Professional Documents
Culture Documents
Net Quiz: Ammatory Pruritic Nodules and Plaques On The Fac in Ammatory Pruritic Nodules and Plaques On The Face
Uploaded by
JohnOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Net Quiz: Ammatory Pruritic Nodules and Plaques On The Fac in Ammatory Pruritic Nodules and Plaques On The Face
Uploaded by
JohnCopyright:
Available Formats
Net Quiz
Inflflammatory pruritic nodules and plaques on the face
In fac
A 31-year-old male schoolteacher presented with mildly Investigations done included skin biopsy for
pruritic erythematous crusted plaques and nodules studded histopathological examination, including special stain
with pustules on chin and left malar region of 20 days duration [Figure 3]. Patch testing including that with plant allergens
[Figures 1-2]. He complained of increased itching and burning gave a negative result. Gram staining of the discharge
ns om
sensation after application of soap, aftershave lotion and from pustules did not reveal any bacteria and swab for
perfume. He was not using any other cosmetic. He had no bacterial culture and sensitivity taken from the pustules
tio fr
previous history of atopy, drug allergy, photosensitivity or did not reveal any growth.
). lica ad
any systemic complaints. He occasionally visited the barber’s
om b lo
shop for shaving his beard. There were no pets at home. WHAT IS YOUR DIAGNOSIS?
DIAGNOSIS
.c Pu wn
ow w do
kn kno ee
ed d fr
m e or
w. M f
w by le
(w ed ilab
st va
ho a
te is
Figure 1: Inflammatory nodules and plaques with superficial Figure 3: Skin biopsy with special staining (x 400)
crusting and oozing on beard region
si F
a PD
is
Th
Figure 2: Erythematous nodules and plaques over left malar
area
How to
to cite this article
article: Rao R, Prabhu S, George M, Shenoi SD. Inflammatory pruritic nodules and plaques on the face. Indian J Dermatol
Venereol Leprol 2007;73:142.
Received: April, 2006. Accepted: November, 2006. Source of Support: Nil. Confl
Conflict of interest: None declared.
Indian J Dermatol Venereol Leprol|March-April 2007|Vol 73|Issue 2 161
Net Quiz
high temperature and humidity. In the past, it was frequently
transmitted by barbers who used unsanitary razors- the
so-called barber’s itch. Causative organisms include both
zoophilic and anthropophilic dermatophytes, which release
several enzymes, including keratinases which help them to
invade the epidermis. In tinea barbae, hair and hair follicles
are invaded by fungi, producing an inflammatory response.
Tinea barbae may present in three forms- inflammatory,
sycosiform or circinate.[1]
Inflammatory tinea barbae is caused primarily by zoophilic
dermatophytes and presents as solitary or multiple
ns om
Figure 4: Fluffy white growth of Trichophyton mentagrophytes in plaques or nodules; localized to the chin, cheeks or neck;
SDA. (Left) Positive urease test (Right)
involvement of the upper lip is rare. The characteristic
tio fr
lesion is an inflammatory reddish nodule with pustules and
). lica ad
draining sinuses on the surface. Hair are loose or broken
om b lo
and depilation is easy and painless. Pus-filled whitish
.c Pu wn
masses involve the hair root and follicle. Over time, the
surface of the indurated nodule is covered by exudate and
ow w do crust. Noninflammatory superficial tinea barbae is caused
by anthropophilic dermatophytes and resembles common
kn kno ee
tinea corporis or bacterial folliculitis. Typically, erythematous
ed d fr
patches show an active border composed of papules, vesicles
m e or
and/or crusts, the so-called circinate type. Hair are loose or
w. M f
broken next to the skin or they plug the hair follicle. This
w by le
variety represents a chronic variant of tinea barbae. In the
(w ed ilab
Figure 5: Reduction in size of papules and nodules in beard area sycosiform variety, small follicular pustules are observed.
after 2 weeks of itraconazole therapy Complications of tinea barbae include secondary bacterial
st va
infection and permanent scarring alopecia following
ho a
resolution of inflammatory plaques and nodules.
te is
Tinea barbae may mimic sycosis barbae, contact dermatitis,
si F
a PD
acneiform dermatitis etc. and thus pose a diagnostic
problem.[1,2] Mycologic examination forms the basis of
is
diagnosis. Procedures include direct microscopy, culture
Th
and a Wood’s lamp examination in certain cases. Biopsy
specimens occasionally may be required to diagnose tinea
barbae. [2,3] Biopsy shows folliculitis and perifolliculitis
with a mixed cellular infiltrate and spongiosis within the
follicular epithelium. Lymphocytes or neutrophils are seen
Figure 6: Marked resolution of malar lesions after treatment within the follicular epithelium. Periodic acid-Schiff stain
(PAS) is recommended to clearly visualize fungal elements.
Arthroconidia and/or hyphae may be evident within the hair
Diagnosis: Tinea barbae shaft and follicle. An inflammatory infiltrate is present in the
dermis, which in chronic lesions may contain giant cells.
DISCUSSION
Tinea barbae is usually treated with specific systemic
Tinea barbae is a dermatophytosis of facial terminal hair of antifungals, griseofulvin (1 g/ day). Newer antifungals used
men, commonly seen in farmers, in rural areas and in those include terbinafine (250 mg/day), itraconazole (400 mg/day)
in contact with infected animals, especially in areas with and fluconazole (150 mg/week). All antifungals are used for
162 Indian J Dermatol Venereol Leprol|March-April 2007|Vol 73|Issue 2
Net Quiz
periods of two to four weeks depending upon the clinical improvement within two weeks of treatment [Figures 5-6].
response.[1,2,4]
Raghavendra Rao, Smitha Prabhu,
In our patient, a differential diagnosis of allergic contact Mamatha George, Shrutakirthi D. Shenoi
dermatitis and sycosis barbae had been considered. Patch Department of Skin and STD, KMC, Manipal, India.
test was negative and he had responded partially to oral and
topical antibiotics. KOH mount (20% KOH) of the hair from the Address for correspondence: Dr. Smitha Prabhu, Department of Skin
and STD, Kasturba Medical College, Manipal, Karnataka-576 104,
affected area showed ectothrix type of invasion. The diagnosis India. E-mail: smithaprabhu@msn.com
was further clinched by punch biopsy from a plaque lesion on
the malar area, which showed superficial dermatophytosis REFERENCES
with PAS stain. Another biopsy specimen sent for fungal
culture in Sabouraud’s dextrose agar (SDA) showed white, 1. Kanwar AJ, Mamta, Chander J. Superficial fungal infections. In: Valia
ns om
granular growth in the form of concentric circles after 10 RG, Valia AR, editors. IADVL Textbook and Atlas of Dermatology.
days. Trichophyton mentagrophytes was isolated from the 2nd ed. Bhalani Publishing House: Mumbai; 2001. p. 224.
tio fr
SDA tubes [Figure 4]. Christensen’s urease medium showed 2. Lin RL, Szepietowski JC, Schwartz RA. Tinea faciei, an often
). lica ad
deceptive facial eruption. Int J Dermatol 2004;43:437-40.
urease production [Figure 4]. Hair-perforation test showed
om b lo
3. Tinea barbae. Szepietovsky JC, Schwartz AR. [Last updated on
wedge-shaped perforations.
2005 May 26]. Available from: http://www.emedicine.com/derm/
.c Pu wn
topic419.htm. [Last accessed on 2006 Oct 11].
With this revised diagnosis of tinea barbae, the patient was
ow w do
4. Lesher JL Jr. Oral therapy of common superficial fungal infection
put on itraconazole 400 mg per day. There was a dramatic of the skin. J Am Acad Dermatol 1999;40:S31-4.
