Professional Documents
Culture Documents
10 1001@jamaoto 2020 0047
Uploaded by
neuro a2021Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
10 1001@jamaoto 2020 0047
Uploaded by
neuro a2021Copyright:
Available Formats
Research
JAMA Otolaryngology–Head & Neck Surgery | Original Investigation
Intratympanic vs Systemic Corticosteroids in First-line Treatment
of Idiopathic Sudden Sensorineural Hearing Loss
A Systematic Review and Meta-analysis
Christian Mirian, MD; Therese Ovesen, MD, DMSc
Supplemental content
IMPORTANCE To our knowledge, evidence-based recommendations on the intratympanic vs
systemic administration of corticosteroids for the treatment of idiopathic sudden
sensorineural hearing loss remain unestablished, and contradictory conclusions have been
reported in previous meta-analyses.
OBJECTIVE To compare recovery from idiopathic sudden sensorineural hearing loss based on
systemic, intratympanic, or a combined treatment with corticosteroids as first-line treatment.
DATA SOURCES We adhered to the Preferred Reporting Items for Systematic Reviews and
Meta-analyses guidelines. We searched PubMed, Embase, OvidSP, CINAHL, and Cochrane
Library from January 1, 1966, to July 1, 2018. This study was registered in the International
Prospective Register of Systematic Reviews (CRD42018109314).
STUDY SELECTION We included randomized studies. Included studies must have excluded
identifiable causes. Corticosteroids must have been administered solitarily. We excluded
studies that did not define hearing loss as a minimum 30 dB within 72 hours.
DATA EXTRACTION AND SYNTHESIS We identified 170 titles, of which 56 (32.9%) were eligible
for full-text screening. We independently extracted data. We applied a fixed-effects model to
investigate our objectives.
MAIN OUTCOMES AND MEASURE We aimed to (1) estimate the difference in mean pure tone
average (PTA) gain in decibels from intratympanic treatment vs systemic treatment and
(2) investigate odds ratios for recovery between the different treatment groups.
RESULTS We included 7 eligible studies. A total of 710 patients were allocated to receive either
intratympanic treatment (IT group, 235 [33%]), systemic treatment (ST group; 325 [46%])
or combined intratympanic and systemic treatment (CB group; 150 [21%]). The PTA was
measured by taking the mean of 4 frequencies: 4 studies measured at 500, 1000, 2000, and
3000 Hz and 3 studies measured at 500, 1000, 2000, and 4000 Hz. The ST group had a
2.01-dB higher PTA gain (95% CI, −5.61 dB to 1.59 dB; P = .96; I2 = 0%) compared with the IT
group and the odds for achieving complete recovery was not significantly different at an odds
ratio of 0.94 (95% CI, 0.61 to 1.44; P = .19; I2 = 34.5%). For the CB group vs the ST group,
the odds ratio was 1.11 (95% CI, 0.68 to 1.82; P = .75; I2 = 0%). The analysis of the CB group
vs IT group comprised only 2 studies.
CONCLUSIONS AND RELEVANCE This study does not suggest that corticosteroid delivered
intratympanically is more beneficial than systemic treatment in the case of moderate to
severe idiopathic sudden sensorineural hearing loss. There were no indications that
combined treatment was associated with improved hearing outcomes compared with either
systemic or intratympanic treatment.
Author Affiliations: Department of
Clinical Medicine, Aarhus University,
Aarhus C, Denmark (Mirian, Ovesen);
Department of Otorhinolaryngology,
Region Hospital Holstebro,
Holstebro, Denmark (Mirian, Ovesen).
Corresponding Author: Christian
Mirian, MD, Department of
Otorhinolaryngology, Region Hospital
Holstebro, Lægårdvej 12,
JAMA Otolaryngol Head Neck Surg. doi:10.1001/jamaoto.2020.0047 7500 Holstebro, Denmark
Published online March 12, 2020. (christian.mirian.larsen@regionh.dk).
(Reprinted) E1
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
Research Original Investigation Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss
A
sudden sensorineural hearing loss has an identifiable
cause in approximately 10% to 15% of cases. Retroco- Key Points
chlear disorders, such as vestibular schwannoma, com-
Question Is the outcome of first-line treatment of idiopathic
prise approximately 1%, whereas the remaining identifiable sudden sensorineural hearing loss associated with how the
cases are mostly associated with causes such as Meniére dis- corticosteroid is administered?
ease, autoimmune disease, or perilymphatic fistula.1
Findings This systematic review and meta-analysis of
Idiopathic sudden sensorineural hearing loss (ISSNHL) con-
7 randomized clinical trials did not find evidence that recovery
stitutes up to 90% of cases and is defined by acute hearing loss from moderate to severe hearing loss was different in patients for
developed within 72 hours with a decrease in hearing of at least whom corticosteroids were administered intratympanically vs
30 dB at 3 consecutive frequencies on pure-tone audiometry.2 systemically. It also found no evidence that combining the
Idiopathic sudden sensorineural hearing loss is almost exclu- 2 administration routes improved hearing recovery.
sively unilateral and typically occurs between ages 43 to 53 Meaning Future research and guidelines should determine which
years with equal sex distribution. The incidence rate has been patient groups should be allocated to receive what administration
estimated between 5 and 20 per 100 000 person-years but is (eg, systemic corticosteroids in elderly patients may be associated
most likely underestimated because many who recover quickly with increased risk of adverse effects, and so these patients should
and spontaneously never seek medical attention.1,3,4 be treated intratympanically).
A widely used standard treatment of ISSNHL is a tapering
course of oral corticosteroid. This practice is primarily based
on a randomized, double-blind placebo-controlled study from Search Strategy and Identification of Eligible Studies
1980 in which Wilson et al5 demonstrated significant hearing PubMed, Embase, OvidSP, CINAHL, and Cochrane Library were
improvement in 61% of patients treated with oral corticoste- searched from January 1, 1966, to July 1, 2018, as follows: “sud-
roid compared with 32% in the placebo group. Intratympanic den deafness OR ISSNHL OR sudden sensorineural hearing loss
treatment (ie, corticosteroid injected directly into the middle OR acute hearing loss” AND “steroid OR corticosteroid OR dexa-
ear) has gained wide popularity because of the theoretical ad- methasone OR methylprednisolone” AND “randomised OR ran-
vantage of an increased drug concentration at the targeted or- domized.” We restricted the search to randomized clinical trials
gan and the potential benefit of reduced systemic corticoste- (either placebo controlled or not), systematic reviews, and
roid exposure and associated systemic adverse effects. meta-analyses. We imposed no language restrictions.
We aimed to systematically review the current literature The preliminary search identified 170 publications, which
on corticosteroids as first-line treatment of ISSNHL. We iden- were screened by title or abstract by both authors (C.M. and
tified randomized trials and sought to meta-analytically (1) es- T.O.). A total of 56 publications (32.9%) were eligible for full-
timate the difference in mean pure tone average (PTA) gain in text assessment. Subsequently, the abstract of these articles
dB from intratympanic treatment vs systemic treatment and were jointly read by both authors: in total, 51 studies (91.1%)
(2) investigate odds ratios for recovery between intratym- were excluded because they violated the inclusion criteria, in-
panic treatment, systemic treatment, or the combination of the cluding nonrandomized studies (eg, retrospective reviews and
2 in first-line treatment of ISSNHL. case reports) and studies investigating combination therapy
with other drugs (eg, antiviral medicine). We screened the ref-
erence lists of systematic reviews and meta-analyses. Two stud-
ies were identified and added (eFigure in the Supplement).
Methods In total, 7 eligible articles were identified and reviewed in-
This systematic review and meta-analysis adhered to the Pre- dependently by both authors. Data of interest were subse-
ferred Reporting Items for Systematic Reviews and Meta- quently extracted in consensus and compiled, of which the re-
Analyses (PRISMA) guidelines.6 This study was registered in ported PTA gain in dB from baseline to follow-up was included
the International Prospective Register of Systematic Reviews first. The PTA was measured by taking the mean of 4 frequen-
(CRD42018109314). This systematic review and meta- cies: 4 studies measured at 500, 1000, 2000, and 3000 Hz8-11
analysis of aggregated, published data did not require approval and 3 studies measured at 500, 1000, 2000, and 4000 Hz.12-14
from the institutional review board nor the ethical committee The second type of data extracted was the severity of the mean
according to Danish law because it used deidentified patient hearing loss. Based on the baseline mean PTA, data from the
data. individual studies were allocated accordingly to the Good-
man criteria of hearing loss: mild (26 dB-40 dB), moderate (41
Study Inclusion dB-55 dB), moderate to severe (56 dB-70 dB), severe (71 dB-90
Included studies were randomized studies that must have ex- dB), and profound (≥91 dB). Third, data were included on the
cluded identifiable causes of sensorineural hearing loss, such proportion of patients achieving complete recovery as de-
as vestibular schwannoma or Meniére disease. Corticoste- fined within each study and in the different treatment arms.
roids must have been administered exclusively and not as com-
bination therapy (such as with antiviral medicine or hyper- Data Management
baric oxygen therapy). We excluded 1 study that did not apply Data were aggregated and allocated according to the differ-
the diagnostic criteria of a hearing loss of a minimum 30 dB ent treatment arms: patients receiving the intratympanic cor-
within 72 hours.7 ticosteroid (IT group), systemic treatment (ST group); and a
E2 JAMA Otolaryngology–Head & Neck Surgery Published online March 12, 2020 (Reprinted) jamaotolaryngology.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss Original Investigation Research
Table 1. Patient Characteristics of Intratympanic Treatment vs Systemic Treatment vs Combined Treatment
Pre-IT Pre-CB
PTA,a Hearing Gain Pre-ST PTA, Hearing Gain PTA, Mean Hearing Gain
Study Mean (SD) IT Dosage IT, Mean (SD) Mean (SD) ST Dosage ST, Mean (SD) (SD) CB Dosage CB, Mean (SD)
Rauch et al14 86.4 (NA) 40 mg × 4b 28.7 (21.6) 86.7 (NA) Prednisolonec 30.2 (21.6) NA NA NA
Hong et al10 77.5 (27.6) 1.5-2 mg × 8 NA 79.9 (23.5) Prednisoloned NA NA NA NA
Swachia et al13 66.1 (24.2) 40 mg × 4b 18.2 (8.7) 61.0 (22.0) Prednisolonee 14.7 (12.9) NA NA NA
Gundogan et al9 NA 25 mg × 4b NA 76.3 (272) Prednisolonef 25.7 (19.8) 80.7 (22.8) f) + IT dosage 44.0 (21.5)
Tsounis et al12 81.4 (23.3) 25-37.5 mg 27.0 (24.3) 81.1 (28.8) Prednisoloneg 29.0 (21.1) 79.1 (25.1) g) + IT dosage 29.8 (17.8)
× 4b
Ahn et al11 NA 1.5-2 mg × 3 NA 70.3 (21.3) Prednisoloneh NA 74.3 (27.8) h) + IT dosage NA
8
Lim et al 58.9 (31.2) 1.5-2 mg × 4 12.1 (14.6) 57.8 (28.5) Prednisolonei 12.8 (15.4) 56.8 (28.3) i) + IT dosage 21.9 (26.2)
e
Abbreviations: CB, combined treatment; IT, intratympanic treatment group; 14-day taper: 1 mg/kg × 10, 0.5 mg/kg × 2, and 0.25 mg/kg × 2.
NA, not available; PTA, pure tone average; ST, systemic treatment group. f
14-day taper: participants received 1 mg/kg and a 10 mg taper every 3 days.
a
PTA is calculated as the arithmetic mean of hearing thresholds in decibels at g
17-day taper: 1 mg/kg × 7, 0.5 mg/kg × 3, 32 mg × 4, and 16 mg × 3.
the stated audiometry frequencies in kilohertz. h
14-day taper: participants received 48 mg prednisolone for 9 days, followed
b
Methylprednisolone and not dexamethasone. by tapering for 5 days.
c
19-day taper: 60 mg × 14, 50 mg × 1, 40 mg × 1, 30 mg × 1, 20 mg × 1, i
10-day taper: 60 mg × 5, 40 mg × 2, 20 mg × 2, and 10 mg × 1.
and 10 mg × 1.
d
8-day taper: 60 mg × 4, 40 mg × 2, and 20 mg × 2.
combination of intratympanic and systemic treatment (CB Supplement. The randomization and treatment allocation were
group). The odds for achieving complete recovery were com- known in all 7 studies (to the key staff and patient), yielding a
puted for the IT, ST, and CB groups. Odds ratios were subse- high risk of bias in all 7 studies. Further associations with a high
quently calculated between the groups. An assessment of risk risk of bias were observed in the included studies: first, the al-
of bias was performed in accordance with previously estab- location of patients was not concealed in 2 studies9,10; sec-
lished Cochrane Collaboration tools.15 ond, 1 study allocated patients based on a principle of rota-
tion and alternation8; and finally, 1 study did not report the
Statistical Analysis length of follow-up.11 Hence, insufficient concealment of ran-
The fixed-effect model, assuming that 1 true effect size un- domization and nonmasked personnel and patients are pre-
derlies all included studies in the analysis, was used for effect dominant in the current literature, with the latter affecting all
size calculation. Heterogeneity was quantified accordingly to current publications. Similarly, there were numerous un-
Higgins et al,16 with low, moderate, and high corresponding known risks of bias because of insufficient reporting (eTables 2
to I2 values of 25%, 50%, and 75%.16 We performed the statis- and 3 in the Supplement).
tical analyses in R-Studio by using the metafor package.17 Sta-
tistical significance was set at P< .05. Intratympanic Treatment vs Systemic Treatment
Five studies investigated the IT group compared with the ST
group,8,10,12-14 composed of a total of 464 patients, of whom
235 (51%) were allocated to the IT group and 229 (49%) to the
Results ST group. According to the Goodman criteria, 3 studies had a
We included 7 randomized studies that investigated the effi- baseline PTA equivalent to a severe hearing loss,10,12,14 whereas
cacy of corticosteroids as first-line treatment of ISSNHL.8-14 In the remaining 2 were classified as moderate to severe hearing
total, 710 patients were allocated to receive either intratym- loss8,13 (Table 18-14). The mean days until treatment initiation
panic treatment (IT group; 235 [33%]), systemic treatment (ST ranged from 3.4 to 10.1 days in the IT group vs 3.1 to 7.1 days
group; 325 [46%]), or combined intratympanic and systemic in the ST group. One study did not report days until treat-
treatment (CB group; 150 [21%]). The follow-up time ranged ment initiation.13 Follow-up ranged from 17 days to 3 months
from 17 days to 3 months but was not reported in 1 study.11 The (eTable 1 in the Supplement).
mean time from symptom presentation to treatment initia- Four studies were eligible for analysis of differences in
tion ranged between 3.1 to 10.1 days but was not reported in 1 mean PTA gain.8,12-14 The fixed-effects model estimated no sig-
study.13 The mean PTA at the time of diagnosis was equiva- nificant difference in mean PTA gain between the 2 groups
lent to a severe hearings loss according to Goodman criteria (−2.01 dB; 95% CI, −5.61 dB to 1.59 dB; P = .96; I2 = 0%; χ2
in five studies9-12,14 and moderate to severe in the remaining P = .62). The model indicated no significant heterogeneity
two.8,13 The mean age ranged between 45.9 to 56.9 years (Figure 18,12-14).
