Professional Documents
Culture Documents
Wound Management For The 21st Century: Combining Effectiveness and Efficiency
Uploaded by
Heba VerebceanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wound Management For The 21st Century: Combining Effectiveness and Efficiency
Uploaded by
Heba VerebceanCopyright:
Available Formats
International Wound Journal ISSN 1742-4801
REVIEW ARTICLE
Wound management for the 21st century: combining
effectiveness and efficiency
Christina Lindholm1 & Richard Searle2
1 Sophiahemmet University, Stockholm, Sweden
2 Smith & Nephew Medical Ltd, Hull, UK
Key words Lindholm C, Searle R. Wound management for the 21st century: combining effective-
Efficiency; Health economics; Resources; ness and efficiency. Int Wound J 2016; 13 (suppl. S2):5–15
Service improvement; Wound healing
Abstract
Correspondence to
Treatment of wounds of different aetiologies constitutes a major part of the total health
R Searle, PhD care budget. It is estimated that 1⋅5–2 million people in Europe suffer from acute
Health Economics Manager or chronic wounds. These wounds are managed both in hospitals and in community
Smith & Nephew Medical Ltd care. The patients suffering from these wounds report physical, mental and social
Hull, UK consequences of their wounds and the care of them. It is often believed that the use
E-mail: Richard.Searle@Smith-Nephew.com
of wound dressings per se is the major cost driver in wound management, whereas
in fact, nursing time and hospital costs are together responsible for around 80–85%
doi: 10.1111/iwj.12623
of the total cost. Healing time, frequency of dressing change and complications are
three important cost drivers. However, with the use of modern, advanced technology
for more rapid wound healing, all these cost drivers can be substantially reduced. A
basic understanding of the terminology and principles of Health Economics in relation
to wound management might therefore be of interest.
The impact of wounds on the health system – a wounds [defined as wounds that fail to heal with ‘standard
growing challenge therapy’ in an orderly and timely manner (5)] cause further
deterioration in quality of life and increase the burden on the
Wounds have been called ‘The Silent Epidemic’ health care system over a prolonged period.
Wounds have a variety of causes; some arise from surgical Sometimes, it is thought that the financial cost of wound
intervention, some are the result of injury, and others are a management is just the cost of the materials used, such as
consequence of extrinsic factors, such as pressure or shear, dressings, bandages or topical antiseptics. This is not the case;
or underlying conditions such as diabetes or vascular disease. most of the cost relates to the use of health care professionals’
time and the cost of staying in hospital, as we will see later. The
They are often classified as a result of their underlying cause
choice of materials and treatments, however, can have a major
into acute wounds, such as surgical wounds and burns, and
influence on the total cost.
chronic wounds, such as leg ulcers, diabetic foot ulcers (DFUs)
and pressure ulcers (1). Whatever the cause, wounds have a
substantial but often unrecognised impact on those who suffer How many people in the population have wounds?
from them, on their carers and on the health care system. In Prevalence surveys in the UK and Denmark indicate that there
fact, the phenomenon of wounds has been called the ‘Silent are about three to four people with one or more wounds
Epidemic’ (2). per 1000 population (6–9).∗ Many of these wounds become
Living with a wound can have a profound effect on quality ‘chronic’, with studies reporting that around 15% of wounds
of life (3). The human cost of wounds manifests itself in, remain unresolved 1 year after presentation (7), often resulting
among other things, pain, distress, social isolation, anxiety, in a prolonged, yet avoidable, burden to patients, their families
extended hospital stay, chronic morbidity or even mortality. and health systems. Based on the above figures, it is estimated
Many of these issues are preventable (4). Furthermore, because that in a population of 1 million people, approximately 3500
of underlying factors such as the age of the patient and the
presence of underlying chronic comorbidities, some wounds ∗ Hospitaland community data from Denmark were combined to give a
do not follow the normal healing process. These ‘hard-to-heal’ prevalence of around three people with a wound per 1000 population
© 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd 5
Wound management for the 21st century C. Lindholm & R. Searle
people will be living with a wound, of which, 525 will have infections or amputations occur, with a study from the USA
had their wound for over 1 year. reporting a cost per amputation of $38 077 (13).
The majority of chronic wounds are treated in non-acute The costs of managing surgical wounds are equally difficult
health care settings, such as clinics or home health (7–9). to estimate with any accuracy. The management of an uncom-
Studies suggest that wound management accounts for over plicated surgical incision is relatively inexpensive; however,
half of community health nurse resources in European settings when infections occur, these costs can increase significantly. A
(4,10). However, a substantial number of people with wounds study from the USA estimated the costs of treating a surgical
require hospital treatment at some stage, which can escalate the site infection (SSI) to be approximately $20 800 (18).
costs of care significantly (4,11). Previous studies have sug- As well as costs incurred by the health system, there are also
gested that between 27% and 50% of hospital beds are occupied significant indirect costs that fall on individuals and the broader
by patients requiring some form of wound management (4). economy. In the USA, it has been estimated that venous ulcers
cause the loss of 2 million working days per year, costing the US
health care system an estimated $2⋅5–3⋅5 billion annually (13).
Prevalence of wounds
There are estimated to be around 1⋅5–2 million people
living with a chronic wound across Europe (12). In the The total cost of treating wounds
USA, chronic wounds affect around 6⋅5 million people at Wound management has been estimated to account for 3%
any one time (13). of all health care expenditure (2).
Data from Europe suggest that 64% of wounds treated in The cost of treating pressure ulcers alone in the USA is
home care were chronic in aetiology (7). Of these, 24% are estimated to be $11 billion/year (13).
estimated to have been living with their wound for 6 months In Europe, the cost o7f managing DFUs is estimated to be
or more, and almost 16% had remained unhealed for a year €4–6 billion/year (4).
or more (9). In the USA, foot ulcers and other complications are
Audit data from hospital settings suggest that as many as ‘responsible for 20% of the nearly 3 million hospitalisa-
50% of in-patients have a wound. A study of 5800 patients tions every year related to diabetes’ (13).
in Western Australian public hospitals found that 49% The cost per case is highly dependent on a number of
had a wound. 31% of patients had acute wounds, 9% had factors, such as wound type, complications and the site
pressure ulcers and 8% had skin tears. The authors stated of care. For example, uncomplicated surgical wounds are
their belief that a quarter of these wounds had the potential relatively inexpensive to manage, but costs increase sharply
to be prevented (14). if infection occurs. In Europe, surgical wound infection is
Data from the USA demonstrate a pressure ulcer preva- estimated to add, on average, 11 days to in-patient hospital
lence of 22% in acute critical care settings (13). Audit stay, with an average cost of €5800 per case (19), whilst
data from Europe indicate that 22⋅7% of hospital patients data from the USA suggest that the cost of treating a
had signs of pressure damage [Bermark et al. 2004 (15), surgical site infection (SSI) is in excess of $20 000 (18).
reported in Posnett et al. 2009 (4)]. A hospital performing 10 000 operations annually can
expect 300–400 infections, resulting in 3300–4000 excess
bed-days, ∼€1⋅74–2⋅32 m in excess costs and 15–20
infection-attributable deaths (20).
Wounds result in a significant economic cost
to the health care system
Wounds are estimated to account for almost 3% of total health
system costs (2) – approximately £5billion annually according The cost of managing wounds is largely hidden,
to data from the UK (16). A recent study in Wales showed that and the impact is often not recognised
the cost of managing patients with chronic wounds amounted to Much of the financial cost of treating wounds is hidden because
5⋅5% of total health service expenditure (17). Most of this cost many health care professionals across a wide range of profes-
relates to hospital stay and nursing time for treating patients at sions and care settings are involved, and so, the total cost is
home or in clinics, whereas materials such as dressings account spread across many different budgets. As a result, their impact
for a small part of the total cost. In the USA, it is reported goes largely unrecognised by policy makers, is poorly under-
that over US$25 billion is spent each year on the treatment of stood by health care system decision makers and is seldom
chronic wounds (13). reported in the media (2).