kn kno ee
ed d fr
m e or
w. M f
w by le
(w ed ilab
st va
ho a
te is
si F
a PD
is
Th
Indian J Dermatol Venereol Leprol|March-April 2007|Vol 73|Issue 2 163
You might also like
- Unit 2 MycoDocument11 pagesUnit 2 MycoElyssa VergaraNo ratings yet
- dermatophytes_20240314_214707_0000Document18 pagesdermatophytes_20240314_214707_0000khushi.gupta2122No ratings yet
- Tinea BarbaeDocument4 pagesTinea BarbaeKevin EdroNo ratings yet
- BJFM March 14 p22-23 Tinea Infection PDFDocument2 pagesBJFM March 14 p22-23 Tinea Infection PDFAlex WestNo ratings yet
- DERMATOLOGY - FinalsDocument5 pagesDERMATOLOGY - FinalsAdviento AngelicaNo ratings yet
- Mycology and Virology MYCV311: Bsmls TermDocument6 pagesMycology and Virology MYCV311: Bsmls TermIgnacias //No ratings yet
- Clinical Forms of DermatophytesDocument2 pagesClinical Forms of Dermatophytesbaihern24No ratings yet
- Microsporum canis Tinea CapitisDocument4 pagesMicrosporum canis Tinea CapitisAnonymous hxXpvZdZNo ratings yet
- Microbiology and Parasitology ReviewerDocument4 pagesMicrobiology and Parasitology ReviewerChrister Jon AcostaNo ratings yet
- FSPT Derma - CrumbsDocument8 pagesFSPT Derma - CrumbsGio GelilangNo ratings yet
- Superficial Mycoses: Causes, Symptoms and TreatmentDocument5 pagesSuperficial Mycoses: Causes, Symptoms and TreatmentEinstein ObladesNo ratings yet
- Dermatomycosis 18th July 2021Document120 pagesDermatomycosis 18th July 2021Sekar OktaviaNo ratings yet
- Fungal & Parasitic Infestations of The SkinDocument67 pagesFungal & Parasitic Infestations of The SkinGhaith HamdiNo ratings yet
- Dermatologic PresentationsDocument28 pagesDermatologic PresentationsSNo ratings yet
- Superficial Mycosis Diagnosis and TreatmentDocument3 pagesSuperficial Mycosis Diagnosis and TreatmentAmalia TauziahNo ratings yet
- Mycology Classification and Treatment GuideDocument5 pagesMycology Classification and Treatment GuideMnemo SyneNo ratings yet
- Birao Sas 14 Microbiology and ParasitologyDocument6 pagesBirao Sas 14 Microbiology and ParasitologyFrancis Jacob Dejecacion GarcesNo ratings yet
- Onychomycosis Identification Culture MethodsDocument1 pageOnychomycosis Identification Culture MethodsChristina A. SaleebNo ratings yet
- Cutaneous Mycoses Dermatophytoses: Dr. Vian B. Barzinjy MSC, PHD - MycologyDocument28 pagesCutaneous Mycoses Dermatophytoses: Dr. Vian B. Barzinjy MSC, PHD - MycologyPshtiwan MahmoodNo ratings yet
- KAYE ROJAS Skin Infection BSN 1 Y2 3Document10 pagesKAYE ROJAS Skin Infection BSN 1 Y2 3HERLIN HOBAYANNo ratings yet
- Skin ConditionsDocument3 pagesSkin ConditionsAlyssa AmayaNo ratings yet
- MYCOSESDocument41 pagesMYCOSESDayana PrasanthNo ratings yet
- Dermatophytes: Fungal Infections of the Skin, Hair and NailsDocument3 pagesDermatophytes: Fungal Infections of the Skin, Hair and NailsRabinNo ratings yet
- Scarlet Fever (Scarlatina) : Bacterial Infection Etiology Oral Manifestations Prevention and ControlDocument16 pagesScarlet Fever (Scarlatina) : Bacterial Infection Etiology Oral Manifestations Prevention and ControlFatima CarlosNo ratings yet
- Tinea Capitis Inggris CKDocument3 pagesTinea Capitis Inggris CKBhagawanta AptakayanaNo ratings yet
- FUNGIDocument11 pagesFUNGIIzenn De PazNo ratings yet
- Superficial and Cutaneous Mycoses: 2. Disease CharacteristicsDocument4 pagesSuperficial and Cutaneous Mycoses: 2. Disease CharacteristicsMA. ANGELI DELA CRUZNo ratings yet