(eTable 1 in the Supplement). For the IT group, complete recovery was achieved in 56 of
235 patients (24%), and for the ST group, complete recovery
Risk of Bias Assessment was achieved in 58 of 229 patients (25%) (Table 22,8-14,18).
We assessed the risk of bias in each of the included studies. Figure 28,10,12-14 comprises odds for recovery stratified for base-
We present the detailed assessment in eTables 2 and 3 in the line PTA; first, moderate to severe hearing loss, which indi-
jamaotolaryngology.com (Reprinted) JAMA Otolaryngology–Head & Neck Surgery Published online March 12, 2020 E3
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
Research Original Investigation Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss
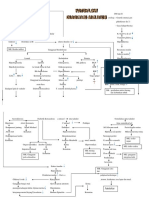
Figure 1. Mean Hearing Gain in Decibels (dB) From Baseline (Pretreatment) Pure Tone Average (PTA) Compared With PTA at Follow-up
(Between 1 to 3 Months)
Intratympanic Systemic
Group Treatment Group Mean Difference Weight,
Study Mean (SD) Total Mean (SD) Total (95% CI) %
Severe PTA at baseline
Tsounis et al,12 2018 27 (24.3) 34 29 (21.1) 35 –2.00 (–12.75 to 8.75) 11.21
Rauch et al,14 2011 28.7 (21.6) 129 30.2 (21.6) 121 –1.50 (–6.86 to 3.86) 45.13
Sum for severe fixed-effects 0.20 (0.00 to 24.43)
modela
Moderate to severe PTA at baseline
Swachia et al,13 2016 14.7 (12.9) 20 18.2 (8.7) 22 –3.50 (–10.22 to 3.22) 28.68
Lim et al,8 2013 12.1 (14.6) 20 12.8 (15.4) 20 –0.70 (–10.00 to 8.60) 14.98
Sum for moderate to severe 0.08 (0.00 to 18.33)
fixed-effects modelb
Fixed-effects model for all studiesc –2.01 (–5.61 to 1.59) 100
–9 –6 –3 0 3 6 9
Mean Difference in dB (95% CI)
b
The forest plot illustrates the mean difference, which is the PTA mean gain in dB Q1 = 0.23; P = .63; I2 = 0%.
of intratympanic therapy subtracted from the PTA mean gain in dB of systemic c
Q3 = 0.30; P = .96; I2 = 0%.
therapy. Total indicates the number of patients.
a
Q1 = 0.01; P = .93; I2 = 0%.
Table 2. Definitions of Recovery Used in the Different Studies and Recovery Rates of Intratympanic vs Systemic vs Combined Treatment
Complete Recovery, Events/Total Group
No. of Patients Size, No./Total No. (%)
Goodman
Source Definition of Recovery Criteria IT ST CB IT Group ST Group CB Group
Rauch et al14 PTA <30 dB: hearing recovery to normal Severe 129 121 NA 32/129 (25) 25/121 (21) NA
30 dB to 90 dB: hearing aid range
Swachia et al13 From Furuhashi et al18 complete recovery: PTA ≤25dB Moderate 20 22 NA 5/20 (25) 4/22 (18) NA
Marked recovery: PTA improvement >30 dB to severe
Slight recovery: 10 dB< PTA improvement <30 dB
No recovery: PTA improvement <10 dB
Hong et al10 Siegel criteria Severe 32 31 NA 10/32 (31) 9/31 (29) NA
Complete recovery: final hearing better than 25 dB
Partial recovery: >15 dB gain and final hearing 25-45 dB
Slight improvement: >15 dB gain and final hearing
poorer than 45 dB
No improvement: <15 dB gain and final hearing
poorer than 75 dB
Gundogan et al9 Siegel criteria Severe 36 37 NA 10/36 (28) 14/37 (38)
Complete recovery: final hearing better than 25 dB
Partial recovery: >15 dB gain and final hearing 25-45 dB
Slight improvement: >15 dB gain and final hearing
poorer than 45 dB
No improvement: <15 dB gain and final hearing poorer
than 75 dB
Tsounis et al12 Siegel criteria Severe 34 35 33 6/34 (18) 14/35 (40) 12/33 (36)
Ahn et al11 Siegel criteria Severe 60 60 NA 16/60 (27) 15/60 (25)
Lim et al8 Defined accordingly to the AAO-HNS2 Moderate 20 20 20 3/20 (15) 6/20 (30) 8/20 (40)
Complete recovery: Within 10 dB of the unaffected PTA to severe
Abbreviations: AAO-HNS, American Academy of Otolaryngology–Head and Neck Surgery; CB, combined treatment; IT, intratympanic treatment group;
NA, not available; PTA, pure tone average; ST, systemic treatment group.
cated no significant difference, and second, severe hearing loss, Combined Treatment vs Systemic Treatment
which indicated no significant difference. The heterogeneity Four studies investigated the CB vs ST group.8,9,11,12 In total,
was moderate but not significant. the studies comprised 301 patients, of whom 150 (49.8%) were
For the entire cohort comprising all 5 studies, the fixed- randomly allocated to the CB group and the remaining 151 pa-
effects model estimate indicated no significant difference be- tients (50.2%) randomized to the ST group. The definition of
tween the 2 groups, with an odds ratio of 0.94 (95% CI, 0.61 complete recovery varied between studies and is listed in
to 1.44). The heterogeneity was low and not significant Table 2. All studies had a mean PTA at baseline correspond-
(I2 = 34.5%; χ2 P = .19; Figure 2). ing to severe hearing loss according to Goodman criteria ex-
E4 JAMA Otolaryngology–Head & Neck Surgery Published online March 12, 2020 (Reprinted) jamaotolaryngology.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss Original Investigation Research
Figure 2. Odds for Complete Recovery When Treated With Intratympanic Corticosteroids vs Systemic Corticosteroids
Intratympanic Group Systemic Treatment Group Favors Favors
Not Not Systemic Intratympanic Weight,
Study Complete Complete Total Complete Complete Total OR (95% CI) Treatment Treatment %
Severe PTA at baseline
Tsounis et al,12 2018 6 28 34 14 21 35 0.32 (0.11-0.98) 15.08
Hong et al,10 2009 10 22 32 9 22 31 1.11 (0.38-3.26) 16.05
Rauch et al,14 2011 32 97 129 25 96 121 1.27 (0.70-2.30) 52.71
Sum for severe fixed-effects 0.97 (0.60-1.55)
modela
Moderate to severe PTA at baseline
Lim et al,8 2013 3 17 20 6 14 20 0.41 (0.09-1.95) 7.69
Swachia et al,13 2016 5 15 20 4 18 22 1.50 (0.34-6.61) 8.47
Sum for moderate to severe 0.81 (0.28-2.37)
fixed-effects modelb
Fixed-effects model for all studiesc 0.94 (0.61-1.44) 100
0.05 0.37 2.72
OR (95% CI)
a
Complete indicates the proportion of patients achieving complete recovery as Q2 = 4.63; P = .10; I2 = 56.8%.
defined within the individual study. Not complete indicates the proportion of b
Q1 = 1.39; P = .24; I2 = 28.0%.
patients not achieving complete recovery. Total indicates number of patients in c
Q4 = 6.11; P = .19; I2 = 34.5%.
the study. OR indicates odds ratio; PTA, pure tone average.