At an individual level, the costs of managing wounds are Studies have found that between 70–80% of wound patients
highly dependent on the wound type, complexity and site of are treated in the community, predominantly by community
care. A study from Sweden in 2002 found that the weekly cost nurses (9,20). Managing wounds is often the single most impor-
of managing a venous leg ulcer (VLU) was around €103 per tant use of their time – one study estimated that over 60% of
patient, with annual costs estimated to be between €1332–2585 community nurses’ time was spent on dressing changes (21).
(4). DFUs are estimated to be more costly to treat than VLUs, Studies in the UK and Denmark have shown that on average,
with studies indicating a cost per episode of ∼€10 000 (4). dressings are changed around three times per week, resulting in
Treatment costs increase rapidly when complications such as three home health visits per week (7,9). In a community care
6 © 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd
C. Lindholm & R. Searle Wound management for the 21st century
setting in Denmark, a survey found that at least half of the
patients surveyed were having their wounds dressed three or in municipalities in Denmark was DKK 735 m (18 000
more times per week, with 23% of patients having daily dress- wounds per year requiring over 3 m dressing changes). This
ing changes (7). is predicted to rise by up to 30% between 2010 and 2020
This places a significant, and arguably unsustainable, burden (27). In the UK, the cost of providing services for the treat-
on over-stretched nurse resources in community and home ment of wounds could rise by over £200 million annually
health settings. Acute care facilities are constantly looking for from 2014 to 2019. This would include around an addi-
ways of reducing length of stay; expediting discharge means tional 950 nursing staff and an additional 267 500 hospital
that community health care providers are having to deal with bed-days. The total additional cost to the health system
greater acuity of patients with more complex needs. In addition of providing wound management services over this 5-year
to this, the number of patients requiring wound management is period is estimated to be £600 m (22).
expected to increase with an ageing population and increased
prevalence of multiple underlying conditions (22).
The impact of these factors on nurses is already starting
to manifest itself. A study from Denmark estimates that the
activity of health professionals has increased by 40% since 2001 How can we reconcile increasing patient
(23). Today, 72 nurses are doing what 100 nurses did in 2001, demands with scarce nurse resources?
according to this analysis by the Danish Nurses Organization
The answer to this question is improvements in efficiency. Effi-
(23). In the UK, the number of district nurses decreased by 39%
ciency is an economic term that means increasing the output of a
between 2002 and 2012, partly because of funding constraints
constant resource – put another way, increasing the productiv-
but also as a result of an increase in the number of nurses
ity of nurses. Health economists seek to measure efficiency by
leaving practice (24). This is compounded by increasing rates
contrasting the resources required to deliver health care with the
of retirement and reducing rates of newly qualified nurses (24).
health benefits that they produce. Health care resources might
This trend is clearly unsustainable, and as a result, it is vital that
include:
health care providers seek more efficient ways of managing a
resource-intensive casemix with increasingly complex needs, • the time used by health care professionals such as nurses,
such as patients with a wound. podiatrists, GPs and surgeons
• dressings and other materials and equipment
• hospital beds
• operating theatre time
• resources used in documentation and administration
Demand for wound management services
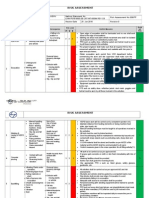
Wound management is estimated to account for over 50% Figure 1 indicates how resources are allocated to the man-
of community nurse time in European studies, with patients agement of wounds (6).
often having three or more home health visits per week When looking for efficiency improvements, health care
(7,9,10,21). providers will often select the easy targets, such as supplies bud-
The demands on nurse time are expected to increase further gets, which are quantifiable and easily manipulated in the short
because of earlier hospital discharge, ageing populations term. However, it is important that they focus their attention on
and increasing rates of morbidities associated with wounds the main cost drivers and also consider the opportunity cost of
(22). resources, which is often less easy to quantify. The opportu-
For example, the International Diabetes Foundation esti- nity cost of a resource refers to the benefits that are foregone
mates that worldwide diabetes prevalence will continue to by allocating a resource to a particular activity. For example, a
increase to 9⋅9% by 2030 (25). nurse making three home visits to a patient with a wound could
Diabetic patients have up to a 25% lifetime risk of devel- have allocated the same time to running a diabetes clinic for 10
oping a foot ulcer (26). patients. In some cases, it is questionable whether resources can
The increasing demands on nurse time will become unsus- be so easily moved between activities – can the same nurse pro-
tainable if the present trend continues, and health sys- viding wound care also provide diabetes management advice?
tems need to identify more efficient ways of managing the However, in many cases, the conscious decision to manage a
increased workload. patient in an inefficient way results in foregone benefits for
other patients.
This is an important consideration for individuals involved
in the management of wounds. The concept of freeing up nurse
resources – for example, through less frequent home visits –
Question: Are there any estimates of how much demand for means that the same nurse resource is now available to treat
wound management services will increase? additional patients. Health care planners and nurses need to
Answer: Yes, in some countries. For example, in 2010, continuously challenge themselves by asking ‘could I be using
it was estimated that the cost of wound management my time more efficiently to provide better quality care or treat
more patients?’
© 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd 7
Wound management for the 21st century C. Lindholm & R. Searle
used, especially in community services. Much of this time is
used to change the patient’s wound dressings, which is why the
frequency of dressing change is a very important driver of cost.
Researchers who have audited wound management have
found that, on average, wound dressings are changed about
three times a week. One study of home care in Denmark found
an average of 3⋅53 changes per week, with 23% of wounds
having dressings changed every day (7).
Dressings need to be changed at a frequency that is appro-
priate for the patient and the wound. However, unnecessary
dressing changes can have an impact on both patient well-being
and resources. Higher dressing change frequency can increase
dressing and nursing costs and may lead to an increased risk
of complications because of the increased frequency of wound
exposure (29). It may also mean that the patient has the inconve-
Figure 1 Resources used in treating wounds. nience of multiple appointments and the physical and emotional
impact of repeated dressing removal and application (29).
Question: Nurses are already there, and paid for, so why
does it matter how often they visit patients? Saving nurse The incidence of complications
time doesn’t save the system any money – surely, it is Wounds do not always follow the expected healing trajectory,
better to save money on dressings? particularly because many patients with wounds have comor-
Answer: We need to think about the opportunity cost. What bidities and underlying long-term conditions. Complications
have we given up in order for the nurse to undertake the occur along the way, and these can have a profound effect, not
treatment? We have given up the opportunity to treat some- only for the patient but also for the health system. Complica-
one else or undertake some other valuable activity. This tions are the third of the three drivers of cost we are consider-
time has a monetary cost that we can calculate if we know ing here.
the cost per hour of nursing time. Releasing nurse time As an example, let us consider SSIs. SSIs can lead to pro-
is about freeing up time to increase efficiency – the key longed hospital stay, readmission, additional surgical proce-
to solving the problem of increasing demand for services. dures and use of antibiotics. Several years ago, a study in the
Releasing nurse visits may also reduce the number of dress- UK estimated that SSIs add, on average, 11 days per episode to
ings required. This has the potential to provide procurement the patient’s stay in hospital (4).
savings (28). Other wound types can also become infected. It has been
noted that heavy bioburden/infection of chronic wounds is a
major cause of non-healing and a significant contributor to the
How can we deliver improved efficiency increasing cost of health care (30,31). A UK survey across
in wound management? hospitals and community providers found that 13⋅3% of leg/foot
The first step in identifying how to improve efficiency is to ulcers and 10⋅4% of pressure ulcers were infected (Figure 3) (9).
consider the inputs and outputs of wound care. Inputs might be Wound infections, whether they are at surgical sites or
considered to be the nurse time, hospitalisations and dressings in other wound types, can lead to further consequences. A
consumed, whilst the outputs are the health benefits to patients. Swedish study reported that for non-healing chronic wounds,
Figure 2 indicates the main inputs that make up the cost of 26⋅6% were receiving systemic antibiotics, and over 60% had
treating wounds. received at least one antibiotic treatment over a 6-month period
(32). Wound infection is commonly associated with heavy exu-
dation of the wound, which has recently been reported to have
The time it takes to heal a wound
an influence on costs for wound management if inappropriate
As described earlier, surveys would suggest that in a region dressings are selected (33).
of one million people, there are approximately 3500 people In some cases, further complications such as osteomyelitis
living with a wound, of which, around 525 people will have may occur, resulting in further resource use. For example, the
had a wound for 1 year or more. For Europe, with a population additional cost of treating osteomyelitis in Category III and
of approximately 500 million people, there would be about IV pressure ulcers is substantial (estimated at over £30 000 in
262 000 people with these long-standing wounds. The total cost the UK) because the daily cost of treatment is increased and
of treating these long-standing wounds in Europe runs into the time to healing is lengthened (34). This includes costs for
millions of Euros. biopsies, MRI, antibiotics, microbiological tests and surgery,
sometimes including major plastic reconstructive surgery.