- Homeopathic Management of Ring WormDocument3 pagesHomeopathic Management of Ring WormEditor IJTSRDNo ratings yet
- JR Type of FolliculitisDocument8 pagesJR Type of FolliculitisridhaNo ratings yet
- Myco Myco OwnDocument4 pagesMyco Myco OwnMarielle Anne TuazonNo ratings yet
- Ms 1 Integumentary NursingDocument10 pagesMs 1 Integumentary NursingTrinity Veach100% (1)
- Guide to Fungal Skin Infections (DermatomycosisDocument128 pagesGuide to Fungal Skin Infections (DermatomycosisDevy KurniawatiNo ratings yet
- Superficial Fungal Infections ExplainedDocument69 pagesSuperficial Fungal Infections Explainedputri.SpANo ratings yet
- DERMATOPHYTOSES: LAB DIAGNOSIS AND CLASSIFICATIONDocument34 pagesDERMATOPHYTOSES: LAB DIAGNOSIS AND CLASSIFICATIONKana FajarNo ratings yet
- Derma-Chronicles-issue 1 - 26-5-16 HiResDocument4 pagesDerma-Chronicles-issue 1 - 26-5-16 HiResParthMairNo ratings yet
- Superficial Mycosis and DermatophytosisDocument6 pagesSuperficial Mycosis and Dermatophytosisadinda sandyaNo ratings yet
- Cutaneous Mycoses Guide: Classification, Agents and Clinical ManifestationsDocument56 pagesCutaneous Mycoses Guide: Classification, Agents and Clinical ManifestationsHafsa ImranNo ratings yet
- Classification of Fungal Diseases ExplainedDocument8 pagesClassification of Fungal Diseases ExplainedLlermi LiborioNo ratings yet
- Skin Condition AssignmentDocument6 pagesSkin Condition AssignmenthahmendaNo ratings yet
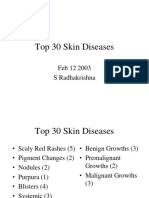
- Top 30 Skin DiseasesDocument32 pagesTop 30 Skin DiseasesjalalfaizNo ratings yet
- Inflammatory Tinea Capitis. A Clinical Case Presentation Treated With Oral TerbinafineDocument2 pagesInflammatory Tinea Capitis. A Clinical Case Presentation Treated With Oral TerbinafineSuci Triana PutriNo ratings yet
- Top 30 Skin DiseasesDocument32 pagesTop 30 Skin Diseasesapi-3728446No ratings yet
- Tinea BarbaeDocument4 pagesTinea BarbaewinNo ratings yet
- Microbiology 19 PDFDocument6 pagesMicrobiology 19 PDFLyka Villagracia AsiloNo ratings yet
- DDX Chart Part 4Document7 pagesDDX Chart Part 4api-26938624No ratings yet
- Mycology: Clinical FindingsDocument5 pagesMycology: Clinical FindingsLuqman Al-Bashir FauziNo ratings yet
- Causes, Types and Diagnosis of Superficial Fungal InfectionsDocument6 pagesCauses, Types and Diagnosis of Superficial Fungal InfectionsIM CTNo ratings yet
- Fungal Diseases of the Skin, Hair and Nails (DermatophytosisDocument48 pagesFungal Diseases of the Skin, Hair and Nails (DermatophytosisAsdfghjklNo ratings yet
- Macules - Week 1Document18 pagesMacules - Week 1Jordan ChuNo ratings yet
- Mycology Lecture FinalDocument258 pagesMycology Lecture FinalBahaa Shaaban100% (1)
- Fungal InfectionDocument3 pagesFungal InfectionNicole TorralbaNo ratings yet
- Microscopic Examination of Fungal SmearDocument73 pagesMicroscopic Examination of Fungal SmearAmeliaNo ratings yet
- Gerhard Grevers - M.D Rudolf Probst - Iro Heinrich Iro - Basic Otorhinolaryngology - A Step-By-Step Learning Guide (2018) - Libgen - LiDocument1 pageGerhard Grevers - M.D Rudolf Probst - Iro Heinrich Iro - Basic Otorhinolaryngology - A Step-By-Step Learning Guide (2018) - Libgen - LiShai SorianoNo ratings yet
- Fungal Diseases of the Skin: Types, Causes and TreatmentsDocument6 pagesFungal Diseases of the Skin: Types, Causes and TreatmentsputraimanullahNo ratings yet