Figure 3. Odds for Complete Recovery Between Combined Intratympanics (Dexamethasone or Methylprednisolone)
and Systemic Corticosteroids vs Systemic Corticosteroids
Combined Treatment Group Systemic Treatment Group Favors Favors
Not Not Systemic Combined Weight,
Study Complete Complete Total Complete Complete Total OR (95% CI) Treatment Treatment %
Severe PTA at baseline
Ahn et al,11 2008 15 45 60 16 44 60 0.92 (0.40-2.08) 36.05
Gundogan et al,9 2013 14 23 37 10 26 36 1.58 (0.59-4.24) 24.78
Tsounis et al,12 2018 12 21 33 14 21 35 0.86 (0.32-2.28) 25.11
Sum for severe fixed-effects 1.05 (0.62-1.79)
modela
Moderate to severe PTA at baseline
Lim et al,8 2013 8 12 20 6 14 20 1.56 (0.42-5.76) 14.06
Sum for moderate to severe 1.56 (0.42-5.76)
fixed-effects modelb
Fixed-effects model for all studiesc 1.11 (0.68-1.82) 100
0.15 0.5 1 2.5 5 10
OR (95% CI)
a
Complete indicates the proportion of patients achieving complete recovery as Q2 = 0.93; P = .63; I2 = 0%.
defined within the individual study. Not complete indicates the proportion of b
Q0 = 0; P > .99; I2 = 0%.
patients not achieving complete recovery. Total indicates number of patients in c
Q3 = 1.23; P = .75; I2 = 0%.
the study. OR indicates odds ratio; PTA, pure tone average.
cept for 1 study that corresponded to moderate to severe hear- geneity was low and not significant (I2 = 0%; χ2 P = 0.75)
ings loss8 (Table 1). The mean days until treatment initiation (Figure 3).
ranged between 4.0 to 9.6 days in the CB group and 3.1 and
7.1 days in the ST group. Follow-up ranged from 17 days to 3 Combined Treatment vs Intratympanic Treatment
months. One study did not report the duration of follow-up11 Two studies investigated the CB group compared with the IT
(eTable 1 in the Supplement). group,8,12 comprising a total of 107 eligible patients. The CB
For the CB group, complete recovery was achieved in 49 group consisted of 53 patients (50%), whereas the IT group con-
of 150 patients (33%), and for the ST group, complete recov- sisted of 54 patients (50%). Neither of the 2 studies solitarily
ery was achieved in 46 of 151 patients (30%) (Table 2). indicated any significant difference between the treatments;
The fixed-effects model estimated no significant differ- for severe hearing loss, the odds ratio was 2.7 (95% CI, 0.86
ence. The odds ratio was 1.11 (95% CI, 0.68 to 1.82). The hetero- to 8.27), and for the moderate to severe hearing loss, the odds
jamaotolaryngology.com (Reprinted) JAMA Otolaryngology–Head & Neck Surgery Published online March 12, 2020 E5
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
Research Original Investigation Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss
ratio was 3.78 (95% CI, 0.83 to 17.25) (eFigure 2 in the minimum 30 dB. Hence, this implies heterogeneity and we con-
Supplement). sequently excluded the article.
Further, none of the remaining 4 studies reported the PTA
mean gain in dB ± the standard deviation. Three of the four
studies defined complete recovery as a gain of a minimum 10
Discussion dB in PTA,20,25,26 whereas the remaining defined complete re-
This meta-analysis did not indicate any differences in hear- covery as a gain of a minimum 15 dB.27 Thus, recovery rates
ing outcomes for intratympanic vs systemic corticosteroids in were not graduated but dichotomous in association with
a first-line treatment of ISSNHL equivalent of a moderate to whether complete recovery was achieved. Consequently, if we
severe hearing loss. This was derived from several observa- included the 4 studies in this meta-analysis, we would have
tions: first, there was no mean difference in average PTA gain had to define a gain of 10 dB as criteria for achieving com-
between the IT and ST groups based on 4 studies, 8,12-14 and plete recovery. Therefore, we included studies with gradu-
second, there was no difference in the odds for recovery be- ated recovery exclusively.
tween the IT and ST groups based on 5 studies.8,10,12-14
Association With Future Clinical Practice and Research
Comparison With Existing Literature The International Consensus (ICON) on treating sudden sen-
In the investigation of the IT group vs the ST group, a meta- sorineural hearing loss is a product of a panel discussion at the
analysis applied a random-effects model to estimate a non- International Federation of Otorhinolaryngological Societies
significant mean difference between the 2 groups.19 We were 2017 ENT World Congress. The ICON Study agreed that the
surprised to learn that specific data apparently used from 2 of main limitations present in the current literature are associ-
the included studies did not appear in the original articles.7,20 ated with the wide heterogeneity, which characterizes the ini-
Further, the meta-analysis included Kosyakov et al,21 who re- tial hearing deficit and the amount of hearing recovery. Sys-
port baseline PTA characteristics as a mean (SD) 41.0 (12.87) temic steroids are considered as the current standard care;
dB and 37.1(16.67) dB, respectively. This indicates that an un- however, the evidence is debatable. The ICON Study pro-
known proportion of the included patients are not confined poses that the number of participants for future studies should
within the ISSNHL-definitory criteria of a minimum 30-dB be restricted to moderate to profound levels of hearing loss to
hearing loss.21 improve the comparability.28 This meta-analysis qualita-
Another meta-analysis applied a fixed-effects model to tively adds to this consensus.
estimate the effect sizes of the IT and ST group.22 The mean
difference in dB was reported significantly as 3.42 dB (95% Strengths and Limitations
CI, 0.17-6.67 dB; I2 = 37%; P = .04) in favor for the IT group. One major strength of meta-analyses of randomized studies
However, we are concerned of the validity of these results. is the reduced risk of bias. However, in general, the included
We observed that data from the Kosyakov et al 19 were studies did not provide a placebo: patients allocated to re-
included and used equivalently to the beforementioned ceive oral treatment should concomitantly be given intratym-
meta-analysis. Similarly, the meta-analysis included results panic placebo (and vice versa). When a placebo was not ad-
from the Battaglia et al7 study; however, this specific study ministered, randomization was not masked to the personnel
defined ISSNHL as a hearing loss of a minimum of 20 dB nor the patient. Thus, we associated all included studies with
and not 30 dB. The meta-analysis stated to have included a high risk of bias on masking and it cannot be denied that the
randomized trials exclusively. Therefore, we were surprised presented results were biased. We encountered other limita-
to learn that the included study of Filipo et al23 was clearly tions too: first, the individual studies applied different guide-
stated as nonrandomized. These observations might high- lines in evaluating hearing recovery. Complete recovery was
light some perspectives as to why findings remain contra- defined as a final PTA of at least 25 dB in 3 studies,10,12,13 at least
dictory and evidence-based recommendations have not yet 30 dB in 1 study14 and, finally, as a PTA within 10 dB from the
been established. unaffected ear in 1 study.8 The definitions of complete recov-
One randomized study concluded that patients in the CB ery were fairly comparable and similar; however, we could not
group had a significantly higher likelihood of hearing recov- adjust for the heterogeneity implied within the use of differ-
ery compared with the ST group.7 However, in addition to de- ent assessment schemes, nor the difference in baseline prog-
fining ISSNHL as a hearing loss of a minimum 20 dB, the mean nostic factors,29 including (1) time to treatment onset, (2) age
days to treatment was 4 days in the CB group vs 11 days in in at baseline, and (3) PTA at baseline. We observed that the mean
the ST group. Acknowledging time-to-treatment initiation as time to treatment onset varied no more than 7 days between
an important prognostic parameter, this baseline discrep- the studies (ST group range, 3.1-7.1 days; IT group, 3.4-10.1 days;
ancy is highly associated with treatment outcomes and could CB group, 4.0-9.6 days). We could not quantify the associa-
explain the results.24 tion of this difference with the results, but it has been esti-
Five randomized trials met the inclusion criteria but were mated that the treatment window is between 2 to 4 weeks from
not included for analysis.7,20,25-27 First, the previously men- the onset of symptoms.24,30 As the maximum duration be-
tioned study from Battaglia et al7 defined ISSNHL as a hear- tween the presentation of symptoms to treatment was 10.1
ing loss of a minimum 20 dB. This conflicts with the interna- days, we do not consider this aspect a limitation of signifi-
tional consensus that ISSNHL is defined as a hearing loss of cance. We observed that the mean age range at the time of
E6 JAMA Otolaryngology–Head & Neck Surgery Published online March 12, 2020 (Reprinted) jamaotolaryngology.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss Original Investigation Research
symptom presentation ranged between 45.9 to 56.9 years. at concise recommendations. Finally, there is the effect of ap-
Older age is often described as a prognostic factor,24,31 al- plying different corticosteroids. There is also an emerging ques-
though older age is not defined. Typically, the age described tion on whether differences in hearing outcomes exist be-
is presented as categories in the literature (eg, 20-29, 30-39) tween dexamethasone vs methylprednisolone. The literature
exclusively and is not treated as a continuous covariate. Thus, is sparse concerning this question, but it has been reported that
it is difficult to assess whether the presented mean ages of the no difference exists between the 2 drugs in association with
included studies has inherent bias; however, we have ob- intratympanic administration.33 Based on this, we do not in-
served that the older ages described in literature comprise the tuitively consider the application of different corticosteroids
age categories 70 to 79 years and 80 to 89years.24,31 There- to be a significant limitation; however, future randomized or
fore, we do not consider the varying mean ages as a limita- noninferiority trials should settle this question.
