Professional Documents
Culture Documents
CHAPTER 27 - Heart Failure With A Preserved Ejection Fraction
Uploaded by
Reda SoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CHAPTER 27 - Heart Failure With A Preserved Ejection Fraction
Uploaded by
Reda SoCopyright:
Available Formats
CHAPTER 27: Heart Failure with a Preserved Ejection Fraction
Ma. Arnee V. Anico-Tondo,M.D., FPCP (CGH)
Patients with heart failure can be divided into those with:
(1) heart failure with a reduced ejection fraction (HFrEF) and
(2) heart failure with a preserved ejection fraction (HFpEF)
Patients with HFpEF have a:
Devastating 5-year mortality rate (approaching 60%)
Costly morbidity (6-month hospitalization rate of 50%)
Debilitating symptoms (maximum myocardial oxygen consumption [MVO2] averaging 14 mL/g/min)
Patients with preserved EF are older and more likely to be female; however, HFpEF occurs in both men and women
throughout the 5th to the 9th decades of life
SYSTOLIC Most common antecedent disease leading to HFpEF
HYPERTENSION Present in more than 85% of patients
Ischemic heart disease is much less common than in HFrEF
Patients with HFpEF have normal LV end-diastolic volume and normal (or near-normal) EF and stroke volume and
commonly exhibit concentric remodeling of either LV chamber and/or cardiomyocytes
Standard heart failure therapy shown to be effective in HFrEF has not been found to reduce morbidity or mortality
associated with HFpEF, leaving a substantial area of unmet need
EPIDEMIOLOGY
Substantial proportion (more than 50% in many studies) of patients who are diagnosed or hospitalized with heart failure have
HFpEF
Prevalence of HFpEF increases dramatically with age
Much more common in women than in men at any age
Distribution of EF across unselected populations of patients with heart failure is bimodal, with peaks centered on 35% and
55% ( Data from OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart
Failure) registry and examined EF in 48,612 subjects)
Chapter 27: Heart Failure with a Preserved Ejection Fractions
NATURAL HISTORY
MORTALITY
5-year survival rate for all patients with heart failure, regardless of EF, is less than 50%
FIGURE 27-1 Prevalence and heart failure–related hospital admissions in patients with HFpEF
A, The percentage of patients with the HFpEF form of heart failure increased from 1987 to 2001, demonstrating that HFpEF
prevalence continues to rise
B, Over this same 15-year time frame, the number of heart failure– related hospitalizations in patients with HFrEF
remained stable or trended slightly downward, whereas in patients with HFpEF, the number increased significantly
Data from epidemiologic studies of HFpEF find that the annual mortality is approximately 10%, but RCTs in patients with
HFpEF suggest that the annual mortality is about 5%
In the RCTs, patients with HFpEF, who have antecedent and comorbid factors such as hypertension, coronary artery disease
and diabetes mellitus, were found to have more than twice the mortality rate of patients with hypertension, coronary artery
disease, or diabetes who do not have HFpEF
MODE OF DEATH
Most (>70%) of the deaths in patients with HFpEF are cardiovascular in nature, with 20% due to heart failure and 35% due to
sudden death
Incidence of noncardiovascular deaths is significantly higher for HFpEF (30%) than for HFrEF (15%), reflecting the higher age and
increased comorbidity in patients with HFpEF
arnee anico-tondo2018 “ad miorem dei gloriam”
1
MORBIDITY
Heart failure–related hospital readmission rates approximate 50% at 6 months for both HFrEF and HFpEF
Rates of progressive functional decline after hospital admission for heart failure also are similar in patients with HFpEF and in
those with HFrEF
Abnormalities in exercise tolerance, MVO2, and quality-of-life assessment are similar for HFrEF and HFpEF
CONVERSION FROM HEART FAILURE WITH PRESERVED EJECTION FRACTION TO HEART FAILURE WITH
REDUCED EJECTION FRACTION
Uncommon and generally is associated with an incident injury (such as myocardial ischemia)
One study, 1233 patients with heart failure had serial echocardiograms to determine the time course of changes in the LV EF over a 5-year
observation period
On average, the LV EF decreased by approximately 0.06 over 5 years in the HFpEF group, whereas it increased by nearly 0.07 in the HFrEF
group.
Rates should be interpreted in light of the following limitations: HFpEF and HFrEF were divided on the basis of an EF of 50%, no uniform
deterioration in EF occurred in patients with HFpEF
Study of 343 subjects with concentric LV remodeling (but no heart failure) found that over 7 years, only 7% developed eccentric
remodeling with LV dilation and a fall in EF
Although treatment of HFrEF may result in normalization of EF, a decline in EF in HFpEF appears usually to be due to an
intercurrent event, most frequently ischemic injury
PATHOPHYSIOLOGY
Pathophysiologic mechanisms that cause the development of HFpEF are reflected in changes in LV relaxation and filling, LV
structural remodeling and altered geometry, and changes in LV and vascular compliance
Chapter 27: Heart Failure with a Preserved Ejection Fractions
NORMAL DIASTOLIC PROPERTIES
Normal diastolic function allows the ventricle to fill adequately during rest and exercise, without an abnormal increase in left
atrial (LA) pressure
Phases of diastole:
Isovolumic pressure decline and filling
arnee anico-tondo2018 “ad miorem dei gloriam”
2
Filling phase is divided into early rapid filling, diastasis, and atrial systole
Contributes 70% to 80% of LV filling in normal individuals
Contribution diminishes with age and various disease states
Early diastolic filling is driven by the LA-to-LV pressure gradient, which is dependent on a
complex interplay of factors:
EARLY RAPID FILLING
- Myocardial relaxation
- LV elastic recoil
- LV diastolic stiffness
- LA pressures
- Ventricular interaction
- Pericardial constraint
- Pulmonary vein properties
- Mitral orifice area
Occurs in mid-diastole
DIASTASIS When the LA and LV pressures usually are almost equal
It contributes less than 5% of the LV filling, and its duration shortens with tachycardia
In normal subjects, contributes 15% to 25% of LV diastolic filling without raising the mean LA
pressure
ATRIAL SYSTOLE Contribution depends on the PR interval, atrial inotropic state, atrial preload, atrial afterload,
autonomic tone, and heart rate
LEFT VENTRICULAR RELAXATION
Active, energy-dependent process
Begins with the decay of force-generating capacity, follows the completion of the ejection phase of systole, and continues
through isovolumic pressure decline and the rapid filling phase
Filling is dependent both on active relaxation and on the recoil/suction that results from the release of potential energy
stored during systole by contraction. Thus blood is effectively “pulled” into the left ventricle
In normal hearts, over a range of normal heart rates, relaxation and recoil are adequate to allow LA pressures to remain
normal
In addition, catecholamine induced enhancement of relaxation and recoil during exercise lowers LV pressures in early
diastole, thereby increasing the LA-to-LV pressure gradient without increasing LA pressures as well as enhancing filling
during exercise
In patients with HFpEF, relaxation and recoil are abnormal at rest and are not enhanced during increased HR or exercise
As a result, filling can be maintained only by increased LA pressure; blood must be “pushed” into the left ventricle
ISOVOLUMIC PRESSURE DECLINE
Time course of isovolumetric pressure decline has been quantitatively described by the peak rate of pressure fall (dP/dt min)
Chapter 27: Heart Failure with a Preserved Ejection Fractions
and the time constant τ (tau) of the exponential fall in LV isovolumetric pressure
dP/dtmin measures the rate of pressure decline at a single point in time, is strongly influenced by the LV pressure at the
time of aortic valve closure, and therefore, like all indices of diastolic function, is afterload-dependent
Patients with HFpEF have a larger dP/dtmin, signifying that relaxation rate is decreased
Time constant τ describes the rate of LV pressure decline throughout isovolumic relaxation
Pressure (P) and time (t) data during the period from end-systole (aortic valve closure) to the onset of LV filling (mitral
valve opening) are fit to an exponential equation such as the following:
LV pressure = P0e−t/τ
Where:
P0 is LV pressure at end ejection
τ is the exponential time constant
The larger the value of τ, the longer it takes for the LV pressure to fall and the more impaired is relaxation
A normal value for τ is less than 40 milliseconds in most age groups, suggesting that relaxation is nearly complete by 3.5 ×
τ (less than 140 milliseconds)
Can be estimated by echo techniques as the time between aortic valve closure and mitral valve
Isovolumic relaxation opening
time (IVRT Useful in the noninvasive assessment of diastolic properties. However, depends not only on the
rate of LV relaxation but also on the aortic pressure at the time of aortic valve closure and the LA
arnee anico-tondo2018 “ad miorem dei gloriam”
3
pressure at mitral valve opening
Can be increased by an elevation of aortic pressure or decreased by an increase in LA pressure
Time course of LV pressure decline during isovolumetric relaxation can also be characterized using noninvasive Doppler
measurement of the velocity of a regurgitant jet across the mitral valve
Modified Bernoulli equation is used to approximate LV pressure during isovolumetric relaxation, allowing calculation of