- Superficial MycosesDocument26 pagesSuperficial Mycosesdhainey100% (3)
- General Surgery Copy 2Document37 pagesGeneral Surgery Copy 2sowmyaraja09No ratings yet
- Tinea CorporisDocument23 pagesTinea CorporisDita lewaherillaNo ratings yet
- Differential Diagnosis: Aureus Is The CommonestDocument5 pagesDifferential Diagnosis: Aureus Is The CommonestHestia Nur AnnisaNo ratings yet
- Macules Papules Plaques Nodules Bullae Pustules Urticaria (Wheals or HivesDocument10 pagesMacules Papules Plaques Nodules Bullae Pustules Urticaria (Wheals or HivesHERLIN HOBAYANNo ratings yet
- Aventus Batch Variation GuideDocument5 pagesAventus Batch Variation GuideJohnNo ratings yet
- Role of small-fiber afferents in pain mechanismsDocument10 pagesRole of small-fiber afferents in pain mechanismsJohnNo ratings yet
- 10 1016@j Jaad 2019 05 096Document8 pages10 1016@j Jaad 2019 05 096JohnNo ratings yet
- The Real One: This Is The Cover PageDocument2 pagesThe Real One: This Is The Cover PageJohnNo ratings yet
- DocumentDocument21 pagesDocumentJohnNo ratings yet
- Marri AGE Regi Strati ON Certi FI Cate: THE Govt OF Khyber Pakhtunkhwa Paki StanDocument1 pageMarri AGE Regi Strati ON Certi FI Cate: THE Govt OF Khyber Pakhtunkhwa Paki StanJohnNo ratings yet
- 100 Papers in Clinical Psychiatry Psychosomatic Medicine Management of Factitious Disorders A Systematic ReviewDocument10 pages100 Papers in Clinical Psychiatry Psychosomatic Medicine Management of Factitious Disorders A Systematic ReviewJohnNo ratings yet
- Treatment of Erythrodermic Psoriasis With BiologicsDocument8 pagesTreatment of Erythrodermic Psoriasis With BiologicsJohnNo ratings yet
- Pha Foundation: Membership Registration Form of Pha Residencia PeshawarDocument1 pagePha Foundation: Membership Registration Form of Pha Residencia PeshawarJohnNo ratings yet
- Erythrodermic Pemphigus Foliaceus A Rare Refractory Variant 2016Document1 pageErythrodermic Pemphigus Foliaceus A Rare Refractory Variant 2016JohnNo ratings yet
- FCPS-II LEPROSY ROTATION AT LADY READING HOSPITALDocument1 pageFCPS-II LEPROSY ROTATION AT LADY READING HOSPITALJohn100% (1)
- Vitiligo - NevuDocument1 pageVitiligo - NevuJohnNo ratings yet
- Handbook For Dermatology ResidentsDocument186 pagesHandbook For Dermatology ResidentsJohn100% (6)
- Rotation Cert - Sehrish SikanderDocument1 pageRotation Cert - Sehrish SikanderJohnNo ratings yet
- Classification Criteria Idiopathic Inflammatory MyopathiesDocument12 pagesClassification Criteria Idiopathic Inflammatory MyopathiesSomnath Das GuptaNo ratings yet
- Pruritis, WT Loss, Anemia, Hiccups, Oligurea, Inc BP, Bruises Edems, OsteoporosisDocument4 pagesPruritis, WT Loss, Anemia, Hiccups, Oligurea, Inc BP, Bruises Edems, OsteoporosisJohnNo ratings yet
- Comparison Between Topical Minoxidil and Topical RCPDocument7 pagesComparison Between Topical Minoxidil and Topical RCPJohnNo ratings yet
- Causes, Pathophysiology, & Teatment of PruritusDocument12 pagesCauses, Pathophysiology, & Teatment of PruritusJohnNo ratings yet
- A Summary of LeprosyDocument80 pagesA Summary of LeprosyJohnNo ratings yet
- Alopecia AreataDocument12 pagesAlopecia AreataJohnNo ratings yet
- Basic Skin Histopathology: Dr. Najeeb Ullah Khan Trainee Fcps Dermatology KTH PeshawarDocument82 pagesBasic Skin Histopathology: Dr. Najeeb Ullah Khan Trainee Fcps Dermatology KTH PeshawarJohn100% (1)
