0% found this document useful (0 votes)
145 views21 pagesCSF Laboratory Diagnosis Guide
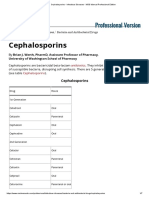
The document discusses the laboratory diagnosis of cerebrospinal fluid (CSF) samples. CSF is collected through lumbar puncture or from ventricular shunt reservoirs to test for meningitis or shunt infections. Samples are tested through Gram stain, culture, and other assays. Positive cultures are identified to the genus and species level to determine pathogenic organisms like Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae that can cause acute meningitis. Fungal pathogens like Cryptococcus are also tested for through culture and antigen assays.
Uploaded by
marc cajucomCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
145 views21 pagesCSF Laboratory Diagnosis Guide
The document discusses the laboratory diagnosis of cerebrospinal fluid (CSF) samples. CSF is collected through lumbar puncture or from ventricular shunt reservoirs to test for meningitis or shunt infections. Samples are tested through Gram stain, culture, and other assays. Positive cultures are identified to the genus and species level to determine pathogenic organisms like Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae that can cause acute meningitis. Fungal pathogens like Cryptococcus are also tested for through culture and antigen assays.
Uploaded by
marc cajucomCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd