infects T-cell Interventions to Reduce Mother-to-Child Transmission
Phases of HIV/AIDS HIV testing in pregnancy
1. Infection Antenatal care
2. Window period Antiretroviral agents
3. Seroconversion Obstetric interventions
4. Asymptomatic period o Avoid amniotomy
5. HIV/AIDS - related illness
o Avoid procedures: Forceps/vacuum Breasfeeding Issues
extractor, scalp electrode, scalp blood Warmth for newborn
sampling Nutrition for newborn
o Restrict episiotomy Protection against other infections
o Elective cesarean section Safety – unclean water, diarrheal diseases
o Remember infection prevention Risk of HIV transmission
practices Contraception for mother
Newborn feeding: Breastmilk vs. formula Cost
Antenatal Care Breastfeeding Recommendations
Watch for signs/symptoms of AIDS and promote exclusive breastfeeding for 6 months
pregnancy-related complications counsel on the safe and appropriate use of
Unless complication develops, no need to formula
increase number of visits HIV-positive and chooses to breastfeed,
Treat STDs and other coinfections promote exclusive breastfeeding for 6 months
Counsel against unprotected Rh Incompatibility
intercourse Rh – mother and Rh+ father
Avoid invasive procedures mostly on the second pregnancy
and external cephalic version during placental accidents
Give antiretroviral agents
Counsel about nutrition (NOT IN THE HANDOUTS)
Anti-retrovirals TYPES OF ANEMIA
Zidovudine (ZDV): Iron Deficiency Anemia
o Long course Megaloblastic Anemia
o Short course Pernicious Anemia
Nevirapine Folic Acid Deficiency Anemia
ZDV/lamivudine (ZDV/3TC) Aplastic Anemia
Obstetric Procedures to be avoided Hemolytic Anemia
Amniotomy Sickle Cell Anemia
Fetal scalp electrode/sampling Physiologic Anemia
Forceps/vacuum extractor Pathologic Anemia
Episiotomy SIGNS AND SYMPTOMS OF ANEMIA
Vaginal tears Pallor
Intrapartum Management Fatigue
Goal is to minimize duration of labor , Shortness of breath
Do not rupture membranes Hypotension
Avoid invasive monitoring Asymptomatic
Avoid episiotomy or instrumental delivery when DIAGNOSTIC EXAMINATIONS OF ANEMIA
possible Hemoglobin count......... 12 – 14 grams/dl
Delivery: Cesarean vs. Vaginal Birth Iron .............................. 50 – 150 grams/dl
Cesarean section before labor and/or rupture of Transferin ......................250 – 430 mg/ml
membranes reduces risk of mother-to-child Ferritin...........................11 – 20 g/ml
transmission by 50–80% Folate.............................7 – 20 g/ml
Cesarean section, however, increases morbidity Vit B12...........................200 – 800 g/ml
and possible mortality to mother MANAGEMENT OF PHYSIOLOGIC ANEMIA
Give antibiotic prophylaxis for cesarean section Rest
in HIV-infected women Fe Supplement
Recommended Infection Prevention Practices O2 Therapy
Needles: Nutrition
o Take care! Minimal use Blood Transfusion
o Suturing: Use appropriate needle and NURSING DIAGNOSIS OF ANEMIA
holder Altered Tissue Perfusion
o Care with recapping and disposal Altered Nutrition Less Than Body Requirements
Wear gloves, wash hands with soap Activity Intolerance
immediately after contact with blood and body HYPEREMESIS GRAVIDARUM
fluids Excessive vomiting that persists beyond 1st
Cover incisions with watertight dressings for trimester
first 24 hours contains:
Use: previous food intake
Plastic aprons for delivery mucus
Goggles and gloves for delivery and surgery bile
Long gloves for placenta removal finally blood
Dispose of blood, placenta and waste safely Predisposing Factors
PROTECT YOURSELF! Pancreatitis
Newborn Biliary tract dse
Wash newborn after birth, especially face Decrease Vit B6
Avoid hypothermia Psychological
Give antiretroviral agents, if available Drug toxicity
Precipitating Factors Tubal/Uterine Surgery
Pregnancy Intrauterine Device
Multiple pregnancy
Hydatidiform mole
Heredity
Female
MANAGEMENT OF HYPEREMESIS GRAVIDARUM
May need hospitalization
IVF infusion
Parenteral nutrition
Antiemetics
Progress diet – clear liquid, full liquid, soft, small
frequent, full diet
Midnight snacks
Parenteral vitamins and electrolyte
NURSING DIAGNOSIS OF HYPEREMESIS GRAVIDARUM
Actual/Potential Fluid Volume Deficit Signs and Symptoms of Ectopic Pregnancy
Imbalance Nutrition; less than Body Symptoms of bleeding
Requirements Bleeding into the uterine cavity
Fatigue Sharp one sided abdominal pain
Ineffective Coping Syncope
Anxiety Referred shoulder pain
Bleeding Complications of Pregnancy Lower abdominal pain
ABORTION Vaginal bleeding
- Termination of pregnancy before the age of Abdominal tenderness
viability Low HCG hormone
Spontaneous Abortion
Threatened Abortion
Imminent Abortion
Complete abortion
Incomplete Abortion
Missed Abortion
Recurrent/Habitual abortion
Septic Abortion
Induced Abortion
Therapeutic Abortion
Eugenic Abortion
Secondary Abortion
Signs and Symptoms of Abortion
Bleeding
Abdominal cramping Diagnostic Examinations of Ectopic Pregnancy
Passage of watery vaginal discharges Transvaginal ultrasound
Passage of product of conception Physical examination
Management of Threatened Abortion Pregnancy test
Bed rest HCG
Tocolytic medications Pelvic examinations
Treat underlying factors Management of Ectopic Pregnancy
No sexual activity Methotrexate
Fetal monitoring by ultrasound Salphingostomy via laparoscope
Avoid stress Laparoscopic salphingectomy
Management of Other Type Of Abortion Nursing Diagnosis
Hospitalization Alteration in Comfort; pain
Oxytocin administration Anticipatory grieving
Completion curettage Fluid volume deficit
Prophylactic antibiotic Hydatidiform Mole (H-MOLE/MOLAR PREGNANCY)
Analgesics Partial Mole
Fluid/blood replacement egg cell + 2 sperm cells
Emotional support Abnormal first meiotic division
NURSING DIAGNOSIS With fetus
Alteration in comfort; Pain Complete Mole
Anticipatory Grieving Empty egg + normal sperm
Risk for Fluid Volume Deficit Embryo dies at very early age
Ectopic Pregnancy No embryonic tissues
Signs and Symptoms of H- Mole
Factors Causing Ectopic Pregnancy Vaginal bleeding
Pelvic Inflammatory Diseases Uterine enlargement is bigger than usual
Previous Ectopic Pregnancy pregnancy
Increase HCG
Hyperemesis gravidarum Fetal death
No FHT/fetal movement Maternal factors
Management of H Mole MANAGEMENT OF PRETERM LABOR
Suction evacuation Bed rest
Dilatation and Curettage Avoid sexual contact
Hysterectomy Limit abdominal handling
Methotrexate Increase fiber in the diet
Placenta Previa Treat underlying factors
Implantation of the placenta at the lower Tocolytic medications
uterine segment Steroid
Risk Factors of Placenta Previa SIGNS AND SYMPTOMS
Advance maternal age Low back pain
Multiparity Suprapubic pressure
Previous uterine surgery Vaginal pressure
Breech and Transverse position Rhythmic uterine contraction
Signs and Symptoms of Placenta Previa Cervical changes
Painless bright red bleeding Possible rupture of membrane
Recurrent and heavier as pregnancy progress Expulsion of cervical mucus plug
No uterine contraction Bloody show
ABRUPTIO PLACENTA
Risk Factors Causing Abruptio Placenta Missed Abortion:
Maternal age Retention of the conceptus in the uterus for a
Previous history of abruptio placenta clinically appreciable time after death of the
Multiparity embryo or fetus.
Smoking
Maternal hypertension (END OF SECOND PART)
Abdominal trauma
Signs and Symptoms of Abruptio Placenta Second and third trimester disorders
Concealed or visible bleeding
Painful bleeding Cervical Incompetence
Dark red bleeding - the inability of the cervix to support a
Board like abdomen pregnancy to term due to structural and or
Fetal distress functional weakness.
Tetanic contraction - painless and bloodless cervical dilatation
Management of Abruptio Placenta - premature cervical dilatation between 16 – 22
Bed rest weeks
Tocolytic Factors Causing IC
Steroids FUNCTIONAL:
Immediate Delivery premature triggering of the normal mechanism
Fluid and blood replacement of cervical dilatation and effacement.
Nursing Diagnosis of Abruptio Placenta Induction of ovulation
Altered Tissue Perfusion 3 or more prior fetal losses during the 2nd
Fluid Volume Deficit trimester
Risk for Infection CONGENITAL
Anxiety/Fear congenital or acquired
Acute pain Congenital:
Complications of Abruptio Placenta Weakness of the internal os
Hypovolemic shock Short hypoplastic cervix
Intrauterine growth restriction Bicornuate uterus
Placenta accreta Septate uterus
Maternal Mortality overzealous dilatation and curettage
Fetal Mortality cone biopsy
Congenital Anomalies cervical amputation
difficult delivery
PRETERM LABOR instrumentation
- Labor that begins after 20 weeks infection
gestation and before 37 weeks PATHOPHYSIOLOGY: (NOT INCLUDED)
gestation DIAGNOSIS:
Etiology of Preterm Labor • Dilators or balloons
Premature rupture of membrane • hysterosalpingograms
Preeclampsia • Digital examination of the cervix
Hydramnios • Sonography
Placenta previa MANAGEMENT:
Abruptio Placenta • Tocolytics
Incompetent cervix • Bed rest
Tauma • Hydration
Uterine structual anomalies • Progesterone
Multiple gestation • Trendelenburg position
Infection • Antibiotics
NURSING DIAGNOSIS: 24hr Urine
• Anxiety HELLP syndrome
• Risk for maternal injury Hemolysis
• Risk for fetal injury Elevated Liver function tests
• Knowledge Deficit Low Platelet count
• Anticipatory grieving COMPLICATIONS:
Eclamptic seizures
HYPERTENSIVE DISORDERS OF PREGNANCY HELLP syndrome
RISK FACTORS: Hepatic rupture
FIRST PREGNANCY DIC
MULTIPLE GESTATION pulmonary edema
POLYHYDRAMNIOS renal failure
HYDATIDIFORM MOLE placental abruption
MALNUTRITION cerebral hemorrhage
FAMILY HISTORY fetal demise
VASCULAR DISEASE MANAGEMENT OF PIH:
TYPES OF PREGNANCY INDUCE HYPERTENSION bed rest with or without BRP
Gestational Hypertension BP monitoring
Preeclampsia weight and urine checks
Eclampsia NST’s early
Chronic Hypertension US for IUGR
Superimposed Preeclampsia IVF
Gestational Hypertension Check for reflexes
* increased blood pressure Antihypertensive drugs
- systolic pressure of more than 130mm/Hg Anticonvulsant drugs
or +30mmHg from baseline Steroids
- diastolic pressure of more than 90mmHg Delivery of the baby
or +15mmHg from baseline MGSO4 THERAPHY
* edema Loading dose IV 4-6 g/20min
PREECLAMPSIA continued at 2 g/hr
Hypertension or PIH check for adverse effects
Proteinuria Respiratory rate<12/minute
Edema (wt gain) DTR of <1
MILD PREECLAMPSIA Urine output<30cc/hour
HYPERTENSION (140/90) POST-TERM PREGNANCY:
PROTEINURIA>300mg/24 hrs S&S
MILD EDEMA,signaled by wt gain Wt loss
(>2 lb/week or >6 lb/month) uterine size
URINE OUTPUT>500ml/24hrs Meconium in AF
SEVERE PREECLAMPSIA Risks
Any of the following symptoms: fetal mortality
BP>160/110 (2X, 6hrs apart, bedrest) cord compression
Proteinuria.5g/24 hours (3+ or 4+ dipstick) mec asp
Massive edema LGA shoulder dystocia CS
Oliguria <400ml/24 hrs episiotomy/laceration
IUGR in fetus depression
Systemic symptoms Treatment
SYSTEMIC SYMPTOMS: fetal surveillance
Pulmonary edema NST, CST, BPP Q wk
headache mom monitors mvmt
visual changes Induction
RUQ pain Pitocin (10-20U/L) @ 1-2
Liver Enzymes mU/min every 20-60 min
Thrombocytopenia DISORDERS OF AMNIOTIC FLUID:
ECLAMPSIA: Polyhydramnios
Hypertension S&S
Proteinuria uterine dist
Edema dyspnea
Seizure edema of lower extr
CHRONIC HYPERTENSION SUPERIMPOSED Treatment
PREECLAMPSIA therapeutic amniocentesis
hypertensive disorders before pregnancy Oligohydramnios
that progresses to preeclampsia Risks
(NOT INCLUDED) cord compression
musculoskeletal deformities
LABORATORY WORK-UPS: pulmonary hypoplasia
Blood--CBC, electrolytes, BUN, Creatinine Treatment
Liver function studies amnioinfusion
Coagulation studies
PREMATURE RUPTURE OF MEMBRANES: Treatment
Premature rupture of membranes (PROM) is a o Tocolytics
rupture (breaking open) of the membranes o IV hydration
(amniotic sac) before labor begins. If PROM o bedrest
occurs before 37 weeks of pregnancy, it is called o steroids, if needed
preterm premature rupture of membranes o abx, if needed
(PPROM). NURSING CARE:
WHAT CAUSES PREMATURE RUPTURE OF Assessment
MEMBRANES? Thorough hx
RUPTURE OF THE MEMBRANES NEAR THE END bleeding
OF PREGNANCY (TERM) MAY BE CAUSED BY A ROM
NATURAL WEAKENING OF THE MEMBRANES OR BPP (for PROM)
FROM THE FORCE OF CONTRACTIONS. BEFORE Teaching
TERM, PPROM IS OFTEN DUE TO AN INFECTION Infection Control
IN THE UTERUS. FMC
OTHER FACTORS THAT MAY BE LINKED TO Fetal Risk: Pre-maturity, infection
PROM INCLUDE THE FOLLOWING: *Prevention of infection
o LOW SOCIO ECONOMIC CONDITONS Monitor temp
o SEXUALLY TRANSMITTED INFECTIONS: Monitor amniotic fluid, you want white and
CHLAMYDIA AND GONORRHEA sticky – not black, green, smelly
o PREVIOUS PRETERM BIRTH Antibiotic within 24 hours and have c-sect
o VAGINAL BLEEDING MANAGEMENT:
o CIGARETTE SMOKING DURING Hospitalized – pre term, NICU, lungs, intubation
PREGNANCY (will be in NICU until Mother’s expected date of
o UNKNOWN CAUSES delivery)
In addition to a complete medical history and physical Limit sterile vaginal exam
examination, PROM may be diagnosed in several ways, Antibiotics
including the following: Bed rest
an examination of the cervix Trendelenberg position- to get pressure off
testing of the pH (acid or alkaline) of the fluid perineum
looking at the dried fluid under a microscope Daily CBC
ultrasound - a diagnostic imaging technique FACTOR MATERNAL FETAL OR NEONATAL
which uses high-frequency sound waves and a IMPLICATIONS IMPLICATIONS
computer to create images of blood vessels,
tissues, and organs. Ultrasounds are used to
view internal organs as they function, and to Social and Poor antenatal Low birth weight
assess blood flow through various vessels. Personal care Intrauterine growth
Possible Nursing Diagnoses: Low income Poor nutrition restriction (IUGR)
Risk for infection related to preterm rupture of level and/or ↑ risk
membranes without accompanying labor. low preecalmpsia
Knowledge deficit. educational
Anxiety related to outcome of labor. level
Risk for fetal injury related to preterm birth.