tion of significance, as we do not consider the age interval of
45.9 to 56.9 years to be older ages nor is presbycusis a rel-
evant parameter for patients in this age interval. Finally, we
do not consider the different PTA at baseline a limitation of sig-
Conclusions
nificance, as we allocated studies accordingly to mean PTA at We evaluated by meta-analysis the association between dif-
baseline and performed our analyses based on the stratifica- ferent administration routes of corticosteroids as first-line
tion according to Goodman criteria.32 We observed that fol- treatment of 710 patients with a diagnosis of ISSNHL. There
low-up in the included studies ranged from 17 days to 3 months. was no difference in therapeutic outcomes between the IT,
We cannot adjust for the inherent heterogeneity of varying fol- ST, and CB groups for patients with moderate to severe
low-up and this must be considered a limitation for arriving hearing loss.
ARTICLE INFORMATION Otolaryngol. 1980;106(12):772-776. doi:10.1001/ Pharmacol. 2016;27(4):371-377. doi:10.1515/jbcpp-
Accepted for Publication: January 8, 2020. archotol.1980.00790360050013 2015-0112
Published Online: March 12, 2020. 6. Moher D, Liberati A, Tetzlaff J, Altman DG; 14. Rauch SD, Halpin CF, Antonelli PJ, et al. Oral vs
doi:10.1001/jamaoto.2020.0047 PRISMA Group. Preferred reporting items for intratympanic corticosteroid therapy for idiopathic
systematic reviews and meta-analyses: the PRISMA sudden sensorineural hearing loss: a randomized
Author Contributions: Drs Mirian and Ovesen had statement. BMJ. 2009;339:b2535. doi:10.1136/ trial. JAMA. 2011;305(20):2071-2079. doi:10.1001/
full access to all of the data in the study and take bmj.b2535 jama.2011.679
responsibility for the integrity of the data and the
accuracy of the data analysis. 7. Battaglia A, Burchette R, Cueva R. Combination 15. Higgins JPT, Altman DG, Gøtzsche PC, et al;
Concept and design: All authors. therapy (intratympanic dexamethasone + Cochrane Bias Methods Group; Cochrane Statistical
Acquisition, analysis, or interpretation of data: high-dose prednisone taper) for the treatment of Methods Group. The Cochrane Collaboration’s tool
All authors. idiopathic sudden sensorineural hearing loss. Otol for assessing risk of bias in randomised trials. BMJ.
Drafting of the manuscript: All authors. Neurotol. 2008;29(4):453-460. doi:10.1097/MAO. 2011;343:d5928. doi:10.1136/bmj.d5928
Critical revision of the manuscript for important 0b013e318168da7a 16. Higgins JPT, Thompson SG, Deeks JJ, Altman
intellectual content: All authors. 8. Lim HJ, Kim YT, Choi SJ, et al. Efficacy of 3 DG. Measuring inconsistency in meta-analyses. BMJ.
Statistical analysis: Mirian. different steroid treatments for sudden 2003;327(7414):557-560. doi:10.1136/bmj.327.
Supervision: All authors. sensorineural hearing loss: a prospective, 7414.557
Conflict of Interest Disclosures: None reported. randomized trial. Otolaryngol Head Neck Surg. 17. Viechtbauer W. Conducting meta-analyses
2013;148(1):121-127. doi:10.1177/0194599812464475 in R with the metafor package. J Stat Softw. 2010;
Additional Contributions: This study has been
supervised by a certified statistician at the Section 9. Gundogan O, Pinar E, Imre A, Ozturkcan S, 36(3):1. doi:10.18637/jss.v036.i03
of Biostatistics at Department of Public Health, Cokmez O, Yigiter AC. Therapeutic efficacy of the 18. Furuhashi A, Matsuda K, Asahi K, Nakashima T.
University of Aarhus, Aarhus, Denmark. combination of intratympanic methylprednisolone Sudden deafness: long-term follow-up and
and oral steroid for idiopathic sudden deafness. recurrence. Clin Otolaryngol Allied Sci. 2002;27(6):
REFERENCES Otolaryngol Head Neck Surg. 2013;149(5):753-758. 458-463. doi:10.1046/j.1365-2273.2002.00612.x
doi:10.1177/0194599813500754
1. Rauch SD. Clinical practice: idiopathic sudden 19. Lai D, Zhao F, Jalal N, Zheng Y. Intratympanic
sensorineural hearing loss. N Engl J Med. 2008;359 10. Hong SM, Park CH, Lee JH. Hearing outcomes glucocorticosteroid therapy for idiopathic sudden
(8):833-840. doi:10.1056/NEJMcp0802129 of daily intratympanic dexamethasone alone as a hearing loss: meta-analysis of randomized
primary treatment modality for ISSHL. Otolaryngol controlled trials. Medicine (Baltimore). 2017;96(50):
2. Stachler RJ, Chandrasekhar SS, Archer SM, et al; Head Neck Surg. 2009;141(5):579-583. doi:10.1016/
American Academy of Otolaryngology-Head and e8955. doi:10.1097/MD.0000000000008955
j.otohns.2009.08.009
Neck Surgery. Clinical practice guideline: sudden 20. Dispenza F, Amodio E, De Stefano A, et al.
hearing loss. Otolaryngol Head Neck Surg. 2012;146 11. Ahn JH, Yoo MH, Yoon TH, Chung JW. Can Treatment of sudden sensorineural hearing loss
(3)(suppl):S1-S35. doi:10.1177/0194599812436449 intratympanic dexamethasone added to systemic with transtympanic injection of steroids as single
steroids improve hearing outcome in patients with therapy: a randomized clinical study. Eur Arch
3. Byl FMJ Jr. Sudden hearing loss: eight years’ sudden deafness? Laryngoscope. 2008;118(2):279-
experience and suggested prognostic table. Otorhinolaryngol. 2011;268(9):1273-1278. doi:10.