If any of these three cost drivers can be reduced, with-
The frequency of changing dressings
out a detrimental impact on patient outcomes, then we can
As we have seen, in wound management, the time spent by deliver an improvement in efficiency. Of course, the best result
health care professionals is a large part of the total resources for health service administrators is the delivery of improved
8 © 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd
C. Lindholm & R. Searle Wound management for the 21st century
Figure 2 Drivers of cost in wound manage-
ment (9,29).
outcomes at lower cost. This is a genuine possibility in wound figures are individual stories of how wounds impact patients,
management – earlier intervention to mitigate the risk of infec- carers and health care professionals. Here are two examples.
tion can result in improved patient outcomes (through the avoid-
ance of complications) and lower treatment costs. There are
fewer and fewer examples of true efficiency gains in health care Case study 1: reducing the frequency of nurse visits
that can deliver both better outcomes and lower costs; improv- for a complex patient
ing the efficiency of wound care should be seen as an opportu- This example was reported as part of an evaluation of com-
nity rather than a challenge. munity health care provision for patients with a wound in a
So, to reduce the economic cost of wounds, the best place to provider in the UK (28). The study results indicate that the
start is by looking at the three drivers. introduction of a novel dressing allowed nurses to reduce the
frequency of their nurse visits by almost two visits per patient
Question: Surely, presenting three factors responsible for per week and that procurement costs were also reduced through
driving cost is an over-simplified picture. Isn’t it a lot more less frequent dressing changes. The implications of this at a
complicated than this? patient level can be illustrated through a case study of one
Answer: In reality, the picture is of course more complex. patient that had a wet leaking leg that was being re-dressed
However, by identifying three major drivers of cost, we twice daily, resulting in 14 nurse visits and dressing changes per
are able to think about how we might use these to release week (28). The cost of these visits and dressing changes was
resources and therefore make services more efficient. We substantial. After switching to an advanced wound dressing,
will look at some ways of doing that in the next section. the nursing team were able to reduce the frequency of dress-
ing change to four changes per week. The number of dressings
used at each change was also reduced, resulting in fewer dress-
ings per week, reduced cost of dressings per change and per
Putting it in practice – delivering improved efficiency week and a dramatic reduction in the overall cost of treatment.
in wound management for individual patients
In fact, the patient’s weekly wound management treatment costs
As we have seen above, wounds have a substantial impact on were reduced by 81⋅6%, with 5 hours of community nurse time
the health system. However, underneath all the statistics and freed up per week (Table 1).
© 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd 9
Wound management for the 21st century C. Lindholm & R. Searle
Case study 2: reducing the duration of wound healing
This example was reported in a case series undertaken in
Denmark in 2014 (35). This case series is also referred to in
the final section. A 56-year-old female had a pressure ulcer on
the hip for more than 2 months, covering an area of 48 cm2 .
This ulcer was being dressed daily, and the area was reducing
at approximately 7% per week, on average, with conventional
treatment. The wound-healing trajectory was tracked at each
dressing change using digital planimetry and tracking software.
Using this software, it was estimated that the ulcer would heal
in October using this treatment regime. Single-use negative
pressure therapy (NPWT) was initiated and used for 14 days,
during which time the average area reduction per week was
31% (Figure 4). After discontinuation of the NPWT, the ulcer
continued to heal until fully healing in May, when the weekly
reduction in area was 28%.
This case illustrates the benefits of bringing forward the point
of healing through effective intervention. Using single-use
NPWT, a shorter care package was required, freeing up health
care professionals’ time and enabling them to treat further
patients. In addition to this release of time, fewer nurse con-
tacts per week and shorter visiting times were required. When
interventions such as this are adopted in routine practice, they
have the potential to make a substantial impact on resources.
The next section gives examples of changes that can be made
to do ‘more with less’.
Making the best use of resources – doing more
with less
Figure 3 MRSA at 31 300× magnification. As we have demonstrated above, the gap between available
services and demand for services will continue to widen, and as
a result, it is necessary to find ways of increasing productivity
by making wound management more efficient.
Table 1 Summary of costs for Case study 1 (28) It may be tempting for decision makers in these circum-
stances to look for ways to reduce resources by targeting easily
Wound management
manageable supplies budgets. However, as illustrated above,
cost after introducing
the advanced
this would fail to address the main cost drivers in wound man-
Wound management wound management agement and may even be perverse if it results in the adoption
cost at baseline product of dressings that may increase nurse visit frequency or result in
decrements to health outcomes.
Cost of materials per £29⋅08 £5⋅95
So what can be done to make the most efficient use of
dressing change
the available resources? In other words, how can resources be
Total cost per dressing £65⋅25 £42⋅12
change
RELEASED or freed up so that they can be better used for other,
Total cost per week £913⋅50 £168⋅48 more productive activities? As a way forward, we can take a
look at the three drivers of cost (previous section) and then see
some examples of how these have been used to free up resources
(Figure 5).
Patients that require high levels of resource, as illustrated Reducing healing time
in this example, form part of the caseload of most commu-
nity providers, and clinical staff with experience of managing Case study 1: early intervention to reduce long-duration
wounds will recognise cases such as this. Patients receiving wounds
dressing changes daily or more frequently represent a signif- One way to release resources is to concentrate on wounds
icant proportion of all wound patients; a Danish community that are not currently healing. These static non-healing or
audit found that 23% of patients fell into this category (7). Later, recalcitrant slow-healing wounds can account for a significant
we look more closely at frequency of dressing change and the proportion of health system resources (2). By intervening to
opportunities that may exist for enhancing efficiency. ‘kick-start’ the healing process, they can be brought back to
10 © 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd
C. Lindholm & R. Searle Wound management for the 21st century
PICO start: After 14 days: 4 weeks post-PICO:
37.5 cm2 20.5 cm2 10.1 cm2
Figure 4 Reduction in ulcer area after
single-use negative pressure therapy
(PICO† ; † Trademark of Smith & Nephew)
initiation (35).
Figure 5 Some ways of releasing resources.
a healing trajectory, with the potential to release substantial to optimise treatment by following each ulcer patient right
resources over a long period. through to the healing endpoint. Data from 1073 patients
A recent study showed that application of single-use NWPT with hard-to-heal ulcers, treated between 2009 and 2012, were
was able to accelerate the healing process of slow-healing reported. Wound types were predominantly leg ulcers but also
chronic wounds (35,36). One case from this study was included other wound types.
described in the previous section. By using healing trajectories The mean healing time was reduced from 269 days in 2009
to compare the rates before and after treatment, the study to 139 days in 2012, whilst the mean total cost of treatment per
showed substantial cost saving as a consequence of healing patient decreased from SEK 38 000 in 2009 to SEK 20 500 in
these wounds earlier (Figure 6). This is an excellent example 2012. Most of the cost of treatment (approximately 87%) rep-
in two ways: resented staff costs. This study shows that the use of systematic
treatment strategies to reduce healing times can have a dramatic
• Firstly, it shows how intervention that appears to be of
impact on the use of resources.
greater cost in the short term can, in fact, save resources
overall.
• Secondly, it illustrates the value of tracking and monitor- Optimising dressing change frequency
ing wound progress. This can be performed very simply,
and can provide a wealth of useful data that can be used Case study 3: evaluations in the UK
to demonstrate resource savings. The second driver of cost that was highlighted above was
the frequency with which dressings are changed. The optimal
frequency will depend on a number of factors relating to the:
Case study 2: report from the Swedish Registry of Ulcer
• wound: infection, exudate level, etc.
Treatment (RUT)
• patient and their circumstances: e.g. comorbidities and
A recently published paper described the use of a registry underlying conditions
to shorten ulcer healing time and thereby reduce the use of • clinician: e.g. their workload and schedule
resources (37). The use of the registry promoted structured • system: e.g. the logistics of when visits can be under-
wound management using a team approach, with documen- taken
tation of diagnosis and wound progress. This system helped • products used: e.g. their ability to manage exudate
© 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd 11
Wound management for the 21st century C. Lindholm & R. Searle
Figure 6 Early intervention to reduce long-duration wounds (35).
Innovative practice and well-designed effective products
together play a major role in this (29), and products designed to conducted in the UK found that 79% of wounds were
help to manage resources as well as to meet the need of patients treated in community health care (home health care,
are inherently valuable. wound clinics, nursing homes, etc.) (6). If we apply these
For example, three recent evaluations have shown that it is figures to a population of one million people, this means
possible to release resources by changes in practice combined that at the time of writing, there are likely to be 2765 people
with the use of appropriate dressings (28,38,39). These studies with a wound being treated in the community.* Jørgensen
described the introduction of a foam dressing into clinical et al. (2013) (7) reported that the average frequency of
practice in three community health care providers in the UK. dressing change in community health care was 3⋅53 times
They reported wound characteristics and details of clinical per week, suggesting that there are approximately 9760
practice, such as frequency of dressing change before and patient contacts for dressing change per week, or around
after the implementation of the dressing, and showed a marked 507 500 per year. If this could be reduced by one visit per
reduction in dressing change frequency (Table 2). From this week per patient, this could potentially release 143 800
information, estimates of the potential to release nurse hours visits or around 74 300 hours of clinician time per year.†
were made. Even reducing visits for a smaller subset of the patient
One of the evaluations also estimated the cost of dressings population would free up a substantial quantity of time.
per dressing change and per wound. On average, the number of For example, reducing frequency by one visit per week
dressings per week on each wound was reduced by 79⋅6%, and for 30% of patients could release almost 22 300 hours of
the mean cost of dressings per patient per week was reduced by nursing time per year. Furthermore, reducing dressing
64⋅0% (28). change frequency in conjunction with a reduction in the
It would be interesting to estimate the potential for releas- number of dressings used per visit could lead to a reduction
ing resources more generally if results such as this were repro- in dressing expenditure. This capacity for reduction in this
duced. Such estimates can be made if we use published wound expenditure will depend on the pattern of dressing usage
prevalence figures (see box below). by a care provider, the mix of products that are used and
the frequency with which they are changed. Nevertheless,
even if only one quarter of the potential reduction reported
by Joy et al. (28) were to be realised, this could indicate a
Potential for resource release through 15–20% saving in dressing costs.
dressing change practice
As discussed earlier, we assume that there are 3⋅5 people * 3⋅5/1000 × 0⋅79 × 1 000 000 = 2765.
with a wound per 1000 population (6–9). A survey †
Assuming 31 minutes per visit (21).
12 © 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd
C. Lindholm & R. Searle Wound management for the 21st century
Table 2 Optimising dressing change frequency (28,38,39)
Frequency of dressing change (per week)
Evaluation Before introduction After introduction Difference Number of wounds
Stephen-Haynes et al. 2013 4⋅52 2⋅88 1⋅64 28
Simon et al. 2014 2 1⋅35 0⋅65 97
Joy et al. 2014 3⋅6 1⋅8 1⋅8 37
Combined* 2⋅80 1⋅71 1⋅09 162
*Mean weighted by the number of wounds in each evaluation.
Preventing complications such as wound infection
implemented changes to the wound management products
Complications such as infection have the potential to delay alongside education for staff and patients. Part of this new
healing, adversely affect the patient’s quality of life and even approach was the targeted use of single-use NWPT based
increase the risk of mortality as a result of sepsis. For surgi- on risk stratification. Obesity is an important risk factor
cal sites, infection may have a dramatic effect on quality of as it has a strong association with the incidence of SSI.
life and a substantial impact on resources as there may be a Therefore, NPWT was used for women with a BMI of 35
variety of additional procedures, drugs and materials and staff and above, whereas a film and pad dressing was used for
time needed to deal with wound complications and their conse- women with a BMI less than 35.
quences. Leaper et al. (2010) (40) cite several examples: The team employed this strategy for a total of 660 women
• peripheral vascular surgery, where catastrophic haemor- who had C-sections between February and November
rhage may follow vascular graft infection 2012. They reported a 50% drop in the incidence of SSIs
• infection of a hip prosthesis, where revision surgery may across the whole patient group. In the high-risk group, there
be necessary were no infections, and the number of readmissions fell
• infection following hysterectomy or intestinal surgery, from three per month to zero. It was estimated that the use
which can result in extensive use of resources and of the new protocol would result in a cost saving of £29 449
repeated antibiotic treatment per year.
• infection following cardiac surgery, where sternal dehis- This study shows the value of targeting high-risk groups
cence may involve extensive multidisciplinary care and demonstrates that using negative pressure on closed
• infection following breast cancer surgery, where an incisions in high-risk patients can potentially reduce wound
SSI may extend the waiting time between surgery and complications and readmission rates.
chemotherapy or radiotherapy
At least 5% of patients develop a post-surgical wound infec-
tion, and it has been pointed out that although SSIs have not Question: There are several examples of releasing
generally received a lot of attention, they may be the type of resources by changing practice. How does an organisation
infection that is the most preventable (41). know which approach to take?
Preventing SSIs therefore may have a significant impact on Answer: This will depend on the priorities for the organi-
resource use. An example of this was published in 2014, where sation and the opportunities for practice change. It is often
a hospital provider in the UK addressed the problem of SSIs useful to conduct a practice audit to ascertain which are
by making systematic changes to their post-surgical C-section the best opportunities for change, and several examples
practice (42). Following the introduction of these measures, of surveys and audits can be found in published literature
the infection rate dropped from 12% to 6%; in the highest-risk (6–9,43). These can be relatively simple, using a question-
group, there were no infections or readmissions. The box below naire format, and are often done over a short, fixed period
shows some further details. of time to give a ‘snapshot’ of wounds and practice. For
example, a community provider might survey each wound
treated over a given week to ascertain characteristics of the
Case study 4: addressing the problem of SSI (43) wounds, which products were used, how often dressings
were changed etc. These surveys give a wealth of informa-
tion, which can be used to inform practice change, with a
A hospital trust in the UK found that about 12% of view to improving efficiency and quality of care.
women experienced a surgical site infection following a
caesarean section. Readmission to hospital was a particu-
lar problem, with women with high body mass index (BMI) Is prevention cheaper than cure?
(≥35 kg/m2 ) being the most likely to have a readmission.
The provider put together a multidisciplinary team includ- One important way to reduce the cost of wound management in
ing a tissue viability nurse and infection control nurse, the future is to make an impact on the number of wounds that
together with the obstetricians and midwives. This team need to be treated. This means that wound prevention has an
important role to play in counteracting the demographic trends
© 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd 13
Wound management for the 21st century C. Lindholm & R. Searle
affecting wound prevalence. For example, below-knee gradu- increased incidence have been introduced in some countries.
ated compression hosiery is recommended to prevent recur- Awareness has increased, and practice has improved, although
rence of VLUs in patients with healed ulcers (44), and regular there is continued debate about the proportion of pressure ulcers
foot assessments are effective to prevent DFUs alongside other that are avoidable (50). However, there is more that can be
interventions such as optimising glycaemic control and smok- carried out to adopt strategic approaches to prevention and to
ing cessation (45). use effective risk-assessment methods (51).