the maximum rate of LV pressure decline and the exponential time constant
RECOIL AND LEFT VENTRICULAR FILLING
During systole, potential energy is stored in the elastic elements of the cardiomyocytes and extracellular matrix (ECM)
Elastic elements are compressed and twisted during systolic contraction
During relaxation, this potential energy is released as the elastic elements recoil and return to their original length and
orientation
Recoil causes LV pressure to fall rapidly during isovolumetric relaxation
For the first 30 to 40 milliseconds after mitral valve opening, the relaxation of LV wall tension normally is rapid enough to
cause LV pressure to continue to decline despite an increase in LV volume
This fall in LV pressure produces an early diastolic pressure gradient from the LA that extends to the LV apex
This accelerates blood out of the LA and produces rapid early diastolic flow that quickly propagates to the apex
Because the diastolic intraventricular pressure gradient pulls blood to the apex, it can be considered a measure of LV
suction
It is reduced in patients with ischemia, hypertrophic cardiomyopathy, and heart failure including HFpEF
Because the LV apex remains fixed during the cardiac cycle, the mitral annular velocity provides a measure of long-axis
lengthening rate
Under normal conditions, peak early diastolic mitral annular velocity (e’) occurs coincidentally with or before the mitral E
This is a manifestation of the symmetric expansion of the left ventricle in early diastole as blood moves rapidly to the LV
apex in response to a progressive pressure gradient from the left atrium to the LV apex
Rapid recoil of the mitral annulus and valve into the left atrium early in diastole relocates blood from the left atrium into
the left ventricle
Under normal circumstances, both E and e’ respond to changes in the LA-to-LV pressure gradient.
For example, both E and e′ normally increase in response to increased volume load and exercise
DETERMINANTS OF LEFT VENTRICULAR RELAXATION
Hemodynamic load (early diastolic load and afterload)
Myofiber inactivation
Uniformity of the distribution of load and inactivation in space and time (dyssynchrony, dyssynergy, Treppe)
HEMODYNAMIC LOAD
Chapter 27: Heart Failure with a Preserved Ejection Fractions
Both isovolumic pressure decline and early filling are affected by afterload (LV systolic stress)
An increase in LV systolic stress results in a delay in and slowed rate of pressure decline and early filling
Increases in LV pressure late in systole hasten the onset of LV relaxation, but relaxation occurs at a slower rate (increased τ)
Increases in LV pressure late in systole occur with aging because of age-related vascular stiffening, which alters the timing of
reflected pressure wave in the vascular tree so that the reflected wave arrives in late systole rather than diastole
An acute increase in blood pressure either at rest or during exercise will impair ejection, slow pressure decline, prolong time
to complete relaxation, and reduce recoil
These changes in relaxation decrease the LA-to-LV gradient, decrease early filling, and result in increased LV diastolic and LA
pressure
HETEROGENEITY
Will enhance LV relaxation...
Synchrony (timing of relaxation of the different myocardial segments)
synergy (extent to which myocardial segments relax)
Dyssynchrony or dyssynergy (e.g., caused by infarction, ischemia, asymmetry of hypertrophy, or conduction abnormalities)
will impair global LV relaxation
Dyssynchrony, measured using a variety of echocardiographic measurements, may be present in patients with HFpEF,
particularly those with left bundle branch block (LBBB) or right ventricular (RV) pacing
CELLULAR MECHANISM
Myofiber inactivation refers to the many cellular processes that ultimately influence the process by which the left ventricle,
arnee anico-tondo2018 “ad miorem dei gloriam”
4
its constitutive cardiomyocytes and individual sarcomeres return to a normal end-diastolic length with minimum cross-
bridge cycling and low force generation
To accomplish this state of complete relaxation requires:
(1) Calcium resequestration into the sarcoplasmic reticulum, followed by calcium extrusion into the extracellular space;
(2) Availability of sufficient ATP
(3) Normal myofilament function
(4) Normal elastic properties of the cardiomyocyte and the ECM
PREVALENCE AND PROGNOSIS FOR ABNORMAL RELAXATION
Impaired relaxation is present in HFpEF and contributes to the development of elevated LA pressure at rest
Rate of relaxation is further impaired during exercise and hemodynamic stress
Factor that shortens the diastolic filling period (prolonged contraction or long PR interval) will enhance the effect of
impaired relaxation on LV diastolic pressures during filling and thus affect the mean LA pressure needed to fill the left
ventricle
LEFT VENTRICULAR DIASTOLIC STIFFNESS, COMPLIANCE, AND DISTENSIBILITY
METHODS OF MEASUREMENT
Passive characteristics of the left ventricle during diastole can be described by the passive diastolic pressure-volume
relationship (DPVR)
Resultant DPVR is nonlinear and can be approximated by an exponential function
LV stiffness Defined as the ratio of LV diastolic pressure and LV diastolic volume (LV dP/dV) at any given LV
diastolic volume
LV compliance Reciprocal of stiffness (LV dV/dP)
Because the DPVR can be approximated as an exponential, stiffness will increase as the left ventricle fills to higher LV
diastolic volumes; thus as the left ventricle fills, it becomes stiffer
LV Defined as the end-diastolic pressure required to distend the left ventricle to an end-diastolic
diastolic distensibility volume
Patients with HFpEF have reduced distensibility, indicated by a normal or reduced end-diastolic volume and an elevated
end diastolic pressure
β does not indicate stiffness but instead describes how rapidly stiffness increased with increases in volume (β = [dP/dV]/V)
Patients with HFpEF have abnormal DPVRs with elevated β and abnormal distensibility
Chapter 27: Heart Failure with a Preserved Ejection Fractions
FIGURE 27-4 Difference in diastolic chamber distensibility in patients with HFpEF (in red) versus HFrEF (in black) versus
age- and gender-matched referent control subjects (in green)
Diastolic pressure-volume relationship in patients with HFpEF is shifted upward and to the left, such that for any given LV
volume, pressure is higher in HFpEF, indicating decreased distensibility (increased stiffness)
By contrast, in patients with HFrEF, the diastolic pressure-volume relationship is shifted to the right, indicating increased
distensibility
arnee anico-tondo2018 “ad miorem dei gloriam”
5
Patients with heart failure and an increased LV diastolic pressure can be divided into four groups defined by patterns of
DPVR (Diastolic Pressure Volume Relationship)
FIGURE 27-5 Mechanisms that result in increased LV diastolic pressure
DPVR in patients with HFpEF may be characterized by graphed curves A to C
In the most prevalent pattern in HFpEF, represented by curve B, the DPVR is shifted upward and to the left, indicating
reduced distensibility, where LV pressure is increased at any LV volume
In patients with HFpEF, when relaxation is markedly prolonged and diastole is abbreviated, as shown in curve A, LV diastolic
pressure falls throughout diastole but remains increased
In curve C, pericardial constraint causes a parallel upward shift in the DPVR
DPVR in patients with HFrEF typically is characterized by curve D, in which eccentric remodelling results in a shift of the
DPVR to the right, representing an increase in distensibility
It should be recognized that although the ventricle is more distensible, the end diastolic volume in these patients typically is
very large and the end-diastolic stiffness in the operating region is high
DETERMINANTS OF LEFT VENTRICULAR PRESSURE-VERSUS-VOLUME RELATIONSHIP
Two of the determinants associated with an upward and leftward shift of the DPRV in patients with HFpEF are the:
Presence of LV and cardiomyocyte concentric remodeling
Hypertrophy and changes in the material properties of myocardial muscle itself (i.e., myocardial stiffness)
Myocardial diastolic stiffness can be determined by assessing the myocardial diastolic LV stress versus strain relationship
Chapter 27: Heart Failure with a Preserved Ejection Fractions
Stress-strain relationship represents the resistance of the myocardium to stretch (increase in length) when subjected to stress
(distending force)
FIGURE 27-6 Changes in cardiomyocyte structure (A-C) and extracellular matrix fibrillar collagen (D-F) in HFpEF (outlined in red) versus HFrEF
(outlined in black) versus findings in referent control group (outlined in green). Arrows indicate fibrillar collagen
HFpEF is associated with concentric cardiomyocyte remodeling with increased diameter but no change in length and increased fibrillar
collagen content, thickness, and number
HFrEF is associated with eccentric cardiomyocyte remodeling with increased length but no change in width and fibrillar collagen
arnee anico-tondo2018 “ad miorem dei gloriam”
6
degradation and abnormal structure and turnover
CLINICAL FEATURES
DIAGNOSTIC CRITERIA
Diagnosis of HFpEF requires that:
Patient have signs and symptoms of heart failure
An EF greater than 50%
Objective evidence of cardiac dysfunction
FIGURE 27-7 Diagnostic criteria for HFpEF from the Heart Failure Society of America (HFSA) (left) and the European Society of Cardiology
(ESC) (right) guidelines.
Clinical manifestations of heart failure are similar regardless of the EF
These include reduced exercise tolerance, dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, peripheral
edema, and pulmonary congestion apparent on chest radiographs
No clinical features (symptoms, signs, or chest radiography) can be used to reliably distinguish between HFpEF
and HFrEF
In HFpEF the EF is not abnormal (i.e., EF >50%) and the end-diastolic volume is not increased, so an elevation of the
biomarker B-type natriuretic peptide (BNP) (or its N-terminal pro form), abnormal LV diastolic function (determined
Chapter 27: Heart Failure with a Preserved Ejection Fractions
noninvasively or by direct measurement of LV diastolic pressure), or elevated LA volume is required for the diagnosis of
HFpEF
Diagnosis of HFpEF requires the exclusion of noncardiac causes of symptoms and signs
BIOMARKERS
Natriuretic peptides, BNP Best-characterized biomarkers in patients with HFpEF
and N-terminal proBNP
(NT-proBNP)
Patients with HFpEF, increased BNP is directly related to LV diastolic filling pressure and end-diastolic wall stress
For any given LV diastolic filling pressure in patients with HFpEF, BNP levels are lower in obese patients and higher in
women, older persons, and patients with concomitant pulmonary disease (chronic obstructive disease, pulmonary
hypertension, and pulmonary embolus) and renal dysfunction
Because patients with HFpEF have a smaller LV cavity and thicker LV walls, their end-diastolic wall stress is much lower
than in HFrEF, even in the setting of high systolic and diastolic pressures, thus producing a lower stimulus for BNP
production
Patients with, HFpEF presenting with acute decompensation have:
BNP value of 100 to 500 pg/mL, versus 500 to 1500 pg/mL in patients with HFrEF
The standard partition values for BNP of 100 pg/mL and for NT-proBNP of 800 pg/mL have been suggested to
support the diagnosis of HFpEF
Both baseline values and change from baseline predict cardiovascular outcomes in patients with HFpEF
Elevation of BNP also indicates increased risk for subsequent events, even in asymptomatic persons
arnee anico-tondo2018 “ad miorem dei gloriam”
7
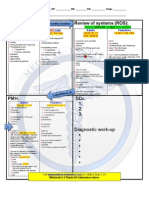
FIGURE e27-2
A, Baseline values of NT-proBNP have significant prognostic value and predict morbidity and mortality outcomes. The higher the baseline
value of NT-proBNP, the higher the rate of the primary and heart failure endpoints in the I-Preserve study.
B, Change from baseline values of NT-proBNP have significant prognostic value and predict morbidity and mortality outcomes. Data from the
I-Preserve study indicated that the directional change in NT-proBNP predicted primary and heart failure outcome rates
DEMOGRAPHIC FEATURES
Incidence of HFpEF increases with age, and the condition is more prevalent in women (may differ in specific populations)
African Americans may develop HFpEF at a younger age
Antecedent and co-morbid conditions are different in HFrEF versus HFpEF
History of hypertension is present in a majority of patients with HFpEF (80% to 90%), and the disorder may have
developed only later in life
Obesity is seen in 30% to 50%
Diabetes in 20% to 30%
Atrial fibrillation in up to 20% to 30% of patients
Prevalence of renal disease is high, and it may be progressive
Prevalence of coronary artery disease is 20% to 40%
Presence of each of these co-morbid conditions predicts higher morbidity and mortality
Medications used by patients with HFpEF and those with HFrEF are similar and include diuretics, digoxin, angiotensin
converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta blocking agents, calcium channel blocking
agents, and various other vasodilators and antihypertensive and antiarrhythmic drugs
Chapter 27: Heart Failure with a Preserved Ejection Fractions
comorbid conditions
AGING Incidence of HFpEF increases with age
LV diastolic function becomes abnormal with normal aging
Arterial, LV systolic, and LV diastolic stiffness increase with aging
Structural cardiac changes with aging (e.g., increased cardiomyocyte size, increased apoptosis
with decreased cardiomyocyte number, altered growth factor regulation, and focal collagen
deposition) and functional changes at the cellular level involving blunted beta-adrenergic
responsiveness, excitation-contraction coupling, and altered calcium handling proteins also may
contribute to diastolic dysfunction with normal aging
Some evidence suggests that prolonged, sustained endurance training may slow or prevent
some of the age-related changes
SEX Female sex is a potent risk factor for HFpEF
Women have more arterial and LV systolic and diastolic stiffness compared with men, and
arterial and ventricular stiffness increases more dramatically with age in women
HYPERTENSION Most commonly associated cardiac condition in patients with HFpEF
Chronically increased systolic blood pressure is an important stimulus for cardiac structural
remodeling and functional changes
Resultant hypertensive heart disease is characterized by concentric remodeling or overt LV
arnee anico-tondo2018 “ad miorem dei gloriam”
8
hypertrophy, increasing arterial and ventricular systolic stiffness, impaired relaxation, and
increased diastolic stiffness—all factors linked to the pathogenesis of HFpEF
CORONARY ARTERY DISEASE
ATRIAL FIBRILLATION Atrial fibrillation is recognized as a frequent precipitant of acute decompensation in patients
AND OTHER RHYTHM with HFpEF
DISTURBANCES Due to the loss of atrial contraction and to the resulting tachycardia
Atrial fibrillation may cause acute decompensation of heart failure in patients with diastolic
dysfunction, diastolic dysfunction (even in the absence of heart failure) results in left atrial
enlargement and increases the risk of atrial fibrillation
OBESITY Associated with an increased risk for heart failure regardless of EF
Patients with HFpEF are more often obese than patients with HFrEF
Prevalence of diastolic dysfunction is increased in obese persons
Increased body mass index (BMI) is a risk factor for hypertension, diabetes mellitus, coronary
artery disease, and atrial fibrillation
Dramatic weight loss with caloric restriction or bariatric surgery is associated with improved LV