- Fungal InfectionDocument114 pagesFungal InfectionAini Shofa Haniah100% (1)
- Week 1 Grade 10 Tle Hair DressingDocument4 pagesWeek 1 Grade 10 Tle Hair DressingIsrael Marquez50% (2)
- Tinea CapitisDocument9 pagesTinea CapitisadityakafiberkahsmgNo ratings yet
- Microbiology: A Systems Approach: Cowan/TalaroDocument81 pagesMicrobiology: A Systems Approach: Cowan/TalaroKim ManlangitNo ratings yet
- Tinea Capitis: Current Review of The Literature: EpidemiologyDocument7 pagesTinea Capitis: Current Review of The Literature: EpidemiologyameliaNo ratings yet
- Goat Diseases and Farm Herd-Health SafetyDocument21 pagesGoat Diseases and Farm Herd-Health Safetyademola sanyaNo ratings yet
- Emergence of Trichophyton mentagrophytes as a common cause of Tinea CorporisDocument5 pagesEmergence of Trichophyton mentagrophytes as a common cause of Tinea CorporisjmuhilanNo ratings yet
- Efficacy and Safety of Terbinafine Hydrochloride 1 PDFDocument4 pagesEfficacy and Safety of Terbinafine Hydrochloride 1 PDFAlexandria Firdaus Al-farisyNo ratings yet
- Chapter-8 Human Health and Diseases ContinuationDocument9 pagesChapter-8 Human Health and Diseases ContinuationKeerthana D SNo ratings yet
- Human Health and Disease TomDocument19 pagesHuman Health and Disease TomReyneil ElumbaNo ratings yet
- Dermatophyte (Tinea) InfectionsDocument70 pagesDermatophyte (Tinea) InfectionsAndréia GomesNo ratings yet
- Microbiology For BNYS students NOTESDocument16 pagesMicrobiology For BNYS students NOTESKhan TestNo ratings yet
- Fungal Infections of The Skin: by Bekele T. (BSC, MSC) 1Document109 pagesFungal Infections of The Skin: by Bekele T. (BSC, MSC) 1desuloveNo ratings yet
- Common Rashes in ChildrenDocument6 pagesCommon Rashes in ChildrenStephanie AbnasanNo ratings yet
- Dermatomycosis 18th July 2021Document120 pagesDermatomycosis 18th July 2021Sekar OktaviaNo ratings yet
- Skin Pathology Notes SummaryDocument19 pagesSkin Pathology Notes SummaryyellowbieNo ratings yet
- Dermatofitosis FitzpatrickDocument28 pagesDermatofitosis FitzpatrickFadli IlhamNo ratings yet
- The 3500-Year History of Alopecia Areata ResearchDocument24 pagesThe 3500-Year History of Alopecia Areata ResearchmedifacuNo ratings yet
- Microbial Diseases of The Skin and Eyes (Microbiology Chapter 21)Document82 pagesMicrobial Diseases of The Skin and Eyes (Microbiology Chapter 21)Katrina Isabel100% (1)
- AkapulkoDocument18 pagesAkapulkoGladys Degala DizonNo ratings yet
- Economic Importance of FungiDocument14 pagesEconomic Importance of FungiShubham Lande100% (1)
- ZW 04 2021 04Document8 pagesZW 04 2021 04Aleksandra RuszewskaNo ratings yet
- Dr. SharanendraDocument156 pagesDr. SharanendraABhinav GangwarNo ratings yet
- Review: Tinea Corporis: An Updated ReviewDocument22 pagesReview: Tinea Corporis: An Updated ReviewMade SetiadjiNo ratings yet
- DermatophyteDocument8 pagesDermatophyteBhuvana RajNo ratings yet
- (OS 212.3) LEC 06.2 Fungal Infections of The Skin (A)Document7 pages(OS 212.3) LEC 06.2 Fungal Infections of The Skin (A)Ciara Marjorie HannaNo ratings yet
- Tinea CapitisDocument7 pagesTinea CapitisNadya LiemNo ratings yet
- TERBINAFINE HCLDocument38 pagesTERBINAFINE HCLBibek Singh MahatNo ratings yet
- Translate TineaDocument12 pagesTranslate TineaIndah Permata SariNo ratings yet
- School ChildcareDocument2 pagesSchool Childcarematt022005No ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)