Often, when we think of wound prevention, it is the preven-
tion of pressure ulcers in acute care that comes to mind, and
indeed this is probably the most widely studied area and has Conclusions
received the most attention. Having a pressure ulcer has a pro- Wounds have a significant impact both on the quality of life of
found adverse effect on many aspects of a person’s quality of those who have them and on the world’s health systems. The
life, and although pressure ulcers are not a new phenomenon, number of people with wounds is growing, and this is likely
they continue to be a significant health problem as a result of an to continue into the future as a result of demographic trends.
ageing population (46). They also represent a significant burden Preventing wounds from occurring has an important role to play
to health systems, with one report estimating that treatment of in mitigating the effects of demographic changes that affect
pressure ulceration costs the US $11 billion annually (47). wound prevalence.
Recently published international guidelines for the preven- We can think systematically about the cost of caring for
tion and treatment of pressure ulcers have demonstrated that people with wounds by considering the resources used. Human
there a number of important considerations for prevention to be resource is the most valuable asset that the health system has,
effective (48): and most of the resource used in wound management is as a
• risk assessment result of hospital treatment or nursing visits. Materials such
• skin and tissue assessment as dressings account for a relatively small amount of the cost;
• preventive skin care however, the choice of materials and dressings used is very
• the use of emerging therapies such as microclimate con- important.
trol, prophylactic dressings, fabrics and textiles and elec- There are three significant drivers of cost: the time it takes
trical muscle stimulation a wound to heal, the frequency of visits by health care profes-
• good nutrition sionals and the incidence of complications.
• repositioning and early mobilisation These three drivers help us to think about how we can make
• the appropriate use of support surfaces wound management more efficient by:
Thorough and comprehensive risk assessment is a vital part • reducing healing time
of prevention, and several assessment tools have been devel- • optimising dressing change frequency
oped that, when used in conjunction with clinical judgement • preventing complications such as wound infection.
and experience, can help to identify the risk level for individual
patients (49). As there are several potential risk factors for
Acknowledgements
pressure damage, there are a number of different prevention
approaches that can be used in a prevention protocol. For With thanks to John Posnett, Paul Trueman, Carina Ekbladh,
a given patient, the mix of these different components will Trine Gram and Jane Hampton for valuable contributions to
vary (49). the content presented here. Christina Lindholm is an indepen-
Suitable support surfaces should be used, and the patient’s dent researcher at Sophiahemmet University, Sweden. Richard
skin should be inspected regularly along with a tailored reposi- Searle is an employee of Smith & Nephew. This work was
tioning programme (49). Incontinence, skin moisture, nutrition funded by Smith & Nephew.
and hydration must all be managed in collaboration with the
appropriate health care professionals (49). The use of multilayer
foam dressings has also, in recent years, become a valuable References
addition to the tools available for pressure ulcer prevention, par- 1. Harding K. Understanding healing after skin breakdown. In: Skin
ticularly for high-risk patients such as those in high-dependency breakdown – the silent epidemic. Hull: Smith & Nephew Foundation,
or intensive care units (49). Such dressings have been shown to 2007:13–16.
2. Smith & Nephew Foundation (2007). Skin breakdown – the silent
reduce the incidence of PU in these patient groups, and some epidemic. Smith & Nephew Foundation, Hull.
hospitals have the use of these dressings as part of their PU 3. Wounds International (2012). International consensus. Optimising
prevention protocol. The choice of dressings is important: they wellbeing in people living with a wound. Wounds International,
must have the ability to redistribute pressure, reduce shear and London.
friction and effectively manage temperature and moisture at the 4. Posnett J, Gottrup F, Lundgren H, Saal G. The resource impact of
skin surface. Where surrounding skin is fragile, as is often the wounds on health-care providers in Europe. J Wound Care 2009;18:
154–61.
case with patients at risk of PU, dressings with a soft silicone
5. Troxler M, Vowden K, Vowden P. Integrating adjunctive therapy
border may be appropriate (49). into practice: the importance of recognising ‘hard-to-heal’ wounds.
Much has been done to improve and implement pressure World Wide Wounds 2006. URL http://www.worldwidewounds.com/
ulcer prevention measures across Europe. Economic incentives 2006/december/Troxler/Integrating-Adjunctive-Therapy-Into-Practice.
for the reduction of PU incidence and financial penalties for html [accessed on November 2015].
14 © 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd
C. Lindholm & R. Searle Wound management for the 21st century
6. Vowden K, Vowden P, Posnett J. The resource costs of wound care 27. Hjort A, Gottrup F. Cost of wound treatment to increase significantly
in Bradford and Airedale primary care trust in the UK. J Wound Care in Denmark over the next decade. J Wound Care 2010;19:173–4, 176,
2009;18:93–102. 178, 180, 182, 184.
7. Jørgensen SF, Nygaard R, Posnett J. Meeting the challenges of wound 28. Joy H, Bielby A, Searle R. A collaborative project to enhance effi-
care in Danish home care. J Wound Care 2013;22:540–2, 544–5. ciency through dressing change practice. J Wound Care 2015;24:312,
8. Gottrup F, Henneberg E, Trangbæk R, Bækmark N, Zøllner K, 314–7.
Sørensen J. Point prevalence of wounds and cost impact in the acute 29. Stephen-Haynes J, Bielby A, Searle R. Putting patients first: reducing
and community setting in Denmark. J Wound Care 2013;22:413–4, the human and economic costs of wounds. Wounds UK 2011;7:47–55.
416, 418–22. 30. Siddiqui AR, Bernstein JM. Chronic wound infection: facts and con-
9. Drew P, Posnett J, Rusling L. The cost of wound care for a local troversies. Clin Dermatol 2010;28:519–26.
population in England. Int Wound J 2007;4:149–55. 31. Vowden P. Hard-to-heal wounds made easy. Wounds International,
10. Srinivasaiah N, Dugdall H, Barrett S, Drew PJ. A point prevalence sur- Schofield Healthcare Media Ltd: Norwich, UK, 2011;2. URL
vey of wounds in north-east England. J Wound Care 2007;16:413–6, http://www.woundsinternational.com.
418–9. 32. Tammelin A, Lindholm C, Hambraeus A. Chronic ulcers and antibiotic
11. Lindholm C, Andersson H, Fossum B, Jörbeck H. Wounds scrutiny in a treatment. J Wound Care 1998;7:435–7.
Swedish hospital: prevalence, nursing care and bacteriology, including 33. Benbow M. The expense of exudate management. Br J Nurs
MRSA. J Wound Care 2005;14:313–9. 2015;24(15 Suppl):S8.
12. Eucomed Wound Care Policy Paper. URL http://ewma.org/fileadmin/ 34. Dealey C, Posnett J, Walker A. The cost of pressure ulcers in the United
user_upload/EWMA/pdf/EWMA_Projects/090923__Wound_Care_ Kingdom. J Wound Care 2012;21:261–266.
Brochure_final.pdf [accessed on June 2015]. 35. Hampton J. Accelerated wound healing in a community setting, 2014.
13. Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, Gottrup URL http://www.smith-nephew.com/documents/nordics/dk/nordic%
F, Gurtner GC, Longaker MT. Human skin wounds: a major and 20network%20meeting/accelerated%20wound%20healing%20in%20a
snowballing threat to public health and the economy. Wound Repair %20community%20setting_jane%20hampton.pdf
Regen 2009;17:763–771. 36. Hampton J. Providing cost-effective treatment of hard-to-heal wounds
14. Santamaria N. Woundswest: identifying the prevalence of wounds in the community through use of NPWT. Br J Community Nurs
within western Australia’s public health system. EWMA Journal 2015;S14:S16–20.