282. doi:10.1097/MLG.0b013e3181585428 1007/s00405-011-1523-0
Laryngoscope. 1984;94(5 Pt 1):647-661. doi:10.1288/
00005537-198405000-00014 12. Tsounis M, Psillas G, Tsalighopoulos M, Vital V, 21. Kosyakov S, Atanesyan A, Gunenkov A,
Maroudias N, Markou K. Systemic, intratympanic Ashkhatunyan E, Kurlova A. Intratympanic steroids
4. Simmons FB. Sudden idiopathic sensori-neural and combined administration of steroids for sudden
hearing loss: some observations. Laryngoscope. for sudden sensorineural hearing loss. J Int Adv Otol.
hearing loss: a prospective randomized multicenter 2011;7:323-332. https://www.advancedotology.org/
1973;83(8):1221-1227. doi:10.1288/00005537- trial. Eur Arch Otorhinolaryngol. 2018;275(1):103-110.
197308000-00005 en/intratympanic-steroids-for-sudden-
doi:10.1007/s00405-017-4803-5 sensorineural-hearing-loss-161247.
5. Wilson WR, Byl FM, Laird N. The efficacy of 13. Swachia K, Sharma D, Singh J. Efficacy of oral Accessed August 1, 2018.
steroids in the treatment of idiopathic sudden vs. intratympanic corticosteroids in sudden
hearing loss: a double-blind clinical study. Arch 22. Qiang Q, Wu X, Yang T, Yang C, Sun H. A
sensorineural hearing loss. J Basic Clin Physiol comparison between systemic and intratympanic
jamaotolaryngology.com (Reprinted) JAMA Otolaryngology–Head & Neck Surgery Published online March 12, 2020 E7
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
Research Original Investigation Intratympanic vs Systemic Corticosteroids in First-line Treatment of Idiopathic Sudden Sensorineural Hearing Loss
steroid therapies as initial therapy for idiopathic sudden hearing loss.Otol Neurotol. 2013;34(4):771- 31. Nosrati-Zarenoe R, Arlinger S, Hultcrantz E.
sudden sensorineural hearing loss: a meta-analysis. 776. doi:10.1097/MAO.0b013e31828bb567 Idiopathic sudden sensorineural hearing loss:
Acta Otolaryngol. 2017;137(6):598-605. 27. Arastou S, Tajedini A, Borghei P. Combined results drawn from the Swedish national database.
doi:10.1080/00016489.2016.1260157 intratympanic and systemic steroid therapy for Acta Otolaryngol. 2007;127(11):1168-1175.
23. Filipo R, Attanasio G, Russo FY, et al. Oral versus poor-prognosis sudden sensorineural hearing loss. doi:10.1080/00016480701242477
short-term intratympanic prednisolone therapy for Iran J Otorhinolaryngol. 2013;25(70):23-28. 32. Anyah A, Mistry D, Kevern E, Markiewicz K.
idiopathic sudden hearing loss. Audiol Neurootol. 28. Marx M, Younes E, Chandrasekhar SS, et al. Idiopathic sudden sensorineural hearing loss:
2014;19(4):225-233. doi:10.1159/000360069 International consensus (ICON) on treatment of average time elapsed before presentation to the
24. Hara JH, Zhang JA, Gandhi KR, et al. Oral and sudden sensorineural hearing loss. Eur Ann otolaryngologist and effectiveness of oral and/or
intratympanic steroid therapy for idiopathic sudden Otorhinolaryngol Head Neck Dis. 2018;135(1S):S23- intratympanic steroids in late presentations. Cureus.
sensorineural hearing loss. Laryngoscope Investig S28. doi:10.1016/j.anorl.2017.12.011 2017;9(12):e1945-e1945. doi:10.7759/cureus.1945
Otolaryngol. 2018;3(2):73-77. doi:10.1002/lio2.148 29. Kang WS, Yang CJ, Shim M, et al. Prognostic 33. Tarkan Ö, Dağkıran M, Sürmelioğlu Ö, et al.
25. Arslan N, Oğuz H, Demirci M, et al. Combined factors for recovery from sudden sensorineural Intratympanic methylprednisolone versus
intratympanic and systemic use of steroids for hearing loss: a retrospective study. J Audiol Otol. dexamethasone for the primary treatment of
idiopathic sudden sensorineural hearing loss.Otol 2017;21(1):9-15. doi:10.7874/jao.2017.21.1.9 idiopathic sudden sensorineural hearing loss. J Int
Neurotol. 2011;32(3):393-397. doi:10.1097/MAO. Adv Otol. 2018;14(3):451-455. doi:10.5152/
30. Mattox DE, Simmons FB. Natural history of iao.2018.4871
0b013e318206fdfa sudden sensorineural hearing loss. Ann Otol Rhinol
26. Koltsidopoulos P, Bibas A, Sismanis A, Tzonou Laryngol. 1977;86(4 Pt 1):463-480. doi:10.1177/
A, Seggas I. Intratympanic and systemic steroids for 000348947708600406
E8 JAMA Otolaryngology–Head & Neck Surgery Published online March 12, 2020 (Reprinted) jamaotolaryngology.com
© 2020 American Medical Association. All rights reserved.
Downloaded From: https://jamanetwork.com/ by a Uppsala University User on 03/12/2020
You might also like
- Diagnostic Problems in Tumors of Central Nervous System: Selected TopicsFrom EverandDiagnostic Problems in Tumors of Central Nervous System: Selected TopicsNo ratings yet
- Ef Tek Harian 2015Document6 pagesEf Tek Harian 2015neuro a2021No ratings yet
- Demirhan 2018Document5 pagesDemirhan 2018darmayanti ibnuNo ratings yet
- Cat OrceDocument22 pagesCat OrceCAMEVANo ratings yet
- Articles: Up To 21% of Adults Will Develop Tinnitus, Which Is One of The Most Distressing and Debilitating AudiologicalDocument9 pagesArticles: Up To 21% of Adults Will Develop Tinnitus, Which Is One of The Most Distressing and Debilitating AudiologicalAlex FloresNo ratings yet
- Sevil 2015Document8 pagesSevil 2015neuro a2021No ratings yet
- Tinitus 4Document6 pagesTinitus 4SiFa Imah RhieshaNo ratings yet
- Impact of Antiplatelet Therapy During Endovascular Therapy For Tandem OcclusionsDocument8 pagesImpact of Antiplatelet Therapy During Endovascular Therapy For Tandem Occlusionsrifki irsyadNo ratings yet
- Methylprednisolone Vs Dexamethasone For Control VertigoDocument8 pagesMethylprednisolone Vs Dexamethasone For Control VertigoBrando PanjaitanNo ratings yet
- BAHRUN - Ondansetron in Patients With TinnitusDocument8 pagesBAHRUN - Ondansetron in Patients With TinnitusBahRunNo ratings yet
- Oral Vs Intratympanic Corticosteroid Therapy For Idiopathic Sudden Sensorineural Hearing LossDocument9 pagesOral Vs Intratympanic Corticosteroid Therapy For Idiopathic Sudden Sensorineural Hearing LossYusmiatiNo ratings yet
- Jurding THTDocument4 pagesJurding THTCharlina Amelia Br-BarusNo ratings yet
- jao-21-9Document7 pagesjao-21-9Miss AmyNo ratings yet
- International Journal of Pediatric OtorhinolaryngologyDocument4 pagesInternational Journal of Pediatric OtorhinolaryngologyDear Farah SielmaNo ratings yet
- Nonsedation or Light Sedation in Critically IllDocument9 pagesNonsedation or Light Sedation in Critically IllPutra SetiawanNo ratings yet
