Professional Documents
Culture Documents
Avclesesaf 5
Uploaded by
Oneng IfayaniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Avclesesaf 5
Uploaded by
Oneng IfayaniCopyright:
Available Formats
Stroke in lupus and APS
LCD de Amorim et al.
532
Sneddon’s syndrome frequently presents with leu- Central venous thrombosis (CVST)
coaraiosis and small lacunar infarcts.31
CVST is an unusual cause of cerebrovascular dis-
Sneddon’s syndrome is not a unique entity.
ease, most of the time under-recognized. It usually
Comparison of patients with or without aPL
presents as a refractory headache, sometimes asso-
showed that the livedo reticularis was clearly
ciated with an epileptic seizure, focal deficits, or
larger in aPL-negative patients who, nevertheless,
intracranial hypertension syndrome. Its association
did not develop thrombocytopenia; and seizures
with SLE has been documented, mostly through
and clinically audible mitral regurgitation were
case reports, and the use of corticosteroids and
more frequently observed in aPL-positive
lumbar puncture may be risk factors that increase
patients.32 It is possible that some of the patients
the incidence of this condition.39 The association of
diagnosed with this syndrome will develop APS or
APS with CSVT is much better recognized as the
SLE over time.
most common acquired thrombophilia associated
with this syndrome, and it requires a high sense
Haemorrhagic stroke
of awareness of this diagnosis, since early treatment
Haemorrhagic stroke frequency is very low and rep- implicates a better prognosis.39
resents approximately 10% of all strokes.33 It occurs
more frequently in patients over 50 years of age with Other CNS manifestations
hypertension.33 Intraparenchymatous haemor-
Vascular cognitive impairment has been increas-
rhagic stroke is three times more common in SLE
ingly recognized as a major cause of neurological
patients than in healthy individuals due to endothe-
deficits in the older population and is frequently
lial dysfunction characteristic of the disease that
associated with white matter lesions burden.40
leads to a rupture of intracerebral vasculature.1,8
In SLE, this pattern of CNS lesions has been
SAH occurs in approximately 5% of all strokes
increasingly studied recently, but its clinical signifi-
and affects mainly young women, with a peak age
cance is not very clear yet.41 In APS, although the
of approximately 50 years.1 The risk of SAH is four
same finding was expected, a study by
times more common in SLE patients compared to
Arvanitakis42 studying post-mortem brains did
healthy individuals, and the disruption of vascular
not show an increased incidence of infarcts in this
aneurysm is the main cause.34 Older age, high ster-
population. SLE itself can cause stroke rarely
oid intake, previous transfusions, cerebral vascu-
due to vasculopathy or vasculitis, and true vascu-
litis, kidney disease, and hypertension are risk
litis is rare. 5
factors for its occurrence.34 As in the general popu-
lation, SAH in SLE occurs in people under age 50
Patient workup
years, in the first five years of disease onset, and has
a mortality rate ranging from 25% to 35%.1,35 When evaluating a patient with a suspected cere-
Importantly, a study observed an earlier onset of brovascular disease caused by SLE, it is important
SAH in SLE patients than in the general popula- to evaluate some aspects of the medical history and
tion (44.5 versus 57.7 years), and SLE patients had physical examination. Regarding symptoms, the
a higher risk of SAH, with an incidence rate ratio of presence of a new headache is frequent in CVST,
4.84 (p < 0.001).35 In addition, age (HR 1.03; 95% SAH, and some strokes related to vasculitis. A
95% CI 1.01–1.05), platelet transfusion (HR 2.75; sudden onset of a focal deficit is usually correlated
95% CI 1.46–5.17), red blood cell transfusion (HR with an embolic or atherosclerotic cause. Seizures
7.11; 95% CI 2.81–17.97), and a mean daily steroid can be present in any of these conditions, but are
dose >10 mg of prednisolone or the equivalent (HR probably more frequent in cases related to
4.36; 95% CI 2.19–8.68) were independent risk fac- vasculitis.