2009;9:13–8. 37. Öien RF, Forssell H, Ragnarson Tennvall G. Cost consequences due to
15. Bermark S, Zimmerdahl V, Muller K. Prevalence investigation of reduced ulcer healing times – analyses based on the Swedish Registry
pressure ulcers. EWMA J 2004;4:1, 7–11. of Ulcer Treatment. Int Wound J 2015. doi: 10.111/iwj.12465.
16. Guest JF, Ayoub N, McIlwraith T, Uchegbu I, Gerrish A, Weidlich D, 38. Stephen-Haynes J, Bielby A, Searle R. The clinical performance of
Vowden K, Vowden P. Health economic burden that wounds impose a silicone foam in an NHS community trust. J Community Nurs
on the National Health Service in the UK. BMJ Open 2015;5:e009283. 2013;27:50–9.
doi: 10.1136/bmjopen-2015-009283. 39. Simon D, Bielby A. A structured collaborative approach to appraise the
17. Phillips CJ, Humphreys I, Fletcher J, Harding K, Chamberlain G, clinical performance of a new product. Wounds UK 2014;10:80–7.
Macey S. Estimating the costs associated with the management of 40. Leaper NJ, Roberts C, Searle R. Economic and clinical contributions
patients with chronic wounds using linked routine data. Int Wound J of an antimicrobial barrier dressing: a strategy for the reduction of
2015. doi: 10.1111/iwj.12443. surgical site infections. J Med Econ 2010;13:447–52.
18. Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin 41. Leaper DJ. Surgical site infection. Br J Surg 2010;97:1601–2.
CK, Keohane C, Denham CR, Bates DW. Health care-associated 42. Bullough L, Wilkinson D, Burns S, Wan L. Changing wound care
infections – a meta-analysis of costs and financial impact on the US protocols to reduce postoperative caesarean section infection and
health care system. JAMA Intern Med 2013;173:2039–46. readmission. Wounds UK 2014;10:72–6.
19. Defez C, Fabbro-Peray P, Cazaban M, Boudemaghe T, Sotto A, 43. Ousey K, Stephenson J, Barrett S, King B, Morton N, Fenwick K, Carr
Daurès JP. Additional direct medical costs of nosocomial infections: C. Wound care in five English NHS trusts: results of a survey. Wounds
an estimation from a cohort of patients in a French university hospital. UK 2013;9:20–8.
J Hosp Infect 2008;68:130–6. 44. Scottish Intercollegiate Guidelines Network. Management of chronic
20. Smith & Nephew. The true cost of wounds and how to reduce it. URL venous leg ulcers – a national clinical guideline. Edinburgh: Health-
http://www.smith-nephew.com/documents/uk/the-true-cost-of-wound- care Improvement Scotland, 2010.
booklet.pdf [accessed on April 2016]. 45. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients
21. O’Keeffe M. Evaluation of a community-based wound care pro- with diabetes. JAMA 2005;293:217–28.
gramme in an urban area. Poster presented at EWMA Conference; 46. Moore Z, Cowman S. Quality of life and pressure ulcers: a literature
Prague: Czech Republic, 2006. review. Wounds UK 2009;5:58–65.
22. Dowsett C, Bielby A, Searle R. Reconciling increasing wound care 47. U.S. Department of Health and Human Services. AHRQ Research
demands with available resources. J Wound Care 2014;23:552–62. Activities Issue, 2011; 371: 31.
doi: 10.12968/jowc.2014.23.11.552. 48. National Pressure Ulcer Advisory Panel. European Pressure Ulcer
23. Kjeldsen SB. Tidspres er en trussel mod patientsikkerheden. Sygeple- Advisory Panel and Pan Pacific Pressure Injury Alliance, 2014. Clini-
jersken 2015;2015:24–7. cal practice guideline: prevention and treatment of pressure ulcers.
24. The Royal College of Nursing. Frontline First: Nursing on Red 49. Sammon M, Dunk AM, Verdú J. Advances in pressure ulcer prevention
Alert April 2013. London: The Royal College of Nursing. URL and treatment. Wounds International, Schofield Healthcare Media Ltd:
http://wwwrcnorguk/__data/assets/pdf_file/0003/518376/004446pdf Norwich, UK, 2015.
[accessed on July 2014]. 50. Downie F, Guy H, Gilroy P, Royall D, Davies S. Are 95% of hospital-
25. International Diabetes Federation. Diabetes Atlas 5th Edition, 2015. acquired pressure ulcers avoidable? Wounds UK 2013;9:16–22.
URL www.idf.org [accessed on November 2015]. 51. Källman U, Suserud B. Knowledge, attitudes and practice among
26. Clayton W, Elasy TA. A review of the pathophysiology, classifica- nursing staff concerning pressure ulcer prevention and treat-
tion, and treatment of foot ulcers in diabetic patients. Clin Diabetes ment – a survey in a Swedish healthcare setting. Scand J Caring
2009;27:52–8. Sci 2009;23:334–41.
© 2016 Medicalhelplines.com Inc and John Wiley & Sons Ltd 15
You might also like
- 9 Types of Female Orgasms ExplainedDocument4 pages9 Types of Female Orgasms ExplainedAbdul SyukurNo ratings yet
- Care of Patient With Respiratory DisordersDocument35 pagesCare of Patient With Respiratory Disorderskriiteeabns100% (1)
- Surgical Site InfectionDocument8 pagesSurgical Site Infection1234chocoNo ratings yet
- Fat-Burning FoodsDocument11 pagesFat-Burning FoodsRamzi FaddoulNo ratings yet
- Brief History of Patient Safety Culture and ScienceDocument4 pagesBrief History of Patient Safety Culture and ScienceHoli100% (1)
- Hse Risk Assessment - 006 Ra - Hdpe Duct LayingDocument7 pagesHse Risk Assessment - 006 Ra - Hdpe Duct Layingbinunalukandam83% (12)
- World Patient Safety DayDocument17 pagesWorld Patient Safety DayNam PHẠM THÀNHNo ratings yet
- Food Safety Plan For CateringDocument80 pagesFood Safety Plan For CateringNghia Khang100% (1)
- Prevention of Surgical Site InfectionDocument10 pagesPrevention of Surgical Site InfectionValiant Baybay100% (1)
- Solution Focused TherapyDocument8 pagesSolution Focused Therapyrimpa29No ratings yet
- Scalpel Safety Sinnott2010Document9 pagesScalpel Safety Sinnott2010Guille Puertas100% (1)
- Babu Jagjivan RamDocument24 pagesBabu Jagjivan RamAnonymous qFWInco8cNo ratings yet
- SpitzDocument30 pagesSpitzprabhatNo ratings yet
- Human Skin Wounds: A Growing Threat to Public Health and the EconomyDocument14 pagesHuman Skin Wounds: A Growing Threat to Public Health and the EconomyNurul Mahyani DaudNo ratings yet
- Chandan K. Sen, PHD PDFDocument14 pagesChandan K. Sen, PHD PDFNurul Mahyani DaudNo ratings yet
- Elderly Hip Fracture PatientsDocument7 pagesElderly Hip Fracture PatientspamancastroNo ratings yet
- WHO HIS SDS 2017.11 Eng PDFDocument20 pagesWHO HIS SDS 2017.11 Eng PDFJayalakshmi JayarajanNo ratings yet
- Articulo 2Document9 pagesArticulo 2Gustavo Gonzales ChavezNo ratings yet