diastolic function
DIABETES MELLITUS Potent risk factor for heart failure
Prevalence is similar in patients with HFrEF and in those with HFpEF
Morphologic changes in the diabetic heart include myocyte hypertrophy, increased
extracellular matrix (fibrosis), and intramyocardial microangiopath y
Functional changes include impaired endothelium-dependent and endothelium-independent
vasodilation, impaired LV relaxation, increased passive diastolic stiffness, and contractile
dysfunction
Mechanisms contributing to structural and functional coronary vascular and myocardial
changes include metabolic disturbances, activation of proinflammatory and profibrotic
mediators, cardiac autonomic neuropathy, and increases in advanced glycation end-products
(AGEs), which promote increased collagen accumulation and stiffness
CHRONIC KIDNEY DISEASE
SLEEP APNEA Can contribute to symptom severity
Likely to promote progression of heart failure
Central sleep apnea can occur in association with severe HFpEF
PULMONARY Most patients with HFpEF have at least some degree of pulmonary hypertension, with
HYPERTENSION pulmonary artery systolic pressures commonly greater than 40 mm Hg
Chapter 27: Heart Failure with a Preserved Ejection Fractions
Partly a consequence of the elevated LV filling pressures, with resulting increased pulmonary
venous pressure
Presence of increased pulmonary artery pressures has prognostic implications and is associated
with higher morbidity and mortality rates
RARER CAUSES OF HEART FAILURE WITH PRESERVED EJECTION FRACTION
Hypertrophic cardiomyopathy
Infiltrative cardiomyopathies such as amyloidosis , valvular disease, and constrictive pericarditis should always be
considered in patients with HFpEF
ACUTE DECOMPENSATED HEART FAILURE IN PATIENTS WITH HFPEF
Majority of patients hospitalized for ADHF have preexisting heart failure; at least 50% of these patients have HFpEF
Rehospitalizations are frequent, but many patients with HFpEF may be minimally symptomatic between episodes of ADHF
due to pulmonary congestion that accompanies increases in LV diastolic filling pressure
Both baseline LV diastolic filling pressure and changes in filling pressure are sensitive predictors of future ADHF events
ADHF in patients with HFpEF can result from increased filling pressure with or without significant changes in LV diastolic
volume
In patients with HFpEF, arterial hypertension, myocardial ischemia, and diabetes mellitus can act on preexisting structural
and functional abnormalities to cause deterioration in LV diastolic function and precipitate ADHF.
Atrial arrhythmias can result in loss of atrial function and stimulate compensatory increases in diastolic filling pressure in
arnee anico-tondo2018 “ad miorem dei gloriam”
9
order to maintain LV filling and maintain cardiac output
Decreased LV diastolic function and abnormal LA function can result in neurohormonal activation, which plays an important
role in ADHF by producing increased sodium and water retention, increased venous return, increased splanchnic tone, and
arterial vasoconstriction
CLINICAL ASSESSMENT OF CARDIOVASCULAR STRUCTURE AND FUNCTION
LEFT VENTRICULAR STRUCTURE
LEFT VENTRICULAR VOLUME
Most (>90%) patients with HFpEF have normal LV chamber dimension, area, and volume
Up to 5% of patients have a mild increase in LV volume above the upper normal partition value of 75 mL/m
LV volume less than 75 mL/m2 is one of the guidelines-based diagnostic criteria for HFpEF
LEFT VENTRICULAR MASS
LV mass is increased and reaches criteria for LV hypertrophy in roughly 30% to 50% of patients with HFpEF
Some evidence suggests that the prevalence of LV hypertrophy may be higher among African American patients and
women with HFpEF
When present, LV hypertrophy is associated with significantly worse prognosis
LEFT VENTRICULAR GEOMETRY
Ratio of LV mass to volume (M/V), or of LV wall thickness to LV internal dimension (relative wall thickness [RWT])
When mass or thickness is increased relative to (or out of proportion with) volume or dimension, the resultant changes
are termed concentric remodeling
Concentric remodelling can occur even in the absence of frank LV hypertrophy in approximately 20% to 30% of
patients with HFpEF and is associated with a 25% to 35% higher risk of heart failure events
LEFT VENTRICULAR FUNCTION
DIASTOLIC PROPERTIES
Chapter 27: Heart Failure with a Preserved Ejection Fractions
FIGURE 27-9 Evaluation of diastolic function based on the left ventricular filling dynamics determined by Doppler measurement of
mitral valve flow velocity and tissue Doppler measurement of mitral annular velocity
Normally the early diastolic mitral flow velocity (E) and the mitral annular velocity (e′) are brisk and occur nearly simultaneously
With mild diastolic dysfunction (impaired relaxation pattern—grade 1) the mitral E velocity is reduced and is less than the late
diastolic mitral flow velocity (A) The E deceleration time (DT) is increased
With more severe diastolic dysfunction (grades 2 and 3), E is increased and the DT is reduced. In these patterns, e′ is reduced and
delayed relative to the mitral E.
DIASTOLIC FUNCTION GRADE
(Echocardiographic and Doppler-echo based grading scale)
Most common clinical method of assessing severity of diastolic dysfunction
GRADE
0 Normal
Presence of mild diastolic dysfunction with slow LV relaxation
1 Abnormal Early diastolic pressure gradient between the left ventricle and the left
relaxation atrium that accelerates transmitral flow into the left ventricle is decreased
because there is no increase in LA pressure, and early LV diastolic
pressure is higher owing to abnormal relaxation
arnee anico-tondo2018 “ad miorem dei gloriam”
10
Decrease in both the early transmitral flow velocity E and early tissue
velocity, e', and an increase in the importance of late diastolic mitral flow
velocity (A), the transmitral velocity resulting from atrial contraction,
producing an E/A ratio less than 1
Occurs when progressive worsening of diastolic dysfunction is associated
with an increase in LA pressure and there is restoration of the early
diastolic pressure gradient despite increased early diastolic LV pressures.