tors for the new onset of SAH.36 During the physical examination, a careful
Aneurysm rupture is the most common cause search for systemic signs related to disease activity
(85%) of SAH followed by a perimesencephalic must be sought (e.g. dermatological features, arth-
SAH, not aneurysmal haemorrhage (10%), and ritis, serositis, livedo reticularis). The neurological
the other 5% is represented by other rare exam must include the level of consciousness deter-
causes.37 Three different mechanisms of SAH in mination, language testing, strength, reflexes, sens-
SLE have been described: multiple saccular aneur- ibility, cranial nerves, coordination, and balance.
ysms, distal fusiform aneurysms with aberrant The NIHSS is a good guide for the gross evaluation
morphology in uncommon locations, and angio- of these patients and is mandatory when a sudden
graphic-negative SAH.38 deficit is being evaluated.21
Lupus
You might also like
- Pmed 1002595 s003Document2 pagesPmed 1002595 s003Oneng IfayaniNo ratings yet
- Biostatistics: Descriptive Analysis and Differences Between GroupsDocument17 pagesBiostatistics: Descriptive Analysis and Differences Between GroupsOneng IfayaniNo ratings yet
- Intervention Type Quality AssessmentDocument5 pagesIntervention Type Quality AssessmentOneng IfayaniNo ratings yet
- PRISMA 2009 Checklist: Section/topic # Checklist Item Reported On Page #Document3 pagesPRISMA 2009 Checklist: Section/topic # Checklist Item Reported On Page #Oneng IfayaniNo ratings yet
- Biostatistics 1Document20 pagesBiostatistics 1Oneng IfayaniNo ratings yet
- Sample Size Required Per Group When Using The T Test To Compare Means of Continuous VariablesDocument11 pagesSample Size Required Per Group When Using The T Test To Compare Means of Continuous VariablesOneng IfayaniNo ratings yet
- Chapter 14Document15 pagesChapter 14Oneng IfayaniNo ratings yet
- Adverse Drug Reactions: Type C - Continuous Reactions Due To Long-Term Drug UseDocument9 pagesAdverse Drug Reactions: Type C - Continuous Reactions Due To Long-Term Drug UseOneng IfayaniNo ratings yet
- Chapter 8Document30 pagesChapter 8Oneng IfayaniNo ratings yet
- Chapter 9Document23 pagesChapter 9Oneng IfayaniNo ratings yet
- Chapter 4Document11 pagesChapter 4Oneng IfayaniNo ratings yet
- Conceiving The Research Question and Developing The Study PlanDocument9 pagesConceiving The Research Question and Developing The Study PlanOneng IfayaniNo ratings yet
- Chapter 1Document12 pagesChapter 1Oneng IfayaniNo ratings yet
- Quality of Antimikrobial - En.idDocument4 pagesQuality of Antimikrobial - En.idOneng IfayaniNo ratings yet
- Vandergarde Thorax2006Document5 pagesVandergarde Thorax2006Oneng IfayaniNo ratings yet
- Applied Statistics Survival AnalysisDocument23 pagesApplied Statistics Survival AnalysisOneng IfayaniNo ratings yet
- Statistik Deskriptif - SDA 2Document30 pagesStatistik Deskriptif - SDA 2Oneng IfayaniNo ratings yet
- Biochemistry and Cell Biology of Dopaminergic NeurotransmissionDocument18 pagesBiochemistry and Cell Biology of Dopaminergic NeurotransmissionOneng IfayaniNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- SERENACE Injection: What Is in This LeafletDocument5 pagesSERENACE Injection: What Is in This LeafletningrumNo ratings yet