Management: Poor diet Inadequate Fetal malnutrition
bed rest either in the hospital or at home nutrition Prematurity
setting ↑ risk anemia
monitor for signs of infection such as fever, ↑ risk of
pain, increased fetal heart rate, and/or preeclampsia
laboratory tests.
giving the mother corticosteroids that may help Living at high ↑ hemoglobin Prematurity
mature the lungs of the fetus. altitude IUGR
avoid vaginal exams to prevent introduction of ↑ hemoglobin
microorganisms (polycythemia)
administer antibiotics
administer tocolytics to stop preterm labor.
prepare for possible immediate delivery. Factor Maternal Fetal & Neonatal
Premature Rupture of Membrane (PPROM – before 37 Implications Implications
weeks)
Spontaneous ROM prior to onset of labor at the
end of 37 weeks [high risk]
Full term = PROM [38 weeks] Multiparity ↑ risk antepartum Anemia
S&S >3 or postpartum Fetal death
o contractions hemorrhage
o cramps
o backache Weight Poor nutrition IUGR
o diarrhea <45.5 kg Cephalopelvic Hypoxia associated
o vag d/c (100 lb) disproportion with difficult labor &
o ROM Prolonged labor birth
Weight ↑ risk ↓ fetal nutrition Factor Maternal Fetal/Neonatal
>91 kg hypertension ↑ risk macrosomia Implications Implications
(200 lb) ↑ risk
cephalopelvic
disproportion
↑ risk diabetes Anemia: Iron-deficiency Fetal death
hemoglobin <9 anemia Prematurity
g/dL (white) Low energy Low birth
Age <16 Poor nutrition Low birth weight
<29% level weight
Poor antenatal ↑ fetal demise
hematocrit ↓ oxygen-
care
(white) carrying
↑ risk
<8.2 g/dL capacity
preeclampsia hemoglobin
↑ risk
(black)
cephalopelvic
<26%
disproportion
hematocrit
Age >35 ↑ risk ↑ risk congenital (black)
preeclampsia anomalies Hypertension ↑ vasospasm ↓ placental
↑ risk cesarean ↑ chromosomal ↑ risk central perfusion→
birth aberrations nervous system low birth
irritability weight
→ convulsions Preterm birth
↑ risk
Factor Maternal Fetal/Neonatal cerebrovascular
Implications Implications accident
↑ risk renal
damage
Smoking one ↑ risk ↓ placental Thyroid disorder ↑ infertility ↑
pack/day or hypertension perfusion →↓ O2 spontaneous
more ↑ risk cancer and nutrients abortion
available
Low birth weight Hypothyroidism ↓ basal ↑ risk
IUGR metabolic rate, congenital
Preterm birth goiter, goiter
myxedema
Use of ↑ risk poor ↑ risk congenital Hyperthyroidism ↑ risk Mental
addicting nutrition anomalies postpartum retardation →
drugs ↑ risk of ↑ risk low birth hemorrhage cretinism
infection with IV weight ↑ risk ↑ incidence
drugs Neonatal withdrawal preeclampsia congenital
↑ risk HIV, Lower serum Danger of anomalies
hepatitis C bilirubin thyroid storm
↑ incidence
Excessive ↑ risk poor ↑ risk fetal alcohol
preterm birth
alcohol nutrition syndrome
↑ tendency to
consumption Possible hepatic
thyrotoxicosis
effects with
long-term
consumption
Factor Maternal Fetal/Neonatal
Preexisting ↑ risk Low birth weight
Implications Implications
Medical preeclampsia, Macrosomia
Disorders hypertension Neonatal
Diabetes Episodes of hypoglycemia
mellitus hypoglycemia ↑ risk congenital Renal disease ↑ risk renal ↑ risk IUGR
and anomalies (moderate to failure ↑ risk preterm
hyperglycemia ↑ risk respiratory severe) birth
↑ risk cesarean distress syndrome
birth Diethylstilbestrol ↑ infertility, ↑ spontaneous
(DES) exposure spontaneous abortion
Cardiac Cardiac ↑ risk fetal demise
abortion ↑ risk preterm
disease decompensation ↑ prenatal mortality
↑ cervical birth
Further strain
incompetence
on mother’s
body
↑ maternal
death rate
Obstetric ↑ emotional or ↑ risk IUGR Factor Maternal Fetal/Neonatal
Considerations psychological ↑ risk preterm Implications Implications
Previous distress birth
Pregnancy
Syphilis ↑ incidence ↑ fetal demise
Stillborn
abortion Congenital
syphilis
Habitual ↑ emotional or ↑ risk abortion
abortion psychological
distress
Abruptio ↑ risk Fetal or
↑ possibility
placenta and hemorrhage neonatal
diagnostic
placenta previa Bed rest anemia
workup
Extended Intrauterine
hospitalization hemorrhage
Cesarean birth ↑ possibility ↑ risk preterm ↑ fetal demise
repeat cesarean birth
birth ↑ risk Preeclampsia or See ↓ placental
respiratory eclampsia hypertension perfusion
distress → low birth
weight
Factors Maternal Fetal/Neonatal
Multiple ↑ risk ↑ risk preterm
Implications Implications
gestation postpartum birth
hemorrhage ↑ risk fetal
Rh or blood ↑ financial Hydrops fetalis
↑ risk preterm demise
group expenditure for Icterus gravis
sensitization testing Neonatal anemia labor
Kernicterus
Hypoglycemia Elevated Increased Fetal death rate
hematocrit viscosity of 5 times normal
Large baby ↑ risk cesarean Birth injury >41% (white) blood rate
birth Hypoglycemia >38% (black)
↑ risk
gestational Spontaneous ↑ uterine ↑ risk preterm
diabetes premature infection birth
Current Congenital heart rupture of membranes
Pregnancy disease
Rubella (first Cataracts
trimester) Nerve deafness
Bone lesions MONITORING FETAL WELL-BEING
Prolonged virus • Early US for accurate gestational dating
shedding • US if macrosomia is suspected
• amniocentesis for fetal lung maturity
Rubella (second Hepatitis
• antepartum NST weekly p. 34 wks
trimester) Thrombocytopenia
PREGNANCY CATEGORY OF MEDICATIONS:
Cytomegalovirus IUGR • Category A--safe (vitamins)
Encephalopathy • Category B--no animal effects (penicillin)
• Category C--no studies available
Herpes virus Severe Neonatal herpes • Category D--evidence of risk but benefits
type 2 discomfort virus type 2 outweigh the risks
Concern about 2% hepatitis with • Category X--risks outweigh benefits
possibility of jaundice
cesarean birth, Neurologic (END OF 3RD PRESENTATION)
fetal infection abnormalities
NURSING CARE OF THE CLIENT WITH HIGH RISK LABOR
& DELIVERY AND HER FAMILY
ESSENTIAL FACTORS IN LABOR:
1. PASSENGER
a. FETUS-
b. PLACENTA
2. PASSAGEWAY
3. POWERS
a. primary power
b. secondary power
4. POSITION OF THE MOTHER
5. PSYCHE
PROBLEMS WITH THE PASSENGER THE FONTANELLES
PASSENGER:
• FETUS
o fetal skull
o fetal body size
o fetal presentation
o fetal position
o fetal lie
ANTEROPOSTERIOR DIAMTERE:
MOULDINGS:
MEMBRANE SPACES
Synclitism & Asynclitism:
• Asynclitic refers to a fetal head that is not
parallel to the anteroposterior plane of the
pelvis.
• The head is synclitic when the sagittal suture
lies midway between the symphysis pubis and
the sacral promontory.
FETAL MALPRESENTATION
VERTEX MALPRESENTATION
1. BROW PRESENTATION
2. FACE PRESENTATION
Risk of Brow Presentation
longer labor
ineffective contraction
slow or arrest fetal descent
cesarean delivery
neonatal neck and cerebral compression
damage to the neonatal larynx and trachea
neonatal facial edema and bruises
Management of Brow Presentation
monitor for CPD
left or right mediolateral episiotomy
cesarean delivery
Risk of Face Presentation
increase risk of CPD
prolongation of labor
increase risk of infection
Cesarean birth
neonatal cephalhematoma
edema of neonatal face and throat
pronounced molding
Management of Face Presentation
vaginal birth may be anticipated if not CPD,
reassuring fetal heart pattern, and labor pattern
is effective
cesarean birth if mentum remains posterior
Risk of Breech Presentation
higher perinatal morbidity and mortality rate
cord prolapsed
neonatal cord injury due to hyperextension
birth trauma especially the head
Management of Breech Presentation
external cephalic version at 36 – 38 weeks or
prior to labor
method of delivery depends on:
gestational age
FETAL MALPOSITION presence of other fetuses
Persistent Occiput Posterior EFW
fetus enters the birth canal, descends, and is types of breech presentation
delivered in occiput posterior position and physician’s preferences
fetus is facing up instead of facing down as it Shoulder Presentation
enters the vagina Fetus is in a transverse lie
Transverse Occiput Arrest ETIOLOGY OF FLUPP
baby is head-down but the head is turned Fetal
completely sideways towards the mother’s prematurity
hipbone, causing baby to ‘arrest’ (get stuck)
multiple
because it doesn’t fit well.
anomalies: often those that restrict the ability
Factors Causing POP
of the fetus to assume a vertex presentation
lack of rotation due to poor contraction
major malformation:hydrocephaly,
abnormal flexion of the head
anencephaly, meningomyemocoele
incomplete rotation
most common malformation:congenital
inadequate maternal pushing effort
dislocation of the hip
epidural anesthesia
Liquor
large baby
Risk of Fetal Malposition oligohydramnios/polyhydramnios
prolonged labor Uterine
third to fourth degree perineal lacerations anomalies (bicornuate, fibroid)
extension of midline episiotomy Placenta
forceps/vacuum assisted or caesarean delivery Previa
Management of Fetal Malposition Pelvis
monitoring on fetal and maternal status contracture, pelvic tumors obstructing birth
cesarean birth if necessary canal
Scanzoni’s maneuver Management of Shoulder Presentation
Forceps assisted expectant – fetus may change presentation
Vacuum assisted without intervention if discovered before term
Regional anesthesia external cephalic version if evident at 37 weeks
cesarean delivery if unsuccessful
Compound Presentation Amnionitis
There are two presenting part Maternal Hyperthyroidism
COMPOUND: Fetal Anemia
• baby's hand presents alongside its head Fetal Bradycardia
(sometimes called a 'nuchal hand'), making a late/profound fetal hypoxia
larger size that has to go through the pelvis; Maternal Hypotension
many of the same symptoms as other Umbilical cord compression
malpositions. Vagal Stimulation
• One other variation of this is when the baby's Fetal Arrhythmia
arm or elbow is across its face ('nuchal arm'), Uterine hyperstimulation
which can cause intense pain.