These changes result in a return of the E wave to the normal range
2 Pseudonormalized (pseudonormal mitral inflow pattern)
Displacement of the left ventricle onto a steeper portion of the pressure-
volume curve results in a shortening of the DT
With slower relaxation, the e′ is delayed, occurring after the E
Indicates that the left ventricle is not expanding symmetrically in
diastole, but that propagation of filling to the apex and longitudinal
expansion occurs slowly after the left ventricle is filled by the movement
of blood from the left atrium into the LV inflow tract
Pseudonormal mitral inflow pattern is distinguished from normal by a reduced and delayed e′ and increase in the E/e′
ratio
3a Reversible restrictive Occurs when severe diastolic dysfunction causes a markedly slowed
3b Irreversible relaxation and elevated LA pressure
restrictive E increases further, DT becomes very short, and e′ is further reduced and
delayed resulting in a marked elevation of E/e′
Late diastolic annular velocity (a′) also may be reduced, and pulmonary
venous systolic forward flow velocity is reduced as well, to less than
diastolic forward flow velocity
If a Valsalva maneuver causes a reduction of E wave velocity, the
condition is designated reversible
If Valsalva does not change E, it is designated irreversible
NONINVASIVE ESTIMATION OF LEFT VENTRICULAR DIASTOLIC FILLING PRESSURE
Pseudonormalized and restricted filling patterns indicate the presence of both diastolic dysfunction and elevated LA
pressure
Impaired relaxation pattern indicates diastolic dysfunction without a marked elevation in LA pressure
Chapter 27: Heart Failure with a Preserved Ejection Fractions
Additional echo Doppler measurements that may reflect diastolic filling pressures include estimation of peak RV systolic
pressure (PRVSP) from the tricuspid regurgitation velocity and LA volume
Most common cause of increased pulmonary artery systolic pressure in HFpEF is an elevation of LA pressure
Echocardiographic parameters best correlated with PRVSP are DT and E/e′
Changes in LA volume reflect longer-term changes in LV filling pressures
LA volume is dependent on the product of diastolic pressure and time, so the longer pressures are increased and the
higher they are increased, the larger the LA volume
Abnormal diastolic dysfunction grade, increased PRVSP, and increased LA volume are highly prevalent in patients with
HFpEF and have significant prognostic value
See FIGURE 27-10 Prognostic significance of alterations in cardiac structure and function in patients with HFpEF. Left atrial enlargement (A),
diastolic dysfunction grade (B), and LV hypertrophy (C) increased the risk of primary and heart failure endpoints in the I-Preserve study
Most commonly used and easily interpretable parameter to estimate LA pressure is the E/e′ ratio
E/e′ has been found to correlate with pulmonary capillary wedge pressures (PCWPs)
E/e′ greater than 15 has been found to clearly indicate elevated PCWP
E/e′ less than 8 is associated with normal LA pressure
Cut-off value of E/e′ of 15 to recognize elevated LA pressure was obtained using e′ velocity from the medial mitral
annulus
Because e′ velocity from the lateral annulus usually is higher than the medial e′ velocity, the cut-off value should be
adjusted to 12 if the lateral annular velocity is used
Limitations in Use of E/e (see page 674 ebook)
arnee anico-tondo2018 “ad miorem dei gloriam”
11
1.In a normal heart, e′ occurs coincidentally with E and responds to changes in LA pressure
2.E/e′ does not increase in patients with constrictive pericarditis despite elevated PCWPs
Median e′ increases as constriction becomes worse, which results in a decrease in E/e′ as constriction gets more severe
and diastolic filling pressure increases (annulus paradoxus)
If the patient has clinical signs of heart failure, especially with increased jugular venous pressure, a normal or increased
median e′ velocity strongly suggests constrictive pericarditis
3.E/e′ may not provide an estimate of LA pressure in patients with mitral stenosis or mitral regurgitation, especially without a
reduction in EF
4.Although E/e′ correlates with LA pressure in patients with hypertrophic cardiomyopathy, the substantial scatter of data limits
its use alone in an individual patient
PREVALENCE AND PROGNOSIS FOR DIASTOLIC DYSFUNCTION IN HFPEF
Stage of diastolic dysfunction correlates with the impairment of exercise capacity in patients without myocardial ischemia,
whereas LV EF does not
In patients with heart failure, the stage of diastolic dysfunction is a stronger predictor of mortality than
EF
Indicates an increased LV operating stiffness
SHORT DT Hallmark of restrictive filling pattern
Connotes poor prognosis in patients with a history of myocardial infarction, persons with dilated
cardiomyopathy, heart transplant recipients, and patients with hypertrophic or restrictive
cardiomyopathy
Both pseudonormalized and restricted filling patterns are associated with a four-fold increase in the risk of death in patients
with heart failure and coronary artery disease
Patients with HFpEF, abnormal diastolic function measured as diastolic dysfunction grade or LA enlargement also predicts
marked increase in morbidity and mortality events
SYSTOLIC PROPERTIES
Patients with HFpEF have a normal (or near-normal) EF
Patients with HFpEF have normal dP/ dtmax, stoke volume, stroke work, and preload recruitable stroke work
Indices of chamber contractility such as LV end-systolic elastance are actually increased in HFpEF, matching the increased
arterial elastance, so that the coupling between these properties is preserved
Because systolic and arterial elastances are increased in HFpEF, exercise-induced increases in RAAS and sympathetic
stimulation are unable to augment systolic properties sufficiently to maintain adequate stroke volume
THERAPY
Chapter 27: Heart Failure with a Preserved Ejection Fractions
“No treatment has yet been shown, convincingly, to reduce morbidity or mortality in patients with HFpEF”
SUMMARY RANDOMIZED CONTROLLED TRIALS
988 patients with ambulatory HFpEF (EF >45%) in normal sinus rhythm
Digoxin did not alter the primary endpoint of heart failure-–related hospitalization
Digitalis Investigators Group or cardiovascular mortality but did reduce the number of such hospitalizations
(DIG) Trial Total cardiovascular hospitalizations were not reduced, however, because of an
increased rate of admissions for unstable angina, which completely negated the
benefit of reduced heart failure hospitalizations
Evaluated the ARB candesartan in patients with heart failure
Candesartan in Heart Failure: In the CHARM Preserved arm, patients with heart failure and an EF above 40%
Assessment of Reduction in were randomly assigned to receive candesartan or placebo in addition to standard
Mortality and Morbidity
therapy
(CHARM)
Fewer patients in the candesartan group than in the placebo group reached the
primary endpoint of cardiovascular death or heart failure–related hospitalization, a
finding that reached statistical significance only after adjustment for small
differences in baseline characteristics
Furthermore, there was no impact on mortality
arnee anico-tondo2018 “ad miorem dei gloriam”
12
Older than 70 years of age with HFpEF (EF >0.45) with echocardiographic evidence
of diastolic dysfunction
Randomly assigned to receive perindopril (an ACE inhibitor) or placebo
Perindopril in Elderly People Primary endpoint was a composite of all-cause mortality or unplanned heart
with Chronic Heart Failure failure–related hospitalization
(PEP-CHF) trial Both enrolment and event rates were lower than anticipated, and a high rate of
cessation of blinded therapy, with crossover to open-label ACE inhibitor use, was
reported for both groups.
These factors limited the power of the study, which did not show significant
reduction in the primary endpoint
Some trends toward benefit, primarily driven by reduction in heart failure–related
hospitalizations, were observed in a post hoc analysis of the results at 1 year, when
crossover therapy rates were lower
Tested the ARB irbesartan in 4128 patients who were at least 60 years of age and
had New York Heart Association (NYHA) class II, III, or IV heart failure, with an EF
Irbesartan in Heart Failure with above 45%
Preserved Ejection Fraction Primary outcome was death from any cause or hospitalization for a cardiovascular
Study (I-Preserve) cause (heart failure, myocardial infarction, unstable angina, arrhythmia, or stroke)
Secondary outcomes included death from heart failure or hospitalization for heart
failure, death from any cause and from cardiovascular causes, and impaired quality
of life.
Irbesartan had no effect on any of the prespecified outcomes
Tested the effect of the beta1-selective blocking agent nebivolol in patients
Study of the Effects of with heart failure without an EF requirement
Nebivolol Intervention on Modest but significant reduction was observed in the primary endpoint of all-cause
Outcomes and mortality or cardiovascular hospitalizations, driven primarily by the effect on
Rehospitalization in Seniors hospitalizations
with Heart Failure (SENIORS) Prespecified subgroup analysis in patients with EF above versus below 35% did not
trial detect any trends toward reduced benefit in those with higher EF very few patients
with EF above 50% were included in the trial
Thus it is not possible to draw conclusions about the benefit of beta blocking agents
in HFpEF from this study
Analysis of a large observational study found no mortality benefit of treatment with
a beta blocking agent after a hospitalization for heart failure in patients with EF
Chapter 27: Heart Failure with a Preserved Ejection Fractions
above 40%
Phase II Studies of Novel Pharmacologic Treatment of HFpEF
Prospective comparison of ARNI Patients with NYHA class II or III HFpEF (EF >45%) and NT-proBNP level greater than
versus ARB on Management of 400 pg/mL
Heart Failure with Preserved Cohort of 149 patients were assigned to receive therapy with LCZ696 (200 mg twice
Ejection Fraction daily) and another 152 patients to receive valsartan (160 mg twice daily) for 36
(PARAMOUNT) weeks
Primary endpoint was change in NT-proBNP from baseline to 12 weeks
At 12 weeks, LCZ696 significantly reduced NT-proBNP by approximately 15%,
compared with valsartan (no significant change; for difference in response, P = .005)
At 36 weeks, LCZ696 significantly reduced LA volume by approximately 5%
compared with valsartan (no significant change; for difference in response, P = .003)
LCZ improved NHYA functional class versus valsartan (P = .05)
LCZ696 was well tolerated, with adverse effects similar to those for valsartan.