- Articles: BackgroundDocument14 pagesArticles: BackgroundinescubertaNo ratings yet
- Measurement of Correlation Between Dizziness Handicapped Inventory and Pure Tone Audiometry For Early Diagnosis of Menieres DiseaseDocument6 pagesMeasurement of Correlation Between Dizziness Handicapped Inventory and Pure Tone Audiometry For Early Diagnosis of Menieres DiseaseIJAR JOURNALNo ratings yet
- Electronic Physician (ISSN: 2008-5842) : 1.1. BackgroundDocument5 pagesElectronic Physician (ISSN: 2008-5842) : 1.1. BackgroundFi NoNo ratings yet
- Pre-Treatment Ongoing Cortical Oscillatory Activity Predicts Improvement of Tinnitus After Partial Peripheral Reafferentation With Hearing AidsDocument11 pagesPre-Treatment Ongoing Cortical Oscillatory Activity Predicts Improvement of Tinnitus After Partial Peripheral Reafferentation With Hearing AidsFelipe Asenjo ÁlvarezNo ratings yet
- Hearing Outcomes in Small Acoustic Neuroma ManagementDocument9 pagesHearing Outcomes in Small Acoustic Neuroma ManagementNindya AugestiNo ratings yet
- The Effect of Transcutaneous Electrical Nerve Stimulation (TENS) On Chronic Subjective TinnitusDocument5 pagesThe Effect of Transcutaneous Electrical Nerve Stimulation (TENS) On Chronic Subjective TinnitusSameer AlladinNo ratings yet
- Nosrati Zarenoe2012Document9 pagesNosrati Zarenoe2012neuro a2021No ratings yet
- A Preliminary Report On The Investigation of Prestin As A Biomarker For Idiopathic Sudden Sensorineural Hearing LossDocument4 pagesA Preliminary Report On The Investigation of Prestin As A Biomarker For Idiopathic Sudden Sensorineural Hearing LossNoviTrianaNo ratings yet
- 58420_CE (Vi)_F[SK]_PF1(AG_KM)_PN(KM)Document4 pages58420_CE (Vi)_F[SK]_PF1(AG_KM)_PN(KM)parimaladvnNo ratings yet
- PatersonDocument6 pagesPatersonCristhian Jover CastroNo ratings yet
- Acupuncture For Anxiety in Dental Patients Systematic Review and 2018Document39 pagesAcupuncture For Anxiety in Dental Patients Systematic Review and 2018Marcio OliveiraNo ratings yet
- YgukhnDocument6 pagesYgukhnPin Han NaNo ratings yet
- NIH Public AccessDocument3 pagesNIH Public AccessCamilo MoraNo ratings yet
- Sedacion Ligera en UciaDocument9 pagesSedacion Ligera en UciaDario Neri CortezNo ratings yet
- A Comparison of Effects of Systemic and Intratympanic Steroid Therapies For Sudden Sensorineural Hearing Loss: A Meta-AnalysisDocument6 pagesA Comparison of Effects of Systemic and Intratympanic Steroid Therapies For Sudden Sensorineural Hearing Loss: A Meta-AnalysisIndahEkaPutriNo ratings yet
- Effect of Antioxidant Vitamins As Adjuvant Therapy For Sudden Sensorineural Hearing Loss: Systematic Review StudyDocument7 pagesEffect of Antioxidant Vitamins As Adjuvant Therapy For Sudden Sensorineural Hearing Loss: Systematic Review Studyfpm5948No ratings yet
- WNL 2022 201671Document14 pagesWNL 2022 201671PeyepeyeNo ratings yet
- Ketamine Vs Haloperidol For Prevention of CognitivDocument8 pagesKetamine Vs Haloperidol For Prevention of CognitivSilvia MoraNo ratings yet
- Sudden Hearing Loss: An Effectivity Comparison of Intratympanic and Systemic Steroid TreatmentsDocument7 pagesSudden Hearing Loss: An Effectivity Comparison of Intratympanic and Systemic Steroid Treatmentsneuro a2021No ratings yet
- Implante y TinnitusDocument6 pagesImplante y TinnitusjavierNo ratings yet
- fneur-13-962376 (1)Document8 pagesfneur-13-962376 (1)Miss AmyNo ratings yet
- Jama Andersen 2021 Oi 210108 1632503925.26159Document9 pagesJama Andersen 2021 Oi 210108 1632503925.26159AlizaPinkyNo ratings yet
- Davis 2008Document11 pagesDavis 2008Suchada SangpetchNo ratings yet
- Casani 2011Document8 pagesCasani 2011Anamaria SNo ratings yet
- Low Dose Intratympanic Gentamicin For Control of Intractable VertigoDocument9 pagesLow Dose Intratympanic Gentamicin For Control of Intractable VertigoJose ManuelNo ratings yet
- Status and Clinical Experiences From The Challenge Trial - A Randomized Controlled Trial Investigating Virtual Reality-Based Therapy For Auditory HallucinationsDocument6 pagesStatus and Clinical Experiences From The Challenge Trial - A Randomized Controlled Trial Investigating Virtual Reality-Based Therapy For Auditory HallucinationsKatalin VikukNo ratings yet
- 9. Analysis of Prognostic Factors. yukselDocument6 pages9. Analysis of Prognostic Factors. yukselMiss AmyNo ratings yet
- 2018 - AJA-18-0085 FaltaDocument7 pages2018 - AJA-18-0085 FaltaLuis Fernando GarciaNo ratings yet
- Variations of High Frequency Parameter of Heart Rate Variability Following Osteopathic Manipulative TreatmentDocument13 pagesVariations of High Frequency Parameter of Heart Rate Variability Following Osteopathic Manipulative Treatmentthe_walnutNo ratings yet
- Acupuncture for Immediate Tinnitus ReliefDocument11 pagesAcupuncture for Immediate Tinnitus ReliefMauricio RodriguezNo ratings yet
- Intratympanic Mixture Gentamicin and De... Asone For Unilateral Meniere - S DiseaseDocument4 pagesIntratympanic Mixture Gentamicin and De... Asone For Unilateral Meniere - S DiseaseMarianneTee-ruhNo ratings yet
- Research Report: BackgroundDocument10 pagesResearch Report: BackgroundVenice Marie CordetaNo ratings yet
- Smartphone-Based Hearing Test As An Aid in The Initial Evaluation of Unilateral Sudden Sensorineural Hearing LossDocument8 pagesSmartphone-Based Hearing Test As An Aid in The Initial Evaluation of Unilateral Sudden Sensorineural Hearing LossAnsyah EdisonNo ratings yet
- Nature Sound-Pasien Coronary ArteriographyDocument10 pagesNature Sound-Pasien Coronary ArteriographyDwi AndayaniNo ratings yet
- Haloperidol For The Treatment of Delirium in ICU PatientsDocument11 pagesHaloperidol For The Treatment of Delirium in ICU PatientsArgenis SalinasNo ratings yet
- Overminus Lens Therapy For Children 3 To 10 Years of Age With Intermittent Exotropia JAMA Ophthalmol 2021Document13 pagesOverminus Lens Therapy For Children 3 To 10 Years of Age With Intermittent Exotropia JAMA Ophthalmol 2021Shirley M. Cerro RomeroNo ratings yet
- Fneur 14 1138354Document14 pagesFneur 14 1138354diego.arancibianutNo ratings yet
- Costae - Bedah DDocument41 pagesCostae - Bedah Dchoco coffeNo ratings yet
- JRMS 18 43Document4 pagesJRMS 18 43Ricardo PietrobonNo ratings yet