- Electroconvulsive Therapy: Aban, Katherine Maebelle G. Esguerra, Dianne Carmela RDocument46 pagesElectroconvulsive Therapy: Aban, Katherine Maebelle G. Esguerra, Dianne Carmela REdgar ManoodNo ratings yet
- Biology 2 JournalDocument5 pagesBiology 2 JournalKadymars JaboneroNo ratings yet
- Cabaran Membesarkan Anak-Anak Autisme Daripada Perspektif Ibu (The Challenges of Nurturing Autistic Children From The Mother's Perspective) PDFDocument15 pagesCabaran Membesarkan Anak-Anak Autisme Daripada Perspektif Ibu (The Challenges of Nurturing Autistic Children From The Mother's Perspective) PDFsalwani salmizanNo ratings yet
- Soal Ujian PsikiatriDocument22 pagesSoal Ujian PsikiatriArya Ganesha100% (1)
- W6L28Document16 pagesW6L28N SinghNo ratings yet
- Klinefelter SyndromeDocument15 pagesKlinefelter SyndromeصادقNo ratings yet
- What Is Dissociative Identity DisorderDocument3 pagesWhat Is Dissociative Identity DisorderShifaDhinaNo ratings yet
- Manajemen Nyeri Neuropati Pada Pasien Diabetes Melitus Tipe 2: Studi LiteraturDocument7 pagesManajemen Nyeri Neuropati Pada Pasien Diabetes Melitus Tipe 2: Studi LiteraturEka NursafitriNo ratings yet
- 96-Article Text-328-1-10-20211022Document7 pages96-Article Text-328-1-10-20211022Asaad AlnhayerNo ratings yet
- GBS MCQDocument6 pagesGBS MCQMoonNo ratings yet
- Brief Psychotic Disorder Case PresDocument43 pagesBrief Psychotic Disorder Case PresTheressa TironaNo ratings yet
- DSM 5 Vs DSM 4 Case StudiesDocument18 pagesDSM 5 Vs DSM 4 Case Studiesapi-261267976100% (1)
- H.6 Internet Addiction PowerPoint 2015Document23 pagesH.6 Internet Addiction PowerPoint 2015Khoi NguyenNo ratings yet
- Psychiatry Summaries PDFDocument30 pagesPsychiatry Summaries PDFBEATRICE SOPHIA PARMANo ratings yet
- 14 OT Pediatrics AOTA Exam Prep.130Document51 pages14 OT Pediatrics AOTA Exam Prep.130Jarred Adams100% (1)
- Neuro Dr. RehabDocument142 pagesNeuro Dr. RehabMohammed Saad NabhanNo ratings yet
- Adhd BrochureDocument2 pagesAdhd BrochureJohanna MaraNo ratings yet
- Powerpoint On HemophiliaDocument26 pagesPowerpoint On HemophiliaTheo Sanson100% (1)
- Dissociation and Trauma: in Young PeopleDocument4 pagesDissociation and Trauma: in Young Peopleyeney armenterosNo ratings yet
- Emergency Care Emt 13th Edition Ebook PDFDocument61 pagesEmergency Care Emt 13th Edition Ebook PDFadolfo.milliken17896% (49)
- Solwezi General Mental Health TeamDocument35 pagesSolwezi General Mental Health TeamHumphreyNo ratings yet
- Cognitive Therapy: Past, Present, and Future: Aaron T. BeckDocument5 pagesCognitive Therapy: Past, Present, and Future: Aaron T. BeckLuisa LageNo ratings yet
- Scid2 BPDDocument4 pagesScid2 BPDRamonaStereaNo ratings yet
- A Beautiful MIND"": Movie AnalysisDocument8 pagesA Beautiful MIND"": Movie AnalysisRonita Nuqui0% (1)
- Phtls 9th Edition Prep Packets 2019aDocument19 pagesPhtls 9th Edition Prep Packets 2019ajuan4401100% (2)
- Management of Cerebral Palsy: A Literature Review From A Physiatric PerspectiveDocument4 pagesManagement of Cerebral Palsy: A Literature Review From A Physiatric Perspectivefebry firmansyahNo ratings yet
- Abnormally High Heart RateDocument2 pagesAbnormally High Heart RateEinah EinahNo ratings yet
- The Dangers of Binge EatingDocument2 pagesThe Dangers of Binge EatingJulio AlvesNo ratings yet
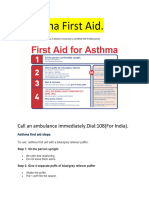
- Asthama First Aid.Document3 pagesAsthama First Aid.Manoj KumarNo ratings yet