Whether these findings will translate into improved outcomes need to be tested in a
large randomized trial
RELAX trial Sildenafil was studied in a larger group of patients with HFpEF without a requirement
for having pulmonary hypertension, no improvement was observed in exercise
arnee anico-tondo2018 “ad miorem dei gloriam”
13
tolerance or diastolic function
To date, spironolactone has been shown to improve indices of diastolic function but not clinical outcomes
MANAGEMENT OF HEART FAILURE WITH PRESERVED EJECTION FRACTION
Three main components
Reduction and prevention of Fluid and sodium restriction, judicious use of diuretics and nitrates, selective
pulmonary and peripheral venous application of neurohormonal modulation, and appropriate remote monitoring–
congestion based tailored care
Aggressive treatment of antecedent Controlling blood pressure at rest and modifying blood pressure response to
and comorbid diseases exercise, controlling glucose, treating and preventing ischemia, and maintaining
adequate renal function
Optimization of cardiac functional Prevent excessive tachycardia or bradycardia, to match heart rate to metabolic
status needs, to maintain or restore normal sinus rhythm, and to control ventricular
response rate during atrial arrhythmias
NONPHARMACOLOGIC THERAPY
Attention to diet and lifestyle, avoidance or reversal of obesity, increase in exercise, adherence to management strategies,
daily monitoring of weight, patient education, and close medical follow-up using facilitated home management
Sodium restriction to less than 2 g/day may be effective
TREATMENT OF COMORBID CONDITIONS
Most important and frequent comorbid conditions include arterial hypertension, obesity, diabetes, chronic kidney disease,
obstructive sleep apnea, and anemia
Most patients (>85%) with HFpEF have either current or previous hypertension
Untreated hypertension is a strong risk factor for the development of heart failure
Treatment of systolic hypertension in elderly patients (who have the highest risk for development of HFpEF) is associated
with a more than 50% reduction in the frequency of heart failure
Goal of therapy is systolic arterial pressure below 140 mm Hg and diastolic blood pressure below 90 mm Hg
GFR is an important predictor of outcomes in patients with HFpEF, with decreasing estimated GFR predicting increased
event rates
Anemia is common in HFpEF and is associated with a worse prognosis
PHARMACOLOGIC AND DEVICE-BASED STRATEGIES
Prospective RCTs have evaluated the efficacy of digitalis, ACE inhibitors, ARBs, and beta blocking agents in patients with
HFpEF; each of these studies found no clear benefit to these therapies
RAAS antagonism is thus an important component of treatment in patients with HFpEF, particularly to manage hypertension,
prevent or reverse LV hypertrophy, and preserve renal function in patients with diabetes
REMOTE MONITORING SYSTEMS TO HELP TAILOR MANAGEMENT
Chronicle Offers Management to 70 patients with HFpEF (with EF >50%) were studied using an implantable
Chapter 27: Heart Failure with a Preserved Ejection Fractions
Patients with Advanced Signs hemodynamic monitor (IHM) that measured an estimated pulmonary artery diastolic
and Symptoms of Heart Failure pressure (ePAD)
(Compass-HF) trial Measurement that in the absence of pulmonary vascular disease approximates
PCWP
This study demonstrated that:
(1) patients with HFpEF demonstrated significantly increased filling pressures even
while they were considered to be in a compensated state by their physicians;
(2) these pressures rose further when they became decompensated
(3) both baseline pressures and change from baseline pressures predicted outcomes
CardioMEMS Heart Sensor Allows Those in the active treatment arm demonstrated a 152% decrease in pulmonary
Monitoring of Pressure to Improve artery diastolic and systolic pressures and a 52% decrease in heart failure– related
Outcomes in NYHA class III Heart events (both P < .0001 and control)
Failure Patients (CHAMPION) trial
Left Atrial Pressure Monitoring to
Optimize Heart Failure Therapy
(LAPTOP-HF) trial
Repeated measurements of biomarkers, both office- and home-based, are being evaluated. These include use of BNP (HABIT-I
and -II study) and galectin (REGAL-HF study)
arnee anico-tondo2018 “ad miorem dei gloriam”
14
NEUROHORMONAL MODULATION
Aggressive and effective management of hypertension is an essential component of treatment in HFpEF
Complete management of HFpEF includes the prevention of the development of LV hypertrophy or the induction of its
regression.
ACC/AHA GUIDELINES
Systolic and diastolic blood pressure should be controlled in patients with 2013 recommendation remains
I B HFpEF in accordance with published clinical practice guidelines to prevent current.
morbidity
Diuretics should be used for relief of symptoms due to volume overload in 2013 recommendation remains
I C
patients with HFpEF. current.
Coronary revascularization is reasonable in patients with CAD in whom 2013 recommendation remains
IIa C symptoms (angina) or demonstrable myocardial ischemia is judged to be current.
having an adverse effect on symptomatic HFpEF despite GDMT.
Management of AF according to published clinical practice guidelines in 2013 recommendation remains
IIa C
patients with HFpEF is reasonable to improve symptomatic HF. current.
The use of beta-blocking agents, ACE inhibitors, and ARBs in patients with 2013 recommendation remains
IIa C
hypertension is reasonable to control blood pressure in patients with HFpEF. current.
In appropriately selected patients with HFpEF (with EF ≥45%, elevated BNP NEW: Current recommendation
levels or HF admission within 1 year, estimated glomerular filtration rate >30 reflects new RCT data.
IIb B-R
mL/min, creatinine <2.5 mg/dL, potassium <5.0 mEq/L), aldosterone receptor
antagonists might be considered to decrease hospitalizations.
The use of ARBs might be considered to decrease hospitalizations for patients 2013 recommendation remains
IIb B
with HFpEF. current.
Chapter 27: Heart Failure with a Preserved Ejection Fractions
III: No Routine use of nitrates or phosphodiesterase-5 inhibitors to increase activity NEW: Current recommendation
B-R
Benefit or QoL in patients with HFpEF is ineffective. reflects new data from RCTs.
III: No Routine use of nutritional supplements is not recommended for patients with 2013 recommendation remains
C
Benefit HFpEF. current.