Abruptio Placenta
• A baby can be born with a nuchal hand
Uterine Rupture
alongside its head, although the process is
Variability
usually slow.
a measure of interplay (push-pull effect)
VERSION:
between the sympathetic and parasympathetic
• Turning of the fetus.
nervous system
• is a procedure used to change the fetal
two abnormal variability:
presentation by abdominal or intrauterine
manipulation. Decreased variability
External Cephalic Version (ECV) Increased variability
most common wherein the fetus is changed Decreased Variability
from a breech to a cephalic presentation Hypoxia
Podalic Version- Acidosis
less common type CNS depressant agents
used only with the 2nd fetus during a vaginal Fetal sleep
twin birth and only if the twin does not descend < 32 weeks fetus
readily or if the heart rate is non-reassuring. Fetal anomalies
medication is used to relax the uterus Previous neurologic insult
The OB places a hand inside the uterus, grabs Tachycardia
the fetus’s feet and draws them down thru the Increased Variability
cervix. Early mild hypoxia
Contraindications of Versions: Fetal stimulation or activity
3rd trimester bleeding Alteration in placental blood flow
uterine anomalies Fetal Heart Acceleration
ROM, oligohydramnios tansient increase of FHT normally caused by
need for CS for other reasons (placenta previa, fetal movements
contracted pelvis, hyperextended head) indicates fetal well being
indicated vaginal delivery (fetal death) no accelerations is an ominous sign
Fetal Heart Deceleration
(END OF 4TH PART) periodic decrease of FHT from its baseline rate
three types:
FETAL DISTRESS o Early deceleration
Compromise of the fetus during the antepartum o Late deceleration
period or intrapartum period o Variable deceleration
Fetal hypoxia (NOT INCLUDED) – 3 types
Criteria in Determining Signs of Fetal Distress Fetal Movements
Fetal Heart Rate: at least 10x in 3 hours
Baseline rate affected by:
Variability o fetal sleep
Accelerations of Fetal Heart rate Decelerations o sound
Fetal Movements/Activities o time of day
Meconium Staining o blood glucose level
Fetal Stimulation o cigarette smoking
Fetal Scalp Blood Sampling o Drugs
Fetal Oxygen Saturation o Oxygenation status
Fetal Heart Rate less than 10 movements in 3 hours or absent
A. Baseline Rate movement are ominous
average FHR observed during a 10-minute (MECONIUM STAINING – NOT INCLUDED)
period of monitoring
normal rate ranges from 110 – 160 bpm Fetal Stimulation
two abnormal baseline: fetus should response by fetal heart
o Fetal tachycardia accelerations
o Fetal Bradycardia o Fetal scalp stimulation
Fetal Tachycardia applying pressure to fetal scalp by
early fetal hypoxia gently stroking or massaging it for 15
Maternal fever seconds while doing vaginal
Maternal Dehydration examination
Beta-sympathomimetic drugs o Vibroaccoustic stimulation
Fetal Blood Scalp Sampling
acid-base status of fetus
must be done when:
o RBOW
o 2-3 cms cervical dilatation
o station -2 and below
must not done when:
o FHR pattern are ominous
o acute emergencies
o vaginal bleeding
normal during labor is above 7.25 pH
pH 7.2 – 7.25 is borderline
below 7.2 is non reassuring and necessitate
birth SIGNS:
Fetal Oxygenation Saturation (FSpO2) Ill-fitting or non-engaged presenting
40% - 70% are considered reassuring part
30% - 40% mild acidosis and requires Prolapsed umbilical cord
continuous monitoring umbilical cord visualized in
below 30% indicates hypoxia and requires vagina or at vulva
immediate birth umbilical cord palpated on
Factors Causing Fetal Distress pelvic exam
Breathing problems Fetal distress on Fetal Heart Tracing
Abnormal position and presentation of the May follow rupture of
fetus membranes
Multiple births PROGNOSIS:
Shoulder dystocia High perinatal mortality for delayed delivery
Umbilical cord prolapse >40 min
Nuchal cord RISK FACTORS:
Placental abruption Premature rupture of the amniotic sac
Premature closure of the fetal ductus Polyhydramnios
arteriosus Long umbilical cord
Fetal Distress Management Fetal malpresentation
continuous fetal monitoring Multiparity
Oxytocin if indicated Multiple gestation
discontinue oxytocin if with prolonged late Placenta previa
decelerations Intrauterine tumors
intrauterine fetal resucitations: A small fetus
left lateral position CPD
Oxygen administration DIAGOSTICS:
Hydration A pelvic examination can also be conducted by a
fetal stimulation physician and may see the prolapsed cord, or
prepare for immediate delivery palpate (feel) the cord with the fingers.
NURSING DIAGNOSIS: Cardiotocograph ( Electronic Fetal Monitoring)
Decreased Cardiac Output (fetal) Ultrasound
Impaired Gas Exchange (fetal) (PATHOPHYSIOLOGY – NOT INCLUDED)
Ineffective Tissue Perfusion (fetal) NURSING DIAGNOSIS:
Risk for fetal injury Impaired Gas Exchange (fetal)
Anxiety (maternal) Risk for Injury (fetal)
Deficient Knowledge (maternal) Fear (maternal)
UMBILICAL CORD PROLAPSE Anxiety (maternal)
A rare, obstetrical emergency that occurs when Deficient Knowledge (maternal)
the umbilical cord descends alongside or Umbilical Cord Prolapse Management
beyond the fetal presenting part. Initial management of cord prolapse in hospital
TYPES OF UMBILICAL CORD PROLAPSE: setting:
Overt Prolapse • immediate delivery
Refers to protrusion of the cord • minimal handling of loops of cord lying outside
in advance of the fetal the vagina.
presenting part, often through To prevent cord compression, the presenting part MUST
the cervical os and into or BE elevated:
beyond the vagina. • knee–chest position or head-down
Occult Prolapse • tilt (preferably in left-lateral position).
Occurs when the cord descends • Tocolysis
alongside, but not past, the Optimal mode of delivery with cord prolapse:
presenting part. • category 1 caesarean section
• Category 2 caesarean section
Vaginal birth, in most cases operative,
can be attempted at full dilatation
A practitioner competent in the
resuscitation of the newborn should
attend all deliveries with cord Antenatal risk factors
prolapse. • Mother’s birthweight >90th centile
Management in community setting: • Maternal obesity or massive weight gain
• assume the knee–chest face-down position • Diabetes mellitus—can be despite seemingly
while waiting for hospital transfer. good blood sugar
• Transport woman to nearest consultant-led control
institution • Prolonged pregnancy (beyond 42 completed
• Left lateral position during transport weeks)
• Elevate presenting part • Previous shoulder dystocia (10% risk of
UMBILICAL CORD ABNORMALITIES recurrence) or large baby
• Velamentous insertion of the cord • Recognized macrosomia this pregnancy.
• Umbilical cord compression
• Umbilical cord prolapse
• Hypercoiling of the cord PROBLEMS WITH THE POWERS
• Cord Coil
Velamentous Insertion of the Cord DYSTOCIA:
• Condition where the umbilical cord joins the General information:
placenta at the edge, rather than the typical Any labor or delivery that is prolonged and
insertion in the center. difficult.
Usually results form a change in the
interrelationships among the
PROBLEMS WITH THE PASSAGEWAY 5 Ps (factors in labor and delivery):
>passenger
CEPHALOPELVIC DISPROPORTION >passage
Disproportion of fetal head and mother’s pelvis >powers
CAUSES: >placenta
increased fetal weight >psyche of mother.
fetal position Cesarean birth is needed if disproportion is
problems with the pelvis great.
problems with the genital tract Problems with presentation: any
S/S: presentation unfavorable for delivery (e.g.
• the delivery of the baby is obstructed breech, shoulder , face, transverse lie.
• The labor is prolonged Posterior presentation that does not rotate
(PATHOPHYSIOLOGY – NOT INCLUDED) or cannot be rotated with ease.
DIAGNOSTICS: 1. Problems with maternal soft tissue
Estimation of the size of the pelvis: A full bladder may impede the progress of labor,
Clinical Pelvimetry as can myomata uteri, cervical edema, scar
Radiologic Pelvimetry tissue, and congenital anomalies.
Estimation of fetal size Emptying the bladder may allow labor to
MANAGEMENT: continue; the other conditions may necessitate
CESAREAN SECTION caesarean birth.
NURSING DIAGNOSIS: 2. Dysfunctional uterine contractions
• Anxiety Contraction may be too weak, too short, too far
• Fatigue apart, ineffectual
• Risk for fetal injury Classification
• Risk for impaired skin integrity A.) Primary: inefficient pattern present from
• Situational low self- esteem beginning of labor; usually prolonged latent phase.
INTERVENTIONS: B.) Secondary: efficient pattern that changes to efficient
• Monitor heart sounds and uterine contractions or stops; may occur in any stage.
continuously, if possible, during trial labor. Assessment findings:
• Urge the woman to void every 2 hours s Progress of labor is slower than expected rate
• Assess FHR carefully of dilatation, effacement, descent for specific
• Establish a therapeutic relationship, conveying client.
empathy and unconditional positive regard Length of labor prolonged; prolonged latent
• Instruct in methods to conserve energy phase (>20 hrs in nullipara pt. or >4 h in a
• Massage bony prominences gently and change multipara pt), protacted active phase dilatation
position on bed in a regular schedule np. <1-2cm, mp <1.5cm; protacted descengt <1
• Convey confidence in client’s ability to cope cm per hr change in station in the nullipara pt.
with current situation or <2 cm per hour in the mp pt.
SHOULDER DYSTOCIA: Maternal exhaustion/ distress
Incidence: about 0.2–1%. Fetal distress
This is one of the most frightening obstetric Arrest of descent: no progress in fetal station
emergencies greater than 1 hour
It occurs when the fetal shoulders fail to negotiate Nursing intervention:
the pelvic inlet Individual as to cause
Prompt (but not forcible) action is required to Provide comfort measures for client
prevent fetal Provide client, supportive descriptions of all
morbidity or mortality (see Stirrat and Taylor in actions taken
‘Further reading’) Administer analgesia if ordered
Monitor mother/ fetus continuously Powerlessness
Pathophysiology: (DIAGRAM NOT INCLUDED) Provide rest period
Relaxation technique
PREDISPOSING FACTORS: Support person
• Genetic Deficient knowledge related to measures that can be
• Overweight used to enhance labor and facilitate birth.
• Multiple gestation Teach proper breathing techniques used during
• Hydramnios labor
• Maternal fatigue Educate about the complication of the delivery
• Pelvic malformation Explain client that caesarean is necessary due to
• Inappropriate timing of analgesic and difficult labor.
anaesthetic administration Ineffective individual coping related to inadequate
• Gestational DM support system.
• STDs Support mechanism:
• Other diseases Stay with the patient during labor process
PRECIPITATING FACTORS: Encourage patient to discuss about her
• Malpresentation and malposition of the fetus condition
• Congenital malformation of the uterus
• Over stimulation with oxytocin DYSFUNCTIONAL LABOR:
• CPD • Possible Causes:
• Fetal anomalies such as neural tube defects, • Catecholamines (response to
large tumor, and gross ascites anxiety/fear), increase
Signs/ symptoms: physical/psychological stress, leads to
Pain myometrial dysfunction; painful &
Increase heart rate, pulse, body temp. ineffective labor.
Increased BP • Premature or excessive analgesia,
Diaphoresis particularly during latent phase.