- Falls Prevention in Hospitals-The Need For A New Approach An Integrative ArticleDocument4 pagesFalls Prevention in Hospitals-The Need For A New Approach An Integrative ArticleDwi NopriyantoNo ratings yet
- 4839701Document12 pages4839701mkoffietranhanssaviolaNo ratings yet
- Evidence-Based Medicine: The Evaluation and Treatment of Pressure InjuriesDocument12 pagesEvidence-Based Medicine: The Evaluation and Treatment of Pressure InjuriesIndahEkaPutriNo ratings yet
- Pressure Ulcer Assessment and Treatment (PDFDrive)Document88 pagesPressure Ulcer Assessment and Treatment (PDFDrive)Amna AliNo ratings yet
- Late Immune Consequences of Combat Trauma: A Review of Trauma-Related Immune Dysfunction and Potential TherapiesDocument13 pagesLate Immune Consequences of Combat Trauma: A Review of Trauma-Related Immune Dysfunction and Potential TherapiesQariahMaulidiahAminNo ratings yet
- Acute Management of Open Fractures An Evidence Based Review PDFDocument9 pagesAcute Management of Open Fractures An Evidence Based Review PDFSusPa Naraha100% (1)
- MSC Proposal - Quantitative - 2019Document32 pagesMSC Proposal - Quantitative - 2019Lihle Mirriam MdlaloseNo ratings yet
- 2018 Seasonal InfluenzaDocument47 pages2018 Seasonal InfluenzaMariaNo ratings yet
- The Most Effective Fall Prevention Program For Patients Over 65 Years - An Integrated Literature ReviewDocument26 pagesThe Most Effective Fall Prevention Program For Patients Over 65 Years - An Integrated Literature Reviewhal kadduNo ratings yet
- Hard-To-Heal Wounds, Biofilm and Wound Healing: An Intricate InterrelationshipDocument6 pagesHard-To-Heal Wounds, Biofilm and Wound Healing: An Intricate InterrelationshipHan's OfficialNo ratings yet
- Jurnal LainDocument22 pagesJurnal LainBudi ArsanaNo ratings yet
- Atls MedscapeDocument5 pagesAtls MedscapeCastay GuerraNo ratings yet
- Surgical Site InfectionsDocument29 pagesSurgical Site Infectionsalfredochelo1921No ratings yet
- Burden of Surgical Site Infections in The NetherlandsDocument10 pagesBurden of Surgical Site Infections in The NetherlandsKanokwan BorwornphiphattanachaiNo ratings yet
- 2016 Article 329Document6 pages2016 Article 329anon_242145531No ratings yet
- Dr. Santi Rahayu Dewayanti, MM, Sp. P, FCCP, FISR - RevDocument31 pagesDr. Santi Rahayu Dewayanti, MM, Sp. P, FCCP, FISR - RevRensa KaruniaNo ratings yet
- Influenza GuidelinesDocument47 pagesInfluenza GuidelinesKok Hui DiongNo ratings yet
- Improving global patient safety through coordinated actionDocument8 pagesImproving global patient safety through coordinated actioncynthiaNo ratings yet
- Updated IDSA GuidelinesDocument47 pagesUpdated IDSA GuidelinesAhmed EzzatNo ratings yet
- Global Patient Safety Challenge - WHODocument35 pagesGlobal Patient Safety Challenge - WHOjoaopinheiro88No ratings yet
- HHS Public Access: Chest Trauma Outcomes: Public Versus Private Level I Trauma CentersDocument19 pagesHHS Public Access: Chest Trauma Outcomes: Public Versus Private Level I Trauma CentersIthaNo ratings yet
- Healthcare Costs of Injuries in the PhilippinesDocument6 pagesHealthcare Costs of Injuries in the Philippineshaechan's fluffy bucket hatNo ratings yet
- Clinical Errors and Medical Negligence: ReviewDocument11 pagesClinical Errors and Medical Negligence: ReviewAnggreanyAshariNo ratings yet
- Pathophysiology in Patients With PolytraumaDocument13 pagesPathophysiology in Patients With PolytraumaRodolfo M. N.B.No ratings yet
- Avoidable Surgical Disasters: Errors or Preventable OutcomesDocument7 pagesAvoidable Surgical Disasters: Errors or Preventable OutcomesGopi JaladiNo ratings yet
- Pre Hos TraumaDocument11 pagesPre Hos TraumaGel OmugtongNo ratings yet
- Antimicrobials and Non-Healing WoundsDocument92 pagesAntimicrobials and Non-Healing WoundsNelu CastravetNo ratings yet
- Duodeno-Pancreatic and Extrahepatic Biliary Tree Trauma - WSES-AAST Guidelines Open AccessDocument23 pagesDuodeno-Pancreatic and Extrahepatic Biliary Tree Trauma - WSES-AAST Guidelines Open AccessDiego Andres VasquezNo ratings yet
- Management of Burns Patient Before Arrival at National Orthopedic Hospital EnuguDocument41 pagesManagement of Burns Patient Before Arrival at National Orthopedic Hospital EnuguDONEKE MIRACLENo ratings yet
- Ren 2018Document7 pagesRen 2018atikahanifahNo ratings yet
- Patient Safety Menurut WHODocument9 pagesPatient Safety Menurut WHOAlwan NugrohoNo ratings yet
- 10 Facts On Patient SafetyDocument3 pages10 Facts On Patient SafetySafiqulatif AbdillahNo ratings yet
- Does Pressure Cause Pressure Ulcers? An Inquiry Into The Etiology of Pressure UlcersDocument9 pagesDoes Pressure Cause Pressure Ulcers? An Inquiry Into The Etiology of Pressure Ulcersvaleria molinaNo ratings yet
- 68 2020 Article 1412Document7 pages68 2020 Article 1412Andres De LeonNo ratings yet
- Risk FactorDocument5 pagesRisk FactorBima AryaputraNo ratings yet
- Trauma ThoraxDocument7 pagesTrauma ThoraxLuqmanul Hakim JunaiddenNo ratings yet
- Wound CareDocument42 pagesWound CareNorma Khoirun Nisa100% (1)
- Acute Nursing Care of The Older Adult With Fragility Hip Fracture: An International Perspective (Part 2)Document26 pagesAcute Nursing Care of The Older Adult With Fragility Hip Fracture: An International Perspective (Part 2)spring flowerNo ratings yet
- The Impact of Pressure Ulcers: Bony Sacrum Coccyx Heels Hips Elbows Knees Ankles CraniumDocument48 pagesThe Impact of Pressure Ulcers: Bony Sacrum Coccyx Heels Hips Elbows Knees Ankles CraniumVanessa Camille DomingoNo ratings yet
- Risk Factors For Falls in Hospital In-Patients: A Prospective Nested Case Control StudyDocument7 pagesRisk Factors For Falls in Hospital In-Patients: A Prospective Nested Case Control StudyNurhasanah HaryaniNo ratings yet
- Pitt Et 2008Document8 pagesPitt Et 2008GrevaldoNo ratings yet
- Maxillofacial TraumaDocument15 pagesMaxillofacial TraumadewiswahyuNo ratings yet
- Patient Safety WHODocument8 pagesPatient Safety WHONovitaSariNo ratings yet
- Eichinger2021_Article_ChallengesInThePREHOSPITALEmerDocument12 pagesEichinger2021_Article_ChallengesInThePREHOSPITALEmerBarry TraceyNo ratings yet
- Presus DR HardDocument5 pagesPresus DR HardAhmad MusafiNo ratings yet
- Ronald V. Maier, M.D.: Awards: FundingDocument5 pagesRonald V. Maier, M.D.: Awards: Fundingyanuar andaniNo ratings yet
- Peek Et Al. Rib Fractures Nation-Wide StudyDocument7 pagesPeek Et Al. Rib Fractures Nation-Wide StudyRut Herdianti P. EkasiwiNo ratings yet
- Sciadv Ade7007Document11 pagesSciadv Ade7007Poramate PITAK-ARNNOPNo ratings yet