arnee anico-tondo2018 “ad miorem dei gloriam”
15
You might also like
- Welcome Plan Welcome CorpsDocument20 pagesWelcome Plan Welcome CorpsAxmed Cadnaan50% (2)
- Cardiovascular System: Mungcal, Dharlynette RTRPDocument77 pagesCardiovascular System: Mungcal, Dharlynette RTRPDharlyn MungcalNo ratings yet
- Valvular Heart DiseaseDocument27 pagesValvular Heart DiseaseOwen J. WieseNo ratings yet
- ECG Rhythm Strip Interpretation Lesson 4Document5 pagesECG Rhythm Strip Interpretation Lesson 4phoebjaetanNo ratings yet
- Interview-Questions (ADNOC LNG)Document19 pagesInterview-Questions (ADNOC LNG)Chen XinNo ratings yet
- Anesthesia for Congenital Heart DiseaseFrom EverandAnesthesia for Congenital Heart DiseaseStephen A. StayerNo ratings yet
- Assessment of bleeding Shock in a Politraumatized PatientFrom EverandAssessment of bleeding Shock in a Politraumatized PatientNo ratings yet
- Rhythm Control Versus Rate Control in Atrial Fibrillation - UpToDocument39 pagesRhythm Control Versus Rate Control in Atrial Fibrillation - UpTohatsune100% (1)
- LTF InterpretationDocument3 pagesLTF InterpretationkiethyanNo ratings yet
- Use of Vasopressors and Inotropes - UpToDateDocument18 pagesUse of Vasopressors and Inotropes - UpToDateAlbertoMarteNo ratings yet
- Atrial Fibrillation and Flutter After Cardiac Surgery - UpToDateDocument22 pagesAtrial Fibrillation and Flutter After Cardiac Surgery - UpToDateFlavia SaccomaniNo ratings yet
- Heart DiseaseDocument38 pagesHeart DiseaseDr.Sunil KumarNo ratings yet
- Prevention of DVT/PE: Noornadia BT Yahaya 050100841Document32 pagesPrevention of DVT/PE: Noornadia BT Yahaya 050100841Nadia YahayaNo ratings yet
- Left Ventricular Assist DevicesDocument14 pagesLeft Ventricular Assist DevicesLuis Alberto Caneo VergaraNo ratings yet
- Acls Course HandoutsDocument8 pagesAcls Course HandoutsRoxas CedrickNo ratings yet
- Acute Heart FailureDocument71 pagesAcute Heart FailureVivek Anandan100% (1)
- HW InotropesDocument3 pagesHW InotropesNatalie YeohNo ratings yet
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDocument4 pagesRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniNo ratings yet
- Dysrhythmias: Sinus Node Dysrhythmias Tachycardia, and Sinus ArrhythmiaDocument5 pagesDysrhythmias: Sinus Node Dysrhythmias Tachycardia, and Sinus ArrhythmiaKayelyn-Rose Combate100% (1)
- Approach To The Patient With Respiratory DiseaseDocument6 pagesApproach To The Patient With Respiratory DiseaseRem AlfelorNo ratings yet
- Cerebrovascular AccidentDocument31 pagesCerebrovascular AccidentRam ReddyNo ratings yet
- Acid-Base BalanceDocument5 pagesAcid-Base BalanceCarl Earvin L. FavoritoNo ratings yet
- HANDOUTS-Non Invasive VentilationDocument15 pagesHANDOUTS-Non Invasive VentilationKristine MangasepNo ratings yet
- PFT Interpretation AlgorithmDocument4 pagesPFT Interpretation AlgorithmJason Steel50% (2)
- Ischemic Heart DiseaseDocument28 pagesIschemic Heart DiseaseLiusHarimanNo ratings yet
- Cardiac Output and Hemodynamic MeasurementDocument29 pagesCardiac Output and Hemodynamic Measurementdeepa100% (1)
- ASCITESDocument25 pagesASCITESGanesh BabuNo ratings yet
- Valvular Heart Disease: Presented by DR Mirjana Milutinovic Professor, SJSMDocument69 pagesValvular Heart Disease: Presented by DR Mirjana Milutinovic Professor, SJSMAbanoub AwadallaNo ratings yet
- 01 Hypertension - 2019 2020 PDFDocument122 pages01 Hypertension - 2019 2020 PDFbaraa abu sneineh100% (1)
- Renal - Replacement - TherapyDocument128 pagesRenal - Replacement - TherapyEmNo ratings yet
- Mitral Valve Prolapse, Flailed Mitral Valve Mitral Annular CalcificationDocument33 pagesMitral Valve Prolapse, Flailed Mitral Valve Mitral Annular CalcificationcafemedNo ratings yet
- Acs Nstemi PathwayDocument3 pagesAcs Nstemi PathwayAliey's SKeplek NgeNersNo ratings yet
- Pakrat 10Document67 pagesPakrat 10towexpertNo ratings yet
- Acid-Base Disorders NotesDocument10 pagesAcid-Base Disorders NotesLovely100% (1)
- How To Treat: Septic ShockDocument6 pagesHow To Treat: Septic ShockmeeandsoeNo ratings yet
- Cardiovascular Nursing: Study Online atDocument7 pagesCardiovascular Nursing: Study Online atLilly DayeNo ratings yet
- Vasoactive Agents For Adult Septic Shock: An Update and ReviewDocument10 pagesVasoactive Agents For Adult Septic Shock: An Update and ReviewntnquynhproNo ratings yet
- Treatment of Resistant and Refractory HypertensionDocument21 pagesTreatment of Resistant and Refractory HypertensionLuis Rodriguez100% (1)
- Ch-13 Drugs Used in Heart FailureDocument49 pagesCh-13 Drugs Used in Heart FailureShabrin SadikhNo ratings yet
- Milrinone Can ONLY Be Mixed With NS!: Alpha 1 Beta 1 & Alpha 1Document1 pageMilrinone Can ONLY Be Mixed With NS!: Alpha 1 Beta 1 & Alpha 1njones33No ratings yet
- VasculitidesDocument13 pagesVasculitidesIrene Zae MwandotoNo ratings yet
- Valvular Heart Disease and Non Cardiac Surgery: Lakshmi P. YalavarthyDocument44 pagesValvular Heart Disease and Non Cardiac Surgery: Lakshmi P. YalavarthyLakshmi YalavarthyNo ratings yet
- MayoclinprocDocument12 pagesMayoclinprocpriyaNo ratings yet
- COPD Updated Guidelines and Newer TherapiesDocument90 pagesCOPD Updated Guidelines and Newer TherapiesVlad Constantin100% (1)
- 10.08.07 Cardiac Tamponade HaagDocument16 pages10.08.07 Cardiac Tamponade HaagfoetorNo ratings yet
- DO /VO Relationships: J. L. VincentDocument8 pagesDO /VO Relationships: J. L. VincentLucas Cárcamo SaavedraNo ratings yet
- Clinical Cheat Sheet: Radiographic AssessmentDocument1 pageClinical Cheat Sheet: Radiographic AssessmentTracy PopeNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Heart Failure With Preserved Ejection FractionDocument19 pagesHeart Failure With Preserved Ejection Fractioncosmin balanNo ratings yet
- Pre Assessment Diabetes Nursing CareDocument4 pagesPre Assessment Diabetes Nursing CareHabib UllahNo ratings yet
- Rosenberg Circulatory Assist DevicesDocument61 pagesRosenberg Circulatory Assist DevicesMilisha Albro100% (1)
- Cardio-Vascular Disease: Mitral Stenosis & Mitral RegurgitationDocument25 pagesCardio-Vascular Disease: Mitral Stenosis & Mitral Regurgitationyulia silviNo ratings yet
- Sign and SymptomsDocument8 pagesSign and SymptomsCaral Grace Gatdula-PenalbaNo ratings yet
- 2018 AHA Guidelines BradicardiaDocument106 pages2018 AHA Guidelines BradicardiaArio Richard NinaNo ratings yet
- Left Ventricular Non-CompactionDocument20 pagesLeft Ventricular Non-CompactionlawlietNo ratings yet
- Hemodynamics in The Cath Lab 2Document45 pagesHemodynamics in The Cath Lab 2usfcards100% (1)
- Guidelines For Platelet Transfusions in Dengue FeverDocument4 pagesGuidelines For Platelet Transfusions in Dengue FeverGuru Prasad100% (1)
- Cardiac - Potpourri Rev 2015Document80 pagesCardiac - Potpourri Rev 2015Sanaz NikiNo ratings yet
- S1 and S2: Valves) at The Start of The Systolic Contraction of The VentriclesDocument10 pagesS1 and S2: Valves) at The Start of The Systolic Contraction of The VentriclesCHARIEMAE CA�AZARESNo ratings yet