Body weakness • Maternal factors.
Exhausted appearance • Fetal factors.
SOB • Placental factors.
Nasal flaring • Physical restrictions (position in bed).
Anxiety ASSESSMENT:
Restlessness • Antepartal history.
Vaginal hemorrhage • Emotional status.
Medical Management: • Vital signs, FHR.
1. Treatment for contraction abnormalities • Contraction pattern (frequency, duration,
involves stimulation of labor through the use of intensity).
oxytocin. An intrauterine pressure catheter may • Vaginal discharge.
be used. GOAL = to minimize physical/psychological stress during
2. Management for maternal passageway or fetal labor/birth. Emotional support.
passage problems involves delivery in the safest
manner for the mother and fetus. DYSFUNCTIONAL LABOR PATTERN:
If the problem is related to the inlet or • Hypertonic labor
midpelvis, a CS delivery is indicated. • Hypotonic labor
If the size of the outlet is the problem, a • Precipitate labor level
forceps or vacuum extraction maybe HYPERTONIC DYSFUNCTION:
perform. • Increased resting tone of uterine myometrium;
Surgical Management: diminished refractory period; prolonged latent
1. Caesarean in necessary for delivery of the fetus phase.
• Nullipara: more than 20 hours.
NURSING DIAGNOSIS: • Multipara: more than 14 hours.
Acute pain related difficulty in labor. • Etiology: unknown. Theory – ectopic initiation
Promoting comfort: of incoordiante uterine ctx.
Relaxation technique such as breathing • Assessment:
techniques during labor • Onset (early labor)
Changing position • Contractions:
Support person • Continuous fundal tension,
Pain medications incomplete relaxation.
Anxiety related to threat of change in health status of • Painful.
self and fetus. • Ineffectual – no effacement or
Decreasing anxiety: dilation.
Give brief explanation to the women about the • Signs of fetal distress:
nature of contraction associated with induce • Meconium-stained fluid.
labor • FHR irregularities.
Provide anticipatory guidance regarding use of • Maternal VS.
meds, procedures and equipment. • Emotional status.
Prepare for caesarean if necessary • Medical evaluation: to rule out CPD.
• Vaginal examination, x-ray
pelvimetry, ultrasonography.
INTERVENTIONS: -Preterm labor is always serious because if it
• Short-acting barbiturates (to encourage rest, results in infant’s birth, the infant may be
relaxation). immature.
• IV fluids (to restore / maintain hydration & ASSESSMENT:
fluid-electrolyte balance). During tocolytic therapy, assess the following:
• If CPD – c/s. • Fetal status by electronic fetal monitoring
• Provide emotional support. • Uterine activity pattern
• Provide comfort measures. • Respiratory status
• Prevent infection (strict aseptic technique). • Muscular tremors
• Prepare patient for c/s if needed. • Palpitations
• Dizziness
HYPOTONIC DYSFUNCTION: • Lightheadedness
• After normal labor at onset, ctx diminish in • Urinary output
frequency, duration, & strength. • Patient education to S/Sx of PTL
• Lowered uterine resting tone; cervical • Patient education to S/Sx of infection
effacement & dilation slow / cease. RISK FACTORS:
• Etiology: • Race: African-American women
• Premature or excessive analgesia / • Age: Adolescents
anesthesia (epidural, spinal block). • Those with inadequate prenatal care
• CPD. • Those who continue to work at strenuous jobs
• Overdistention (hydramnios, fetal during pregnancy
macrosomia, multifetal pregnancy). • Those who have shift works that leads to
• Fetal malposition / malpresentation. extreme fatigue
• Maternal fear / anxiety. Signs and Symptoms:
• Assessment: • Persistent, dull, low backache
• Onset (latent phase & most common in • Vaginal spotting
active phase). • A feeling of pelvic pressure (abdominal
• Contractions - normal previously, will tightening)
demonstrate: • Menstrual-like cramping
• Decreased frequency. • Vaginal discharges
• Shorter duration. • Uterine contractions
• Diminished intensity (mild to • Intestinal cramping
moderate). • Feeling that baby is “pushing down” or that
• Less uncomfortable. “something” is in the vagina
• Cervical changes – slow or cease. Nursing Diagnosis & Interventions:
• Signs of fetal distress – rare. Anxiety r/t medication and fear of outcome of
• Usually late in labor d/t pregnancy
infection secondary to Know the C/I and potential complications of
prolonged ROM. tocolytic therapy
• Tachycardia. Explain the purpose and common A/E of
• Maternal VS (elevated temperature) – tocolytic therapy
may indicate infection. Provide accurate information on the status of
• Medical diagnosis – procedures: vaginal the fetus and labor (contraction pattern).
examination, x-ray pelvimetry, Allow the woman and her support person to
ultrasonography. To rule out CPD (most verbalize their feelings regarding the episode of
common cause). PTL and the treatment.
• Management: If a private room is not used, do not place the
• Amniotomy (artificial ROM). woman in a room with a woman who is in labor
• Oxytocin augmentation of labor. or who has lost an infant.
• If CPD, prepare for c/s. Situational Low Self-Esteem r/t Inability to carry
• Emotional support, comfort measures, pregnancy
prevent infection. Provide support persons because she is apt to
PRECIPITATE LABOR: be more concerned than the average person
• Labor that progresses rapidly and ends with the about labor.
delivery occurring less than 3 hours after the Encourage expression of feelings and anxieties
onset of uterine activity. to facilitate coping with actual situation.
• Rapid labor and delivery. Provide frequent assurance during labor that
PRETERM LABOR: she is breathing well with contractions and
-Labor that occurs before the end of the thirty- continue until postpartum period because she
seventh week of gestation. It occurs may not be mentally prepared for the labor
approximately 9%- 11% of pregnancies. Any because it has come unexpectedly.
woman having persistent uterine contractions Comment on strengths of the family unit.
(4 very 20 min) should be considered to be in Convey confidence in client’s ability to cope
labor. A woman is documented as being in with current situation.
actual labor rather than having false labor Risk for Fetal Injury r/t Preterm Birth
contractions if she is having uterine Monitor fetal status and labor problems.
contractions that cause cervical effacement Assess WBC count frequently. A count of
over 80% and dilation over 1cm. 18,000-20,000/mm3 suggests infection.
Reassure misconceptions about difficulty of Genetic counseling for those with a history of
labor after preterm rupture of the membranes genetic disease/ a previously affected
(dry labor) since amniotic fluid is always being pregnancy.
formed so there is no such thing as dry labor Antepartum Treatment
Encourage the woman to assume positions that Educate mother regarding S/Sx of PTL.
will enhance placental perfusion. Instruct mother and provide resources for
Assist with delivery of infant as needed. lifestyle modifications.
Risk for Injury Secondary to Tocolytic therapy o If mother smokes, encourage smoking
Maintain accurate I/O at least every hour. Limit cessation classes.
intake to 2,500mL/day. o Ensure mother has a healthy diet and
Assess maternal VS. adequate maternal weight gain during
Notify Physician if maternal pulse is greater pregnancy.
than 120 bpm. Initial treatment for a patient who is at risk for
Assess for S/Sx of pulmonary edema. PTL is the use of bed rest in a left lateral
Educate woman on tocolytic therapy, explaining position with continuous monitoring of fetal
the purpose and common A/E. status and uterine activity.
Compromised Family Coping Secondary to Hydration with IV fluids, with careful
Hospitalization assessment of I/O and auscultation of lungs to
Encourage private time for woman and partner. assess for the development of pulmonary
Encourage family members to verbalize feelings edema.
openly and clearly. If this stops the contractions, tocolytic therapy
Allow visitation with other children as tolerated is not needed.
by the woman. (PATHOPHYSIOLOGY – NOT INCLUDED)
Comment on strengths of the family unit.
Promote assistance of family in providing client UTERINE PROLAPSE (Uterine Prolapse/Pelvic
care as appropriate. relaxation/Pelvic floor hernia)
Medical Management: • a descent or herniation of the uterus into or
• Antibiotics beyond the vagina
• Prostaglandin Inhibitors • considered under the broader heading of
Indomethacin (Indocin) "pelvic organ prolapse" which also includes
• Calcium Channel Blockers cystocele, urethrocele, enterocele, and
Nifepidine (Procardia) rectocele.
• Corticosteriods • anatomically, the vaginal vault has 3
Betamethazone 12 mg IM q 24 hrs 2 compartments:
doses an anterior compartment (consisting of the
Dexamethazone 6 mg IM q 12 hrs 4 anterior vaginal wall)
doses - a middle compartment (cervix)
• Magnesium sulfate posterior compartment (posterior vaginal
• Beta-sympathomimetic drugs wall).
Ritodrine hydrochloride (yutopar) • UP involves the middle compartment
Terbutaline (brethine) Four stages of uterine prolapse are defined:
Surgical Management: stage I - descent of the uterus to any point in
Cesarean Section the vagina above the hymen
stage II - as descent to the hymen
NURSING MANAGEMENT: stage III - as descent beyond the hymen
• Hydration (Oral or IV) stage IV - as total eversion or procidentia
• Bedrest (Home or Hospital), usually left side ∆ Uterine prolapse always is accompanied by
lying some degree of vaginal wall prolapsed.
• Medications to stop labor (Magnesium sulfate,
brethine, terbutaline, etc.) ASSESSMENT:
• Medication to help prevent infection (More • A complete pelvic examination is required,
likely if your membranes have ruptured or if the including a rectovaginal examination to assess
contractions are caused by infection) sphincter tone.
• Evaluation of your baby. Biophysical profile, • A Sims speculum or a standard bivalve
non-stress or stress tests speculum with the anterior blade removed may
• Medications to help your baby's lung develop facilitate diagnosis.
more quickly • Physical findings may be enhanced by having
Preconception Care the patient strain during the examination or by
Baseline assessment of health and risks with having her stand or walk prior to examination.
advice to decrease the risks attributable to Standing with an empty bladder may result in a
preterm labor/PTB. 1-2 stage difference in the degree of prolapse
Pregnancy planning and identification of noted on examination when compared to a
barriers to care. supine position with a full bladder.
Adjustment of prescribed and OTC that may • Mild uterine prolapse may be recognized only
pose a threat to the developing fetus. when the patient strains during the bimanual
Advise to improve maternal nutrition. examination.
Screening for and treatment of diseases. • Evaluate all patients for estrogen status.
• Signs of decreased estrogens
• Loss of rugae in the vaginal o + colpopexy - involves the use of
mucosa surgical mesh for supporting the uterus
• Decreased secretions o + hysterectomy – removal of uterus
• Thin perineal skin NURSING MANAGEMENT:
• Easy perineal tearing • preventive measures:
• Physical examination should also be directed Early visits to HC provider = early
toward ruling out serious conditions that may detection
rarely be associated with uterine prolapse, such Teach Kegel’s exercises during PP
as infection, urinary outflow obstruction with period
renal failure, and hemorrhage. • preoperative nursing care:
• If urinary obstruction is present, the Thorough explanation of procedure,
patient may exhibit suprapubic expectation and effect on future sexual
tenderness or a tympanitic bladder. f(x)
• If infection is present, purulent cervical Laxative and cleansing edema
discharge may be noted. (rectocele) – independently, at home a
LABORATORY STUDIES: day prior procedure
• Laboratory studies are unnecessary in Perineal shave prescribed also
uncomplicated cases…. Lithotomy position for surgery
• Cervical cultures - cases complicated by • postop nursing care:
ulceration or purulent discharge Pt. is to void few hours after surgery;
• Papanicolaou test (Pap smear cytology) or catheter if unable (after 6 hrs)
biopsy - in rare cases of suspected carcinoma NURSING DIAGNOSIS:
• BUN and creatinine measurement - if PE PAIN
findings suggest urinary obstruction o Administer analgesic as prescribed.
IMAGING STUDIES: o Provide comfort measures such as backrub.
• Pelvic ultrasound examination o Provide diversional activities such as guided
• Ultrasonography
imagery and socialization.
• MRI - to grade pelvic organ prolapse
SIGNS AND SYMPTOMS: CONSTIPATION
• Pelvic heaviness or pressure o Administer stool softeners/laxatives as
• Protrusion of tissue: A patient who reports of a prescribed.
"bulge" has been found to be a valuable o Encourage increase in fluid and fiber intake.
screening tool for the detection of pelvic organ o Encourage early ambulation.
prolapse (81% PPV, 76% NPV).
• Pelvic pain URINARY INCONTINENCE
• Sexual dysfunction, including dyspareunia, o Determine if client is aware of incontinence.
decreased libido, and difficulty achieving Developmental issues/ medical conditions
orgasm that can impair patient’s awareness and
• Lower back pain sensory perception of voiding.