- Ol 20 1 441 PDFDocument7 pagesOl 20 1 441 PDFeka satyani belinaNo ratings yet
- Pressure Ulcers in the Aging Population: A Guide for CliniciansFrom EverandPressure Ulcers in the Aging Population: A Guide for CliniciansDavid R. Thomas, MDNo ratings yet
- Defect eDocument2 pagesDefect eHeba VerebceanNo ratings yet
- The Use of Chitin and Chitosan in MDocument21 pagesThe Use of Chitin and Chitosan in MHeba VerebceanNo ratings yet
- Gerry Rayman Prashanth Vas Ketan Dhatariya Vicki Driver Agnes Hartemann Magnus Londahl Alberto Piaggesi Jan Apelqvist Chris Attinger Fran GameDocument17 pagesGerry Rayman Prashanth Vas Ketan Dhatariya Vicki Driver Agnes Hartemann Magnus Londahl Alberto Piaggesi Jan Apelqvist Chris Attinger Fran GameHeba VerebceanNo ratings yet
- Structura ProteinelorDocument6 pagesStructura Proteinelorconstiinta47No ratings yet
- Cazuri CliniceDocument32 pagesCazuri CliniceHeba VerebceanNo ratings yet
- Ijerph 19 01338 v2Document25 pagesIjerph 19 01338 v2Heba VerebceanNo ratings yet
- 6 Parenteral Nutrition Online PDF-62175Document42 pages6 Parenteral Nutrition Online PDF-62175Heba VerebceanNo ratings yet
- Health-Related Quality of Life, Self-Esteem, and Functional Status of Patients With Leg UlcersDocument8 pagesHealth-Related Quality of Life, Self-Esteem, and Functional Status of Patients With Leg UlcersHeba VerebceanNo ratings yet
- Mo Loney 2004Document4 pagesMo Loney 2004Heba VerebceanNo ratings yet
- Wound Management For The 21st Century: Combining Effectiveness and EfficiencyDocument11 pagesWound Management For The 21st Century: Combining Effectiveness and EfficiencyHeba VerebceanNo ratings yet
- Hydrocolloid Dressing PDFDocument17 pagesHydrocolloid Dressing PDFeyleenNo ratings yet
- Chronic Cutaneous Ulcers: Etiology and Epidemiology: Taniaj. PhillipsDocument5 pagesChronic Cutaneous Ulcers: Etiology and Epidemiology: Taniaj. PhillipsHeba VerebceanNo ratings yet
- Dr. Amit Gupta Associate Professor Dept of SurgeryDocument43 pagesDr. Amit Gupta Associate Professor Dept of SurgeryHeba VerebceanNo ratings yet
- 37b7c2326a4dcbaa729c0a733d8b8c42Document1 page37b7c2326a4dcbaa729c0a733d8b8c42Heba VerebceanNo ratings yet
- Special Wound Healing Methods Used in Ancient Egypt and The Mythological BackgroundDocument6 pagesSpecial Wound Healing Methods Used in Ancient Egypt and The Mythological BackgroundHeba VerebceanNo ratings yet
- Krull 1985Document8 pagesKrull 1985Heba VerebceanNo ratings yet
- Krull 1985Document8 pagesKrull 1985Heba VerebceanNo ratings yet
- Mo Loney 2004Document4 pagesMo Loney 2004Heba VerebceanNo ratings yet
- 10 3389@fbioe 2020 00182Document17 pages10 3389@fbioe 2020 00182Heba VerebceanNo ratings yet
- Chronic Wound Healing Review: Current Management and TreatmentsDocument12 pagesChronic Wound Healing Review: Current Management and TreatmentsHeba VerebceanNo ratings yet
- Chronic Cutaneous Ulcers: Etiology and Epidemiology: Taniaj. PhillipsDocument5 pagesChronic Cutaneous Ulcers: Etiology and Epidemiology: Taniaj. PhillipsHeba VerebceanNo ratings yet
- Student Letter 2022Document1 pageStudent Letter 2022Heba VerebceanNo ratings yet
- Student Letter 2022Document1 pageStudent Letter 2022Heba VerebceanNo ratings yet
- Study Case Analysis GuidelineDocument1 pageStudy Case Analysis GuidelineHeba VerebceanNo ratings yet
- Study Case Analysis GuidelineDocument1 pageStudy Case Analysis GuidelineHeba VerebceanNo ratings yet
- Alcoholism and mental health conditionsDocument2 pagesAlcoholism and mental health conditionsHeba VerebceanNo ratings yet
- 10 3389@fbioe 2020 00182Document17 pages10 3389@fbioe 2020 00182Heba VerebceanNo ratings yet
- Study Case Analysis GuidelineDocument1 pageStudy Case Analysis GuidelineHeba VerebceanNo ratings yet
- 01 Raspuns La Teste. SensibilitateaDocument1 page01 Raspuns La Teste. SensibilitateaHeba VerebceanNo ratings yet
- Calculator NotesDocument4 pagesCalculator NotessdiamanNo ratings yet
- Young InfantDocument69 pagesYoung InfantAurora Doris BatagaNo ratings yet
- Human Population and EnvironmentDocument4 pagesHuman Population and Environmentmonkeybike88No ratings yet
- A Study On Environmental Impact of Madukkarai Limestone Mine, CoimbatoreDocument11 pagesA Study On Environmental Impact of Madukkarai Limestone Mine, CoimbatoreRamasamyNagarajan100% (1)
- Vacation With Sunny Leone - Without FlightDocument4 pagesVacation With Sunny Leone - Without FlightkalidasdoraemonNo ratings yet
- Republic Act 10932 Anti-Hospital Deposit LawDocument9 pagesRepublic Act 10932 Anti-Hospital Deposit LawVenus PangilinanNo ratings yet
- Central Pain Syndrome - Pathophysiol., Diag., Mgmt. - S. Canavero, Et. Al., (Cambridge, 2006) WW PDFDocument398 pagesCentral Pain Syndrome - Pathophysiol., Diag., Mgmt. - S. Canavero, Et. Al., (Cambridge, 2006) WW PDFRomeo-Remus RaffaiNo ratings yet
- (Bio 024) Lab Activity 12 - BloodDocument9 pages(Bio 024) Lab Activity 12 - Bloodelaq dr100% (1)
- MSDSDocument3 pagesMSDSSiti Nurjanah SeptianiNo ratings yet
- Intrathecal MTX & Cytarabine & Hydrocortisone V4 2.15Document2 pagesIntrathecal MTX & Cytarabine & Hydrocortisone V4 2.15GabrielNo ratings yet
- Pathological Urine ConstituentsDocument22 pagesPathological Urine Constituentsmanni1001100% (3)
- Soal Bahasa Inggris Kelas 5Document8 pagesSoal Bahasa Inggris Kelas 5imam hambaliNo ratings yet
- Nursing Care Plan for Patient SafetyDocument9 pagesNursing Care Plan for Patient SafetyACOB, Jamil C.No ratings yet
- Maynilad Valenzuela Sewerage Project Environmental ReportDocument297 pagesMaynilad Valenzuela Sewerage Project Environmental ReportmarvilouNo ratings yet
- Que No4 & 5-With Clues and Without CluesDocument4 pagesQue No4 & 5-With Clues and Without CluesMir Yamin Uddin ZidanNo ratings yet
- Nursing and Midwifery Board Candidate Handbook RN OSCE ExaminationDocument25 pagesNursing and Midwifery Board Candidate Handbook RN OSCE ExaminationkemalayazNo ratings yet
- Exercises For Task 3 InglesDocument3 pagesExercises For Task 3 InglesNoelia De Los SantosNo ratings yet
- CV 2020Document3 pagesCV 2020api-519861494No ratings yet
- Marihuana EsquizofreniaDocument30 pagesMarihuana EsquizofreniaJ Elver SilvaNo ratings yet
- Connectors 2Document14 pagesConnectors 2Irene SánchezNo ratings yet
- Guide To Patient Support and Regional Cancer ServicesDocument76 pagesGuide To Patient Support and Regional Cancer Servicesgiovanna2004No ratings yet
- Awarness About Breast CancerDocument4 pagesAwarness About Breast CancerliaahlanNo ratings yet