- Pericarditis 65 SlidesDocument65 pagesPericarditis 65 SlidesAtifBhoreNo ratings yet
- Lecture 4: Hypovolemic ShockDocument20 pagesLecture 4: Hypovolemic Shockj.doe.hex_87No ratings yet
- Chinese General Hospital and Medical Center Department of Medical Education and Research Research Ethics Review Board (Rerb)Document11 pagesChinese General Hospital and Medical Center Department of Medical Education and Research Research Ethics Review Board (Rerb)Reda SoNo ratings yet
- Name: - Year LevelDocument6 pagesName: - Year LevelReda SoNo ratings yet
- Tilt Table Testing: Name Age/Sex APDocument1 pageTilt Table Testing: Name Age/Sex APReda SoNo ratings yet
- EXAM-MITRAL VALVE DISEASE - Reda SoDocument5 pagesEXAM-MITRAL VALVE DISEASE - Reda SoReda SoNo ratings yet
- Answer Key-Mitral ValveDocument6 pagesAnswer Key-Mitral ValveReda SoNo ratings yet
- Ward Reflection PaperDocument1 pageWard Reflection PaperReda SoNo ratings yet
- Chapter 32 - Genetic Cardiac ArrythmiasDocument7 pagesChapter 32 - Genetic Cardiac ArrythmiasReda SoNo ratings yet
- Private Ward Admission Census 1Document6 pagesPrivate Ward Admission Census 1Reda SoNo ratings yet
- Risk Factors in Developing Diabetic Foot Ulcers Among Patients in DM Foot Clinic at East Avenue Medical Center From January 2013 To January 2015Document7 pagesRisk Factors in Developing Diabetic Foot Ulcers Among Patients in DM Foot Clinic at East Avenue Medical Center From January 2013 To January 2015Reda SoNo ratings yet
- CHAPTER 11: The History and Physical Examination: An Evidence Based ApproachDocument5 pagesCHAPTER 11: The History and Physical Examination: An Evidence Based ApproachReda SoNo ratings yet
- Coronary Blood Flow & Myocardial Ischemia Cardiology Fellows Exam July 23, 2018Document3 pagesCoronary Blood Flow & Myocardial Ischemia Cardiology Fellows Exam July 23, 2018Reda SoNo ratings yet
- Vascular Conference: JUNE 2018 - MARCH 2019Document2 pagesVascular Conference: JUNE 2018 - MARCH 2019Reda SoNo ratings yet
- Rapid Response Team and Cardiac Arrest/Resuscitation TeamDocument11 pagesRapid Response Team and Cardiac Arrest/Resuscitation TeamReda SoNo ratings yet
- Trials SummaryDocument12 pagesTrials SummaryReda SoNo ratings yet
- Daily Activities 2019Document1 pageDaily Activities 2019Reda SoNo ratings yet
- Team BLDG LetterDocument1 pageTeam BLDG LetterReda SoNo ratings yet
- Tilt Table Testing: Name Age/Sex APDocument1 pageTilt Table Testing: Name Age/Sex APReda SoNo ratings yet
- ECHO CensusDocument9 pagesECHO CensusReda SoNo ratings yet
- Case Protocol 3Document5 pagesCase Protocol 3Reda SoNo ratings yet
- Compu Ted Tomogra Phy: (M90Us - LiDocument1 pageCompu Ted Tomogra Phy: (M90Us - LiReda SoNo ratings yet
- 2011 PadDocument19 pages2011 PadReda SoNo ratings yet
- December 12Document12 pagesDecember 12Reda SoNo ratings yet
- Research ProtocolDocument13 pagesResearch ProtocolReda SoNo ratings yet
- Mckee 2012Document10 pagesMckee 2012Reda SoNo ratings yet
- Sept 3 2017Document7 pagesSept 3 2017Reda SoNo ratings yet
- 7 Overview of LipidDocument85 pages7 Overview of LipidReda SoNo ratings yet
- IungDocument8 pagesIungReda SoNo ratings yet
- Punjab Medicolegal Manual Jan30 PDFDocument18 pagesPunjab Medicolegal Manual Jan30 PDFFrank NobodNo ratings yet
- Application Form - FMU (New Form BUPA)Document16 pagesApplication Form - FMU (New Form BUPA)gabinicolescu9999No ratings yet
- Autism PDFDocument25 pagesAutism PDFTalal 197No ratings yet
- 04telkom OkDocument248 pages04telkom OksilvaniNo ratings yet
- A - Pratic Guide Pediatric Wound CareDocument9 pagesA - Pratic Guide Pediatric Wound CareLicia GabrielleNo ratings yet
- Personal Development: Performance TaskDocument3 pagesPersonal Development: Performance TaskharrygolunaNo ratings yet
- Surveying Lab Manual 21cv32 - 2022Document82 pagesSurveying Lab Manual 21cv32 - 2022Tamil Selvi CIVILNo ratings yet
- PCT For BodybuildersDocument12 pagesPCT For BodybuildersJon Mester100% (4)
- Biotech SyllabusDocument2 pagesBiotech Syllabusmeet2abhayNo ratings yet
- AcuitSign M8&M6&M5&M3 User's Manual 20141215 - CompressedDocument305 pagesAcuitSign M8&M6&M5&M3 User's Manual 20141215 - CompressedElectromedycal EQUIPO MEDICONo ratings yet
- Reading and Writing - q3 - Las 1-2 RTPDocument4 pagesReading and Writing - q3 - Las 1-2 RTPRenz Ian T. DacoronNo ratings yet
- Makassar 1: Total Target OptimisDocument2 pagesMakassar 1: Total Target OptimisAchaElmanNo ratings yet
- Mil PRF 680CDocument12 pagesMil PRF 680CfltpNo ratings yet
- OSCE Checklist Cervical Screening SmearDocument2 pagesOSCE Checklist Cervical Screening SmearNoreen Hannah GabrielNo ratings yet
- Erich Fromm - A Therapeutic Vision Well Ahead of Its TimeDocument8 pagesErich Fromm - A Therapeutic Vision Well Ahead of Its TimeSteluța DrâmbuNo ratings yet
- TOK SampleDocument5 pagesTOK SampleLucianna CheilasNo ratings yet
- THE - Jose SILVA - METHODDocument43 pagesTHE - Jose SILVA - METHODszijsaNo ratings yet
- Sonography ProjectDocument9 pagesSonography Projectapi-685351719No ratings yet
- Time Management Training by Lisa J DownsDocument6 pagesTime Management Training by Lisa J DownssoberNo ratings yet
- InformationDocument3 pagesInformationابراهيم عماد نجم محمدNo ratings yet
- CS Blue Sheet Mnemonics - USMLE Step 2 CS - WWW - MedicalDocument1 pageCS Blue Sheet Mnemonics - USMLE Step 2 CS - WWW - MedicalRavi Parhar75% (4)
- New Harbinger Self-Help Workbook the Mindfulness and Acceptance Workbook for Social Anxiety and Shyness_ Using Acceptance and Commitment Therapy to Free Yourself From Fear and Reclaim Your Life [1st Ed.Document132 pagesNew Harbinger Self-Help Workbook the Mindfulness and Acceptance Workbook for Social Anxiety and Shyness_ Using Acceptance and Commitment Therapy to Free Yourself From Fear and Reclaim Your Life [1st Ed.Wesley Ramalho100% (1)
- Food Safety Is Everybody's Responsibility: PhilippinesDocument3 pagesFood Safety Is Everybody's Responsibility: PhilippinesMa. Regina GasparNo ratings yet
- Sample File: Lamentations Flame PrincessDocument5 pagesSample File: Lamentations Flame PrincessBraunerNo ratings yet
- Agricultural Stage Agriculture Was Started Affecting SoDocument8 pagesAgricultural Stage Agriculture Was Started Affecting Soyangi dokaNo ratings yet
- Gallucci (2004) - Immediate Loading With Fixed Screw-Retained Provisional Restorations in Edentulous Jaws, The Pickup Technique.Document10 pagesGallucci (2004) - Immediate Loading With Fixed Screw-Retained Provisional Restorations in Edentulous Jaws, The Pickup Technique.Antonio González Ruiz0% (1)
- Health Education of Menstrual Hygiene 1Document12 pagesHealth Education of Menstrual Hygiene 1chaudharitrushar007No ratings yet
- Personal Hygiene Kit Product Details PDFDocument3 pagesPersonal Hygiene Kit Product Details PDFZulfirdaus A'AdnanNo ratings yet