• Constipation o Determine patient’s particular symptoms
• Difficulty walking (e.g. continuous dribbling).
• Difficulty urinating o Implement bladder training for
• Urinary frequency incontinence management by providing
• Urinary urgency ready acces to bathroom or commode,
• Urinary incontinence encouraging adequate fluid intake, and
• Nausea establishing voiding/bladder emptying.
• Purulent discharge (rare)
• Bleeding (rare) SEXUAL DYSFUNCTION
• Ulceration (rare) o Provide factual information about individual
(PATHOPHYSIOLOGY NOT INCLUDED) condition involved to promote informed
decision making.
COMPLICATIONS: o Provide for ways to obtain privacy to allow
• Urinary retention for sexual expression for individual and/or
• Constipation between partners with out embarrassment
• Hemmorhoids and/or objection of others.
• Cervical ulceration o Establish therapeutic nurse-client
• Infection (possible) relationship to promote treatment and
• Cystitis facilitate sharing of sensitive information.
TREATMENT/MEDICAL MANAGEMENT: RISK FOR INFECTION
• Pessaries o Observe for localized signs of infection.
o + fitted into the vagina to hold the o Note for signs and symptoms for sepsis.
uterus in place o Stress proper hand hygiene.
o + temporary or permanent form
o + fitted individually for each woman UTERINE RUPTURE
o + attaining and maintaining optimal spontaneous or traumatic rupture of the uterus
weight is recommended ie., the actual separation of the uterine
• Surgery myometrium/ previous uterine scar, with
o + uterus sutured back into place & rupture of membranes and extrusion of the
fetus or fetal parts into the peritoneal cavity.
Dehiscence - partial separation of the old NURSING DIAGNOSIS WITH INTERVENTIONS:
uterine scar; DEFICIENT FLUID VOLUME:
- the fetus usually stays inside the uterus and Start or maintain an IV fluid as prescribed. Use a
the bleeding is minimal when dehiscence large gauge catheter when starting the IV for
occurs. blood and large quantities of fluid replacemnt.
RISK FACTORS: Maintain CVP and arterial lines, as indicated for
• Women who have had previous surgery on the hemodynamic monitoring.
uterus (upper muscular portion) Maintain bed rest to decrease metabolic
• Having more than five full-term pregnancies demands.
• Having an overdistended uterus (as with twins Insert Foley catheter, and moniter urine output
or other multiples) hourly or as indicated.
• Abnormal positions of the baby such as Obtain and administer blood products as
transverse lie. indicated.
• Use of Pitocin (oxytocin) and other labor- FEAR
induced medications (prostaglandin) Give brief explanation to the woman and her
• Rupture of the scar from a previous CS support person before beginning a procedure.
delivery/hysterectomy. Answer questions that the family or woman
• Uterine/abdominal trauma may have.
• Uterine congenital anomaly Maintain a quiet and calm atmosphere to
• Obstructed labor; maneuvers within the uterus enhance relaxation.
• Interdelivery interval (time between deliveries) Remain with the woman until anesthesia has
(PATHOPHYSIOLOGY NOT INCLUDED) been administered; offer support as needed.
Keep the family members aware of the situation
ASSESSMENT: while the woman is in surgery and allow time
evaluate maternal vital signs for them to express feelings.
note an increase in rate and depth of DECREASED CARDIAC OUTPUT
respirations, an increase in pulse , or a drop in Administer supplemental oxygen, blood/fluid
BP indicating status change replacement, antibiotics, diuretics, inotropic
assess fetal status by continuous monitoring drugs, antidysrhythmics, steroids,
speak with family, and evaluate their vassopressors, and/or dilators as ordered.
understanding of the situation Position HOB flat or keep trunk horizontal while
observe for signs and symptoms of impending raising legs 20 to 30 degrees in shock situation
rupture Activities such as isometric exercises, rectal
-lack of cervical dilatation stimulation, vomiting, spasmodic coughing
-tetanic uterine contractions which may stimulate Valsalva response should
restlessness be avoided; administer stool softener as
anxiety indicated.
severe abdominal pain INEFFECTIVE TISSUE PERFUSION
fetal bradycardia Administer O2 using a face mask at 8-12 L/min
late or variable decelerations of the or as ordered to provide high oxygen
FHR) concentration.
SIGNS AND SYMPTOMS: Apply pulse oximeter, and monitor oxygen
CLINICAL MANIFESTATIONS: saturation as indicated.
Developing Rupture Monitor ABG levels and serum electrolytes as
Abdominal pain and tenderness indicated to assess respiratory status, observing
Uterine contractions will usually continue but for hyperventilation and electrolyte imbalance.
will diminish in intensity and tone. Continually monitor maternal and fetal vital
Bleeding into the abdominal cavity and signs to assess pattern because progressive
sometimes into the vagina. changes may indicate profound shock.
Vomiting RISK FOR INFECTION
Syncope; tachycardia; pallor Observe for localized signs of infection.
Significant change in FHR characteristics – Cleanse incision or insertion sites daily and PRN
usually bradycardia (most significant sign) with povidone iodine or other appropriate
Violent Traumatic Rupture solutions.
Sudden sharp abdominal pain during or Change dressings as needed or indicated.
between contractions. Encourage early ambulation, deep breathing,
Abdominal tenderness coughing and position changes.
Uterine contractions may be absent, or may Maintain adequate hydration and provide.
continue but be diminished in intensity and Provide perineal care.
cord MEDICAL MANAGEMENT:
bleeding vaginally, abdominally, or both • Immediate stabilization of maternal
Fetus easily palpated in the abdominal with hemodynamics and immediate caesarean
shoulder pain delivery
Tenses, acute abdominal with shoulder pain • Oxytocin is given to contract the uterus and the
Signs of shock replacement .
Chest pain from diaphragmatic irritation due to • After surgery, additional blood, and fluid
bleeding into the abdomen. replacement is continued along with antibiotic
theory.
SURGICAL MANAGEMENT:
• Caesarean Section
• Laparotomy
• Hysterectomy
NURSING MANAGEMENT:
• Continually evaluate maternal vital signs; Oligohydramnios Maternal fear ↑ Incidence of
especially note an increase in rate and depth of of “dry birth” congenital anomalies
respirations, an increase in pulse , or a drop in ↑ Incidence of renal
BP indicating status change. lesions
• Assess fetal status by continuous monitoring. ↑ Risk of IUGR
• Speak with family, and evaluate their ↑ Risk of fetal
understanding of the situation. acidosis
• Anticipate the need for an immediate caesarean ↑ Risk of cord
birth to prevent rupture when symptoms are compression
present. Postmaturity
• Provide information to the support person and Meconium staining ↑ ↑ Risk of fetal
inform him or her about fetal outcome, the of amniotic fluid Psychologic asphyxia
extent of the surgery and the woman’s safety. stress due to ↑ Risk of meconium
• Let the pt express her emotion without feeing fear for baby aspiration
threatened. ↑ Risk of pneumonia
due to aspiration of
meconium
PROBLEMS WITH THE PSYCHE
Factors that may affect the woman’s psyche during Premature rupture ↑ Risk of ↑ Perinatal
labor include the woman’s: of membranes infection morbidity
Current pregnancy experience (chorioamnio Prematurity
Unplanned versus planned pregnancy nitis) ↑ Birth weight
Amount of difficulty conceiving ↑ Risk of ↑ Risk of respiratory
Presence of risk factors preterm labor distress syndrome
Complications of pregnancy ↑ Anxiety Prolonged
Previous birth experiences Fear for the hospitalization
Complications of delivery baby
Mode of delivery (cesarean versus vaginal) Prolonged
Birth outcomes (e.g., fetal demise, birth hospitalizatio
defects) n
Expectations for current birth experience ↑ Incidence
View of labor as a meaningful or a stressful of tocolytic
event therapy
Realistic and attainable goals versus
Induction of labor ↑ Risk of Prematurity if
idealistic views that conflict with reality (a
hypercontrac gestational age not
situation that can lead to disappointment)
tility of assessed correctly
Preparation for birth
uterus Hypoxia if
Type of childbirth preparation ↑ Risk of hyperstimulation
Familiarity with institution and its policies uterine occurs
and procedures rupture
Type of relaxation techniques learned and Length of
practiced labor if cervix
Support system not ready
Presence and support of a birth companion ↑ Anxiety
Husband
Mother Abruptio Hemorrhage ↑ Perinatal
Lesbian partner placentae/placenta Uterine atony mortality
Friend previa ↑ Incidence Fetal
Doula of cesarean hypoxia/acidosis
Culture birth Fetal exsanguination
A woman’s culture influences and
defines Pain
The childbirth experience Meaning and context of pain
Shameful versus joyful Acceptable responses to pain
Superstitions and beliefs about pregnancy and birth The significance of touch
Prescribed behaviors and taboos during Soothing versus intruding
the intrapartum period May be a symbol of intimacy
Relationships
Interpersonal interactions
SUMMARY
Parent–infant interactions
INTRAPARTAL HIGH RISK FACTORS
Role expectations of family members
Support person involvement
Factor Maternal Fetal-Neonatal Fetal heart ↑ Fear for baby Tachycardia,
Implications Implications aberrations ↑ Risk of chronic asphyxic
cesarean birth, insult,
forceps, vacuum bradycardia,
Abnormal ↑ Incidence of ↑ Incidence of Continuous acute
presentation cesarean birth placenta pre electronic Asphyxic insult
↑ Incidence of Prematurity monitoring and Chronic hypoxia
prolonged labor ↑ Risk of congenital intervention Congenital heart
abnormality in labor block
Neonatal physical
trauma
↑ Risk of intrauterine Uterine rupture Hemorrhage Fetal anoxia
growth restriction Cesarean birth Fetal
(IUGR) for hysterectomy hemorrhage
via ↑ Risk of death ↑ Neonatal
morbidity and
mortality
Multiple ↑ Uterine Low birth weight
gestation distention →↑risk Prematurity
of postpartum ↑ Risk of
hemorrhage congenital Postdates ↑ Anxiety Postmaturity
↑ Risk of cesarean anomalies (>42 weeks) ↑ Incidence of syndrome
birth Feto-fetal induction of labor ↑ Risk of fetal-
↑ Risk of preterm transfusion ↑ Incidence of neonatal mortality
labor cesarean birth and morbidity
↑ Use of ↑ Risk of
technology to antepartum fetal
monitor fetus death
Hydramnios ↑ Discomfort ↑ Risk of ↑ Risk of ↑ Incidence or
↑ Dyspnea esophageal or shoulder dystocia risk of large baby
↑ Risk of preterm other high-
labor alimentary-tract Diabetes ↑ Risk of ↑ Risk of
atresias hydramnios malpresentation
↑ Risk of CNS ↑ Risk of ↑ Risk of
anomalies hypoglycemia or macrosomia
(myelocele) hyperglycemia ↑ Risk of IUGR
Edema of lower ↑ Risk of ↑ Risk of
extremities preeclampsia- respiratory
eclampsia distress syndrome
↑ Risk of
congenital
anomalies
Preeclampsia- ↑ Risk of seizures ↑ Risk of small-
eclampsia ↑ Risk of stroke for-gestational-age
Failure to Maternal Fetal
↑ Risk of HELLP baby
progress in labor exhaustion hypoxia/acidosis
↑ Risk of preterm
↑ Incidence of Intracranial birth
birth
augmentation of injury
↑ Risk of mortality
labor
↑ Incidence of AIDS/STI ↑ Risk of ↑ Risk of
cesarean birth additional transplacental
infections transmission
Precipitous labor Perineal, vaginal, Tentorial tears
(<3 hours) cervical (END OF 5TH PART)
lacerations
↑ Risk of COMMON POSTPARTUM COMPLICATIONS
postpartum
hemorrhage POST PARTUM ASSESSMENT:
A pperance
Prolapse of ↑ Fear for baby Acute fetal V ital Signs
umbilical cord Cesarean birth hypoxia/acidosis B reasts
U terus
B ladder
B owel
L ochia
E pisiotomy/Episiorrhapy
H oman’s sign
E motions
R hogam
NORMAL ABNORMAL
Temperature 36.2 – 38 C on the 38 C and above in
first 24 hours any or two
Occasionally consecutive 24-hour
febrile on the 3rd period (excluding
to 4th day the first 24 hours)
ASSESSMENT OF THE BREAST
ASSESSMENT NORMAL ABNORMAL
TECHNIQUE
Inspection Increase in size • Localized
Colostrum • swelling
Milk changes • Localized Pain
from thin • Redness
watery to • Purulent
bluish white discharges
Becomes • Cracked and
heavier irritated
Veins become nipples
apparent
ASSESSMENT NORMAL ABNORMAL
TECHNIQUE
Palpation Warm and firm Localized mass
Engorged
ASSESSMENT OF THE GENERAL APPEARANCE
Assessment Normal Abnormal
Technique Assessment Assessment
Findings Findings
Inspection/ Exhaustion Extreme
Observation Fatigue exhaustion,
Sleep hunger Weakness, and
depression at the
end of 6th week ASSESSMENT OF THE UTERUS
Pallor
ASSESSMENT NORMAL ABNORMAL
Anxiousness and
TECHNIQUE
restlessness
Dizziness
Inspection • Weight 1000 • No weight
Fainting
gms changes
immediately • Visible cervix or
after birth uterus
ASSESSMENT OF THE VITAL SIGNS
• 500 gms at • Severe
VITAL SIGNS NORMAL ABNORMAL the end of abdominal pain
first week and tenderness
• 50 grms at 6th • Lateral
Blood 90/60 – 130/80 Below 90/60
week displacement
Pressure 40 – 80 bpm 130/90 & above
• After pains of the uterus
Pulse Rate Tachycardia
during
Weak Thready
contractions
Palpitations
Measurement of descent of fundus for the woman with
NORMAL ABNORMAL vaginal birth. The fundus is located two finger-breadths
below the umbilicus. Always support the bottom of the
uterus during any assessment of the fundus.