- Comparative Efficacy and Tolerability of 32 Oral Antipsychotics For The Acute Treatment of Adults With Multi-Episode Schizophrenia PDFDocument13 pagesComparative Efficacy and Tolerability of 32 Oral Antipsychotics For The Acute Treatment of Adults With Multi-Episode Schizophrenia PDFfrancesca_valdiviaNo ratings yet
- 407-Article Text-935-1-10-20210102Document7 pages407-Article Text-935-1-10-20210102Raditya Maulana AkbarNo ratings yet
- Jamapsychiatry Thyrian 2017 Oi 170051Document9 pagesJamapsychiatry Thyrian 2017 Oi 170051Francisco Javier RamosNo ratings yet
- New 2Document3 pagesNew 2Aldy Putra UltrasNo ratings yet
- Accepted Manuscript: Complementary Therapies in MedicineDocument19 pagesAccepted Manuscript: Complementary Therapies in MedicinePaskah Parlaungan PurbaNo ratings yet
- In Ammatory Indicators in Peripheral Blood in Sudden Sensorineural Hearing Loss Patients With Different Shape of AudiogramsDocument6 pagesIn Ammatory Indicators in Peripheral Blood in Sudden Sensorineural Hearing Loss Patients With Different Shape of AudiogramsAnnisa Dhiya UlhaqNo ratings yet
- Klotz 2017Document13 pagesKlotz 2017neuro a2021No ratings yet
- Klotz 2017Document13 pagesKlotz 2017neuro a2021No ratings yet
- Tea and Coffee Consumption and Risk of Laryngeal Cancer: A Systematic Review Meta-AnalysisDocument15 pagesTea and Coffee Consumption and Risk of Laryngeal Cancer: A Systematic Review Meta-Analysisneuro a2021No ratings yet
- Sudden Hearing Loss: An Effectivity Comparison of Intratympanic and Systemic Steroid TreatmentsDocument7 pagesSudden Hearing Loss: An Effectivity Comparison of Intratympanic and Systemic Steroid Treatmentsneuro a2021No ratings yet
- Nosrati Zarenoe2012Document9 pagesNosrati Zarenoe2012neuro a2021No ratings yet
- Nosrati Zarenoe2012Document9 pagesNosrati Zarenoe2012neuro a2021No ratings yet
- Tea and Coffee Consumption and Risk of Laryngeal Cancer: A Systematic Review Meta-AnalysisDocument15 pagesTea and Coffee Consumption and Risk of Laryngeal Cancer: A Systematic Review Meta-Analysisneuro a2021No ratings yet
- 10 1001@jamaoto 2020 0047Document8 pages10 1001@jamaoto 2020 0047neuro a2021No ratings yet
- Sudden Hearing Loss: An Effectivity Comparison of Intratympanic and Systemic Steroid TreatmentsDocument7 pagesSudden Hearing Loss: An Effectivity Comparison of Intratympanic and Systemic Steroid Treatmentsneuro a2021No ratings yet
- Digital Portable 4.0/8.0 KW Dragon LW System Digital Portable 4.0/8.0 KW Dragon LW SystemDocument8 pagesDigital Portable 4.0/8.0 KW Dragon LW System Digital Portable 4.0/8.0 KW Dragon LW Systemteacher_17No ratings yet
- SCIENTIFIC BASIS OF HUMAN MOVEMENT EFFECTS OF EXERCISE ON RESPIRATORY SYSTEM - Wbshce PDFDocument9 pagesSCIENTIFIC BASIS OF HUMAN MOVEMENT EFFECTS OF EXERCISE ON RESPIRATORY SYSTEM - Wbshce PDFlancetNo ratings yet
- PilatesDocument65 pagesPilatesAna MariaNo ratings yet
- Separation of Plant Pigments PDFDocument3 pagesSeparation of Plant Pigments PDFneelNo ratings yet
- Unika Hole SawDocument21 pagesUnika Hole SawQin DieselNo ratings yet
- Vacon NXP System Drive Hardware Manual DPD01365A UDocument72 pagesVacon NXP System Drive Hardware Manual DPD01365A UTanuTiganu100% (3)
- ASTM C309: Do Liquid Hardeners Meet This Standard?Document2 pagesASTM C309: Do Liquid Hardeners Meet This Standard?Kishore Nayak kNo ratings yet
- 2 TABLE 1.1. Key Events in The Development of Cell and Tissue CultureDocument1 page2 TABLE 1.1. Key Events in The Development of Cell and Tissue CultureCatalina ColoradoNo ratings yet
- Service ProgramDocument47 pagesService ProgramHuseyn aliyevNo ratings yet
- Fenergo's KYC Efficiently Manages ComplianceDocument4 pagesFenergo's KYC Efficiently Manages ComplianceTEL COMENo ratings yet
- TWC FLC H-2B Job Posting Request Form Transmittal InformationDocument4 pagesTWC FLC H-2B Job Posting Request Form Transmittal InformationEnrique padillaNo ratings yet
- DM tipe I dan II: Etiologi, Patofisiologi, dan KomplikasiDocument2 pagesDM tipe I dan II: Etiologi, Patofisiologi, dan KomplikasiAngel da CostaNo ratings yet
- L23Document29 pagesL23Mary MorseNo ratings yet
- IOC CoachingResearchStudiesList PDFDocument87 pagesIOC CoachingResearchStudiesList PDFJeane LucenaNo ratings yet
- Benefits of SwimmingDocument3 pagesBenefits of Swimmingaybi pearlNo ratings yet
- Arduino CertificationDocument8 pagesArduino Certificationhack reportNo ratings yet
- 12 29 11editionDocument27 pages12 29 11editionSan Mateo Daily JournalNo ratings yet
- Dont Sweat The Small Stuff For Men - Richard CarlsonDocument226 pagesDont Sweat The Small Stuff For Men - Richard CarlsonAaliyah Csmrt100% (1)
- 6 Ijasrjun20196Document8 pages6 Ijasrjun20196TJPRC PublicationsNo ratings yet
- The Three Modern Relationship Models and Why They Are All FlawedDocument5 pagesThe Three Modern Relationship Models and Why They Are All FlawedBingoNo ratings yet
- The Thermal ConductivityDocument6 pagesThe Thermal ConductivityLuc LeNo ratings yet
- 2019 PSRANM Conference Program FinalDocument24 pages2019 PSRANM Conference Program FinalKimmie JordanNo ratings yet
- Worksheet. 5. Sexual Reproduction in PlantDocument4 pagesWorksheet. 5. Sexual Reproduction in PlantLeonita SwandjajaNo ratings yet
- Comparison Between VR, PM and Hybrid Stepper MotorsDocument2 pagesComparison Between VR, PM and Hybrid Stepper MotorsMuhammed IfkazNo ratings yet
- Narayani and Soham Remedies by Jaco Malan Descriptions & RatesDocument40 pagesNarayani and Soham Remedies by Jaco Malan Descriptions & RatesAlex VimanNo ratings yet
- Sample Cylinders - PGI-CYLDocument8 pagesSample Cylinders - PGI-CYLcalpeeNo ratings yet
- Alcohol Facts and Statistics: Alcohol Use in The United StatesDocument6 pagesAlcohol Facts and Statistics: Alcohol Use in The United StatesVictor EnemNo ratings yet
- Paper 4 Nov 2000Document2 pagesPaper 4 Nov 2000MSHNo ratings yet
- Imaging-Guided Chest Biopsies: Techniques and Clinical ResultsDocument10 pagesImaging-Guided Chest Biopsies: Techniques and Clinical Resultsweni kartika nugrohoNo ratings yet
- Tutorial SessionDocument5 pagesTutorial SessionKhánh LinhNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (20)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (5)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)























![58420_CE (Vi)_F[SK]_PF1(AG_KM)_PN(KM)](https://imgv2-2-f.scribdassets.com/img/document/720580790/149x198/906bbee0db/1712407097?v=1)