Respiratory 16 -24 Tachypnea
Rate breaths/cycle Shallow & Irregular
Dyspnea
ASSESSMENT NORMAL ABNORMAL
TECHNIQUE
• Palpation • Cannot be • Hard and firm
• Percussio palpated • Resonant
n • Dull,
thudding
ASSESSMENT OF THE BOWEL:
ASSESSMENT NORMAL ABNORMAL
TECHNIQUE
Inspection • Constipation • Passage of
• Decrease stool out
flatus from the
• Abdominal vaginal orifice
distention
• Decrease
bowel
The uterus becomes displaced and deviated to the right movement
when the bladder is full. •
Hemorrhoids
Auscultation • decrease • Absent
bowel bowel
sound sound
ASSESSMENT OF LOCHIA
ASSESSMENT NORMAL ABNORMAL
TECHNIQUE
Palpation • Contracted • Boggy
uterus
• Cervix is soft
and malleable • Board-like
• Cervical os is abdomen
narrowed
ASSESSMENT OF THE BLADDER
ASSESSMENT NORMAL ABNORMAL
TECHNIQUE
Inspection • Temporary • Burning
difficulty of sensation
voiding • Hematuria
• Void within • Inability to void
6 to 8 hours more than 10
postpartum hours
• 3Liters • Oliguria
urinary • Severe
output/day proteinuria
• Zero-trace • Glycosuria
protein
• Zero-trace
sugar
• Urinary
stasis
TYPES OF NORMAL ABNORMAL
LOCHIA Inspect the perineum for
episiotomy/lacerations with REEDA assessment
Lochia 2 to 3 days Large Inspect C/S abdominal incisions for REEDA
Rubra postpartum clots R = redness (erythema)
E = edema
Dark Red in
E = ecchymosis
color
D = drainage, discharge
Contains blood
A = approximation
and fragments of
Postpartum Hemorrhage
the deciduas and
mucus
POSTPARTUM HEMORRHAGE
1. EARLY POSTPARTUM HEMORRHAGE
TYPES OF NORMAL ABNORMAL Uterine Atony
LOCHIA Lacerations
Hematomas
Lochia • 3 to 10 days • Reappearanc Uterine Rupture
Serosa postpartum e of bright Uterine Inversion
• Pink in color red colored 2. LATE POSTPARTUM HEMORRHAGE
• Contains blood, lochia Retention of Fragments
mucus, and • Foul-smelling Subinvolution
invading Dessiminated Intravascular Coagulation
leukocytes
UTERINE ATONY
SIGNS AND SYMPTOMS:
Boggy uterus
TYPES OF NORMAL ABNORMAL Large Uterus
LOCHIA Expulsion of large clots
Bright red bleeding
LOCHIA ALBA 10 to 14 days Reappearance Hypovolemic shock
postpartum of bright red FACTORS CAUSING UTERINE ATONY
color Multiple Gestation
Hydramnios
Contains Foul-smelling Large baby
mucus, whitish Uterine Myoma
Anestheia
Oxytoxic drugs
Multiparity
Advanced maternal age
Prolonged tocolytic agents
Dystocia
Previous Uterine surgery
Chorioamnionitis
Full bladder
MANAGEMENT OF UTERINE ATONY
Promote Uterine Contraction
Stop Bleeding
Prevent Complications:
Hypovolemic Shock - Death
MEDICAL MANAGEMENT OF UTERINE ATONY
Intravenous Fluid
Oxytoxic Medications:
ASSESSMENT OF EPISIOTOMY/EPISSIORRHAPY Oxytocin
Maleate
ASSESSMENT NORMAL ABNORMAL
Cytotec
TECHNIQUE
Antibiotics
Blood Transfusion
Catheterization
Inspection • Redness, • Hematomas Oxygen Administration
edema, and • 1 or 2 stitches SURGICAL MANAGEMENT OF UTERINE ATONY
bruises on sloughed away Ligation of Uterine Arteries
the • Large Hysterectomy
perineum lacerations NURSING DIAGNOSIS & MANAGEMENT OF UTERINE
• Slight • Purulent ATONY
separation discharges Actual/Potential Fluid Volume Deficit
of wound fundal massage
edges ice pack application on fundus
• 1st degree encourage voiding
laceration administer oxytocics as ordered
regulate IVF and BT severe perineal and pelvic pain not relieved by
Altered Tissue Perfussion analgesia
assess VS, NVS, CRT bluish bulging under the skin
assess skin color and turgor tenderness
trendelenburg position firm to palpate
oxygen administration as ordered minor bleeding
Anxiety FACTORS CAUSING HEMATOMA
emotional support Rapid Spontaneous birth
give factual information about the condition Varicosities
explain the procedures Episiorrhaphy
provide calm environment Lacerations
MANAGEMENT OF HEMATOMAS
LACERATIONS MEDICAL MANAGEMENT:
Vaginal : Analgesics
anterior Cold Compress
posterior SURGICAL MANAGEMENT:
lateral wall Incision and drainage
Perineal: Removal of sutures
first degree – skin Packing
second degree – muscles Ligation of vessels
third degree – external anal sphincter NURSING DIAGNOSIS AND INTERVENTIONS
fourth degree – rectal sphincter and Alteration in comfort; Pain
rectal mucus membrane proper referral
Cervical: ice pack application on the perineum
lateral analgesics as ordered
SIGNS AND SYMPTOMS OF LACERATIONS assist for surgical intervention
Firm and Contracted Uterus
Bright red Bleeding UTERINE RUPTURE
Tear in the birth canal, and perineum COMPLETE
FACTORS CAUSING LACERATIONS: involves endometrium, myometrium
Precipitate labor and perimetrium
Dystocia INCOMPLETE
Malpresentation intact peritoneum
Large babies SIGNS AND SYMPTOMS OF UTERINE RUPTURE
Instrumentation Localized abdominal pain
Lithotomy position Abdominal tenderness
Rapid cervical dilatation Tearing feeling
Primigravida Hypovolemic shock
MANAGEMENT OF LACERATIONS: Concealed bleeding
Surgical Repair Change in abdominal contour
Cessation of bleeding FACTORS CAUSING UTERINE RUPTURE
Prevent Infection Difficult Vaginal Delivery
Alleviate pain Weak uterine operative site
MEDICAL MANAGEMENT vertical uterine scar from previous CS
o Vaginal pack Faulty presentation
o Analgesics Multiple gestation
o Antibiotics Traumatic manuevers using instruments
o Stool softener for delivery
SURGICAL MANAGEMENT OF LACERATIONS Injudicious use of oxytoxic agents
Surgical Repair Obstructed Labor
Regional anesthesia GOAL OF MANAGEMENT OF UTERINE RUPTURE
NURSING DIAGNOSIS AND MANAGEMENT OF Repair of tear or laceration
LACERATIONS Prevent Hemorrhage
Alteration in Comfort; Pain Prevent Hypovolemic shock
cold compress on the perineum Prevent Infection
perineal douch Prevent Death
high fiber diet MEDICAL MANAGEMENT OF UTERINE RUPTURE
increase OFI Intravenous fluid
NSAIDS as ordered Blood Transfusion
Potential for infection Antibiotics
pat dry the perineum Oxytoxics
frequent change of gowns and perineal pads SURGICAL MANAGEMENT OF UTERINE RUPTURE
proper nutrition Laparotomy
increased OFI Tubal ligation
prophylactic antibiotic as ordered Hysterectomy
NURSING DIAGNOSIS AND INTERVENTIONS OF
HEMATOMA UTERINE RUPTURE
SIGNS AND SYMPTOMS OF HEMATOMA Fluid Volume Deficit
Altered Cardiac Output
Altered Tissue Perfusion Emotional support
Monitor VS every 15 minutes Stay with the client
Evaluate blood loss Listen
IVF and BT Give factual informations
Administer oxygen as ordered Risk for infection
Dysfunctional Grieving Aseptic technique
Anxiety Administer prophylactic antibiotics
Fear
o Obtain consent for surgery LATE POSTPARTUM HEMORRHAGE
o Give factual informations Retained Placental Fragments
o Explain procedures Subinvolution
o Do not give reassurance Endometritis
o Emotional support RETAINED PLACENTAL FRAGMENTS
Signs and Symptoms:
UTERINE INVERSION Incomplete placental delivery
DEGREE OF INVERSION Uterus remains large
First-degree - the inverted fundus extends to, Bright red bleeding
but not through, the cervix. + HCG in the blood
Second-degree - the inverted fundus extends + ultrasound result
through the cervix but remains within the FACTORS CAUSING RETAINED PLACENTAL FRAGMENTS
vagina. Failure to inspect after placental delivery
Third-degree - the inverted fundus extends Placenta accreta
outside the vagina. MEDICAL MANAGEMENT OF RETAINED PLACENTA
Total inversion - the vagina and uterus are Oxytoxin administration
inverted. Methotrexate
SIGNS AND SYMPTOMS: IVF
Visualization of protruded uterus SURGICAL MANAGEMENT OR RETAINED PLACENTA
Sudden gush of large amount of blood Dilatation and Curettage
Hypovolemic shock after 10 minutes Hysterectomy
FACTORS CAUSING UTERINE INVERSION NURSING DIAGNOSIS AND MANAGEMENT
Pulling the umbilical cord before placental Fluid Volume Deficit
separation Decreased cardiac Output
Extreme pushing of the fundus Altered Tissue Perfusion
Fundal implantation of the placenta Risk for infection
GOAL OF CARE OF UTERINE INVERSION Anxiety
Prevent Hemorrhage
Jhonson’s Maneuver SUBINVOLUTION OF THE UTERUS
Prevent Shock Signs and Symptoms:
Prevent Infection Uterus remains large
Prevent Death Lochia is profused
MEDICAL MANAGEMENT Altered pattern of lochia
Initially: FACTORS CAUSING UTERINE SUBINVOLUTION
Tocolytic Retained Placental fragments
General anesthesia Endometritis
Nitroglycerine Uterine Myoma
Oxytocic agents MEDICAL MANAGEMENT OF UTERINE SUBINVOLUTION
Double intravenous fluid Oxytocin
Oxygen administration Maleate
Ready for CPR IVF
Antibiotics SURGICAL MANAGEMENT OF UTERINE
Blood Transfusion SUBINVOLUTION
SURGICAL MANAGEMENT Hysterectomy
Jhonson’s Maneuver NURSING DIAGNOSIS AND MANAGEMENT
Surgical Replacement Fluid Volume Deficit
Hysterectomy Altered Cardiac Output
Laparotomy Altered Tissue Perfusion
General Anesthesia Alteration in thermoregulation; hyperthermia
NURSING DIAGNOSIS AND INTERVENTION Anxiety
Fluid Volume Deficit Fear
Altered Cardiac Output
Altered Tissue Perfusion DISSEMINATED INTRAVASCULAR COAGULATION
Determine the degree of inversion Signs and Symptoms:
Assess VS, NVS, and CRT Mild oozing of venipuncture site
Evaluate blood loss Petechiae
Use large needles/cannula for FACTORS CAUSING DIC
intravenous fluid PIH
Regulate IVF and BT as ordered Abruptio Placenta
Administer oxygen by face mask Incomplete Abortion
Anxiety Septic Abortion
Prolonged retention of dead fetus PERITONITIS
Amniotic fluid Embolism an infection of the peritoneal cavity
Hypertonic labor usually an extension of endometritis
Sepsis gravest of postpartum complications
GOAL OF MANAGEMENT OF DIC common cause of mortality death from
Treat underlying conditions puerperal infection
Stop Clotting Signs and Symptoms of Peritonitis
Restore normal clotting functions rigid abdomen with guarding behavior
MEDICAL MANAGEMENT OF DIC abdominal pain
Heparin high fever
Blood Replacement rapid pulse
Fresh Frozen Plasma vomiting
Platelet Replacement appearance of acutely ill
NURSING DIAGNOSIS AND INTERVENTIONS Management of Peritonitis
Actual/Potential Fluid Volume Deficit large dose of antibiotics
Frequent monitoring NGT to relieve vomiting and rest the bowel
Evaluate blood loss IVF
Gentle handling of patient parenteral feeding
Frequent turning to sides analgesics
antipyretics
PUERPERAL INFECTION
Infection of the genital tract during postpartum MASTITIS
TYPES OF INFECTION infection of the breast tissues
Endometritis occurs as early as 7 days postpartum or not
Infection of the Perineum until the baby is weeks or months of age
Peritonitis ETIOLOGY:
Mastitis Staphylococcus
Endometritis Streptococcus
an infection of the inner lining (endometrium) Eschericia
of the uterus Signs and Symptoms of Mastitis
bacteria may gain access from the vagina into localized pain, swelling, and redness
the uterus maybe during delivery process fever
Signs and Symptoms of Endometritis body malaise
fever for 2 consecutive 24 hours usually on the rapid pulse
3rd or 4th day excluding the first 24 hours scanty breast milk
postpartum Management of Mastitis
chills broad spectrum antibiotics
loss of appetite analgesics
general malaise antipyretics
abdominal tenderness warm or cold compress
uterine atony supportive bra
strong afterpains constant emptying
dark brown foul smelling lochia incision and drainage
Management of Endometritis Nursing Diagnosis of Puerperal Infection
antibiotics Actual/potential for infection
oxytocic Alteration in thermoregulation; hyperthermia
analgesics Alteration in comfort; pain
antipyretics Social Isolation
Infection of the Perineum
very rare because of improved aseptic THROMBOPHLEBITIS
technique It is the inflammation of the lining of the
occurs at the suture line or repair of lacerations vessel in which a clot attaches to the vessel
Signs and Symptoms of Infection of the Perineum wall.
pain on the perineum May not appear until 10-20 days after
swelling delivery
heat THREE MAJOR CAUSES:
pressure on the perineum venous stasis
one or two stitches slough off hypercoagulability
purulent discharges from suture line damage of the intima of the blood vessels
may be afebrile unless systemic Other Factors:
Management of the Infection of the Perineum varicosities
systemic or topical antibiotics obesity
analgesics history of thrombophlebitis
hot sitz bath oral contraceptives
warm compress age >35 years old
perineal sutures may be removed to allow multiparity
drainage diabetes millitus
packing with gauze smoking
Classifications of Thrombophlebitis according to the avoid pillows under the knees
depth don’t smoke
a) Superficial venous thrombosis EMOTIONAL AND PSYCHOLOGICAL POSTPARTAL
limited to the calf only COMPLICATIONS
swelling of extremity, redness, Phases of Puerperium:
tenderness, and warm, pain while 1. Taking-in Phase
walking This is the time of reflection for a woman.
b) Deep vein thrombosis The woman is passive letting other people
often absent or diffused signs (husband, nurse, etc.) do things for her and
swelling, erythema, edema, heat, make decisions for her.
tenderness 2. Taking-hold Phase
phlegmasia This is the phase where the woman begins to
Classifications of Thrombophlebitis according to initiate action herself.
location shows a woman with great interest on caring
a) Femoral for the baby.
fever, chills, pain, redness, 3. Letting-go
swelling of extremeties, The woman finally defines her new role.
White - stretched skin, She gives up the fantasized image of her child
+ homan’s sign for the real one.
b) Pelvic POSTPARTUM BLUES
ovarian, uterine, hypogastric vein It is a maternal adjustment reaction
high fever
chills accompanied by irritability, anxiety, and a mild
body malaise let-down feeling
Management of Thrombophlebitis usually occurring between the 2nd to 3rd
Anticoagulant (Warfarin, Heparin) postpartum day through the 1st to 2nd
Thrombolytic (Streptokinase, Urokinase) postpartum week.
Analgesics ( except aspirin) Signs and symptoms of Postpartum Blues
laparotomy – locate and incise to remove Insomnia
affected veins Depressed mood
monitoring of prothrombin time Headache
Nursing Diagnosis and Management of Poor concentration
Thrombophlebitis Tearfulness
Alteration in Comfort; pain Confusion
rest Mood labile
elevate legs Factors causing Postpartum Blues
antiembolic stockings sudden drop of hormone at about 72
avoid standing for long period of time hours postpartum
moist heat application disappointments of body changes
DO NOT MASSAGE extreme disappointments of labor and
Altered Tissue Perfusion birth
constantly check the skin inadequate emotional support from
passive range of motion exercise partner
prevent skin ulcerations extreme stress from mothering role
proper nutrition Management of Postpartum Blues
avoid gatch or pillow under the knee allow woman to talk and cry
Risk for Injury (bleeding) related to therapy work through their feelings
btain baseline coagulation encourage family support
avoid IM injection of other drugs
rotate injection site POSTPARTUM DEPRESSION
inject heparin subcutaneously, do not It is a mood disturbance that is characterized by
massage feelings of sadness, despair, apathy, and
prepare Protamin Sulfate ( antidote of discouragement caused by loss in the person’s
Heparin) life or by neurobiological imbalance of
prepare Vitamin K ( antidote of Warfarin) neurotransmitters.
How to prevent thrombophlebitis? It occurs 30 days to 6 months after birth
avoid wearing constricting clothings SIGNS AND SYMPTOMS OF POSTPARTUM DEPRESSION
rest while feet elevated Excessive crying
ambulate daily during pregnancy Feeling of inadequacy
limit woman in lithotomy position Low self-esteem
aseptic technique in invasive procedures Inability to cope
if with varicose veins, wear support Anorexia
stockings Insomnia
first 2 weeks postpartum Psychosomatic symptoms
avoid in 1 position for long period of time Depressive or manic mood fluctuation
avoid leg crossing Social withdrawal
increase oral fluid intake
early ambulation after pregnancy
if cannot ambulate, PROM exercises
Factors causing Postpartum Depression Cervical:
history of depression changes during ovulation
troubled childhood cervical incompetence
stress in the home or at work Etiology of Female Infertility
lack self-esteem
lack of support system Uterine
Management of Postpartum Depression functional
Nurse-patient relationship structural
- therapeutic relationship Tubal
Psychopharmacologic scarring
- antidepressive drugs PID
Milleu therapy endometriosis
– forceful manipulation of the environment Ovarian
anovulation
POSTPARTUM PSYCHOSIS oligo-ovulation
It is a disrupted mental state in which an Etiology of Male Infertility
individual struggles to distinguish the external Congenital
world from his internally generated absence of vas deferens and testes
perceptions. Ejaculatory
The disorder may become apparent 2 to 3 retrograde ejaculation
weeks after birth to as long as 6 to 12 months. Sperm abnormalities
Factors causing Postpartum Psychosis oligospermia
major life crisis aspermia
previous mental illness inadequate maturation
family history of mental illness inadequate motiliy
hormonal changes inability to deposit sperm into the vagina
Signs and Symptoms of Postpartum Psychosis blockage of sperm
suicidal and infanticidal thoughts Testicular
dissociated orchitis
delusional cryptorchidism
confused trauma
distortion of reality radiation
Management of Postpartum Psychosis Coital
professional psychiatric counselling obesity
antipsychotic drugs nerve damage
hospitalization impotence
woman must be observed during her Drugs
interaction with her child Methotrexate
Nursing Diagnosis and Management of Postpartum Amebicides
Emotional Disturbances Other factors:
Risk for/Actual Ineffective coping STD
Convey a caring attitude stress
Acknowledge that the woman feels inadequate nutrition
depressed alcohol & nicotine
Assure that it is not her fault Interactive Problems
encourage support from family Insufficient frequency of SI
members Poor timing of intercourse
Adequate rest and nutrition Development of antibodies
INFERTILITY against partner’s sperm
The inability to conceive after at least 1 year of Use of spermicidal lubricants
sexual intercourse at least 4 times a week Inability of the sperm to
without contraception. penetrate the egg
Normally……. Diagnostic Studies
50% of couples conceive within 6 Semen Analysis after 48 – 72 hours of
months abstinence
35% conceive within 12 months
Primary infertility Cervical Mucous assessment
no previous history of conception o fern test
Secondary Infertility o spinnbarkeit test
inability to conceive after previous successful Postcoital Test
pregnancy o SI at presumed ovulatory state
Etiology of Female Infertility o after48 hour abstinence
Vaginal problems: o Check cervical mucus
vaginal infections Basal Body Recording
anatomic abnormalities o oral temp when awakening
sexual dysfunction o increase temp 12-14 days
highly acidic vaginal environment o before menses- ovulation
MANAGEMENT OF INFERTILITY IVF may be an option if you or your partner have been
1. Management of underlying problems diagnosed with:
douche with alkaline solution 30 minutes Endometriosis
before intercourse Low sperm counts
surgery Problems with the uterus or fallopian tubes
medications Problems with ovulation
antibiotic Antibody problems that harm sperm or eggs
testosterone The inability of sperm to penetrate or survive in
estrogen the cervical mucus
sexual therapy An unexplained fertility problem
2. Assisted Reproductive Techniques Surrogate embryo transfer
artificial insemination embryos are placed into the uterus of a female
In vitro fertilization with the intent to establish a pregnancy.
Surrogate embryo transfer embryos are typically transferred 3 days
Surrogate mothering after fertilization.
ARTIFICIAL INSEMINATION PROCESS:
The process by which a woman is medically After the follicles are aspirated from the
impregnated using semen from her husband or Intended Mother or Egg Donor they will be
from a third-party donor. examined and mixed with the intended father
Injecting collected semen into the woman's or a donors sperm.
uterus and is performed under a physician's They are then incubated for 3 - 5 days to allow
supervision. fertilization to occur.
INDICATION The gestational surrogate, intended parents and
men who have very low sperm counts. reproductive physician will have a consult to
sperm that aren't strong enough to swim determine the number of embryos to transfer.
through the cervix and up into the fallopian Then, the embryos will be placed in the
tubes. surrogates uterus via invitro fertilization
option for women who have endometriosis or the embryo transfer procedure will take place in
abnormalities of any of their reproductive a sterile, surgical room within the fertility clinic
organs. or hospital.
PROCESS: The process does not cause discomfort and
washing the sperm requires no medication or anesthesia. .
liquefying the sperm at room temperature for The process usually takes approximately ten-
30 minutes fifteen minutes.
harmless chemical is added to separate out the surrogates will be required to remain at the
most active sperm. clinic for at least one-two hours after the
centrifuge is used to collect the best sperm. completion of the transfer procedure to rest .
sperm are then placed in a thin tube called a Surrogates will be required to rest with activity
catheter and introduced through the vagina and restrictions for two-three days following the
cervix into the uterus transfer procedure.
cramping during the procedure and SURROGATE MOTHER
light bleeding afterward A woman who bears a child for another person,
Immediately after the procedure, your doctor often for pay.
will probably have you lie down for about 15 to A substitute mother
45 minutes to give the sperm a chance to get to TWO KINDS OF SURROGATE MOTHER
work. Traditional surrogates
you can resume your usual activities. is a woman who is artificially inseminated with
the father's sperm.
Success rates for artificial insemination vary. Factors She then carries the baby and delivers it for the
that lessen your chance of success include: parents to raise.
Older age of the woman is the baby's biological mother. That's because it
Poor egg quality was her egg that was fertilized by the father's
Poor sperm quality sperm. Donor sperm can also be used for a
Severe endometriosis traditional surrogacy.
Severe damage to fallopian tubes (usually from GESTATIONAL SURROGATES
chronic infection) has no genetic ties to the child. That's because it
Blockage of fallopian tubes (IUI will usually not wasn't her egg that was used.
work in this case) is called the "birth mother.
IN VITRO FERTILIZATION more common than a traditional surrogate
is a process by which an egg is fertilized by WHO USES SURROGATES:
sperm outside the body in a laboratory. Those with medical problems with her uterus.
The fertilized egg (zygote) is then transferred to hysterectomy
the patient's uterus. conditions that make pregnancy impossible or
medically risky, such as severe heart disease.
OTHER REASONS:
age
marital status
sexual orientation
CHOOSING A SURROGATE:
1. Is at least 21 years old
2. Has already given birth to at least one healthy
baby
3. Has passed a psychological screening by a
mental health professional
4. Willingly signs a contract agreeing to her role
and responsibilities in the pregnancy
5. have a complete medical evaluation and
pregnancy history to assess the likelihood of a
healthy, full-term pregnancy.
P
A
A
A
A
A
h
y
s
i
c
a
l
d
e
f
o
r
m
i
t
i
e
s
l
r
e
t
a
r
d
a
t
i
o
n
D
e
v
e
l
o
p
m
e
n
t
a
l
p
r
o
You might also like
- Clinical NutritionDocument27 pagesClinical NutritionKhushiNo ratings yet
- Is Schizophrenia Really Demonic PossessionDocument5 pagesIs Schizophrenia Really Demonic PossessionUproottNo ratings yet
- School Oral Health ProgramDocument24 pagesSchool Oral Health ProgramRinku Roshan100% (1)
- PRN2155A ASHI G2015 BLS Exam VersionA Revised 100516Document5 pagesPRN2155A ASHI G2015 BLS Exam VersionA Revised 100516Clark Angelo Juan100% (1)
- Causes and Types of Bleedings in Early PregnancyDocument136 pagesCauses and Types of Bleedings in Early PregnancyYoseph KassaNo ratings yet
- Hypertension Disorder in PregnancyDocument42 pagesHypertension Disorder in Pregnancyholly girlchy JastinNo ratings yet
- Hematological DisordersDocument45 pagesHematological Disordersbara.jarrar2001No ratings yet
- Drug Abuse in PregnancyDocument91 pagesDrug Abuse in PregnancyCrystal Gayle Nario Sabado100% (1)
- Urinary CatheterDocument4 pagesUrinary CatheterBindu SinghNo ratings yet
- Unit1 HistoryDocument75 pagesUnit1 HistoryChristine Carol FilipinasNo ratings yet
- Physiologic Changes of Pregnancy (Normal) : Local (I.e., Confined To The Systemic (I.e., Affecting TheDocument9 pagesPhysiologic Changes of Pregnancy (Normal) : Local (I.e., Confined To The Systemic (I.e., Affecting TheAli Longasa CortezNo ratings yet
- Treating Pneumonia in Children Under 5Document38 pagesTreating Pneumonia in Children Under 5Arjumand AliNo ratings yet
- Maternal Notes Google DocsDocument24 pagesMaternal Notes Google DocsOracion, Bernette Meiji B.No ratings yet
- PhilHealth guidelines for hospitals outsourcing servicesDocument1 pagePhilHealth guidelines for hospitals outsourcing servicesEJ LomocsoNo ratings yet
- AntepartalDocument43 pagesAntepartalxing414No ratings yet
- Respiratory Distress in NewbornDocument52 pagesRespiratory Distress in NewbornNadia SalwaniNo ratings yet
- Management of Patients With Neurologic DysfunctionDocument24 pagesManagement of Patients With Neurologic DysfunctionYahya AL-HelihNo ratings yet
- Chickenpox What Is Chickenpox?Document19 pagesChickenpox What Is Chickenpox?s.khan9211rediffmail.comNo ratings yet
- Introduction to Pharmacology: Effects of Drugs & Medication AdministrationDocument2 pagesIntroduction to Pharmacology: Effects of Drugs & Medication AdministrationAdri Sinclaire100% (1)
- Individual Aging Vs Population AgingDocument74 pagesIndividual Aging Vs Population AgingAnthony RiggsNo ratings yet
- Pneumonia Definations & ClassificationsDocument29 pagesPneumonia Definations & ClassificationsJimitNo ratings yet
- AntraxDocument17 pagesAntraxEdwin VazquezNo ratings yet
- A Preschool-Based Intervention For Early ChildhoodDocument9 pagesA Preschool-Based Intervention For Early Childhoodmohammed MusaNo ratings yet
- Cardiopulmonary Resuscitation: College of Nursing Madras Medical CollegeDocument48 pagesCardiopulmonary Resuscitation: College of Nursing Madras Medical CollegeNithin ManlyNo ratings yet
- Burns Rule of Nines 2013Document1 pageBurns Rule of Nines 2013ellenningrumNo ratings yet
- TRICHOMONIASISDocument39 pagesTRICHOMONIASISAlunaficha Melody KiraniaNo ratings yet
- Types of PneumoniaDocument6 pagesTypes of PneumoniasakuraleeshaoranNo ratings yet
- AdulthoodDocument5 pagesAdulthoodSherwin Purisima TaguesaNo ratings yet
- Layers of The SkinDocument49 pagesLayers of The SkinBakri MustafaNo ratings yet
- 15.somatization DisorderDocument13 pages15.somatization DisorderGERSON RYANTONo ratings yet
- Chloride Imbalance Causes and TreatmentsDocument2 pagesChloride Imbalance Causes and Treatmentsed123edNo ratings yet
- 03 Unit .Self Concept and Self PerceptionDocument27 pages03 Unit .Self Concept and Self PerceptionIrfan Ali JunejoNo ratings yet
- Nutrition Essentials for Growing PreschoolersDocument6 pagesNutrition Essentials for Growing PreschoolersKeerthana VNo ratings yet
- MuscleDocument91 pagesMusclebGrNo ratings yet
- Pain Assessment & MGTDocument16 pagesPain Assessment & MGTSitti Mardiya SariolNo ratings yet
- K44 - Nutrition During LactationDocument26 pagesK44 - Nutrition During Lactationbilli lisanuddinNo ratings yet
- Assessment of Digestive and Gastrointestinal FunctionDocument19 pagesAssessment of Digestive and Gastrointestinal FunctionMarichelle Vicente- Delos SantosNo ratings yet
- Nursing Process InpDocument21 pagesNursing Process InpFaye EvascoNo ratings yet
- CMCA LEC 12-IntrapartumDocument189 pagesCMCA LEC 12-IntrapartumCarl Josef C. GarciaNo ratings yet
- Assessing The SkinDocument22 pagesAssessing The Skinjasnate84No ratings yet
- Postpartum HemorrhageDocument16 pagesPostpartum HemorrhageLuayon FrancisNo ratings yet
- Common Health Problems of Infancy PowptDocument78 pagesCommon Health Problems of Infancy PowptCiella Dela CruzNo ratings yet
- Dedication SpeechDocument1 pageDedication SpeechchrmnplNo ratings yet
- National Control of Dirrheal Diseases (CDD) Program ObjectivesDocument6 pagesNational Control of Dirrheal Diseases (CDD) Program ObjectivesJoy FucananNo ratings yet
- Diagnosis of Preterm Labor and Overview of Preterm BirthDocument15 pagesDiagnosis of Preterm Labor and Overview of Preterm BirthKenny IncsNo ratings yet
- Signs of LaborDocument40 pagesSigns of LaborDominicSavioNo ratings yet
- Chapter 3Document2 pagesChapter 3Laramy Lacy MontgomeryNo ratings yet
- Maternal and Child Health CareDocument7 pagesMaternal and Child Health CareNessa Layos MorilloNo ratings yet
- Assessment of A Pregnant FamilyDocument4 pagesAssessment of A Pregnant FamilyLuna Sang-anNo ratings yet
- Prenatal Care Assessment: Monitoring Risks and ComplicationsDocument6 pagesPrenatal Care Assessment: Monitoring Risks and ComplicationsSupremo Manuel M DeluaoNo ratings yet
- Instruments and ProceduresDocument11 pagesInstruments and ProceduresKristina Buenaventura0% (1)
- Trichomonas Vaginalis InfectionDocument31 pagesTrichomonas Vaginalis InfectionVeigner Whyng Cabugayan100% (1)
- Management of Patients With Gastric and Duodenal DisordersDocument7 pagesManagement of Patients With Gastric and Duodenal DisordersintotheunknownNo ratings yet
- Systemic Changes During PregnancyDocument2 pagesSystemic Changes During PregnancyARAugusto67% (3)
- TEPID SPONGE BATHDocument3 pagesTEPID SPONGE BATHJeonoh FloridaNo ratings yet
- 6-Health Problems Common in PreschoolerDocument36 pages6-Health Problems Common in PreschoolerPam Lala100% (2)
- Japan Gifts GivingDocument3 pagesJapan Gifts GivingRehan PervaizNo ratings yet
- Skeletal Muscle Physiology PDFDocument6 pagesSkeletal Muscle Physiology PDFAstri Ggamjong Xiao LuNo ratings yet
- Malnutritiom and Anemia ImciDocument30 pagesMalnutritiom and Anemia ImcibaridacheNo ratings yet
- GNRH Agonists Et AnatagonistsDocument44 pagesGNRH Agonists Et Anatagonistshoussein.hajj.md100% (1)
- TLG IV TherapyDocument10 pagesTLG IV TherapyStephanie Joy EscalaNo ratings yet
- Fundal Height DefinedDocument2 pagesFundal Height Definedervin0122No ratings yet
- Teratogens: ND THDocument5 pagesTeratogens: ND THMinhwa KimNo ratings yet
- Baby Friendly Hospital InitiativeDocument38 pagesBaby Friendly Hospital InitiativeSudhir SinghNo ratings yet
- Lumbar Disc HerniationDocument19 pagesLumbar Disc HerniationPutri WulandariNo ratings yet
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesFrom EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNo ratings yet
- Clerk Sheet Imed and ObsDocument4 pagesClerk Sheet Imed and ObsGrace PhiriNo ratings yet
- ScoliosisDocument4 pagesScoliosisDharline Abbygale Garvida AgullanaNo ratings yet
- Sheikh Khalifa Medical City General HospitalDocument3 pagesSheikh Khalifa Medical City General Hospitalamr ahmedNo ratings yet
- Guest Lecture 3Document3 pagesGuest Lecture 3Jim XieNo ratings yet
- Venipuncture: Syringe Draw Procedure Principles of Medical Technology Practice 2 Laboratory Act. 6Document17 pagesVenipuncture: Syringe Draw Procedure Principles of Medical Technology Practice 2 Laboratory Act. 6ALEXANDRA MARIE BUNQUINNo ratings yet
- Herbal Remedies For Mouth Ulcer: A Review: KeywordsDocument7 pagesHerbal Remedies For Mouth Ulcer: A Review: KeywordsumapNo ratings yet
- Bogash 1963Document5 pagesBogash 1963wahyu santikaNo ratings yet
- NCM 417 - Midterm Exam 2015Document5 pagesNCM 417 - Midterm Exam 2015Mae DacerNo ratings yet
- Fundamentals of Medical Ethics by DR Myint Oo GPDocument200 pagesFundamentals of Medical Ethics by DR Myint Oo GPyeyint100% (1)
- Research Article: Plant Leaves Extract Irrigation On Wound Healing in Diabetic Foot UlcersDocument9 pagesResearch Article: Plant Leaves Extract Irrigation On Wound Healing in Diabetic Foot UlcersHyacinth A RotaNo ratings yet
- Cautery To Little's Area: What Is Little's Area and Why Do I Need This Operation?Document4 pagesCautery To Little's Area: What Is Little's Area and Why Do I Need This Operation?Moustafa EzzatNo ratings yet
- Art & Science: Meeting The Needs of Patients' Families in Intensive Care UnitsDocument8 pagesArt & Science: Meeting The Needs of Patients' Families in Intensive Care UnitsRiaNo ratings yet
- Hygiene & SanitationDocument12 pagesHygiene & SanitationEd GopsNo ratings yet
- Test Drils Nseip 103427Document117 pagesTest Drils Nseip 103427Olive NNo ratings yet
- Introduction To PathologyDocument14 pagesIntroduction To PathologyAlfred ChowNo ratings yet
- Terapi ToxoplasmosisDocument9 pagesTerapi Toxoplasmosissarah disaNo ratings yet
- An Anal FissureDocument4 pagesAn Anal FissureErnesErlyanaSuryawijayaNo ratings yet
- 534-Article Text-2238-1-10-20210317Document6 pages534-Article Text-2238-1-10-20210317laila qothrunnadaNo ratings yet
- Using The ACLS Bradycardia Algorithm For Managing BradycardiaDocument2 pagesUsing The ACLS Bradycardia Algorithm For Managing BradycardiasetiamegaNo ratings yet
- Long-Term Surgery Graves Disease 20 YearsDocument3 pagesLong-Term Surgery Graves Disease 20 YearsTambunta TariganNo ratings yet
- Sir ModelDocument5 pagesSir ModelJaehun JeongNo ratings yet
- ENT Guidebook Arab BoardDocument9 pagesENT Guidebook Arab BoardahmedNo ratings yet
- Merec Bulletin Vol15 No6Document4 pagesMerec Bulletin Vol15 No6n4dn4dNo ratings yet
- Cefazolin Drug Study SummaryDocument4 pagesCefazolin Drug Study Summaryshadow gonzalezNo ratings yet